Abstract
Background:
Traumatic injuries are common dental problems in pediatric dentistry that may influence the children's quality of life.
Aim:
the aim of this study is to assess the impact of traumatic dental injuries (TDI) and oral health-related quality of life (OHRQoL) among Egyptian schoolchildren aged 11–14 years.
Materials and Methods:
A cross-sectional study was carried out involving a sample of 11700 schoolchildren from public and private schools of Mansoura city, Egypt. OHRQoL was assessed using Child Perceptions Questionnaire. Clinical examination included the presence and type of TDI, malocclusion status, and dental caries in anterior teeth (decayed, missing, and filled teeth).
Results:
The prevalence of TDI was 13.6%. Untreated TDI was more likely to have a negative impact on the children's daily living regarding pain, functional, emotional, and social aspect than treated injuries and control children. Pearson's correlation test indicated significant association between trauma and malocclusion and dental caries.
Conclusion:
Untreated dental injury has a negative impact on quality of life regarding social, functional, and emotional aspects. However, treated injured teeth appear to improve social and emotional aspects of the OHRQoL of school children, whereas functional limitations may continue because of the pulpal and periodontal effects of the injury.
Keywords: Dental trauma, malocclusion, quality of life
Introduction
Traumatic Dental Injury (TDI) in children can change their future dental health. There are principal causes of TDI as traffic accidents, high levels of violence, and greater participation of children in sports. Some studies claim that boys are more prone to dental trauma than girls which may be explained by male's higher participation in sports and physical activities.[1]
In the early 90s, Andreasen[2] hypothesized that dental trauma, in the future, will probably exceed dental caries and periodontal diseases. Since that hypothesis was made, several studies have been conducted in different populations and reported 7%–50% of the child population has sustained an orodental injury by the age of 15 years.
The prevalence of fractured teeth varies greatly in different population studies; Latin American nations reported dental trauma ranging from 12.2% to 72% in permanent as well as primary teeth.[3] In Kuwait, the prevalence was 14.9%,[4] Saudi Arabia 33%,[5] Iran 27.5%,[6] and Tanzania 21%.[7] The difference may be attributed to nationality, age, sex, and the fracture classification system utilized.[8]
Upper central incisors are the teeth more frequently affected by trauma, possibly because of their position in the mouth, being less protected than other teeth. The presence of an increased incisal overjet and anterior open bite are physical features that have been reported as predisposing factors of TDI.[9] The appearance and position of the anterior teeth have important psychological and social impacts on the children's quality of life. When injuries to incisor(s) produce pain, disfigurement, poor esthetics, or other psychological effects, children may avoid laughing or smiling, and this can affect their social relationships.[10] TDI has a distressing experience on physical, emotional, and psychological levels which have a great concern for the child, the parent, and the dentist.[1,2]
In the field of dentistry, oral health-related quality of life (OHRQoL) should address four dimensions: pain and discomfort; functional aspects concerning the ability to chew and swallow food without difficulty, as well as speaking and pronunciation; appearance and self-esteem; and social aspects reflecting social interaction and communication with people.[10]
Cortes et al.[11] reported that children with fractured teeth had a greater negative impact on eating and enjoying food, cleaning teeth, smiling, laughing than children without injury. In a Brazilian study,[12] there was a statistically significant association between the presence of traumatized treated teeth and children's OHRQoL. Another Brazilian study[13] showed no difference in overall scores between schoolchildren with treated or untreated TDI and without TDI but found that children with untreated TDI experienced a negative impact on social well-being (SW), mainly with regard to avoiding smiling or laughing, and in being concerned about what other people think or say.
Furthermore, TDI could adversely affect the developing occlusion, esthetics, and have a negative impact on these children lives. The development of the occlusion both functionally and esthetically during childhood is dependent on the satisfactory presence of teeth. When a trauma is inadequately treated, disastrous results can occur as malformed, malpositioned teeth, premature tooth loss, and pulpal death with abscess formation.[1]
Reliable data on dental trauma, its frequency and severity are still lacking in most countries, particularly in developing countries. In Egypt, there is a need for adequate information about TDI for the future preventive and management plans.
The purpose of this study is to (1) provide data on the prevalence of TDI among Egyptian schoolchildren aged 11–14 years. (2) Assess the impact of TDI and anterior malocclusion on OHRQoL of children.
Materials and Methods
A cross-sectional study involved 11–14-year-old children attending the last two grades of the primary schools in addition to the children attending the first two grades of the preparatory schools. The study design was approved by the Ethical Committee, Faculty of Dentistry, Mansoura University. The study was performed in Mansoura City, Capital of Dakahlia Governorate, Egypt. The sample size was calculated according to the method described by Scapini et al.[14] to be 12900 children. The city contains two educational districts, with a total of 50 primary (prim) and preparatory (prep) schools. Four public schools (2 prim and 2 prep) and one private school (which include the prim and prep) were randomly selected from Western region. Three public (2 prim and 1 prep) and one private school (also include the prim and prep) were selected randomly from the Eastern region. The purpose of the investigation was explained to the children and distributed to their parents with written consents through the head of each school. A total of 11820 parental approvals were returned. All the children attending the school at the examination day was included in the study. The study design formed of a questionnaire and clinical examination.
Questionnaires
Child Perceptions Questionnaire (CPQ11-14) consisted of 10 questions that measure OHRQoL of the children on 4 items: oral symptoms, functional limitations, emotional well-being, and SW. The questions assessed the frequency of the event during the past 3 months, on a five-point Likert scale. The answer will be “Never” =0; “Once/twice” =1; “Sometimes” =2; “Often” =3; or “Every day/almost every day” =4.[15] The questionnaires were self-administered by each child without any external influence. Questionnaires were distributed in Arabic language based on the validated Arabic translation of the English form of CPQ. The uncompleted questionnaires were excluded from the study. The final sample size was 11700 children who completed their questionnaires and then subjected to oral examination.
Clinical oral examination
Dental examination was done by two examiners. The examiners were calibrated to perform examinations with high inter- and intra-examiner agreement (weighted Kappa values: 0.89 and 0.94, respectively).
Dental examinations were carried out at the classroom using the natural light. Children were seated on ordinary chair, with the examiner seated, or standing behind them. Disposable mouth mirror and periodontal probe were used for dental examination. The examiners used appropriate equipment to protect against individual cross-infection, with all necessary instruments packed and sterilized.
The dental trauma index[16] was used to record evidence of injury to the upper and lower incisors. A score of 0: present and sound tooth; score 1: enamel fractures; score 2: fracture involving dentine; score 3: pulp involvement; score 4: crown discoloration without fracture; score 5: displacement injuries; and score 6: tooth loss.
The anterior malocclusion was assessed overbite, overjet, anterior open bite, crowding, spacing, and anterior crossbite. The presence or absence of anterior malocclusion is recorded as 1 or 0. Each child's caries experience was recorded using the decayed, missing, and filled teeth (DMFT) index with the DMFT components scored separately.
Statistical analysis was performed using the Statistical Package for the Social Sciences version 16.0 (SPSS for Windows; SPSS Inc., Chicago, IL, USA). Data were categorized as male and females, public and private schools, in addition to treated, untreated trauma and no trauma. The impact of trauma on the oral health of children was calculated as negative impacts which comprised of (sometimes, often, every day/almost every day) options and it is given score 1. The options “never” and “once/twice,” were considered as no impact and given a score 0. Chi-square test was used to compare the different groups and Fisher's exact test (F test) for post hoc test. Correlation between dental trauma and gender, malocclusion, and dental caries was determined using Pearson's correlation test.
Results
The number of children examined was 11700, 61% males and 39% females. The prevalence of receiving trauma was 16.2% in males and 9.6% in females with common prevalence to be 13.6%. The percentage of public schools was (91.7%) of the examined children with the prevalence of 12.8%. The prevalence was 22.5% in private school children. The difference was statistically significant. About 63.25% of the traumatized children had received treatment, whereas 36.75% had untreated traumatized teeth.
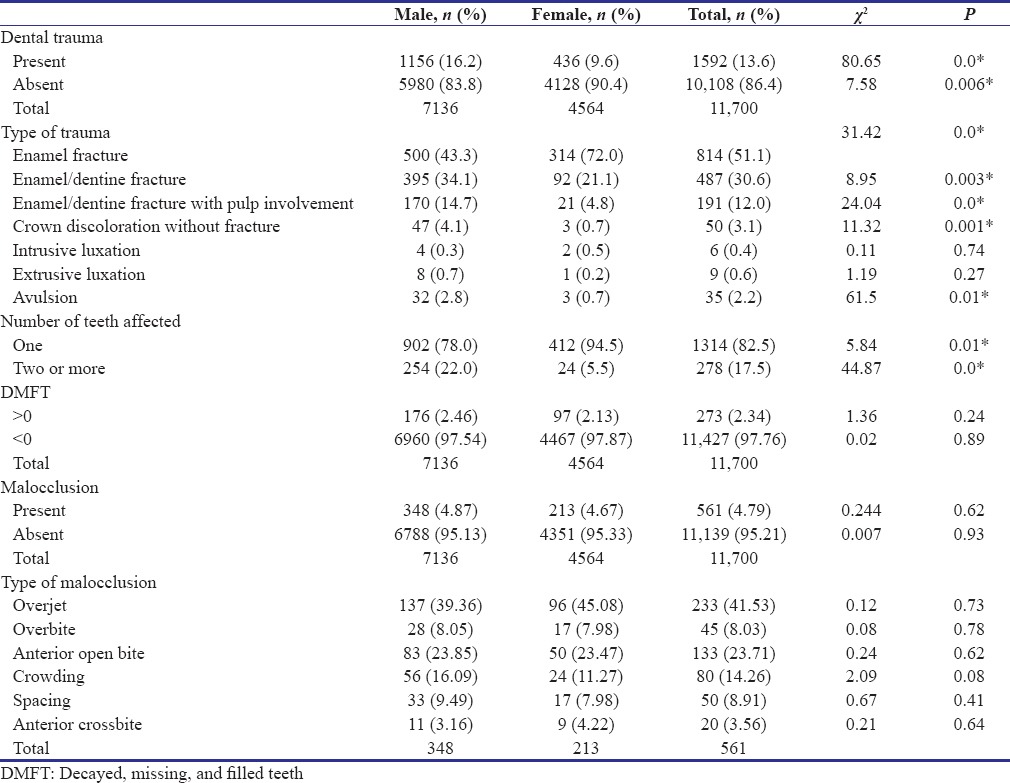
The rates of injury were significantly higher in males than in females [Table 1]. The most commonly observed traumatic injury was enamel fracture (51.1%) followed by enamel-dentin fracture (30.6%), fracture with pulp involvement (12%), crown discoloration without fracture (3.1%), avulsion (2.2%), extrusive luxation (0.6%), and intrusive luxation (0.4%). Although males displayed more prevalence of TDI, females displayed significantly higher prevalence of one fractured tooth. DMFT and malocclusion showed no significant difference between males and females.
Table 1.
The distribution of children according to the prevalence of dental trauma, type of trauma, number of teeth affected regarding gender
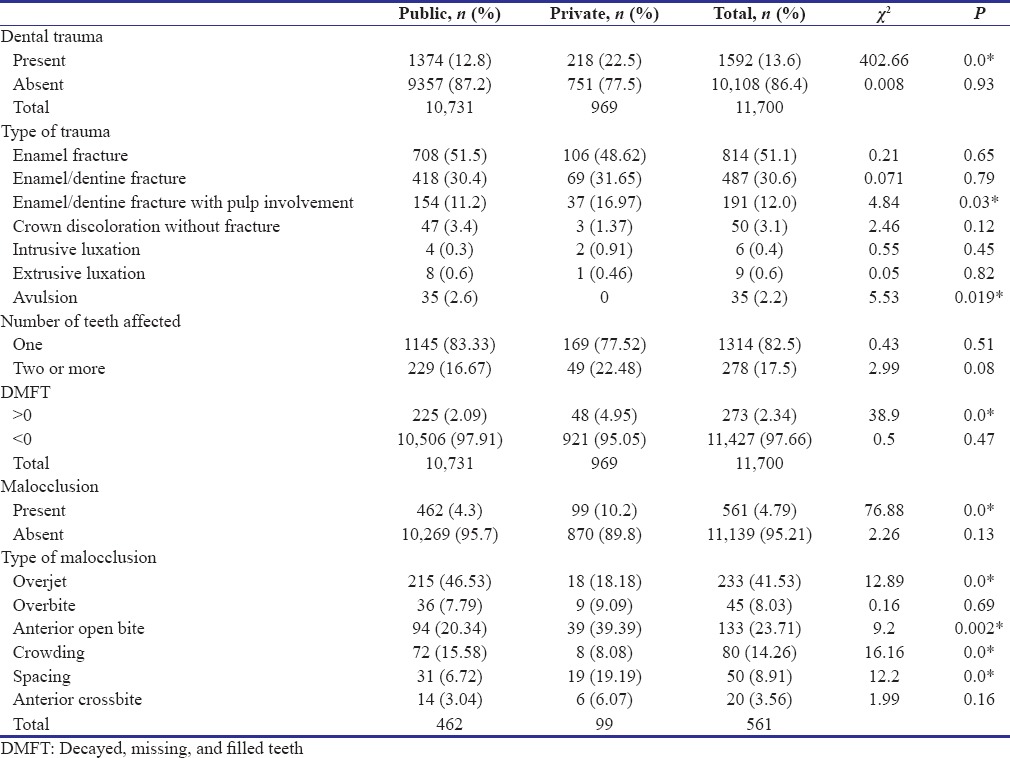
DMFT and malocclusion were significantly higher in the private schools compared to the public schools [Figure 1 and Table 2].
Figure 1.
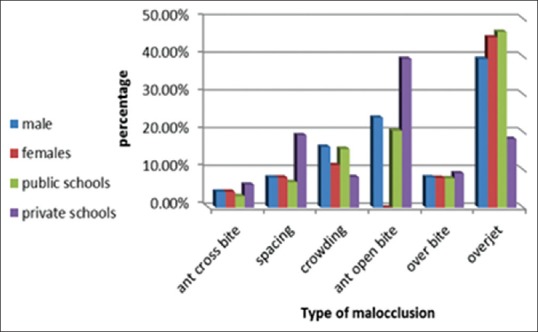
Type of malocclusion regarding the gender and school type
Table 2.
The distribution of children according to the prevalence of dental trauma, type of trauma, number of teeth affected regarding public and private schools
The oral symptoms, functional limitation, SW, and emotional well-being dimensions were negatively affected by dental trauma. The most prevalent CPQ11-14 impact was dental pain (66.49%) for children with untreated dental injuries and (24.6%) for treated dental injuries [Table 3]. The second most prevalent impacts were functional limitation followed by emotional well-being then SW.
Table 3.
The impact of dental trauma on oral health-related quality of life
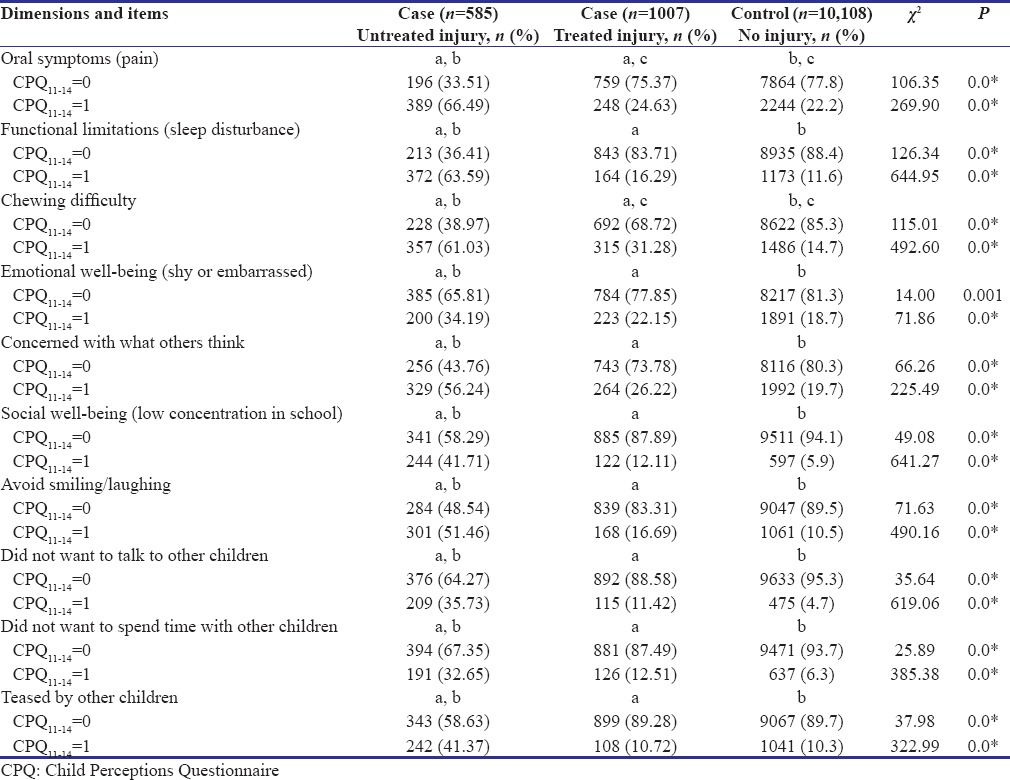
Untreated traumatized children showed a significantly higher impact on their quality of life compared to treated and uninjured groups. On the other hand, there was a statistically significant difference between uninjured versus treated injured teeth regarding pain and difficulty in chewing items only.
Discussion
In the field of pediatric dentistry, one of the common dental problems is TDI. Certainly, dental trauma may result in fractured, displaced, or lost anterior teeth, and this could have significant functional, esthetic, speech, and psychological effects on children thus affecting their quality of life.
The present study showed that the prevalence of TDI in this population was approximately 13.6%. Several studies showed significant differences in the occurrence of TDI between genders, and a higher prevalence in boys had been consistently found.[17,18,19,20] The present survey is in agreement with these studies as it reported higher prevalence of males than females. It was stated that males frequently engage in contact sports and intense/competitive activities, which increase the risk for accidents.[21] Furthermore, this may explain the higher prevalence of male children with >1 fractured teeth in our study.
This study showed a significant negative impact of TDI among Egyptian 11–14-year-old schoolchildren. The unsatisfied appearance of untreated fractured incisors reduced smiling, laughing, and socializing with others. This is in agreement with results of Cortes et al.[11] and Traebert et al.[22] who suggested that esthetics rather than function were major concerns for children with fractured teeth.
This study also showed that children with treated teeth gained improvement in esthetics, emotional well-being, and social interactions following crown restoration. Although they still have some pain and functional limitations with respect to chewing difficulty. Fakhruddin et al.[23] suggested that restored crown is only a part of the injury treatment. Pulpal pain and periodontal ligament damage must be considered as having long-term effects on chewing and possibly on sensibility and pain.
Santos et al.[24] also supported our results, they found a negative impact of TDI on the functional and emotional well-being. The TDI impact was related to “delay and difficulty in chewing,” “embarrassed or ashamed,” and “caring about what others were thinking of appearance.” On the other hand, Bendo et al.[13] showed that children with untreated TDI experienced a negative impact only on SW, mainly with regard to avoiding smiling or laughing, and in being concerned about what other people think or say.
This study showed a significant association of malocclusion and TDI. Malocclusion has a negative impact on OHRQoL. The severity of malocclusion was significantly related to higher scores of CPQ11-14. The scores of CPQ11-14 increased by each increase in the severity of malocclusion. This is in accordance with other studies which showed significant association between increased malocclusion and CPQ11-14 scores mainly for social and emotional well-being.[25] Furthermore, a previous study has shown an increased risk of TDI in children with increased overjets.[26]
The current study showed a significant association of TDI and pain among Egyptian children which is supported by a previous Brazilian study reported a strong association between toothache and dental trauma in preschool children.[27] In a Sudanese study, toothache was the most frequently associated cause of nearly all impacts in both private and public school attendees.[28] An Indian study reported negative impact of toothache on daily living activities of 12-year-old children.[29]
In children with dental trauma experience, dental fear and anxiety are direct consequences of a negative sensation associated with the pain caused by this traumatic injury. Painful experience is expected to have a higher risk to develop dental anxiety, which is a serious reason for avoidance of dental treatment later in life.[30] it is important to introduce an indicated psychological approach and consider every possibility of nonpainful treatment in pediatric dental patients, particularly those with dental trauma injuries.
This study showed that TDI negatively affects schoolchildren's oral health quality of life. Based on this finding, pediatric dentists should exert every effort to reduce the prevalence of TDI and successfully manage dental injury taking into consideration the following measures: 1) elimination or reduction of predisposing factors to create safe environment to avoid the negative impact on children oral health. 2) providing information for children and their parents to avoid situation leading to trauma. 3) providing protective devices for susceptible children to protect the face and teeth from trauma. 4) encourages the use of mouthguards during sporting activities, which reduce the incidence and severity of dental injuries. 5) pediatric dentists should immediately treat any signs of TDI. Since the occlusal relationship is a risk factor of TDI, early orthodontic treatment in predisposed children may be an effective prevention strategy.
Conclusion
It was concluded that untreated dental injuries had a more negative impact on the children's daily life than treated injuries. Malocclusion and caries were significantly associated with the occurrence of TDI.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank all participated children and their parents for their great assistance in this study and everyone who help us in this work.
References
- 1.Peterson EE, Anderson L, Sorensen S. Traumatic oral vs.non-oral injuries. Swedish Dent J. 1997;21:55. [PubMed] [Google Scholar]
- 2.Andreasen JO, Andreasen FM. Textbook and Color Atlas of Traumatic Injuries to the Teeth. 3rd ed. Copenhagen: Munksgaard; 1994. [Google Scholar]
- 3.Llarena del Rosario ME, Acosta Alfaro VM, Garcia-Godoy F. Traumatic injuries to primary teeth in Mexico city children. Endod Dent Traumatol. 1992;8:213–4. doi: 10.1111/j.1600-9657.1992.tb00245.x. [DOI] [PubMed] [Google Scholar]
- 4.Artun J, Behbehani F, Al-Jame B, Kerosuo H. Incisor trauma in a adolescent Abab population: Prevalence, severity, and occlusal risk factors. Am J Orthod Dentofacial Orthop. 2005;128:347–52. doi: 10.1016/j.ajodo.2004.06.032. [DOI] [PubMed] [Google Scholar]
- 5.Al-Majed I, Murray JJ, Maguire A. Prevalence of dental trauma in 5-6- and 12-14-year-old boys in Riyadh, Saudi Arabia. Dent Traumatol. 2001;17:153–8. doi: 10.1034/j.1600-9657.2001.170403.x. [DOI] [PubMed] [Google Scholar]
- 6.Navabazam A, Farahani SS. Prevalence of traumatic injuries to maxillary permanent teeth in 9- to 14-year-old school children in Yazd, Iran. Dent Traumatol. 2010;26:154–7. doi: 10.1111/j.1600-9657.2009.00861.x. [DOI] [PubMed] [Google Scholar]
- 7.Gábris K, Tarján I, Rózsa N. Dental trauma in children presenting for treatment at the department of dentistry for children and orthodontics, Budapest, 1985–1999. Dent Traumatol. 2001;17:103–8. doi: 10.1034/j.1600-9657.2001.017003103.x. [DOI] [PubMed] [Google Scholar]
- 8.Glendor U. Aetiology and risk factors related to traumatic dental injuries – A review of the literature. Dent Traumatol. 2009;25:19–31. doi: 10.1111/j.1600-9657.2008.00694.x. [DOI] [PubMed] [Google Scholar]
- 9.Alonge OK, Narendran S, Williamson DD. Prevalence of fractured incisal teeth among children in Harris County, Texas. Dent Traumatol. 2001;17:218–21. doi: 10.1034/j.1600-9657.2001.170506.x. [DOI] [PubMed] [Google Scholar]
- 10.Slade GD. Assessment of oral health-related quality of life. In: Inglehart MR, Bagramian RA, editors. Oral Health-Related Quality of Life. Chicago, IL: Quintessence; 2002. pp. 66–79. [Google Scholar]
- 11.Cortes MI, Marcenes W, Sheiham A. Impact of traumatic injuries to the permanent teeth on the oral health-related quality of life in 12–14-year-old-children. Community Dent Oral Epidemiol. 2002;30:193–8. doi: 10.1034/j.1600-0528.2002.300305.x. [DOI] [PubMed] [Google Scholar]
- 12.Ramos-Jorge ML, Bosco VL, Peres MA, Nunes AC. The impact of treatment of dental trauma on the quality of life of adolescents: A case-control study in Southern Brazil. Dent Traumatol. 2007;23:114–9. doi: 10.1111/j.1600-9657.2005.00409.x. [DOI] [PubMed] [Google Scholar]
- 13.Bendo CB, Paiva SM, Torres CS, Oliveira AC, Goursand D, Pordeus IA, et al. Association between treated/untreated traumatic dental injuries and impact on quality of life of Brazilian schoolchildren. Health Qual Life Outcomes. 2010;8:114. doi: 10.1186/1477-7525-8-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scapini A, Feldens CA, Ardengh TM, Kramer PF. Malocclusion impacts adolescents’ oral health-related quality of life. Angle Orthod. 2013;83:512–8. doi: 10.2319/062012-509.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jokovic A, Locker D, Guyatt G. Short forms of the child perceptions questionnaire for 11-14-year-old children (CPQ11-14): Development and initial evaluation. Health Qual Life Outcomes. 2006;4:4. doi: 10.1186/1477-7525-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown A, Al-Khayal Z. Validity and reliability of the Arabic translation of the childoral-health-related quality of life questionnaire (CPQ11-14) in Saudi Arabia. Int J Pediatr Dent. 2006;16:405–11. doi: 10.1111/j.1365-263X.2006.00775.x. [DOI] [PubMed] [Google Scholar]
- 17.Naidoo S, Sheiham A, Tsakos G. Traumatic dental injuries of permanent incisors in 11- to 13-year-old South African schoolchildren. Dent Traumatol. 2009;25:224–8. doi: 10.1111/j.1600-9657.2008.00749.x. [DOI] [PubMed] [Google Scholar]
- 18.Marcenes W, Zabot NE, Traebert J. Socio-economic correlates of traumatic injuries to the permanent incisors in schoolchildren aged 12 years in Blumenau, Brazil. Dent Traumatol. 2001;17:222–6. doi: 10.1034/j.1600-9657.2001.170507.x. [DOI] [PubMed] [Google Scholar]
- 19.Nicolau B, Marcenes W, Sheiham A. The relationship between traumatic dental injuries and adolescents’ development along the life course. Community Dent Oral Epidemiol. 2003;31:306–13. doi: 10.1034/j.1600-0528.2003.t01-1-00019.x. [DOI] [PubMed] [Google Scholar]
- 20.Nicolau B, Marcenes W, Sheiham A. Prevalence, causes and correlates of traumatic dental injuries among 13-year-olds in Brazil. Dent Traumatol. 2001;17:213–7. doi: 10.1034/j.1600-9657.2001.170505.x. [DOI] [PubMed] [Google Scholar]
- 21.Damé-Teixeira N, Alves LS, Susin C, Maltz M. Traumatic dental injury among 12-year-old South Brazilian schoolchildren: Prevalence, severity, and risk indicators. Dent Traumatol. 2013;29:52–8. doi: 10.1111/j.1600-9657.2012.01124.x. [DOI] [PubMed] [Google Scholar]
- 22.Traebert J, de Lacerda T, Lyndie A, Thomson W, Bortoluzzi M. Impact of traumatic dental injuries on the quality of life of schoolchildren. Dent Traumatol. 2012;28:423–8. doi: 10.1111/j.1600-9657.2012.01114.x. [DOI] [PubMed] [Google Scholar]
- 23.Fakhruddin KS, Lawrence HP, Kenny DJ, Locker D. Impact of treated and untreated dental injuries on the quality of life of Ontario school children. Dent Traumatol. 2008;24:309–13. doi: 10.1111/j.1600-9657.2007.00547.x. [DOI] [PubMed] [Google Scholar]
- 24.Santos A, Faria D, Spitz B, Volpe A. Impact of traumatic dental injury on the quality-of-life of children and adolescents: A case-control study. Acta Odontol Scand. 2013;71:1123–8. doi: 10.3109/00016357.2012.750011. [DOI] [PubMed] [Google Scholar]
- 25.Ankola AV, Hebbal M, Sharma R, Nayak SS. Traumatic dental injuries in primary school children of South India – A report from district-wide oral health survey. Dent Traumatol. 2013;29:134–8. doi: 10.1111/j.1600-9657.2012.01139.x. [DOI] [PubMed] [Google Scholar]
- 26.Nguyen QV, Bezemer PD, Habets L, Prahl-Andersen B. A systematic review of the relationship between overjet size and traumatic dental injuries. Eur J Orthod. 1999;21:503–15. doi: 10.1093/ejo/21.5.503. [DOI] [PubMed] [Google Scholar]
- 27.Goettems ML, Azevedo MS, Correa MB, Costa CT, Wendt FP, Schuch HS, et al. Dental trauma occurrence and occlusal characteristics in Brazilian preschool children. Pediatr Dent. 2012;34:104–7. [PubMed] [Google Scholar]
- 28.Nurelhuda NM, Ahmed MF, Trovik TA, Šstrøm AN. Evaluation of oral health-related quality of life among Sudanese schoolchildren using child-OIDP inventory. Health Qual Life Outcomes. 2010;8:152. doi: 10.1186/1477-7525-8-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dandi KK, Raom EV, Margabandhu S. Dental pain as a determinant of expressed need for dental care among 12-year-old school children in India. Indian Dent Res. 2010;22:611. doi: 10.4103/0970-9290.90320. [DOI] [PubMed] [Google Scholar]
- 30.Berggren U, Meynert G. Dental fear and avoidance: Causes, symptoms, and consequences. J Am Dent Assoc. 1984;109:247–51. doi: 10.14219/jada.archive.1984.0328. [DOI] [PubMed] [Google Scholar]


