Abstract
The aim of the present study was to investigate the expression levels of the T-cell immunoglobulin and mucin domain-containing protein-3 (TIM-3) and galectin-9 proteins and their clinical value in esophageal squamous cell carcinoma (ESCC) in Chinese patients. The expression profiles of TIM-3 and galectin-9 in ESCC were determined by the immunohistochemical analysis of the postoperative pathological specimens of 45 patients with ESCC; a χ2 test was used to evaluate the association of TIM-3 and galectin-9 expression with clinicopathological parameters, in addition to univariate and multivariate Cox's proportional hazards model to analyze the prognostic value of the expression of TIM-3 and galectin-9 proteins. The proportion of samples exhibiting a high staining intensity for TIM-3 and galectin-9 were 22.22 and 15.56%, respectively: these samples were termed the TIM-3 high-expression group (HEG) and galectin-9-HEG. There was a negative correlation between the expression of TIM-3 and galectin-9 (R=−0.71, P<0.001). The results of Kaplan-Meier survival analysis led to the conclusion that, compared with the TIM-3 low expression group (LEG), patients in the TIM-3-HEG exhibited a poorer overall survival rate (χ2=6.049, P=0.0139). By contrast, patients in the galectin-9-HEG exhibited a significantly better overall survival rate than those in the galectin-9-LEG (χ2=4.915, P=0.0266). However, the levels of TIM-3 and galectin-9 expression were not identified as independent indicators for the prognosis of patients with ESCC. As high TIM-3 and low galectin-9 expression levels were associated with a poor prognosis for patients with ESCC in the present study, these proteins may be potential prognostic indicators for ESCC.
Keywords: T-cell immunoglobulin and mucin domain-containing protein-3, galectin-9, esophageal squamous cell carcinoma, immunosuppression
Introduction
Esophageal carcinoma is the sixth most common cause of cancer-associated mortality worldwide, with a 5-year survival rate of 15–25% in 2000 (1). The incidence and mortality of esophageal cancer are the fifth and fourth in China, respectively; it is particularly prevalent in rural areas (2). Esophageal squamous cell carcinoma (ESCC) is more prevalent than esophageal adenocarcinoma (EAC); it is the predominant form of esophageal cancer worldwide and in Asia, with >100 cases per 100,000 population annually in 2000 (3). Although epidemiological studies indicate that tobacco smoking and alcohol consumption are the primary behavioral risk factors for ESCC, not all tobacco and alcohol users ultimately develop ESCC (4). Genetic risk factors, including single nucleotide polymorphisms, may also affect the susceptibility to ESCC (4,5). The methods by which esophageal cancer typically progresses include direct infiltration, lymphatic metastasis and hematogenous dissemination. Current treatment modalities include surgery, radiotherapy, chemotherapy or combinations of these treatments; however, the 5-year survival rate of parents with ESCC remains unsatisfactory (3). Identifying novel valid tumor esophageal cancer biomarkers, that may potentially be used to achieve early diagnosis, identify therapeutic targets, evaluate the effects of therapy and predict prognosis, is an emerging field (3). The human immune system aids the resistance and elimination of tumors and can influence esophageal carcinogenesis, with the most pivotal antitumor immune response mediated by T lymphocytes (6,7). Therefore, polymorphisms in immune response-associated genes and corresponding proteins that regulate the activation and proliferation of T lymphocytes may contribute to ESCC pathogenesis (8).
Similar to other members of the T-cell immunoglobulin and mucin domain-containing protein (TIM) family, TIM-3 has a structural organization that includes an N-terminal immunoglobulin V (IgV) domain, amucin domain, a transmembrane domain and a cytoplasmic tail, which is selectively expressed by interferon-γ (IFN-γ)-secreting CD4+ T helper 1 (Th1), CD8+ T cytotoxic 1 (Tc1) T cells and on cells of the innate immune system (9–12). TIM-3 binds to its ligand galectin-9, which can induce apoptosis in Th1 cells to downregulate effector Th1/Tc1 cell responses and suppress, as well as induce, peripheral tolerance (13,14). Monoclonal antibodies can block the immune checkpoint pathway, which acts on T-cell inhibitory or immune checkpoint receptors; immunotherapy has demonstrated as an effective strategy for the treatment of cancer (15). TIM-3 is expressed by the majority of suppressed or dysfunctional T cell populations, including CD8+ T cells and Tregs, which exert key roles in immunosuppression in tumor tissue based on preclinical trials (16–18). Evidence indicates that TIM-3 represents a critical immune checkpoint in various types of malignancy (16–19). Compared with the cytotoxic T lymphocyte antigen or programmed cell death-1, which are expressed on all T cells, TIM-3 is selectively expressed on IFN-γ-producing T cells and is likely to be expressed primarily by intratumoral T cells in patients with cancer (20–22). Therefore, targeting TIM-3 could reduce the risk of adverse autoimmune-like toxicity (22). In addition, it has been demonstrated that the knockdown of TIM-3 in tumor cells can weaken their proliferative and invasive ability (23). Evidence indicates that TIM-3 may have a direct role in the occurrence and progression of tumors as it has been observed on tumor cells; it may accelerate oncogenesis, proliferation and invasion of the tumor cells directly or act via immune inhibition (23,24).
The inhibitory capacity of TIM-3 was previously assessed by identifying the effect of the blockade of the interaction of TIM-3 with one or more of its ligands (25). Of these ligands, TIM-3 deficiency decreased the galectin-9-mediated apoptosis of Th1 cells by ~40% (26), which indicates that galectin-9 has multiple target molecules in addition to TIM-3 (14). Further evidence revealed that galectin-9 acts independently of TIM-3 in influencing T cell function (27). Conversely, another study refuted this, reporting thatgalectin-9 and TIM-3 may both serve roles in regulating T cell responses (28). Galectin-9 is widely expressed on the surface of cells and in the cytoplasm, and may interact with TIM-3 by binding to ligosaccharides present on the TIM-3 IgV domain. IFN-γ can promote the expression of galectin-9. Previous research demonstrated that the rate of cell death in TIM-3+ Th1 cells decreased and caused a consequent decline in IFN-γ production when galectin-9 was bound by TIM-3. Thus, the TIM-3-galectin-9 pathway has an inhibitory effect on T cells (14,29).
Blockade of the TIM-3-galectin-9 signal pathway may additionally interact with the external mechanism of interference of T cells in immunosuppression. However, it has yet to be identified whether TIM-3 and galectin-9 are expressed in ESCC tumors and their roles in ESCC. The present study aimed to investigate the association between the expression level of TIM-3 and galectin-9 with a range of clinicopathological characteristics and patient survival time in ESCC patients, in order to investigate the potential prognostic significance of TIM-3 and galectin-9 in ECSS in Chinese patients.
Materials and methods
Clinical samples
Postoperative pathological specimens from 45 patients diagnosed with ESCC who received surgery at the Affiliated Tumor Hospital of Zhengzhou University (Zhengzhou, China) between January 2008 and December 2009 were included the present study. All clinicopathological data was gathered by reviewing medical records and conducting telephone interviews. No patients received radiotherapy or chemotherapy prior to curative resection, from which samples were obtained. Following surgery, patients received postoperative adjuvant therapies and follow-ups regularly in line with National Comprehensive Cancer Network (NCCN) guidelines (30). Patient age ranged from 46–72 years (median, 58 years). The basic information of the 45 ESCC patients is presented in Table I. Tumor pathological specimens were used in the immunohistochemical (IHC) assays. All patients agreed to inclusion in the present study, providing written informed consent. The present study was also approved by the ethics committee of the Affiliated Tumor Hospital of Zhengzhou University.
Table I.
Patient characteristics, and their association with TIM-3 or galectin-9 expression.
| TIM-3, n | Galectin-9, n | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Clinical features | Patients, n (%) | HEG | LEG | χ2 | P-value | HEG | LEG | χ2 | P-value |
| Total | 45 | 10 | 35 | 7 | 38 | ||||
| Sex | 0.495 | 0.482 | 0.000 | 0.984 | |||||
| Female | 13 (28.89) | 2 | 11 | 2 | 11 | ||||
| Male | 32 (71.11) | 8 | 24 | 5 | 27 | ||||
| Age, years | 0.319 | 0.572 | 2.899 | 0.089 | |||||
| <60 | 26 (57.78) | 5 | 21 | 2 | 24 | ||||
| ≥60 | 19 (42.22) | 5 | 14 | 5 | 14 | ||||
| Tumor size, cm | 3.401 | 0.065 | 2.445 | 0.118 | |||||
| <4 | 20 (44.44) | 7 | 13 | 5 | 15 | ||||
| ≥4 | 25 (55.56) | 3 | 22 | 2 | 23 | ||||
| Lymph node metastasis | 0.294 | 0.588 | 0.534 | 0.465 | |||||
| Yes | 14 (31.11) | 4 | 10 | 3 | 11 | ||||
| No | 31 (68.89) | 6 | 25 | 4 | 27 | ||||
| Depth of invasion | 1.086 | 0.297 | 0.846 | 0.358 | |||||
| TI+T2 | 20 (44.44) | 3 | 17 | 2 | 18 | ||||
| T3 | 25 (55.56) | 7 | 18 | 5 | 20 | ||||
| TNM stage | 1.684 | 0.194 | 1.522 | 0.217 | |||||
| II | 34 (75.56) | 6 | 28 | 4 | 30 | ||||
| III | 11 (24.44) | 4 | 7 | 3 | 8 | ||||
| Tumor location | |||||||||
| Upper thoracic | 11 (24.44) | 0 | 11 | 4.211 | 0.122 | 0 | 11 | 2.749 | 0.112 |
| Middle thoracic | 30 (66.67) | 9 | 21 | 6 | 24 | ||||
| Lower thoracic | 4 (8.89) | 1 | 3 | 1 | 3 | ||||
| Pathological type | 0.817 | 0.366 | 1.322 | 0.250 | |||||
| Ulcerated | 28 (62.22) | 5 | 23 | 3 | 25 | ||||
| Non-ulcerated | 17 (37.78) | 5 | 12 | 4 | 13 | ||||
| Differentiation | |||||||||
| Poor | 14 (31.11) | 3 | 11 | 0.030 | 0.985 | 1 | 13 | 1.097 | 0.578 |
| Middle | 26 (57.78) | 6 | 20 | 5 | 21 | ||||
| Well | 5 (11.11) | 1 | 4 | 1 | 4 | ||||
| Smoking history | 1.435 | 0.231 | 0.048 | 0.826 | |||||
| No | 21 (46.67) | 3 | 18 | 3 | 18 | ||||
| Yes | 24 (53.33) | 7 | 17 | 4 | 20 | ||||
| Family history | 1.029 | 0.310 | 0.085 | 0.771 | |||||
| No | 40 (88.89) | 8 | 32 | 6 | 34 | ||||
| Yes | 5 (11.11) | 2 | 3 | 1 | 4 | ||||
TIM-3, T-cell immunoglobulin and mucin-domain containing-3; HEG, high-expression group; LEG, low-expression group.
Follow-up
To determine the condition of each patient, medical records were reviewed or telephone interviews conducted every 3 months for the first year, every 6 months for the second year and annually thereafter. The primary end point was patient mortality, from which overall survival (OS) time was calculated, defined as the time from the date of resection until death; the secondary endpoint was the last follow-up.
IHC staining
Formalin-fixed, paraffin-embedded tissue samples were cut into sections of 4-µm thickness, heated at 60°C overnight and then deparaffinized and rehydrated using a graded alcohol series: xylene I-xylene II-absolute ethanol I-absolute ethanol II-95% ethanol-90% ethanol-80% ethanol-70% ethanol. Sections were then boiled for 30 sec in 10 mmol/l sodium citrate buffer (pH 6) in a high-pressure boiler. Following the blocking of the endogenous peroxidase activity with 3% hydrogen peroxide for 10 min at room temperature, slides were washed with 0.01 mol/lPBS for 3 min. Following incubation with the primary human galectin-9 polyclonal antibody (dilution, 1:250; ab69630; Abcam, Cambridge UK) and Tim-3-phycoerythrin (dilution, 1:200; 565560; BD Biosciences, Franklin Lakes, NJ, USA), respectively, for 1 h at room temperature, biotinylated goat anti-rabbit immunoglobulin (Ig)G (1:200; cat. no. NB7183; Novus Biologicals, LLC, Littleton, CO, USA) was added for 30 min at 37°C. Then the slides were washed with PBS, and counterstained with a diaminobenzidine peroxidase substrate kit (Gene Tech Biotechnology Co., Ltd., Shanghai, China). Hematoxylin and eosin staining was used to evaluate histopathological expression for 1 min at room temperature.
Evaluation of IHC results
The expression of TIM-3 and galectin-9 were evaluated with an optical microscope by two independent pathologists who were unfamiliar with the clinical data of patients and images were captured. To calculate the expression intensity of TIM-3 and galectin-9, representative areas of the stained regions were selected under low-power microscopy (magnification, ×100), and high-power microscopy (magnification, ×400) was used to count TIM-3 and galectin-9 positive cells in 5 fields of view using a Leica DMI 4000B inverted research microscope (Leica Microsystems GmbH, Wetzlar, Germany). As negative controls, the tumor slices were treated with distilled water instead of primary antibody and horseradish-conjugated goat anti-rabbit IgG (1:200; NB7183; Novus Biologicals, LLC) was used instead of the secondary antibody for 30 min at 37°C; all negative controls showed negligible background staining. The percentage of TIM-3-positive and galectin-9-positivecells in ESCC samples were counted and the immunostaining intensity quantified. According to the semi-quantitative HSCORE system (score=stain intensity × mean percentage of stained cells), the stain intensity was ranked into 4 grades: No staining=−, weak staining=+1, moderate staining=+2 and strong staining=+3.0 were pointed as negative (−), 1 as weakly positive (+), 2 as moderately positive (+ +), ≥3 as strong positive (+ + +). Those≥3 points were considered to be positive, the rest were considered to demonstrate negative expression. The percentage of stained cells was identified concurrently. If the final results from the two pathologists were not consistent, specimens were reviewed together until a consensus was agreed upon.
Statistical analysis
SPSS 19.0 statistical software (IBM Corp., Armonk, NY, USA) was used to analyze all statistical data. χ2 test and Spearman's rank correlation coefficient were used to analyze differences in classified variables between groups and the correlation between the expression level of TIM-3 and galectin-9, respectively. The OS rate was assessed using the Kaplan-Meier method; survival differences were evaluated using the log-rank test. Univariate and multivariate analyses of prognostic factors for survival were performed using Cox's proportional hazards model. P<0.05 was considered to indicate a statistically significant difference.
Results
IHC results of TIM-3 and galectin-9 expression in ESCC tissues
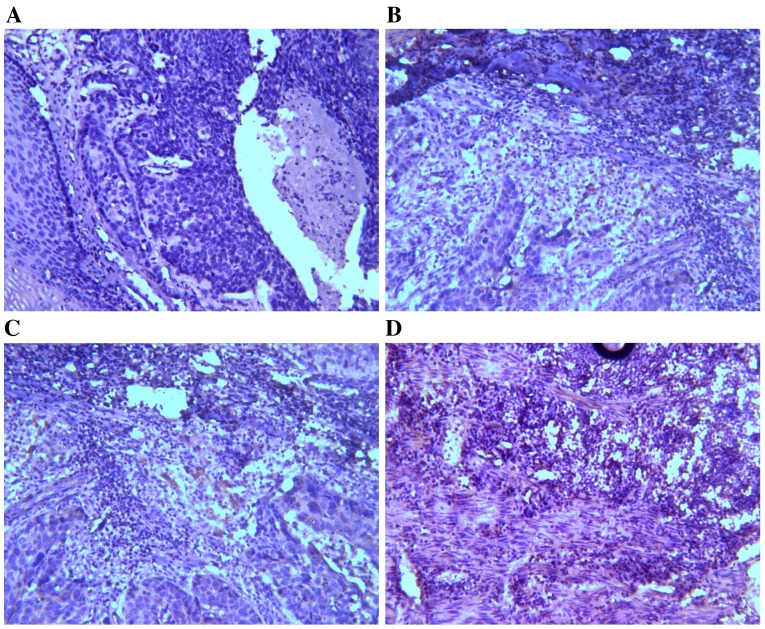
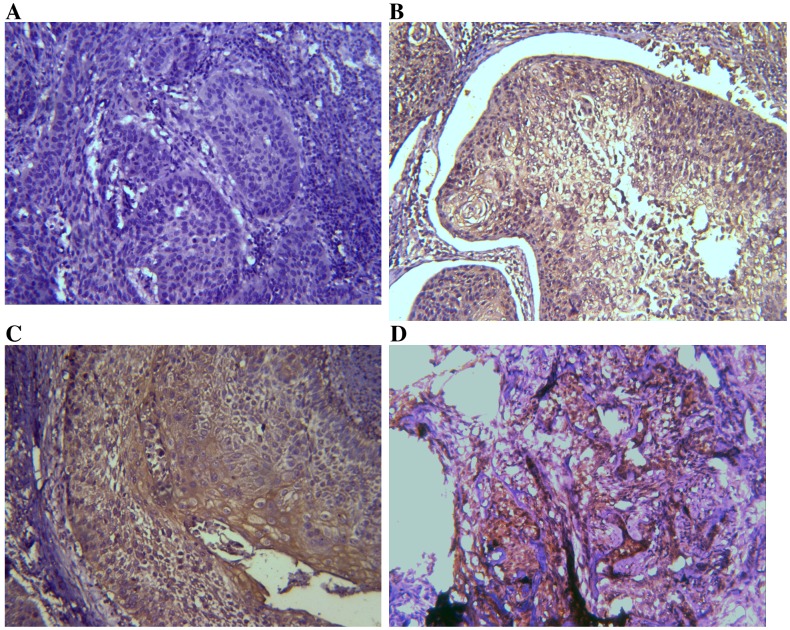
Expression levels of TIM-3 and galectin-9 were investigated by IHC analysis. TIM-3 and galectin-9 are expressed in a variety of cells in the immune system and have also been identified in certain types of tumor (24). It was assessed whether TIM-3 and galectin-9 are also expressed in ESCC tissues (Figs. 1 and 2). On the basis of the positive expression intensity of cancer cells, the protein levels of TIM-3 and galectin-9 were quantified. Of the 45 cases, TIM-3 protein levels were of +3 staining intensity (TIM-3 high-expression group; TIM-3-HEG) in 10 cases (22.22%) and 35 cases (77.78%) were of lower staining intensity (TIM-3 low-expression group; TIM-3-LEG), of which 11 cases were +2, 23 cases were +1 and 1 case was 0. Concerning galectin-9 expression levels, 7 cases (15.56%) were of +3 staining intensity (galectin-9-HEG) and 38 cases (84.44%) were of lower staining intensity (galectin-9-LEG), including 14 cases that were +2, 13 cases that were +1 and 11 cases that were 0.
Figure 1.
Representative images of immunohistochemical staining for T-cell immunoglobulin and mucin domain-containing protein-3 in human esophageal squamous cell carcinoma tissues. (A) No staining; (B) weak staining intensity; (C) intermediate staining intensity; (D) strong staining intensity.
Figure 2.
Representative images of immunohistochemical staining for galectin-9 in human esophageal squamous cell carcinoma tissues. (A) No staining; (B) weak staining intensity; (C) intermediate staining intensity; (D) strong staining intensity.
Association between TIM-3 and galectin-9 expression, and clinicopathological factors
The association of TIM-3 or galectin-9 expression with a variety of associated clinicopathological factors influencing the prognosis in ESCC was investigated. The outcomes are included in Table I. There were no significant statistical differences in age between the HEGs and LEGs for TIM-3 and galectin-9. Additionally, other clinical pathological characteristics, including tumor differentiation, Tumor-Node-Metastasis (TNM) stage (the seventh edition of AJCCTNM staging of esophageal cancer) (31), lymph node metastasis status and tumor size, were also not significantly associated with TIM-3 and galectin-9.
Rank correlation between TIM-3 and galectin-9 expression
Of the 45 ESCC specimens, 3 were TIM-3-HEG and galectin-9-HEG, 7 were TIM-3-HEG and galectin-9-LEG, 4 were TIM-3-LEG and galectin-9-HEG and 31 were TIM-3-LEG and galectin-9-LEG. Through a Spearman's rank correlation test, it was determined that expression of the two proteins exhibited a significant negative correlation (R=−0.71, P<0.001). The results of this analysis are included in Table II.
Table II.
Correlation between the expression of TIM-3 and galectin-9 protein in esophageal squamous cell carcinoma.
| Expression of galectin-9 | ||||
|---|---|---|---|---|
| Expression of TIM-3 | HEG | LEG | R-value | P-value |
| HEG | 3 | 7 | −0.71 | <0.001 |
| LEG | 4 | 31 | ||
TIM-3, T-cell immunoglobulin and mucin-domain containing-3; HEG, high-expression group; LEG, low-expression group.
Association between TIM-3, galectin-9 and disease-specific survival time
Survival analysis with the Kaplan-Meier method revealed that patients in the TIM-3-HEG attained a significantly shorter disease-specific survival time than those in the TIM-3-LEG (χ2=6.049, P=0.0139; Fig. 3); however, patients in the galectin-9-HEG exhibited a significantly higher disease-specific survival time relative to those in the galectin-9-LEG (χ2=4.915, P=0.0266; Fig. 4). To assess the effect of clinical pathological characteristics on the survival time for patients with ESCC, a univariate analysis was conducted. As included in Table III, TNM stage was a significant risk factor for patients with ESCC (P<0.001). To study the independent factors affecting the prognosis among all the clinicopathological characteristics, Cox's proportional regression analysis was used (Table IV), which revealed that TIM-3 and galectin-9 expression were not independent factors affecting patient prognosis (TIM-3 expression hazard ratio, 1.102; 95% confidence interval, 0.292–4.157; P=0.886 and galectin-9 expression hazard ratio, 0.905; 95% confidence interval, 0.189–4.322; P=0.900).
Figure 3.
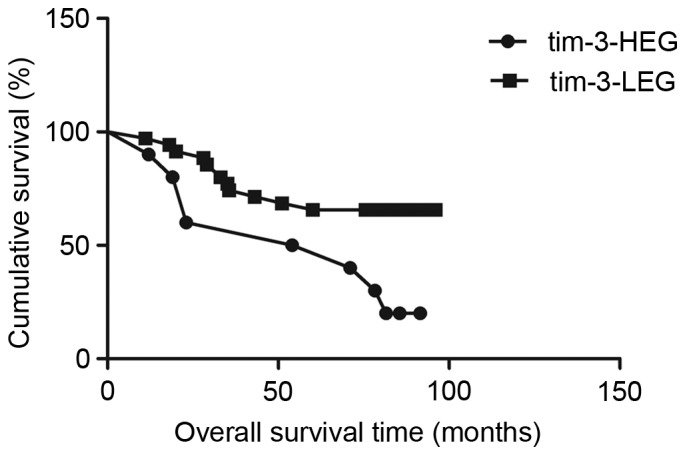
Disease-specific survival analysis for patients with esophageal squamous cell carcinoma depending on tumor TIM-3 expression. Patients in the TIM-3-HEG attained a significantly worse disease-specific survival outcome than the TIM-3-LEG (χ2=6.049, P=0.0139). TIM-3, T-cell immunoglobulin and mucin domain-containing protein-3; HEG, high expression group; LEG, low expression group.
Figure 4.
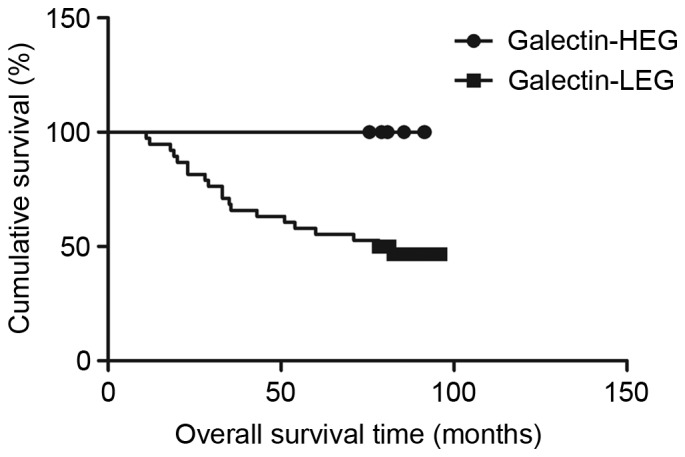
Disease-specific survival analysis for patients with esophageal squamous cell carcinoma depending on tumor galectin-9 expression. Patients in thegalectin-9-HEG attained a significantly better disease-specific survival outcome than the galectin-9-LEG (χ2=4.915, P=0.0266). HEG, high expression group; LEG, low expression group.
Table III.
Univariate analysis of the association of prognosis among clinicopatholocal parameters, TIM-3, galectin-9 in patients with esophageal squamous cell carcinoma.
| Parameters | Hazard ratio | 95% confidence interval | P-value |
|---|---|---|---|
| Sex (female vs. male) | 0.837 | 0.303–2.306 | 0.730 |
| Age (≤60 vs. >60 years) | 1.423 | 0.517–3.917 | 0.495 |
| Tumor size (≥5 vs. <5 cm) | 0.360 | 0.116–1.121 | 0.078 |
| Lymph node metastasis (yes vs. no) | 0.458 | 0.170–1.234 | 0.123 |
| Depth of invasion (TI/2 vs. T3) | 0.354 | 0.114–1.100 | 0.734 |
| TNM stage (II vs. III) | 0.179 | 0.066–0.485 | 0.001 |
| Tumor location(upper/lower vs. middle) | 0.048 | 0.000–23,863.841 | 0.649 |
| Pathological type (ulcerated vs. non-ulcerated) | 1.347 | 0.468–3.882 | 0.581 |
| Differentiation (poor vs. moderate/well) | 1.629 | 0.591–4.488 | 0.345 |
| Smoking history (yes vs. no) | 1.158 | 0.434–3.088 | 0.769 |
| Family history (yes vs. no) | 25.568 | 0.57–11453.023 | 0.298 |
| TIM-3 expression (HEG vs. LEG) | 2.517 | 0.913–6.937 | 0.074 |
| Galectin-9 expression (HEG vs. LEG) | 1.816 | 0.585–5.639 | 0.302 |
TIM-3, T-cell immunoglobulin and mucin-domain containing-3; HEG, high-expression group; LEG, low-expression group; TNM, Tumor-Node-Metastasis.
Table IV.
Multivariate analysis of the association of prognosis with clinicopathological parameters, and TIM-3 and galectin-9 expression, in patients with esophageal squamous cell carcinoma.
| Parameters | Hazard ratio | 95% confidence interval | P-value |
|---|---|---|---|
| Tumor size (≥5 vs. <5 cm) | 0.592 | 0.169–2.067 | 0.411 |
| TNM stage (II vs. III) | 0.148 | 0.022–1.007 | 0.051 |
| Lymph node metastasis (yes vs. no) | 1.625 | 0.257–10.284 | 0.051 |
| Depth of invasion (TI/2 vs. T3) | 0.803 | 0.201–3.206 | 0.756 |
| Pathological type (ulcerated vs. non-ulcerated) | 1.670 | 0.522–5.345 | 0.387 |
| Differentiation (poor vs. moderate/well) | 1.094 | 0.307–3.900 | 0.890 |
| TIM-3 expression (HEG vs. LEG) | 1.102 | 0.292–4.157 | 0.886 |
| Galectin-9 expression (HEG vs. LEG) | 0.905 | 0.189–4.322 | 0.900 |
TIM-3, T-cell immunoglobulin and mucin-domain containing-3; TNM, Tumor-Node-Metastasis; HEG, high-expression group; LEG, low-expression group.
Discussion
The results of the present study revealed that the expression levels of TIM-3 and galectin-9 ranged from low to high among different specimens of ESCC tumors. The disease-specific survival rate differed significantly between TIM-3-LEG and HEG, and similarly between galectin-9-LEG and HEG.
Although there no association was observed between TIM-3 or galectin-9 expression and clinicopathological parameters associated with the prognosis of patients with ESCC, including the TNM stage, lymph node metastasis, tumor size, depth of invasion, pathological type, differentiation and patient age, the disease-specific survival time differed significantly depending on the expression levels of TIM-3 and galectin-9. The results of the present study are in accord with previous similar studies in breast cancer and gastric cancer (24,32). A study by Cao et al (23) revealed that the migratory and invasive ability of HeLa cells was markedly reduced by the knockdown of TIM-3 expression, demonstrating that TIM-3 expression may be associated with tumor metastasis. TIM-3 has also been demonstrated to exert a direct role in promoting the occurrence and development of certain types of tumor, including cervical, gastric and colon cancer (23,24,33). The results of the present study were not consistent with the previous reports. A role for TIM-3 in ESCC was not explicitly identified, which may be associated with the small sample of TIM-3-HEG tumors.
All patients obtained further treatment following surgery, as per NCCN guidelines. Therefore, TIM-3 and galectin-9 could represent novel molecular markers to forecast the response of patients to ESCC treatments. In recent years, studies have aimed to identify potential ESCC risk factors and strategies to interfere with them, and at the time of writing, few markers have been identified that maybe used as predictors of ESCC patient prognosis, including interleukin 6 (34), early mitotic inhibitor-1 (35) and X-ray repair cross complementing 5 (36). However, the pathogenesis of ESCC cannot be adequately predicted using the current criteria for risk factors (37,38). It is therefore necessary to search for more accurate and specific indexes to evaluate the occurrence, development or prognosis of ESCC.
Previous studies have identified that TIM-3 and galectin-9 expression levels may be associated with patient prognosis in other types of human cancer (23,24,32,33), but the association between them and the prognosis of ESCC is not clear. Therefore, the purpose of the present study was to assess whether TIM-3 and galectin-9 were suitable as prognostic molecular markers for ESCC. In this experiment, it was concluded that TIM-3-HEG andgalectin-9-LEG were associated with shorter disease-specific survival times for Chinese patients with ESCC. TIM-3-HEG is a poor prognostic factor for ESCC, which is consistent with the review by Anderson (22).
To conclude, the present study identified that the expression levels of TIM-3 and galectin-9 varied in ESCC, and that the high expression of TIM-3 or the low expression of galectin-9 may indicate a poor prognosis for patients with ESCC. The data of the present study indicated that TIM-3 and galectin-9 may be suitable for development as novel biomarkers in ESCC.
Acknowledgements
The authors would like to thank Dr Quanli Gao (Department of Biological Immunotherapy, Henan Cancer Hospital, Zhengzhou, China), for his professional guidance.
References
- 1.Domper Arnal MJ, Ferrández Arenas Á, Lanas Arbeloa Á. Esophageal cancer: Risk factors, screening and endoscopic treatment in Western and Eastern countries. World J Gastroenterol. 2015;21:7933–7943. doi: 10.3748/wjg.v21.i26.7933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 3.Napier KJ, Scheerer M, Misra S. Esophageal cancer: A review of epidemiology, pathogenesis, staging workup and treatment modalities. World J Gastrointest Oncol. 2014;6:112–120. doi: 10.4251/wjgo.v6.i5.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pennathur A, Gibson MK, Jobe BA, Luketich JD. Oesophageal carcinoma. Lancet. 2013;381:400–412. doi: 10.1016/S0140-6736(12)60643-6. [DOI] [PubMed] [Google Scholar]
- 5.Chen W, Zheng R, Zhang S, Zhao P, Li G, Wu L, He J. The incidences and mortalities of major cancers in China, 2009. Chin J Cancer. 2013;32:106–112. doi: 10.5732/cjc.013.10027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xie J, Wang J, Cheng Sh, Zheng L, Ji F, Yang L, Zhang Y, Ji H. Expression of immune checkpoints in T cells of esophageal cancer patients. Oncotarget. 2016;27:63669–63678. doi: 10.18632/oncotarget.11611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12:252–264. doi: 10.1038/nrc3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qiu H, Zheng L, Tang W, Yin P, Cheng F, Wang L. Programmed death-1 (PD-1) polymorphisms in Chinese patients with esophageal cancer. Clin Biochem. 2014;47:612–617. doi: 10.1016/j.clinbiochem.2013.12.023. [DOI] [PubMed] [Google Scholar]
- 9.Monney L, Sabatos CA, Gaglia JL, Ryu A, Waldner H, Chernova T, Manning S, Greenfield EA, Coyle AJ, Sobel RA, et al. Th1-specific cell surface protein Tim-3 regulates macrophage activation and severity of an autoimmune disease. Nature. 2002;415:536–541. doi: 10.1038/415536a. [DOI] [PubMed] [Google Scholar]
- 10.Cao E, Zang X, Ramagopal UA, Mukhopadhaya A, Fedorov A, Fedorov E, Zencheck WD, Lary JW, Cole JL, Deng H, et al. T cell immunoglobulin mucin-3 crystal structure reveals a galectin-9-independent ligand-binding surface. Immunity. 2007;26:311–321. doi: 10.1016/j.immuni.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 11.Santiago C, Ballesteros A, Martínez-Muñoz L, Mellado M, Kaplan GG, Freeman GJ, Casasnovas JM. Structures of T cell immunoglobulin mucin protein 4 show a metal-Ion-dependent ligand binding site where phosphatidylserine binds. Immunity. 2007;27:941–951. doi: 10.1016/j.immuni.2007.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Santiago C, Ballesteros A, Tami C, Martínez-Muñoz L, Kaplan GG, Casasnovas JM. Structures of T Cell immunoglobulin mucin receptors 1 and 2 reveal mechanisms for regulation of immune responses by the TIM receptor family. Immunity. 2007;26:299–310. doi: 10.1016/j.immuni.2007.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu B, Yuan L, Gao Q, Yuan P, Zhao P, Yuan H, Fan H, Li T, Qin P, Han L, et al. Circulating and tumor-infiltrating Tim-3 in patients with colorectal cancer. Oncotarget. 2015;6:20592–20603. doi: 10.18632/oncotarget.4112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freeman GJ, Casasnovas JM, Umetsu DT, DeKruyff RH. TIM genes: A family of cell surface phosphatidylserine receptors that regulate innate and adaptive immunity. Immunol Rev. 2010;235:172–189. doi: 10.1111/j.0105-2896.2010.00903.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nicodemus CF. Antibody-based immunotherapy of solid cancers: Progress and possibilities. Immunotherapy. 2015;7:923–939. doi: 10.2217/imt.15.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou Q, Munger ME, Veenstra RG, Weigel BJ, Hirashima M, Munn DH, Murphy WJ, Azuma M, Anderson AC, Kuchroo VK, Blazar BR. Coexpression of Tim-3 and PD-1 identifies a CD8+ T-cell exhaustion phenotype in mice with disseminated acute myelogenous leukemia. Blood. 2011;117:4501–4510. doi: 10.1182/blood-2010-10-310425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fourcade J, Sun Z, Benallaoua M, Guillaume P, Luescher IF, Sander C, Kirkwood JM, Kuchroo V, Zarour HM. Upregulation of Tim-3 and PD-1 expression is associated with tumor antigen-specific CD8+ T cell dysfunction in melanoma patients. J Exp Med. 2010;207:2175–2186. doi: 10.1084/jem.20100637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sakuishi K, Ngiow SF, Sullivan JM, Teng MW, Kuchroo VK, Smyth MJ, Anderson AC. TIM3+FOXP3+ regulatory T cells are tissue-specific promoters of T-cell dysfunction in cancer. Oncoimmunology. 2013;2:e23849. doi: 10.4161/onci.23849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sakuishi K, Apetoh L, Sullivan JM, Blazar BR, Kuchroo VK, Anderson AC. Targeting Tim-3 and PD-1 pathways to reverse T cell exhaustion and restore anti-tumor immunity. J Exp Med. 2010;207:2187–2194. doi: 10.1084/jem.20100643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tarhini A. Immune-mediated adverse events associated with ipilimumab ctla-4 blockade therapy: The underlying mechanisms and clinical management. Scientifica (Cairo) 2013;2013:857519. doi: 10.1155/2013/857519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hamid O, Robert C, Daud A, Hodi FS, Hwu WJ, Kefford R, Wolchok JD, Hersey P, Joseph RW, Weber JS, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369:134–144. doi: 10.1056/NEJMoa1305133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anderson AC. Tim-3: An emerging target in the cancer immunotherapy landscape. Cancer Immunol Res. 2014;2:393–398. doi: 10.1158/2326-6066.CIR-14-0039. [DOI] [PubMed] [Google Scholar]
- 23.Cao Y, Zhou X, Huang X, Li Q, Gao L, Jiang L, Huang M, Zhou J. Tim-3 expression in cervical cancer promotes tumor metastasis. PLoS One. 2013;8:e53834. doi: 10.1371/journal.pone.0053834. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 24.Jiang J, Jin MS, Kong F, Cao D, Ma HX, Jia Z, Wang YP, Suo J, Cao X. Decreased galectin-9 and increased Tim-3 expression are related to poor prognosis in gastric cancer. PLoS One. 2013;8:e81799. doi: 10.1371/journal.pone.0081799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferris RL, Lu B, Kane LP. Too much of a good thing? Tim-3 and TCR signaling in T cell exhaustion. J Immunol. 2014;193:1525–1530. doi: 10.4049/jimmunol.1400557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhu C, Anderson AC, Schubart A, Xiong H, Imitola J, Khoury SJ, Zheng XX, Strom TB, Kuchroo VK. The Tim-3 ligand galectin-9 negatively regulates T helper type 1 immunity. Nat Immunol. 2005;6:1245–1252. doi: 10.1038/ni1271. [DOI] [PubMed] [Google Scholar]
- 27.Su EW, Bi S, Kane LP. Galectin-9 regulates T helper cell function independently of Tim-3. Glycobiology. 2011;21:1258–1265. doi: 10.1093/glycob/cwq214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leitner J, Rieger A, Pickl WF, Zlabinger G, Grabmeier-Pfistershammer K, Steinberger P. TIM-3 does not act as a receptor for galectin-9. PLoS Pathog. 2013;9:e1003253. doi: 10.1371/journal.ppat.1003253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sakuishi K, Jayaraman P, Behar SM, Anderson AC, Kuchroo VK. Emerging Tim-3 functions in antimicrobial and tumor immunity. Trends Immunol. 2011;32:345–349. doi: 10.1016/j.it.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National Comprehensive Cancer Network: (NCCN) Clinical Practice Guidelines in Oncology. Esophageal Cancer. 2009. https://www.nccn.org/professionals/physician_gls/f_guidelines.asp. https://www.nccn.org/professionals/physician_gls/f_guidelines.asp Version 1. [DOI] [PubMed]
- 31.Sobin LH, Gospodarowicz MK, Wittekind C. TNM Classification of Malignant Tumours. 7th edition. Wiley-Blackwell; Hoboken, NJ: 2009. International Union Against Cancer (eds): Title section/chapter; p. 455. [Google Scholar]
- 32.Irie A, Yamauchi A, Kontani K, Kihara M, Liu D, Shirato Y, Seki M, Nishi N, Nakamura T, Yokomise H, Hirashima M. Galectin-9 as a prognostic factor with antimetastatic potential in breast cancer. Clin Cancer Res. 2005;11:2962–2968. doi: 10.1158/1078-0432.CCR-04-0861. [DOI] [PubMed] [Google Scholar]
- 33.Zhou E, Huang Q, Wang J, Fang C, Yang L, Zhu M, Chen J, Chen L, Dong M. Up-regulation of Tim-3 is associated with poor prognosis of patients with colon cancer. Int J Clin Exp Pathol. 2015;8:8018–8027. [PMC free article] [PubMed] [Google Scholar]
- 34.Zhao ZF, Li JX, Ye R, Wu X, Gao LL, Niu BL. Interleukin-6 as a potential molecular target in esophageal squamous cell carcinoma. Oncol Lett. 2016;11:925–932. doi: 10.3892/ol.2015.3990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guan C, Zhang J, Zhang J, Shi H, Ni R. Enhanced expression of early mitotic inhibitor-1 predicts a poor prognosis in esophageal squamous cell carcinoma patients. Oncol Lett. 2016;12:114–120. doi: 10.3892/ol.2016.4611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang S, Wang Z, Yang YU, Shi MO, Sun Z. Overexpression of Ku80 correlates with aggressive clinicopathological features and adverse prognosis in esophageal squamous cell carcinoma. Oncol Lett. 2015;10:2705–2712. doi: 10.3892/ol.2015.3635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feng Z, Xiang-Lei L, Hai-Tao W, Zuo-Pei W, Bao-Li H, Hai-Feng Z, Xiao-Long W, Li L. Programmed cell death 1 expression in esophageal squamous cell carcinoma and association with clinical characteristics. Indian J Cancer. 2015;52(Suppl 3):E176–E178. doi: 10.4103/0019-509X.186574. [DOI] [PubMed] [Google Scholar]
- 38.Jackie Oh S, Han S, Lee W, Lockhart AC. Emerging immunotherapy for the treatment of esophageal cancer. Expert Opin Investig Drugs. 2016;25:667–677. doi: 10.1517/13543784.2016.1163336. [DOI] [PubMed] [Google Scholar]