Abstract
An 88-year-old woman with a prior history of aortic stenosis and history of valvuloplasty presented with worsening symptoms of heart failure and dizziness. She underwent successful transcatheter aortic valve replacement (TAVR) without complications. Follow-up echocardiograms revealed a small fistula connecting aorta to the right ventricle. The patient was initially asymptomatic but 3 months later developed overload of the right ventricle and heart failure and chose to continue medical therapy. She died of progressive heart failure at 9 months from onset of fistula. Aorto-right ventricular fistula is a rare complication of TAVR with only four cases reported in literature thus far.
Key words: Aorto-right ventricular fistula, heart failure, transcatheter aortic valve replacement, transcatheter aortic valve replacement complications
INTRODUCTION
Transcatheter aortic valve replacement (TAVR) is a safe and effective procedure for severe aortic stenosis in patients who are at a high risk for surgical aortic valve replacement. Common complications related to TAVR reported in literature includes moderate-to-severe aortic insufficiency, paravalvular leak, left ventricular perforation, aortic root rupture, coronary artery impingement, valve embolization, complete heart block, ventricular fibrillation/ventricular tachycardia, renal failure, and stroke.[1] The development of an aorto-right ventricular (RV) fistula is an extremely rare complication.
CASE PRESENTATION
An 88-year-old woman, with a medical history significant for coronary artery disease, hypertension, hyperlipidemia, and known severe aortic stenosis, presented to the Structural Heart Clinic with worsening fatigue and dizziness without syncope. She had exertional dyspnea with the New York Heart Association (NYHA) Class III-IV congestive heart failure symptoms and no angina. Transthoracic echocardiogram (TTE) showed severe aortic stenosis with mean gradient of 62 mmHg and an ejection fraction (EF) of 20%. Cardiac catheterization revealed patent coronary angiogram and an aortic valve area of 0.27 cm 2.
She was deemed to be high risk for open heart surgery (Society of Thoracic Surgeons score 26.782%). Due to the lifestyle-limiting symptoms and severe aortic stenosis, a balloon aortic valvuloplasty was initially performed with significant improvement in symptoms (NYHA II). Computed tomography and angiography showed mildly dilated aortic arch with significant atherosclerosis but no aneurysm of the aortic root or sinus of Valsalva.
Six months later, due to the recurrence of symptoms, she underwent successful TAVR with 26 mm SAPIEN XT bioprosthetic valve (Edwards Lifesciences, Irvine, CA, USA) using standard technique without postdeployment dilation. Proper anatomic position, trivial paravalvular leak, and normal valve function were confirmed with transesophageal echocardiogram and completion aortogram. The patient required immediate surgical repair of the utilized iliac artery. Immediately postprocedure, the patient remained largely asymptomatic with stable cardiac function (EF 55%–60%) on echocardiogram.
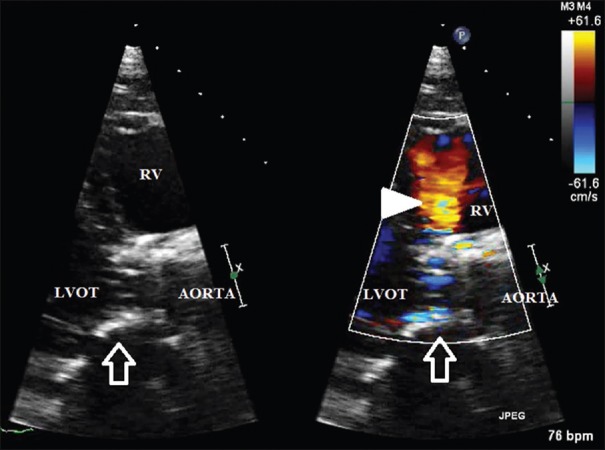
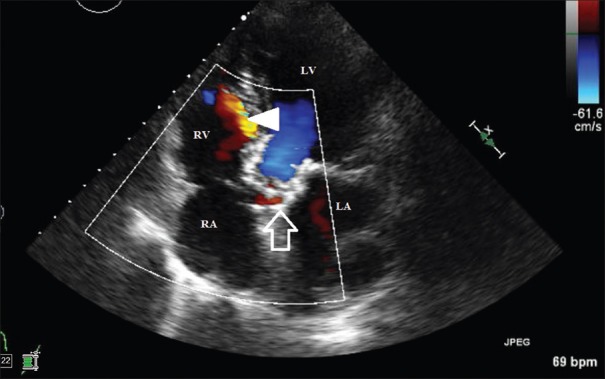
The patient had an uneventful recovery and was discharged to home on the 3rd postoperative day. TTE at 4 days and again 2 weeks after the procedure showed good positioning and functioning of the bioprosthetic valve. A new small fistula connecting the right sinus of Valsalva to the RV [Figures 1, 2 and Videos 1, 2] was noted.
Figure 1.
Transthoracic echocardiographic parasternal long-axis (zoomed) view of the Edwards SAPIEN XT bioprosthetic aortic valve (arrow) with aorto-RV fistula (arrowhead) (with and without color Doppler). RV: Right ventricle, LVOT: Left ventricle outflow tract
Figure 2.
Transthoracic echocardiogram Apical 5 chamber view showing bioprosthetic aortic valve (arrow) with aorto-RV fistula (arrowhead). RA: Right atrium, RV: Right ventricle, LA: Left atrium, LV: Left ventricle
A decision was made to closely monitor the fistula and intervene if patient were to develop symptoms.
She was hospitalized 3 months later with worsening of heart failure symptoms. Electrocardiogram and troponins were normal. Repeat echocardiogram showed enlargement of the fistula with a velocity of >4 m/s, a Qp:Qs of 2:1, an EF reduction from 55%–60% to 30%–35%, and moderate dilation of RV. In view of the extreme risks to undergo repeat cardiac surgical procedure, including percutaneous and open closure options, the patient decided to continue with medical management for heart failure. After another admission with similar symptoms few months later, she was discharged to a skilled nursing facility with hospice care and died due to progressive heart failure. Total duration between onset of fistula and death was 9 months.
DISCUSSION
Ruptured sinus of Valsalva aneurysm (congenital or traumatic), endocarditis, and complications related to cardiothoracic surgical procedures such as repair of ventricular septal defect, Ross procedure, or modified Ravitch procedure for pectus excavatum have been associated with aorto-ventricular fistula.[2,3,4,5,6] There are also reports of this complication with surgical aortic valve replacement. The most commonly reported cases of aorto-RV fistulas are secondary to rupture of congenital aneurysm of one of the sinuses of Valsalva.
Our literature search revealed only four reported cases of aorto-RV fistulas after TAVR, of which two patients became symptomatic due to fistula within months after the procedure.[7,8,9,10] The severity of the shunt determines the symptomatology. Small shunts are usually asymptomatic and can be managed conservatively. The symptoms are similar to the right heart failure due to pressure and volume overload of RV. Most patients complain of dyspnea on exertion, pedal edema, ascites, and fatigue.
The exact mechanism of fistula formation is unknown but thought to be related to trauma from displacement of heavily calcified tissue, usage of larger prosthesis, and depth of prosthesis implantation.[7] In our patient, displacement of the heavily calcified aortic valve might be the etiology for the fistula even though the valve was appropriately sized. An additional report details fistula formation after repeat dilation of a 29 mm Medtronic CoreValve to address significant paravalvular regurgitation.[9] It is recommended to treat symptomatic sinus of Valsalva to RV fistulas, particularly in young patients, due to the high risk of worsening heart failure secondary to RV overload owing to high-pressure difference between aorta and RV. Asymptomatic patients with high surgical risk can be monitored with close follow-up and serial TTE looking for RV dimensions and right side pressures.
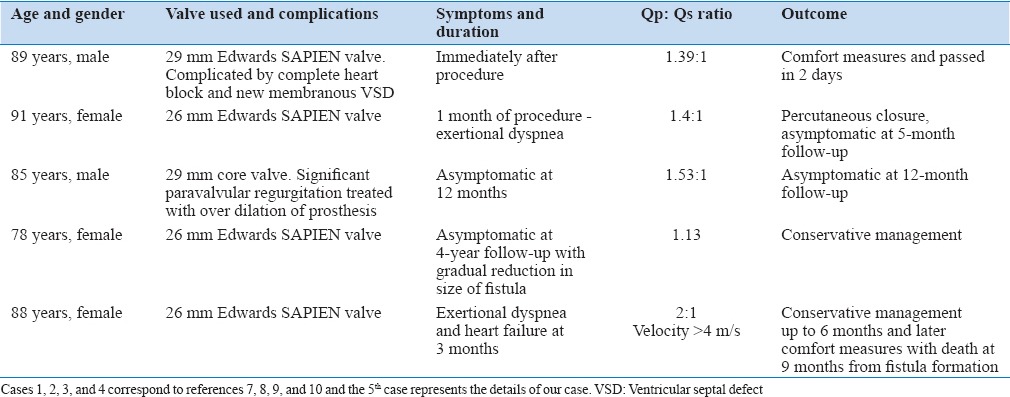
Surgical repair is the treatment of choice; however, transcatheter closures have also been reported in the literature.[2,9,11] In patients with worsening symptoms and who are high-risk surgical candidates, percutaneous closure of the defect can be considered. Among the four reported cases, only one patient was successfully treated with percutaneous closure with coil (IMWC-5-PDA5 coil MReye Flipper Detachable Embolization Coil Delivery System, Cook, Inc., Bloomington, Indiana). A summary of all five cases, including ours, is provided in the table [Table 1].
Table 1.
Comparative features of five cases
CONCLUSION
Post TAVR aorto-right ventricular fistula is a rare complication of TAVR. We need to suspect this complication. The successful management of rare complications associated with innovative procedures, such as transcatheter valve replacement, is often driven by patient symptoms and the limited experiences from previously reported cases. Symptoms and severity of the flow determine the treatment options.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on: www.heartviews.org
REFERENCES
- 1.Lugomirski P, McArdle B, Alak A, Dick A, Labinaz M. Late presentation of left main coronary artery impingement post-transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2015;8:e159–60. doi: 10.1016/j.jcin.2015.03.033. [DOI] [PubMed] [Google Scholar]
- 2.Gao L, Wu Q, Xu X, Zhao T, Yang Y. Minimally invasive transthoracic device closure of an acquired sinus of valsalva-right ventricle fistula in a pediatric patient. Iran J Pediatr. 2014;24:327–30. [PMC free article] [PubMed] [Google Scholar]
- 3.Capín E, López J, De La Hera JM, Corros C, Campos AG, Rodríguez ML, et al. Sinus of Valsalva fistula to right chambers: An infrequent pathology. Hellenic J Cardiol. 2014;55:258–9. [PubMed] [Google Scholar]
- 4.Kawahira T, Iwahashi K, Okada M. Aortocavitary fistula without aneurysm and transient incomplete atrioventricular block due to infective endocarditis. Gen Thorac Cardiovasc Surg. 2010;58:45–8. doi: 10.1007/s11748-009-0473-6. [DOI] [PubMed] [Google Scholar]
- 5.Williams-Phillips S. Post Ross procedure aortic right sinus of Valsalva fistula to right ventricle. West Indian Med J. 2011;60:669–73. [PubMed] [Google Scholar]
- 6.Weiss AJ, Pawale A, Hollinger IB, Stelzer P, Chikwe J. Repair of an aortic sinus right ventricular fistula and aortic leaflet disruption after a stab wound. Ann Thorac Surg. 2012;94:1354. doi: 10.1016/j.athoracsur.2012.03.012. [DOI] [PubMed] [Google Scholar]
- 7.Shakoor MT, Islam AM, Ayub S. Acquired aorto-right ventricular fistula following transcatheter aortic valve replacement. Case Rep Cardiol. 2015;2015:608539. doi: 10.1155/2015/608539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pilgrim T, Meier B, Wenaweser P. Aorto-right ventricular fistula after transfemoral aortic valve implantation. J Invasive Cardiol. 2010;22:E30–1. [PubMed] [Google Scholar]
- 9.Muñoz-García AJ, Rodríguez-Bailón I, Briales JH, Navarro MJ, García JM, de Teresa-Galván E. Aorto-right ventricular fistula after percutaneous aortic valve implantation of a CoreValve prosthesis. Tex Heart Inst J. 2011;38:728–9. [PMC free article] [PubMed] [Google Scholar]
- 10.Leu HB, Chang HH, Wu MH, Chen YH. Four-year follow-up of acquired aorto-right ventricular fistula after transcatheter aortic valve implantation. Eur Heart J. 2016;37:2679. doi: 10.1093/eurheartj/ehv716. [DOI] [PubMed] [Google Scholar]
- 11.Srivastava A, Radha AS. Transcatheter closure of ruptured sinus of valsalva aneurysm into the left ventricle: A retrograde approach. Pediatr Cardiol. 2012;33:347–50. doi: 10.1007/s00246-011-0127-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.