Abstract
Controlling patient temperature is important for a wide variety of clinical conditions. Cooling to normal or below normal body temperature is often performed for neuroprotection after ischemic insult (e.g. hemorrhagic stroke, subarachnoid hemorrhage, cardiac arrest, or other hypoxic injury). Cooling from febrile states treats fever and reduces the negative effects of hyperthermia on injured neurons. Patients are warmed in the operating room to prevent inadvertent perioperative hypothermia, which is known to cause increased blood loss, wound infections, and myocardial injury, while also prolonging recovery time. There are many reported approaches for temperature management, including improvised methods that repurpose standard supplies (e.g., ice, chilled saline, fans, blankets) but more sophisticated technologies designed for temperature management are typically more successful in delivering an optimized protocol. Over the last decade, advanced technologies have developed around two heat transfer methods: surface devices (water blankets, forced-air warmers) or intravascular devices (sterile catheters requiring vascular placement). Recently, a novel device became available that is placed in the esophagus, analogous to a standard orogastric tube, that provides efficient heat transfer through the patient's core. The device connects to existing heat exchange units to allow automatic patient temperature management via a servo mechanism, using patient temperature from standard temperature sensors (rectal, Foley, or other core temperature sensors) as the input variable. This approach eliminates vascular placement complications (deep venous thrombosis, central line associated bloodstream infection), reduces obstruction to patient access, and causes less shivering when compared to surface approaches. Published data have also shown a high degree of accuracy and maintenance of target temperature using the esophageal approach to temperature management. Therefore, the purpose of this method is to provide a low-risk alternative method for controlling patient temperature in critical care settings.
Keywords: Medicine, Issue 129, Targeted temperature management, hypothermia, normothermia, fever, neurogenic fever, cardiac arrest, burn injury
Introduction
There is significant need for patient temperature management when treating a wide range of conditions, including cardiac arrest, refractory or recurrent fever, neurogenic fever, and major surgery. In the United States, a half-million cardiac arrests annually originate either in the hospital (for example, in patients who are undergoing care for general medical or surgical conditions)1 or out of the hospital (for example, at home or in public venues, who are then brought to the emergency department)2. In both scenarios, patient outcomes are significantly improved when active temperature management is administered3 and targeted temperature management (TTM) has been a standard of care for cardiac arrest since 2005. Over 5 million patients are admitted to intensive care units annually in the U.S4 . Of these, fever develops in up to 45% of non-neurologically injured patients5 and up to 70% of neurologically injured patients6. Fever control in the intensive care unit is associated with improved outcomes and reduced risk of death, because elevated temperature increases metabolic demands, worsens cerebral ischemia, and increases neuronal loss7. At least 10 million surgeries performed annually in the U.S. require active patient warming to prevent inadvertent perioperative hypothermia8. In the operating room, patients undergoing surgery should maintain a body temperature above 36 °C to avoid a large number of adverse effects. Unplanned decreases in body temperature before, during, or after surgery increase blood loss, infections, and hospital length of stay, which adds $7,000 or more per patient to hospitalization costs9,10,11,12.
Despite great clinical need, the most widely administered temperature management protocols demonstrate inadequate performance or introduce significant risk to the patient. Surface devices (such as water blankets, conduction mattresses, and forced-air covers) are cumbersome, have limited heat transfer capacity, and must be removed to allow access to the patient for patient care and procedures. Intravascular devices are invasive, difficult to place, and predispose patients to infections and blood clots. Existing approaches to prevent inadvertent perioperative hypothermia fail to maintain normothermia up to 70% of the time12,13,14,15,16 and a retrospective analysis of post-cardiac arrest cooling found that overall, 30% of patients failed to reach target temperature within 6 h17.
The esophageal approach to patient temperature management offers substantial advantages to existing technologies18. The esophageal temperature management device maintains the functionality of the gastric tube typically placed in the critical care and surgical patient populations. It allows continuous gastric suction and decompression of gas and liquids while adding the ability to control a patient's temperature safely and efficiently by leveraging the favorable heat exchange environment of the esophagus (Figure 1). Temperature modulation is achieved by connecting the esophageal temperature management device to any of several external heat exchangers (also called chillers) that use water as the coolant. Several vendors produce compatible heat exchangers that are available in hospitals for powering existing temperature control products (most often water blankets). Nurses, nurse practitioners, or physicians typically place an esophageal temperature management device, but it can also be inserted by any provider trained to place a standard orogastric tube. The esophageal temperature management device does not restrict access to the patient, need not be sterile, avoids the risk of needle stick injuries among providers, and avoids the risks of skin complications, bloodstream infections, and blood clots in the patient. Therefore, the purpose of this method is to provide a low-risk alternative method for controlling patient temperature in critical care and operating room settings.
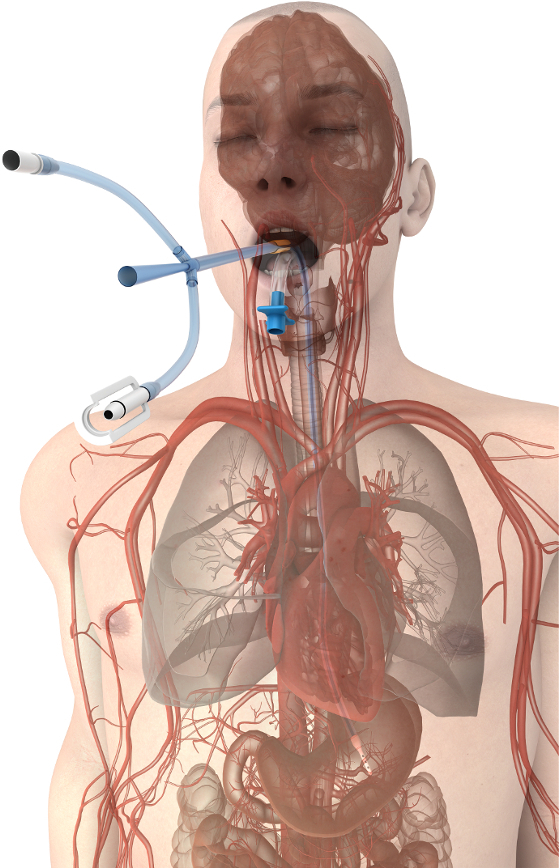
Figure 1. Esophageal temperature management device placement. Device proximity to the great vessels and heart promote efficient heat transfer at the patient's core. Please click here to view a larger version of this figure.
Protocol
This protocol follows the guidelines of our institution's human research ethics committee.
1. Assessment Guidelines Prior to Placement
NOTE: Although there are no formal contraindications listed in the U.S. labelling, it is recommended that the esophageal temperature management device be used with caution in patients with known esophageal deformity, evidence of esophageal trauma, and in patients known to have ingested acidic or caustic poisons within the prior 24 hours.
Obtain all equipment, including appropriate heat exchange unit, the esophageal temperature management device, an appropriate securement device, water-based lubrication packets, and a circumferential bite block.
Place Foley thermistor and/or rectal temperature probe and connect one to the heat exchange unit. A second temperature source is recommended for verification, and may be connected to the patient monitor.
Connect the esophageal temperature management device to the appropriate heat exchanger, power on the unit, set the patient target temperature according to hospital protocol, and place the heat exchanger in automatic mode. Ensure that water is flowing through the esophageal temperature management device and confirm that no leaks are present.
2. Device Insertion
Measure the appropriate insertion depth for the esophageal temperature management device by extending it from the patient's lips to the earlobe and then from the earlobe to the tip of the xiphoid process; mark the insertion depth on the device (Figure 2).
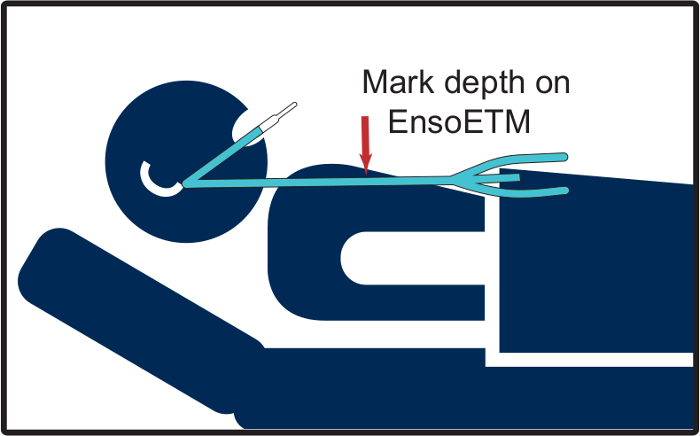
Figure 2. Measuring an esophageal temperature management device for placement. This schematic illustrates the appropriate procedure for determining device placement depth, as described in step 2.1. Please click here to view a larger version of this figure.
Lubricate the esophageal temperature management device generously (approximately 15 cm of the distal end) with water-soluble lubricant (Figure 3).
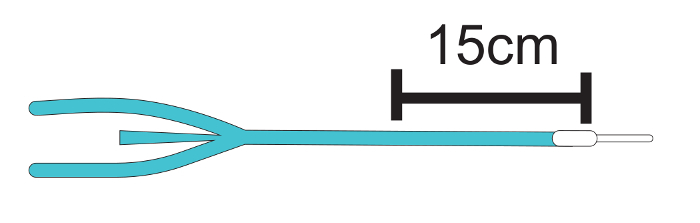
Figure 3. Lubricating the esophageal temperature management device. This schematic illustrates the appropriate procedure for applying water soluble lubrication to the device prior to insertion, as described in step 2.2. Please click here to view a larger version of this figure.
Place the patient as flat as tolerated and insert the esophageal temperature management device using gentle pressure posteriorly and downwards through the mouth, past the oropharynx, and into the esophagus. A gentle jaw thrust may be required to assist passage of the device. If clinically feasible, the addition of slight neck extension, induced with support under the shoulders if needed, may further ease passage of the device. Advance the device with light pressure until the required length of tube has been inserted. Secure the bite block in place (Figure 4).
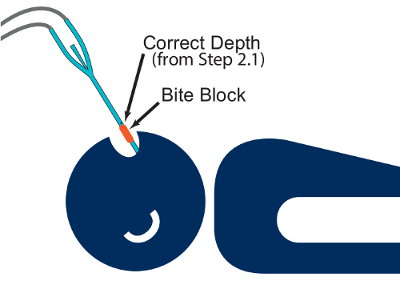
Figure 4. Inserting the esophageal temperature management device. This schematic illustrates the appropriate patient positioning for inserting the device, as described in step 2.3. Please click here to view a larger version of this figure.
- Confirm placement of the esophageal temperature management device in accordance with hospital protocol.
- Inject air with a syringe through the central lumen while auscultating over the stomach for a "swoosh" or a "burp" indicating gastric placement.
- Aspirate gastric contents with a syringe through the central lumen.
- Confirm the location and placement with an x-ray.
Secure with a securement device or tape in accordance with hospital protocol. Ensure the tube and tube set connections are not in contact with the patient's skin, as direct contact between the tube and exposed skin may cause shivering.
For stomach decompression, connect the central lumen to low-intermittent suction using standard suction tubing.
3. Temperature management – cooling
Ensure heat exchanger is set to automatic mode and the appropriate goal temperature (typically from 32 °C to 37 °C, depending on institutional protocol) is set.
Initiate shivering prophylaxis with medications as per unit protocol (prophylactic intervention is recommended with non-sedating medications to start; for example, acetaminophen, buspirone, magnesium, and skin counterwarming).
Evaluate for shivering using the Bedside Shivering Assessment Scale at regular intervals, or anytime temperature reduction is not proceeding as expected. Shivering occurs in a caudal progression and will first be identified at the mandible or pectoralis muscles; early intervention is imperative. Additional treatment for shivering may include meperidine, dexmedetomidine, fentanyl, propofol, or neuromuscular blockade.
4. Temperature management – maintenance
Monitor and record water temperature hourly; if the water temperature drops below 10 °C for 1 h (or more than once when patient is at target temperature), first assess for shivering.
Periodically reposition the esophageal temperature management device in accordance with hospital protocol.
5. Temperature management – warming
Follow local hospital guideline for rewarming rate if rewarming from intentional hypothermia.
Set a maximum rewarming rate if rewarming from accidental hypothermia, or preventing perioperative hypothermia.
6. Troubleshooting
NOTE: A kink or pinch in the system may cause an occlusion alert on the external heat exchanger. If the cause cannot be found, stop treatment and remove the esophageal temperature management device.
Utilize standard approaches for clearing blocked gastric tubes if the central lumen of the esophageal temperature management device becomes clogged or blocked; if unsuccessful, replace the device.
If there is a discrepancy greater than 0.5 °C between temperature sources, pause therapy to investigate the issue.
As leak in the system may cause an increase in accumulated liquid in the suction canister, if a larger than expected volume of water accumulates in the suction canister, stop treatment and remove the esophageal temperature management device to examine for leaks. NOTE: Factors which may affect warming or cooling include body mass, environmental conditions, shivering, and clinical condition; patients greater than 120 kg may exhibit slower responses to intended temperature changes, and smaller patients may take longer to warm.
- If the patient is not cooling or warming as expected:
- Ensure the esophageal temperature management device is at the correct depth.
- Ensure adequate water flow and that the device is cold or warm to touch (as appropriate).
- Ensure the external heat exchanger is set appropriately in automatic mode with desired target temperature and appropriate water temperature (4 °C to 42 °C).
- Confirm the temperature probe is intact and accurate; check with secondary source.
- Check the patient for heat generation (shivering or fever generation for example), heat loss (hemodynamic instability or medication administration) and ensure the environmental temperature is consistent with temperature modulation goal.
7. Device removal
Press "Monitor" to stop the external heat exchanger, close the clamps if present, and withdraw the device.
Disconnect the device from the tube set connections and dispose as per institutional policy.
Turn off the heat exchange unit.
Representative Results
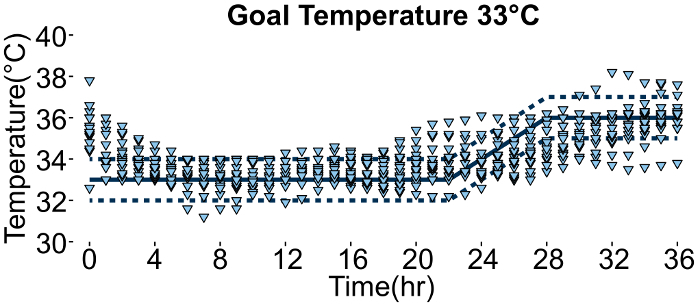
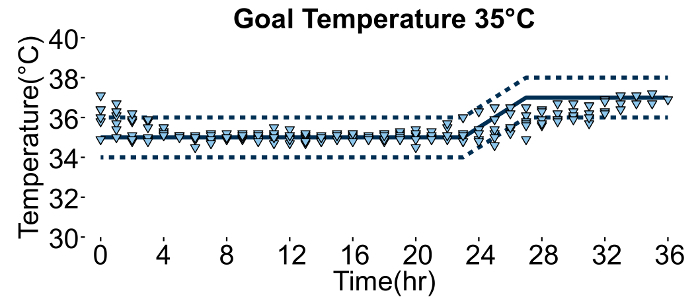
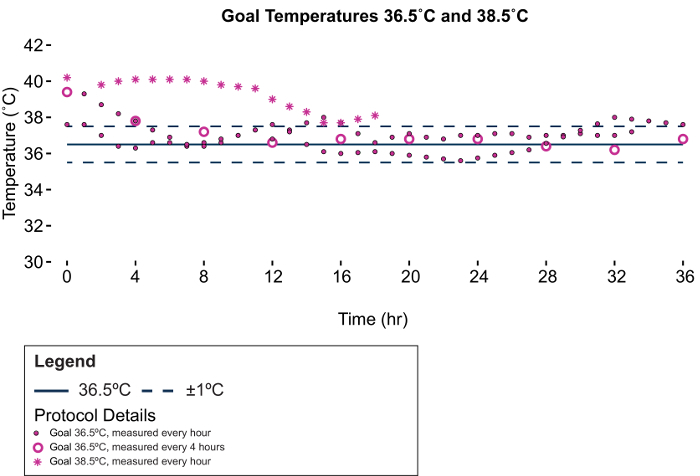
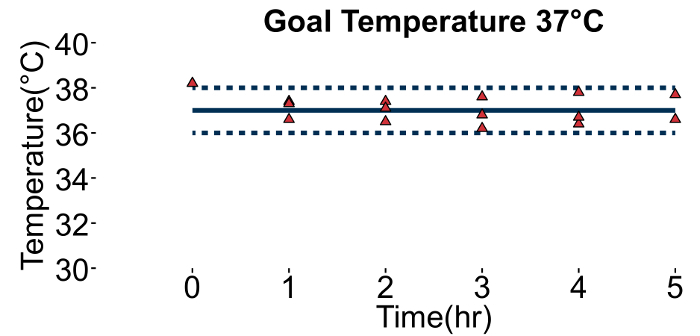
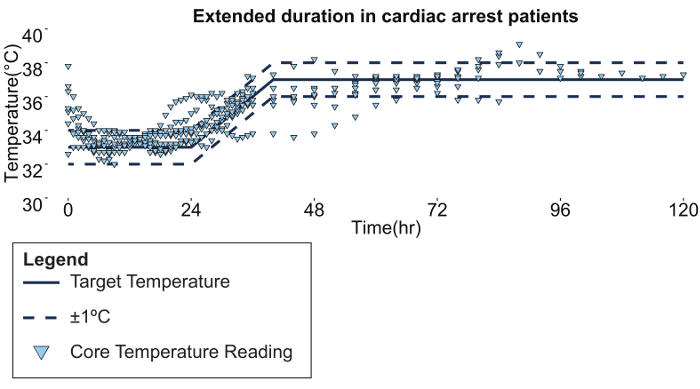
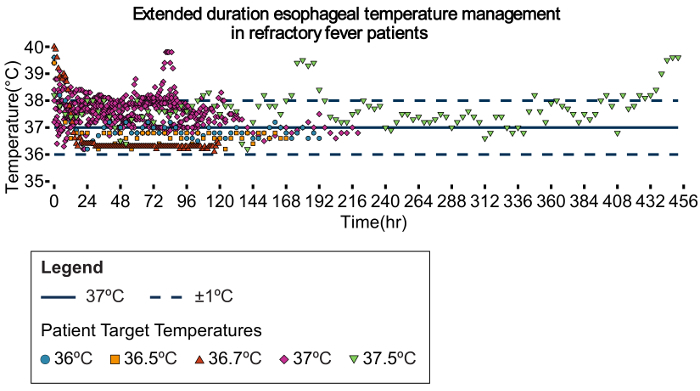
Aggregate Data In terms of cooling, maintenance, and warming rates, esophageal temperature management performs similarly to other advanced temperature management technologies. An analysis of 30 patients treated for up to 36 hours with esophageal temperature management found that the average time to temperature was 2.7 h (SD ±2.8 h) and that 96% of temperature readings recorded during the maintenance period were within ±1 °C19. Performance was consistent across all protocols, regardless of target temperature (Figure 5, Figure 6, Figure 7, Figure 8). Performance remained consistent with treatment durations longer than 72 h (Figure 9 and Figure 10).
Notable Cases Numerous case studies describe the application of esophageal temperature management in practice, including for the treatment of post cardiac arrest ischemia-reperfusion injury, central fever reduction, and maintenance of operative normothermia20,21,22,23,24,25,26,27. Though the esophageal temperature management method was initially conceived in the context of cardiac arrest treatment, the following cases highlight its successful translation into other critical care and perioperative domains.
Case 1: Meningitis A 36 year-old woman with a weight of 64 kg was admitted with severe Streptococcus pyrogenes meningitis. Her body temperature increased from 38.2 °C on admission to 40.0 °C six hours later; IV acetaminophen and external cooling blankets proved unsuccessful to adequately decrease temperature.
The esophageal temperature management was initiated at 48 h and the patient's temperature dropped from 39.4 °C to 37.8 °C in 4 hours. The patient's temperature continued to drop towards 36.6 °C during the next 12 hours and was maintained between 36 °C and 37 °C for 5 days. Gastroscopy on day 7 revealed no changes attributable to the esophageal temperature management device.
Case 2: Severe Burn and Pyrexia Reversal A 49 year-old male weighing 86 kg was admitted with 49% circumferential burns that included full thickness burns to both legs, left arm, and left torso. Two days after admission, the patient was brought to the operating room for surgical procedures that included staged excision and grafting of the leg wounds. Upon placing the esophageal temperature management device and initiating temperature management, the patient's core temperature was maintained at normothermia while allowing the operating suite temperature to be decreased successfully to 24 °C. Subsequently, on day 22 of the patient's hospitalization, the patient developed a fever due to E. coli and Candida septicemia resistant to conventional cooling methods. Esophageal temperature management was again initiated, reducing the patient's temperature from 40 °C to the set point of 38.5 °C, and this temperature was maintained despite restricting the minimum allowable water temperature to 12 °C.
Figure 5. Temperature curve for 33 °C protocol. 17 post-cardiac arrest patients were cooled to 33 °C for 24 h and then rewarmed over a 4 h period to 37 °C. Normothermia was then maintained for another 8 h. Each data point represents a single temperature measurement from a single patient. Please click here to view a larger version of this figure.
Figure 6. Temperature curve for 35 °C protocol. 6 post-cardiac arrest patients were cooled to 35 °C for 24 h and then rewarmed over a 4 h period to 37 °C. Normothermia was then maintained for another 8 h. Each data point represents a single temperature measurement from a single patient. Please click here to view a larger version of this figure.
Figure 7. Temperature curve for refractory fever patients. 4 refractory fever patients were cooled to either 36.5 °C or 38 °C. See inset legend for details. Please click here to view a larger version of this figure.
Figure 8. Temperature curve for perioperative normothermia. 3 severe burn patients (40 - 50% body surface area) were warmed during surgery to prevent inadvertent hypothermia. All patients maintained core temperatures above 36 °C and the ambient temperature in the OR was maintained at 27 °C. Please click here to view a larger version of this figure.
Figure 9. Extended duration esophageal temperature management in cardiac arrest patients. 18 patients were cooled to 33 °C for 24 h and then rewarmed over an 8 h period to 36 °C. Normothermia was then maintained for up to 122 h. Please click here to view a larger version of this figure.
Figure 10. Extended duration esophageal temperature management in refractory fever patients. 18 patients were cooled for up to 454 h according to hospital protocol, including a target temperature of 37.5 °C (green triangles), 37 °C (purple diamonds), 36.7 °C (red triangles), 36.5 °C (orange squares), or 36 °C (blue circles). Please click here to view a larger version of this figure.
Discussion
Modification and troubleshooting required for this protocol is generally limited to that featured above, and involves the typical monitoring of patient care employed in critical care settings. Modulating core temperature is critical to patient outcomes in a growing range of clinical scenarios. These include the intentional induction of hypothermia from normothermia, rewarming from inadvertent or intentional hypothermia, and actively maintaining normal body temperature (i.e., normothermia) during conditions in which inadvertent hypothermia are common, such as in the operating room. As specific clinical examples, patients who suffer ischemia-reperfusion injury, such as occurs during cardiac arrest, benefit from cooling (generally to temperatures below normal body temperature) followed by gentle rewarming and fever prevention for up to 3 days after resuscitation28,29,30. Neonates suffering from hypoxic ischemic encephalopathy obtain improved outcomes if cooled below normal body temperature31. The cooling of kidney donors after neurologic death, prior to organ transplant, has been shown to reduce the rate of delayed graft function32. Controlling fevers in septic shock patients may reduce vasopressor requirements and contribute to reducing early mortality33. Maintaining normothermia in patients undergoing surgical procedures reduces surgical wound infections, myocardial complications, blood loss, and transfusion requirements, while shortening length of stay and reducing the likelihood of death10,11,16.
Limitations of the technique include challenges encountered in managing critical care patients. While targeted temperature management promotes good outcomes, the most common temperature modulation techniques introduce risks to patients and logistical challenges to providers (including difficulties in placement, bloodstream infections, blood clots, skin damage, and cost). Esophageal temperature management is designed to overcome these shortcomings34,35,36. When appropriately managed, the esophageal temperature management device does not come into contact with the vasculature (as do the intravascular temperature modulation devices) or skin (as do the surface temperature modulation devices), thereby avoiding blood clots, bloodstream infection, and skin degradation. The device can be placed quickly by a variety of healthcare providers, typically in a matter of minutes21,37. The insertion technique mimics standard orogastric tube placement, which minimizes workflow disruptions that might delay therapy initiation. Using a core approach also appears to pose significantly less shivering burden than surface approaches27,38,39,40 . This has the advantage of reducing sedative and anti-shivering medication costs, which then shortens the patient length of stay via quicker awakening from the lower degree of sedation required. These features, considered in concert with the clinical performance described above, support esophageal temperature management as a viable option for providers in the emergency department, intensive care unit, and operating room. A growing set of data published on the device likewise supports this new approach21,22,23,24,27,41.
Critical steps within the protocol include initiating flow within the device prior to insertion, providing adequate lubrication to the device in order to assure easy placement, performing gastric suctioning and decompression to allow maximum contact between device and patient, and addressing any patient shivering that may develop. Following this protocol will provide optimum results and allow a high degree of performance and safety in the care of this important patient population.
Disclosures
The authors Melissa Naiman, Maria Gray, and Erik Kulstad are employees of Attune Medical that produces the esophageal temperature management device described in this manuscript. The authors Ahmed Hegazy, Joseph Haymore, Neeraj Badjatia, and Andrej Markota received complimentary devices to conduct clinical evaluations.
Acknowledgments
None.
References
- Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358(1):9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- Callans DJ. Out-of-Hospital Cardiac Arrest -- The Solution Is Shocking. N Engl J Med. 2004;351(7):632–634. doi: 10.1056/NEJMp048174. [DOI] [PubMed] [Google Scholar]
- Kochanek PM, Jackson TC. The Brain and Hypothermia-From Aristotle to Targeted Temperature Management. Crit Care Med. 2017;45(2):305–310. doi: 10.1097/CCM.0000000000002182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Society of Critical Care Medicine. Critical Care Statistics in the United States. 2006. Available from: http://www.sccm.org/Communications/Pages/CriticalCareStats.aspx.
- Laupland KB, et al. Occurrence and outcome of fever in critically ill adults. Crit Care Med. 2008;36(5):1531–1535. doi: 10.1097/CCM.0b013e318170efd3. [DOI] [PubMed] [Google Scholar]
- Diringer MN, Reaven NL, Funk SE, Uman GC. Elevated body temperature independently contributes to increased length of stay in neurologic intensive care unit patients. Critical Care Medicine. 2004;32(7):1489–1495. doi: 10.1097/01.ccm.0000129484.61912.84. [DOI] [PubMed] [Google Scholar]
- Laupland KB. Fever in the critically ill medical patient. Critical care medicine. 2009;37(Suppl 7):S273–S278. doi: 10.1097/CCM.0b013e3181aa6117. [DOI] [PubMed] [Google Scholar]
- Mathias JM. Hospitals to report on normothermia. OR manager. 2009;25(9):22–24. [PubMed] [Google Scholar]
- Auerbach AD. Making Health Care Safer: A Critical Analysis of Patient Safety Practices - Ch. 20 Prevention of Surgical Site Infections. 2001. Available from: http://www.ahrq.gov/clinic/ptsafety/chap20a.htm.
- Rajagopalan S, Mascha E, Na J, Sessler DI. The effects of mild perioperative hypothermia on blood loss and transfusion requirement. Anesthesiology. 2008;108(1):71–77. doi: 10.1097/01.anes.0000296719.73450.52. [DOI] [PubMed] [Google Scholar]
- Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334(19):1209–1215. doi: 10.1056/NEJM199605093341901. [DOI] [PubMed] [Google Scholar]
- Sessler DI. New surgical thermal management guidelines. Lancet. 2009;374(9695):1049–1050. doi: 10.1016/S0140-6736(09)61686-X. [DOI] [PubMed] [Google Scholar]
- Young VL, Watson ME. Prevention of perioperative hypothermia in plastic surgery. Aesthet Surg J. 2006;26(5):551–571. doi: 10.1016/j.asj.2006.08.009. [DOI] [PubMed] [Google Scholar]
- Hedrick TL, et al. Efficacy of protocol implementation on incidence of wound infection in colorectal operations. J Am Coll Surg. 2007;205(3):432–438. doi: 10.1016/j.jamcollsurg.2007.04.042. [DOI] [PubMed] [Google Scholar]
- Forbes SS, et al. Implementation of evidence-based practices for surgical site infection prophylaxis: results of a pre- and postintervention study. J Am Coll Surg. 2008;207(3):336–341. doi: 10.1016/j.jamcollsurg.2008.03.014. [DOI] [PubMed] [Google Scholar]
- Sun Z, et al. Intraoperative core temperature patterns, transfusion requirement, and hospital duration in patients warmed with forced air. Anesthesiology. 2015;122(2):276–285. doi: 10.1097/ALN.0000000000000551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leary M, et al. The association of body mass index with time to target temperature and outcomes following post-arrest targeted temperature management. Resuscitation. 2014;85(2):244–247. doi: 10.1016/j.resuscitation.2013.10.027. [DOI] [PubMed] [Google Scholar]
- Naiman M, Shanley P, Garrett F, Kulstad E. Evaluation of advanced cooling therapy's esophageal cooling device for core temperature control. Expert Rev Med Devices. 2016;13(5):423–433. doi: 10.1080/17434440.2016.1174573. [DOI] [PubMed] [Google Scholar]
- Naiman M, Markota A, Hegazy AF, Dingley J, Kulstad E. Temperature Management in Critical Care and Burn Patients using an Esophageal Heat Transfer Device. Military Medicine. 2017. In Press. [DOI] [PMC free article] [PubMed]
- Hegazy AF, Lapierre DM, Butler R, Martin J, Althenayan E. The esophageal cooling device: A new temperature control tool in the intensivist's arsenal. Heart Lung. 2017. [DOI] [PubMed]
- Hegazy AF, Lapierre DM, Butler R, Althenayan E. Temperature control in critically ill patients with a novel esophageal cooling device: a case series. BMC Anesthesiol. 2015;15:152. doi: 10.1186/s12871-015-0133-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukovnik N, Markota A, Velnar T, Rebol J, Sinkovic A. Therapeutic hypothermia and inhalation anesthesia in a patient with severe pneumococcal meningitis and secondary cardiac arrest. Am J Emerg Med. 2017;35(4):665.e665–665.e666. doi: 10.1016/j.ajem.2016.11.006. [DOI] [PubMed] [Google Scholar]
- Markota A, Fluher J, Kit B, Balazic P, Sinkovic A. The introduction of an esophageal heat transfer device into a therapeutic hypothermia protocol: A prospective evaluation. Am J Emerg Med. 2016;34(4):741–745. doi: 10.1016/j.ajem.2016.01.028. [DOI] [PubMed] [Google Scholar]
- Markota A, Kit B, Fluher J, Sinkovic A. Use of an oesophageal heat transfer device in therapeutic hypothermia. Resuscitation. 2015;89:e1–e2. doi: 10.1016/j.resuscitation.2015.01.032. [DOI] [PubMed] [Google Scholar]
- Schroeder DC, et al. Oesophageal heat exchangers with a diameter of 11mm or 14.7mm are equally effective and safe for targeted temperature management. PLoS One. 2017;12(3):e0173229. doi: 10.1371/journal.pone.0173229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D, et al. Use of an Esophageal Heat Exchanger to Maintain Core Temperature during Burn Excisions and to Attenuate Pyrexia on the Burns Intensive Care Unit. Case Reports in Anesthesiology. 2016;2016:6. doi: 10.1155/2016/7306341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan I, et al. 14th Annual Neurocritical Care Society Meeting. National Harbor, MD: 2016. [Google Scholar]
- HACA. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346(8):549–556. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- Bernard SA, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346(8):557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- Callaway CW, et al. Part 8: Post-Cardiac Arrest Care: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S465–S482. doi: 10.1161/CIR.0000000000000262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyckoff MH, et al. Part 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S543–S560. doi: 10.1161/CIR.0000000000000267. [DOI] [PubMed] [Google Scholar]
- Niemann CU, et al. Therapeutic Hypothermia in Deceased Organ Donors and Kidney-Graft Function. N Engl J Med. 2015;373(5):405–414. doi: 10.1056/NEJMoa1501969. [DOI] [PubMed] [Google Scholar]
- Schortgen F, et al. Fever control using external cooling in septic shock: a randomized controlled trial. Am J Respir Crit Care Med. 2012;185(10):1088–1095. doi: 10.1164/rccm.201110-1820OC. [DOI] [PubMed] [Google Scholar]
- Reccius A, Mercado P, Vargas P, Canals C, Montes J. Inferior Vena Cava Thrombosis Related to Hypothermia Catheter: Report of 20 Consecutive Cases. Neurocrit Care. 2015;23(1):72–77. doi: 10.1007/s12028-014-0069-6. [DOI] [PubMed] [Google Scholar]
- Maze R, et al. Endovascular cooling catheter related thrombosis in patients undergoing therapeutic hypothermia for out of hospital cardiac arrest. Resuscitation. 2014;85(10):1354–1358. doi: 10.1016/j.resuscitation.2014.05.029. [DOI] [PubMed] [Google Scholar]
- Simosa HF, Petersen DJ, Agarwal SK, Burke PA, Hirsch EF. Increased risk of deep venous thrombosis with endovascular cooling in patients with traumatic head injury. Am Surg. 2007;73(5):461–464. [PubMed] [Google Scholar]
- Kulstad E, et al. Induction, maintenance, and reversal of therapeutic hypothermia with an esophageal heat transfer device. Resuscitation. 2013;84(11):1619–1624. doi: 10.1016/j.resuscitation.2013.06.019. [DOI] [PubMed] [Google Scholar]
- van Zanten AR, Polderman KH. Blowing hot and cold? Skin counter warming to prevent shivering during therapeutic cooling. Crit Care Med. 2009;37(6):2106–2108. doi: 10.1097/CCM.0b013e3181a5e4d8. [DOI] [PubMed] [Google Scholar]
- Tommasi E, et al. Cooling techniques in mild hypothermia after cardiac arrest. J Cardiovasc Med. 2014. [DOI] [PubMed]
- Diringer MN. Treatment of fever in the neurologic intensive care unit with a catheter-based heat exchange system. Crit Care Med. 2004;32(2):559–564. doi: 10.1097/01.CCM.0000108868.97433.3F. [DOI] [PubMed] [Google Scholar]
- Hegazy AF, Lapierre DM, Butler R, Martin J, Althenayan E. The esophageal cooling device: A new temperature control tool in the intensivist's arsenal. Heart Lung. 2017;46(3):143–148. doi: 10.1016/j.hrtlng.2017.03.001. [DOI] [PubMed] [Google Scholar]


