Abstract
The Wisconsin Registry for Alzheimer's Prevention is a longitudinal observational cohort study enriched with persons with a parental history (PH) of probable Alzheimer's disease (AD) dementia. Since late 2001, Wisconsin Registry for Alzheimer's Prevention has enrolled 1561 people at a mean baseline age of 54 years. Participants return for a second visit 4 years after baseline, and subsequent visits occur every 2 years. Eighty-one percent (1270) of participants remain active in the study at a current mean age of 64 and 9 years of follow-up. Serially assessed cognition, self-reported medical and lifestyle histories (e.g., diet, physical and cognitive activity, sleep, and mood), laboratory tests, genetics, and linked studies comprising molecular imaging, structural imaging, and cerebrospinal fluid data have yielded many important findings. In this cohort, PH of probable AD is associated with 46% apolipoprotein E (APOE) ε4 positivity, more than twice the rate of 22% among persons without PH. Subclinical or worse cognitive decline relative to internal normative data has been observed in 17.6% of the cohort. Twenty-eight percent exhibit amyloid and/or tau positivity. Biomarker elevations, but not APOE or PH status, are associated with cognitive decline. Salutary health and lifestyle factors are associated with better cognition and brain structure and lower AD pathophysiologic burden. Of paramount importance is establishing the amyloid and tau AD endophenotypes to which cognitive outcomes can be linked. Such data will provide new knowledge on the early temporal course of AD pathophysiology and inform the design of secondary prevention clinical trials.
Keywords: Preclinical Alzheimer's disease, Biomarkers, Risk factors
1. Introduction
Although it is widely recognized that Alzheimer's disease (AD) has an extended preclinical stage, the cognitive and neuropathobiological course of changes in late-middle-aged people who may later develop AD dementia are relatively unknown [1]. Such knowledge is crucial if AD is to be identified in its inchoate form, its pathogenesis illuminated, and the tempo and predictors of its progression characterized as a predicate to successful prevention trials.
The Wisconsin Registry for Alzheimer's Prevention (WRAP), established in 2001 [2], is a longitudinal observational cohort of participants who enrolled at midlife (mean age 54), and that is enriched with risk for late-onset AD due to parental history (PH) of AD dementia. The cohort also serves as a registry for linked studies. The overarching goals of the study shown in Table 1 are to identify early cognitive decline and to characterize midlife factors associated with such decline and the contributing underlying biomarkers of AD and related pathology. The present contribution updates the initial description of the cohort, study design, and protocol [2] and provides new data on the effects of family history, apolipoprotein E (APOE) genotype, and AD biomarkers on longitudinal cognitive decline over time. Key study findings are summarized, and future directions are presented.
Table 1.
The major goals of the WRAP study
|
Abbreviations: WRAP, Wisconsin Registry for Alzheimer's Prevention; AD, Alzheimer's disease.
2. Methods
2.1. Study design
To the present, 1561 participants have enrolled over a continuing enrollment window. Recruitment sources included memory clinics in which a parent was diagnosed or treated, limited radio and newspaper advertisements, and word of mouth. Participants generally meet the following inclusion criteria at study entry: age 40–65 years; fluent English speaker; visual and auditory acuity adequate for neuropsychological testing; good health with no diseases expected to interfere with study participation over time. Participants are excluded from enrollment if they have a prior diagnosis of dementia or evidence of dementia at baseline testing (one was excluded due to baseline dementia). The baseline mean age is 54 years, 73% have a parent with AD dementia, and 40% of the total sample are APOE ε4 carriers (46% of the PH+ participants and 22% of the PH− participants).
2.2. Determination of PH of AD
The characteristic of PH of AD (PH+) is defined as having at least one biological parent diagnosed with dementia due to probable AD based on the NINDS-ADRDA criteria [3]. Three general methods were used to determine PH. First, direct diagnosis of the parent from study physicians or affiliated faculty, or where medical records for the affected parent were available, a panel of study investigators reviewed the parent's clinical evaluation for dementia to determine whether evidence was sufficient to diagnose probable AD. Second was the neuropathological confirmation of AD in the affected parent. Third, in the absence of sufficient prior information, a Dementia Questionnaire (DQ; [4]) was conducted with the adult child regarding the parent's dementia history and course. The DQ asks about the type of dementia symptoms, the course of progression, and the presence or absence of comorbid conditions that could explain or contribute to the symptoms. Diagnostic classifications based on the DQ show very high sensitivity (100%) and specificity (90%) compared to clinical diagnosis [5]. Eight percent of PH subjects were initially qualified for study entry by a parental autopsy; 83% by medical record review or expert physician diagnosis; and 9% by DQ. Two participants (<1%) were qualified based on self report of PH of AD (but without full DQ or medical record review).
2.3. A comparison group without PH of AD
To understand the role of PH, recruitment of additional participants without PH of probable AD dementia began in 2004. This group now consists of 421 persons who by self-report did not have a parent with dementia due to AD or related cause and who in general have a mother who survived to at least age 75 years and a father to at least age 70 years without dementia.
Because parental status changes over time, it is reassessed at each visit and updated as necessary (e.g., in the case that a previously nondemented parent later developed dementia or, rarely, a parent whose dementia was presumed due to AD was later found by autopsy to be another pathology).
2.4. Study visit procedures
Participants are followed at regular intervals with detailed in-person assessments, questionnaires, and blood collection occurring at each study visit. The first follow-up is approximately 4 years after baseline, and further follow-up visits are approximately every 2 years. Persons will remain in the study until age 85 years, unless they withdraw, convert to dementia, or develop another illness precluding participation or accurate assessment of cognition. Each visit requires approximately 5 hours and comprises the assessments shown in Table 2, that is, cognitive measurement, anthropometric measures, laboratory tests, and questionnaire ratings completed by the participant and an informant including the Quick Dementia Rating System or Clinical Dementia Rating [33]. Reliability and consistency of cognitive testing is established through regular review of aspects of testing procedures at team meetings, biannual individual observations of test administration, through adherence to a standardized manual of procedures, and through blinded rescoring by a separate rater (20% annually for each psychometrist).
Table 2.
List of procedures and tests in the current protocol
|
Abbreviations: BMI, body mass index; CSF, cerebrospinal fluid; MRI, magnetic resonance imaging; PET, positron emission tomography; MEGAEX, Expanded Multi-Ethnic Genotyping Array; AD, Alzheimer's disease.
2.5. Consent for brain donation
Neuropathologic confirmation is critical for linking cognitive trajectories to disease-related end points. Accordingly, participants are encouraged to enroll in the Wisconsin Brain Donation Program which is administered by the Neuropathology Core of the Wisconsin Alzheimer's Disease Research Center (ADRC). Brain bank enrollment has not been an entry criterion. However, since 2015, brain donation has been systematically discussed with participants at each visit, and educational material on the value of brain donation is regularly offered at WRAP's statewide series of information sessions and in semiannual newsletters.
2.6. Identifying subtle, preclinical impairment
A critical issue for the field is development and validation of optimal methodology for identifying early cognitive decline and impairment [34]. Simple single-test thresholds are insufficient [35], and available published norms used to define “impaired” and “normal” performances on neuropsychological tests in persons age ∼55+ years may be confounded by unintended inclusion of individuals with incipient disease in the normative samples of those tests [36], [37], [38], thereby reducing sensitivity to subtle dysfunction [37]. Moreover, thresholds and norms may have been validated by others in populations of uncertain relevance to the cohort under investigation. To avoid these potential confounders and to enhance sensitivity to preclinical decline, we developed a “robust” norms approach in which internal normative distributions for cognitive factor scores [39] and individual test scores [40] are generated, where “robust” indicates that the normative group is nondeclining over time. In Koscik et al. [39], deficits on multiple visits via algorithmic criteria were required as evidence of “psychometric mild cognitive impairment (MCI),” whereas in Clark et al. [40], deficits on multiple tests within a specific domain were required to identify persons with psychometric MCI. In practice, and to ensure that these approaches are not falsely overidentifying people with abnormal cognition, we incorporate these algorithms into our consensus review process as described in Section 2.7.
2.7. Classification of cognitive status
If cognitive abnormalities are detected by algorithm on neuropsychological tests, data from participant visits are brought to a consensus review committee consisting of dementia-specialist physicians, neuropsychologists, and nurse practitioners for in-depth review. Thresholds for committee review include performance greater than 1.5 SD below robust internal norms adjusting for age, gender, and literacy level [39], [40], self-report or informant report of cognitive or functional decline on the Clinical Dementia Rating, the Quick Dementia Rating Scale, the Informant Questionnaire on Cognitive Decline in the Elderly, or Instrumental Activities of Daily Living; or threshold-specific absolute scores on key tests (e.g., Wechsler Memory Scale–Revised Logical Memory-II ≤17; Rey Auditory Verbal Learning Test Delayed Recall ≤5; or Mini–Mental State Examination ≤26). The consensus committee assesses cognitive performance at all prior visits to detect intraindividual changes over time and analyzes pertinent findings from the neurological and physical examinations; medical and social histories; and self-survey and informant survey of mood, cognition, and functional status. The diagnosis of “MCI” is based on National Institute on Aging–Alzheimer's Association criteria [34] and requires (1) patient or informant concern regarding change in cognition; (2) unambiguous impairment in one or more cognitive domains; (3) not meeting criteria for dementia. The experimental category of “early MCI” is assigned if there is lower-than-expected objective performance (typically >1.5 SD below internal robust norms), but few or no subjective cognitive complaints or clinically significant deficits (for further discussion, see [41]). This category broadly corresponds to clinical stage 2 in the 2018 diagnostic framework [42].
2.8. Biomarker and genetics procedures
A diversity of magnetic resonance imaging (MRI), molecular positron emission tomography (PET), and cerebrospinal fluid (CSF) biomarkers has been acquired from subsets of participants as funding permits (see Supplementary Table 1 for sample sizes of each to date). Serial MRIs and CSF samples will be obtained from approximately 60% of WRAP participants over the next 5 years, and serial amyloid and tau imaging will be obtained from approximately 30% with current and projected funding.
2.9. MRI protocol
In 2009, a standardized MRI protocol was implemented across the Wisconsin ADRC to include all WRAP-linked studies. The standard protocol comprises an inversion recovery–prepared T1-weighted 3D volume structural scan, a T2-FLAIR 3D volume to assess white-matter hyperintensities, pseudo-continuous arterial spin labeling of cerebral blood flow, multishell diffusion-weighted imaging to assess white-matter integrity and structural connectivity, and 4D-flow imaging to assess intracranial blood flow and vessel stiffness.
2.10. CSF collection and analyses
CSF samples are collected in the core WRAP study and in linked studies. A center-wide standard preanalytic protocol is used to collect approximately 22 mL of CSF that is subsequently gently mixed to remove collection gradients, partitioned into 0.5-mL aliquots in 1.0-mL polypropylene tubes, and stored at −80°C. Assayed analytes include total tau, hyperphosphorylated tau181, amyloid β 1–42 (Aβ42), amyloid β 1–40 , YKL40, neurofilament light-chain protein, and neurogranin (see, for example, [43], [44], [45], [46], [47], [48], [49], [50]).
2.11. Molecular amyloid and tau imaging
Amyloid imaging is conducted with [C-11] Pittsburgh Compound-B (PiB) PET using a dynamic 70-minute protocol. For a full description of the PiB protocol, refer to the study by Johnson et al. [51]. All participants who undergo amyloid imaging are invited to undergo tau PET imaging with [F-18]MK6240 from ∼70- to 110-minute postinjection. Derived maps of AD pathology burden are analyzed for longitudinal change.
2.12. Genetics
APOE ε2/ε3/ε4, 20 common genetic variants from the International Genomics of Alzheimer's Project consortium [52], and low frequency variants in TREM2 [53], [54] and PLD3 [55] were genotyped using competitive allele-specific polymerase chain reaction-based genotyping assays (LGC Genomics, Beverly, MA). Duplicate quality control samples had 99.9% concordance. Cross-validation of APOE genotypes with prior assays was 99.7% concordant. Various polygenic risk scores (PRSs) are derived in which the contribution of each single nucleotide polymorphism to the score is weighted by its risk odds ratio [56].
More recently, genome-wide genotyping was performed using the Illumina Infinium Expanded Multi-Ethnic Genotyping Array (MEGAEX) containing approximately 1.7 million genetic markers.
3. Review of select study findings and new results
3.1. Accrual
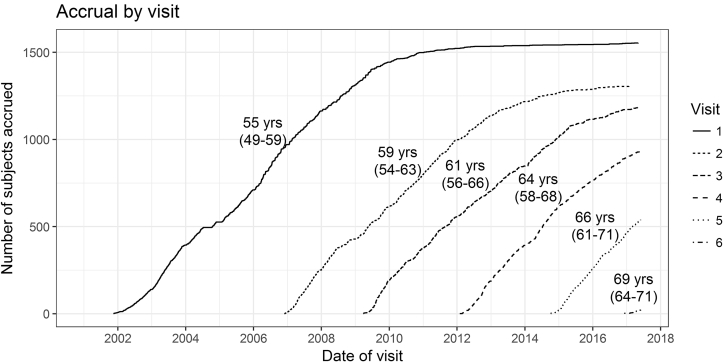
Fig. 1 depicts participant accrual from November 2001 through May 2017. Accrual is shown by visit number together with mean age at each visit. The rolling recruitment window means that individual participants have a different number of follow-up visits to date depending on how long they have been in the study. Sixth visits began in late 2016. Over 5600 study visits have occurred since inception, and over 3000 visits are projected over the next 5 years. Retention is 81% over the 16-year study period.
Fig. 1.
Accrual by study visit. Lines representing each visit are annotated with the median participant age (interquartile range) at that visit.
3.2. Descriptive information
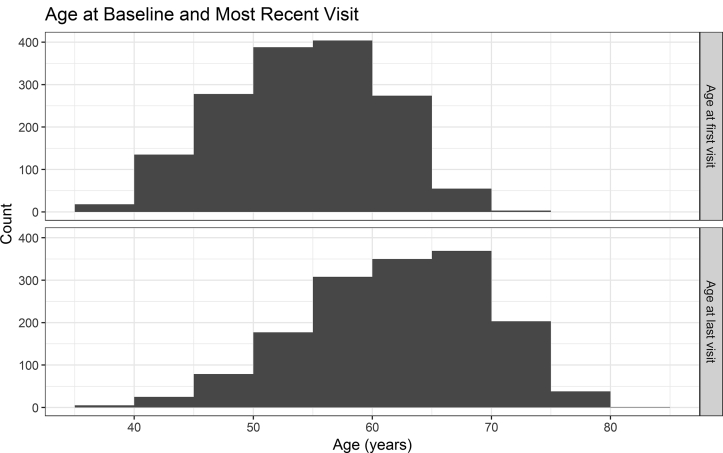
Baseline characteristics of the WRAP sample, including demographics, medical history, and cognition, are described in Table 3. In keeping with the original study design, Table 3 is stratified by parental family history and APOE ε4 carrier status. Histograms showing the sample ages at baseline and at last visit are provided in Fig. 2.
Table 3.
Baseline demographic and health characteristics grouped by parental history and APOE ε4 status
| Variable | PH+/ε4+ | PH+/ε4− | PH−/ε4+ | PH−/ε4− | P value |
|---|---|---|---|---|---|
| N | 515 | 597 | 91 | 330 | |
| Age | 53 (6.4) | 54 (6.7) | 57 (5.7) | 56 (6.1) | <.001 |
| Sex (female) | 72.2% | 71.9% | 72.5% | 64.8% | .095 |
| Literacy (WRAT)† | 105 (66–120) | 107 (45–119) | 107 (68–119) | 109 (58–120) | <.001 |
| High school degree | 99.4% | 99.2% | 100% | 99.7% | .827 |
| Bachelors college degree | 54.4% | 55.6% | 63.7% | 66.4% | .002 |
| BMI∗ | 29 (7) | 29 (6.3) | 28 (5.8) | 28 (5.7) | .131 |
| Hypertension | 18.1% | 20.3% | 22% | 21.2% | .608 |
| Hypercholesterolemia | 37.1% | 30.2% | 33% | 31.8% | .102 |
| Diabetes | 4.08% | 5.36% | 5.49% | 5.45% | .743 |
| Race (white) | 88.2% | 88.1% | 90.1% | 90.9% | .563 |
| AVLT total trials 1–5∗ | 50 (8.1) | 51 (8.4) | 50 (7.6) | 51 (8.2) | .549 |
| AVLT delay∗ | 10 (2.8) | 10 (3) | 10 (2.7) | 10 (2.9) | .87 |
| Trails A time(s)∗ | 27 (9) | 27 (8.8) | 27 (8.4) | 28 (9.3) | .358 |
| Trails B time(s)∗ | 65 (31) | 65 (33) | 64 (25) | 66 (30) | .909 |
| COWAT∗ | 42 (11) | 43 (11) | 43 (11) | 43 (12) | .216 |
| Digit span (forward raw score)∗ | 10 (2.2) | 10 (2.2) | 10 (2.2) | 10 (2.2) | .671 |
| Digit span (backward raw score)∗ | 6.9 (2.3) | 7 (2.2) | 7 (2.2) | 7 (2.2) | .884 |
Abbreviations: PH, parental history; BMI, body mass index; WRAT, Wide Range Achievement Test-III Reading Recognition subtest; AVLT, Rey Auditory Verbal Learning Test; COWAT, Controlled Oral Word Association Test.
NOTE. Except where otherwise indicated, reported values are percentages, and comparisons were performed using a Fisher's exact test.
Mean (SD); P-values obtained via ANOVA.
Median (range); P-values obtained via a nonparametric (Kruskal-Wallis) test.
Fig. 2.
Histograms displaying the WRAP sample age distribution at baseline (upper panel) and most recent visit (lower panel). In the data for the lower panel, 15.9% of the sample have completed only one visit, so the reported numbers reflect age at visit 1; for 7.78%, age at visit 2; 16.4% for visit 3; 25.2% for visit 4; 33.2% for visit 5; and 1.41% for visit 6, respectively. Abbreviation: WRAP, Wisconsin Registry for Alzheimer's Prevention.
3.3. Results and discussion related to goal 1
Goal 1: Determine whether AD dementia–related cognitive trajectories can be detected in midlife and distinguished from normal aging using sensitive cognitive assessments.
3.3.1. Previously published findings
As noted in Section 2, we developed and evaluated two cross-sectional algorithms for identifying performance that is below robust internal norms using factor scores [39], [57] and using individual test scores [40]. Compared to the use of published norms in the same cohort, both psychometric approaches demonstrate improved sensitivity to small but consequential decrements of cognitive function. With the factor score approach [39], we observed greater longitudinal cognitive decline among the 13% of the cohort who were classified as psychometric MCI compared to those who were cognitively normal. Using this approach, we also showed that psychometric MCI is associated with greater dysfunction in connected language [58] and verbal fluency [59]. Using the cognitive test approach [40], the false-positive rate was reduced by requiring a pattern of lower-than-expected performance on multiple tests within or across domains to be affected in order for the participant to be designated as having MCI (similar to [60], [61]). With use of this “multitest, single-visit” approach, 18% of participants were classified as having psychometric MCI. These algorithmic approaches may serve in their own right as intermediate outcomes and are used to inform research visit-by-visit diagnoses made by the diagnostic consensus committee. In analyses of consensus committee–classified cognitive status, higher intraindividual cognitive variability at baseline predicted impaired cognitive status 8–10 years later [41].
3.3.2. New results
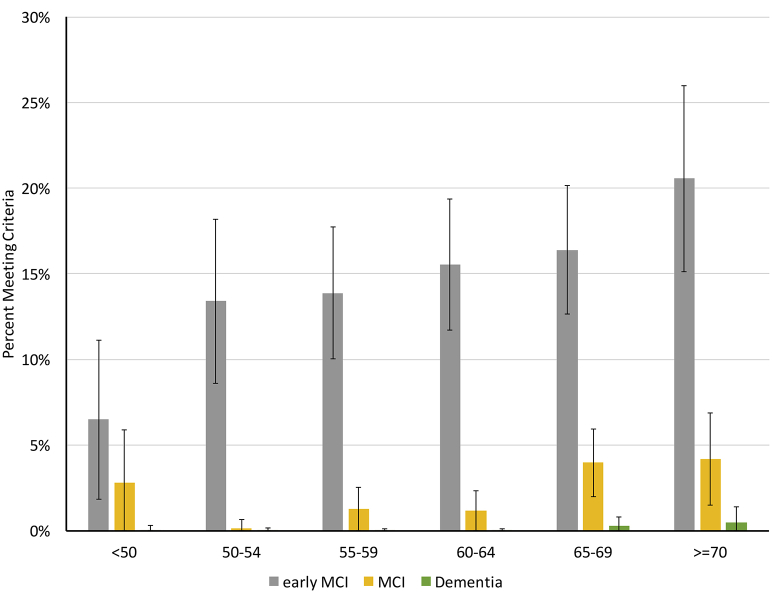
Here, 15.2% of the cohort met early MCI criteria at their last study visit, whereas 2.3% met criteria for MCI and 0.1% met criteria for dementia due to AD. Prevalence for early MCI at the most recent visit was associated with age, ranging from approximately 6% for the youngest participants to 20% for those over 70. Prevalence of early MCI, MCI, and dementia by last visit age is shown in Fig. 3.
Fig. 3.
Cognitive statuses at last study visit, by 5-year age increments. The denominators for each age range were 108 (<50), 194 (50–54), 310 (55–59), 341 (60–64), 378 (65–69), 214 (≥70). Abbreviation: MCI, mild cognitive impairment.
To determine whether demographic and risk features differ by the clinical status and age groups shown in Fig. 3, we conducted Cochran-Mantel-Haenszel tests for independence for the variables APOE ε4 status, PH of AD status, sex, and presence of a college degree on the outcome categorical variable of cognitive status (cognitively normal, early MCI, and MCI/dementia) (combined because there are so few dementia cases), after adjusting for age category. No significant associations between cognitive status and APOE, PH of AD, or education level (<BA vs. ≥BA) were evident after adjusting for age grouping. Sex and cognitive status were not independent (Cochran-Mantel-Haenszel general association test P = .0018) such that men (which comprised 28.6% of the whole sample) were more likely to have early MCI (n = 90 men; 38.3%) or MCI/dementia (n = 16 men; 43.2%). The cohort is relatively young and these associations may change over time.
The designations of “early MCI” and “psychometric MCI” have been used here and in other recent studies to describe cognitive decline that is not sufficiently severe to warrant a diagnosis of MCI. This intermediate stage may have predictive value for identifying persons at risk of progression to MCI or dementia. Specifically, of those who were early MCI at visit 1, 11.4% progressed to a clinical status at their last study visit compared with 2.0% of those who were cognitively normal [χ2(1) = 35.4, P < .0001]. Whether persons with emerging impairment also have greater biomarker signs of AD or vascular pathology is a topic of ongoing investigation. In the parlance of the 2018 research diagnostic framework, these intermediate categories largely overlap with clinical stage 2 which connotes cognitively unimpaired with decline from a prior baseline [42]. Future work will implement the new research criteria in WRAP's diagnostic processes.
3.4. Results and discussion related to goal 2
Goal 2: Characterize the effect of PH and genetic vulnerability on AD-related cognitive trajectories.
3.4.1. Previously published findings
In addition to identifying specific individuals with cognitive impairment, the study seeks to understand how PH of AD and APOE ε4 status (both major risk factors) affect cognitive trajectories from midlife. Earlier cross-sectional analyses of WRAP cognitive data suggested modest relationships between cognitive performance and genetic and/or PH risk factors. For example, at the first visit, PH+ and PH− participants had similarly high scores on a list-learning task, but PH+ participants relied more heavily on recent list items, suggesting greater difficulty with consolidation [62].
As expected, WRAP PH+ participants are more than twice as likely to be APOE ε4 positive (see Table 2). They are also more likely to carry the TREM2 T risk allele [63]. As well, genetic risk features for AD may interact with one another. Two variant alleles of the ABCA7 gene are associated with worse memory and executive function scores in participants with no APOE ε4 alleles but with better scores in those with 1 or 2 APOE ε4 alleles [64]. To the present, longitudinal comparisons have not detected effects of these genetic markers on cognitive trajectories [63], [64]. Boots et al. [65] examined the influence of the brain-derived neurotrophic factor (BDNF) Val66Met polymorphism on cognitive trajectories and PET amyloid load. Compared with Val carriers, BDNF Met carriers exhibit greater decline over time on the Verbal Learning and Memory factor score. In the subset with amyloid imaging, amyloid burden modified the relationship such that those with high amyloid burden who were also BDNF Met carriers exhibited steepest cognitive decline. The aggregate effects of 21 genetic risk alleles on cognition via a PRS identified modest negative effects on working memory performance but not other domains [56]. Darst et al. [56] also examined PRSs specific to causal pathways implicated in AD. Gene clusters affecting Aβ clearance and cholesterol metabolism were strongly predictive of CSF Aβ42, CSF Aβ42/Aβ40, and PiB amyloid burden, as was APOE when considered as an independent predictor on its own (see also [50]).
3.4.2. New results
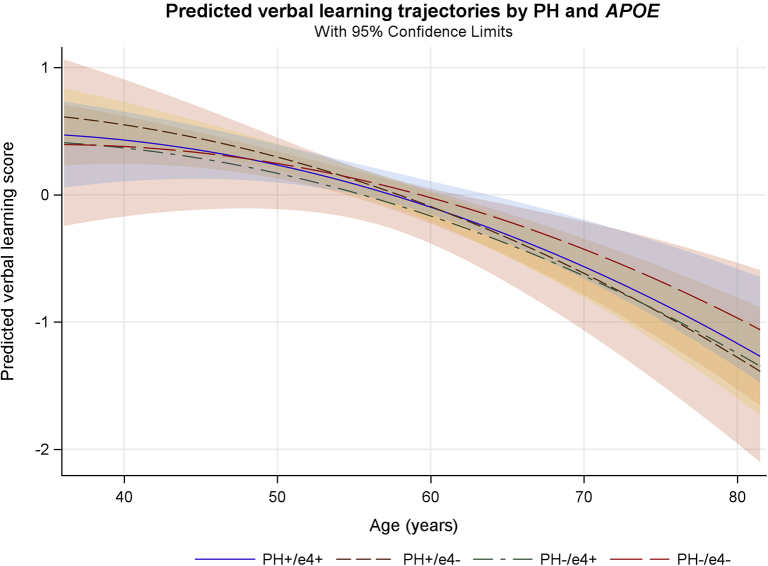
To explore the effects of PH and APOE on longitudinal cognitive trajectories, we modeled the trajectories with a linear mixed effects model [66], [67] using random intercepts at the family and participant levels and a random age slope at the participant level. Fifty-nine participants reporting neurological diagnoses at baseline were excluded from these analyses. Baseline characteristics of this subset were virtually identical to those in Table 3. Covariates included age (linear and quadratic age terms were tested), sex, race, education level, and baseline literacy (WRAT-III Reading), and the number of prior exposures to the neuropsychological test battery [68]. The effects of interest were as follows: (1) the main effects of APOE and PH; (2) their interaction with age (longitudinal effects); and (3) their interaction with prior test exposure, that accounts for the differential benefit from practice. Table 4 lists estimates for each of these terms for Verbal Learning and Memory, an important composite outcome for early cognitive change [57]. Predicted trajectories with age are plotted by APOE and PH status in Fig. 4.
Table 4.
Results of mixed effects model of cognitive decline by APOE ε4 and PH status
| Predictor | PH/APOE status | Estimate | SE | DF | F | P value |
|---|---|---|---|---|---|---|
| Intercept | 0.148 | 0.0635 | ||||
| Practice | 0.0911 | 0.0259 | 1; 3089.8 | 40.9 | <.001 | |
| Age, linear (centered) | −0.0246 | 0.00756 | 1; 1996.5 | 41.7 | <.001 | |
| Age, quadratic | −0.000718 | 0.000167 | 1; 1461.4 | 18.4 | <.001 | |
| Sex (male) | −0.672 | 0.0467 | 1; 1436.9 | 207 | <.001 | |
| Education (BA or greater) | 0.208 | 0.0504 | 1; 1452.9 | 17 | <.001 | |
| Baseline WRAT (centered) | 0.0233 | 0.00253 | 1; 1501.5 | 85.3 | <.001 | |
| Race (nonwhite) | −0.324 | 0.0794 | 1; 1333.8 | 16.6 | <.001 | |
| PH/APOE ε4 Status | PH+/ε4+ | −0.0332 | 0.0668 | 3; 1644 | 0.405 | .749 |
| PH+/ε4− | −0.00163 | 0.0647 | ||||
| PH−/ε4+ | −0.108 | 0.115 | ||||
| PH−/ε4− | – | – | ||||
| PH/APOE ε4 × age | PH+/ε4+ | −0.00748 | 0.00948 | 3; 1698.7 | 0.552 | .647 |
| PH+/ε4− | −0.0116 | 0.00906 | ||||
| PH−/ε4+ | −0.00593 | 0.0168 | ||||
| PH−/ε4− | – | – | ||||
| PH/APOE ε4 × practice | PH+/ε4+ | −0.0123 | 0.0328 | 3; 3153.2 | 0.846 | .468 |
| PH+/ε4− | 0.0268 | 0.0313 | ||||
| PH−/ε4+ | 0.0389 | 0.0584 | ||||
| PH−/ε4− | – | – |
Abbreviation: PH, parental history; WRAT = Wide Range Achievement Test-III Reading Recognition subtest.
NOTE. Coefficients for a linear mixed model of Verbal Learning and Memory performance created using SAS PROC MIXED. Random intercepts were modeled for families and subjects nested within families; age was also included as a subject-level random effect (allowing change with age to vary by individual). F-statistics for fixed effects were calculated using the Kenward-Roger approximation for denominator degrees of freedom.
Fig. 4.
Verbal memory decline by PH of dementia due to probable AD and APOE ε4 binary status (presence/absence of PH and of APOE ε4). All four groups declined with age, but no significant differences between groups are evident. Abbreviations: AD, Alzheimer's disease; PH, parental history.
Although small decrements in performance occur with increasing age, little evidence is observed in these data for effects of APOE or PH on cognitive performance, either in the main analysis or in secondary analyses that (1) excluded participants whose parents developed AD after age 75 years and (2) modeled cognition as a function of APOE genetic risk score rather than an APOE ε4 binary status variable [56]. The lack of APOE or PH risk effects on cognition is unlikely to be due to lack of power. Prospective power calculations using Monte Carlo simulations (k = 1000) indicated power of 0.95 or greater to detect small main effects (mean performance approx. 0.2 SD lower for the highest risk group) and age interactions (age-related slope approx. 20% steeper for the highest risk group). Because the cohort is still relatively young (current mean age 64) and will continue to be followed to determine if an effect unfolds with older age, we caution that the current reported absence of an effect in these data should not be accepted as definitive for the WRAP cohort.
For the subsample who underwent amyloid imaging or CSF collection and on whom Aβ42 assay results were available (N = 211), we classified each participant as amyloid positive (n = 62; 29%) or amyloid negative (n = 149; 71%) using cutoffs described elsewhere [44], [69]. In this subset, amyloid positivity was significantly related to PH and APOE (Table 5; χ2 = 14.22, P = .003). However, follow-up tests indicated the association was largely explained by APOE ε4 carrier status (χ2 = 12.82, P < .001) rather than an independent effect of PH specifically (χ2 = 0.88, P = .35). The significant relationship between APOE ε4 status and amyloid status holds even after controlling for age at the date of biomarker assessment (logistic regression: APOE = 1.263, P < .001). In a smaller subsample for whom longitudinal amyloid (PiB) data were available (N = 142), conversion from amyloid negative to amyloid positive was associated with carriage of at least one APOE ε4 allele (χ2 = 4.24, P = .04) but not with PH, baseline age, gender, or consensus conference diagnosis (all P > .10). Together with the null cognitive findings, these results are consistent with a prevailing biomarker model in which AD pathophysiology precedes cognitive change [1], [70].
Table 5.
Risk (PH and APOE status) versus amyloid positivity
| Amyloid status | PH+/ε4+ (%) | PH+/ε4− (%) | PH−/ε4+ (%) | PH−/ε4− (%) | Total (%) |
|---|---|---|---|---|---|
| Amyloid − | 36 (54) | 70 (80.5) | 9 (69) | 34 (77) | 149 (71) |
| Amyloid + | 31 (46) | 17 (19.5) | 4 (31) | 10 (23) | 62 (29) |
| Total | 67 (100) | 87 (100) | 13 (100) | 44 (100) | 211 (100) |
Abbreviation: PH, parental history.
NOTE. A greater proportion of individuals in the ε4+/PH− and ε4+/PH+ groups were amyloid positive (31–46%) compared to the ε4−/PH− and ε4−/PH+ groups (19.5–23%; χ2(3) = 14.22, P = .003).
3.5. Results and discussion related to goal 3
Goal 3: Determine the biomarker profiles associated with cognitive decline and the development of symptomatic cognitive dysfunction.
The WRAP study spans a period of scientific development in which risk factors like APOE status and PH have given way to more direct biomarkers of AD pathology for characterizing the preclinical stages of AD [1], [70], [71], [72], [73], and less specific brain markers of function and health such as functional and structural MRI have become gauges of the effect of AD pathophysiology on brain function and neurodegeneration. Early structural and functional MRI studies in WRAP (uninformed at the time by AD pathology biomarkers of amyloid and tau) found differences in cerebral activity during memory tasks [74], [75], [76], diffusion tensor imaging [77], and hippocampal morphology [78] as a function of PH or APOE ε4 status. These were interpreted as potentially related to differential AD pathophysiological processes in the PH group, although there was nothing specific to AD pathology about the imaging at the time or about the risk features by which the participants were stratified.
More recently, the effects of CSF Aβ42 and tau and amyloid PET imaging using [C-11]PiB have been examined as indices of the presence or absence of AD pathology. In n = 201 WRAP participants with [C-11]PiB amyloid PET data at a mean age of 61 years, there was no significant relationship with concurrent cognition [51]. This finding was not surprising as amyloid load is expected to increase before cognitive loss. Subsequently, Clark et al. [79] tested cognitive changes over time with mixed effects models and found that greater overall amyloid burden via PiB PET was associated with a greater decline on composite test performance in episodic memory and executive function. Similar results have been found with CSF-derived estimates of amyloid and tau burden [69] suggesting that cognitive consequences of AD pathology may already be present reflecting the gradual accumulation of disease. Moreover, other data suggest that AD pathology in the late-midlife preclinical time frame may coexist with atrophy and/or vascular and other diseases that have secondary effects on neural tissue. Racine et al. [44] used hierarchical clustering analysis of amyloid burden, tau burden, white-matter hyperintensities, and hippocampal atrophy to categorize WRAP and comparable Wisconsin ADRC participants with imaging and CSF data. Four clusters emerged including (1) participants with preclinical AD pathology who were predominantly positive for tau and amyloid; (2) participants with mixed vascular and AD pathology who exhibited white-matter hyperintensities as well as variable AD pathology; (3) participants with suspected non-AD pathology who exhibited atrophy but not Aβ or tau pathology; and (4) participants with healthy aging who exhibited normal imaging and CSF biomarkers. The greatest decline on memory tests over time was observed in the preclinical AD cluster. Taken together, these findings indicate that biomarkers of AD pathology are sensitive to cognitive decline in late middle-aged WRAP participants. As the cohort ages and individuals develop age-related diseases, biomarker profiles will likely become more heterogeneous. Thus, models examining change in biomarkers and cognition over time must include more precise markers of other pathologies as they become available.
3.6. Results and discussion related to goal 4
Goal 4: Characterize the influence of health behaviors on risk and resilience to brain pathology and cognitive decline due to underlying AD.
3.6.1. Previous findings
The effects of modifiable risk factors on cross-sectional cognition have been the target of multiple WRAP investigations. Cognitive activity throughout the lifespan measured by education level [49], job complexity [80], and self-reported current participation in stimulating activities such as games [81], [82] is associated with better performance in several cognitive domains. Participants with greater numbers of stressful life events perform worse on measures of cognitive speed and flexibility, and conversely, in participants with greater social support, performance is better [83]. Of note, the protective effect of social support is diminished by presence of APOE ε4 [84]. Sleep adequacy in WRAP participants is associated with amyloid burden assessed with amyloid imaging [85] and CSF Aβ42 and tau levels [46]. Cardiovascular fitness and metabolic fitness also appear to have a protective effect on gray matter, cerebral blood flow, and episodic memory performance. Insulin resistance in particular is linked with cerebral atrophy, amyloid burden, CSF biomarkers of AD pathology, and lower cerebral glucose uptake [86], [87], [88], [89], [90], [91].
3.6.1.1. Physical activity and brain health
Physical activity (PA) and related variables including cardiorespiratory fitness are well-studied protective factors for AD dementia, with a recent evidence review identifying PA as the modifiable factor with the highest impact on reducing the national prevalence of this disease ([92], but see also [93]). Cross-sectional WRAP publications elucidate the relationship between PA, cognition, brain structure, and neuropathological markers of AD among normal adults. In n = 315 WRAP participants, Boots et al. [94] found that engagement in PA was associated with preserved volume in diverse brain regions including the medial and lateral temporal lobe and medial parietal lobe, together with reduced white-matter ischemic lesions and with fewer memory complaints. Dougherty et al. [95] assessed PA via accelerometer in 91 WRAP participants and found that those meeting recommended PA levels had greater temporal lobe regional volumes including the hippocampus compared to those who did not meet recommended activity levels. In addition to effects on brain structure and cognition, PA moderated the effect of age [96] and genetic risk factors [50] on AD pathophysiological biomarkers in WRAP participants. Specifically, Okonkwo et al. [96] report that a history of PA was associated with an attenuation of age-related alterations in Aβ burden, cerebral glucose metabolism, and hippocampal volume. Similarly, Schultz et al. [50] found that cardiorespiratory fitness attenuated the adverse influence of cholesterol metabolism polygenetic risk on CSF biomarkers. Of note, the beneficial effect of PA on the brain substrates of cognitive health may depend on the level of exercise intensity [97].
In aggregate, these associational studies in WRAP participants suggest that modifiable factors such as physical and cognitive activity, glucose and metabolic regulation, stress, and sleep may be avenues for interventions that enhance brain health and reduce the likelihood and severity of AD pathology.
3.7. Future directions
WRAP and its linked studies are charting the preclinical time course of AD. Ongoing WRAP investigations assess lifestyle, genetic risk, and resilience factors along with longitudinal cognitive and clinical assessments to establish whether AD biomarker trajectories and cognitive trajectories can be identified in midlife. The associational findings from WRAP which have been partially summarized here now require further study to determine whether improving these health behaviors can result in measurable effect on AD biomarkers and brain and cognition health in late-midlife.
Whereas WRAP's organizing theme in 2001 was risk enrichment due to PH of dementia due to probable AD, focus has broadened in the ensuing years to AD biomarkers. In the present phase of WRAP, CSF and PET biomarkers of AD pathology are sought from all willing participants, funding permitting, as visits at 2-year intervals continue. Biannual (and now annual) information sessions with participants to share back what we are learning serve to educate participants on the overarching importance of biomarker enrollment and brain donation and are also an effective retention component. Although PH as an enrichment factor has been supplanted in part by the capability to directly measure AD pathology in vivo, the experience of having a parent with AD dementia motivates many of our participants to remain in WRAP and take part in linked studies at a high level of volunteerism. A caveat is that the participant characteristics are biased toward and most generalizable to persons who have a parent with dementia due to probable AD by design. The cohort is also biased in other ways. Because WRAP is a self-selected sample of convenience, the majority of the cohort are Caucasian (88%), women (71%), and highly educated (mean 16 years). Increasing the ethnic diversity of WRAP participants and assuring that WRAP's findings are generalizable to African Americans in particular is a current priority.
Data from the core WRAP protocol and from a subset of WRAP's linked studies are accessible to qualified researchers via an online request form and data use agreement which can be linked from the Global Alzheimer's Association Interactive Network web site (www.gaain.org). Recent examples of data-sharing collaborations include a study that found consistency in patterns of cognitive aging progression scores across the Baltimore Longitudinal Study on Aging and WRAP [98], a meta-analysis of APOE and sex on dementia incidence [99], and a study involving predictive algorithms for MCI in a consortium of five preclinical AD or adult children cohorts [100].
The WRAP observational longitudinal cohort is AD risk enriched and has been followed with detailed measurements since midlife. This is a time frame that is less well studied than older ages but is nevertheless a critical epoch, as this is when AD pathology likely begins and when its trajectory may be modifiable through pharmacologic and/or lifestyle approaches.
Research in Context.
-
1.
Systematic review: The Wisconsin Registry for Alzheimer's Prevention is a natural history observational cohort enriched for Alzheimer's disease (AD) risk. This article describes the study protocol and reviews study findings and interim new results.
-
2.
Interpretation: The study is determining new ways by which subtle cognitive decline can be identified. The published and new results from this relatively young cohort (current mean age 64) suggest that cognitive trajectories are steeper in people who exhibit elevations in AD biomarkers but not yet by parental history or by apolipoprotein E status. Numerous Wisconsin Registry for Alzheimer's Prevention studies suggest that health and lifestyle features are associated with cognitive decline and with biomarkers of brain health and AD pathophysiology.
-
3.
Future directions: Future directions include broadening collection of AD biomarkers to which cognitive outcomes can be linked. Such data will provide new knowledge on the early temporal course of AD pathophysiology and inform the design of secondary prevention clinical trials.
Acknowledgments
This research was supported by the National Institutes of Health awards (R01 AG027161, R01 AG021155, R01 AG054047, R01 AG037639, P50 AG033514, UL1 TR000427, K23 AG045957, F30AG054115, T32 GM007507, and T32 GM008692) and grants from the Alzheimer's Association, Extendicare Foundation, and Northwestern Mutual Life Foundation to the University of Wisconsin–Madison, and by donor funds including the Wisconsin Alzheimer's Institute Lou Holland Fund and contributions from anonymous donors. Portions of this research were supported by resources at the Wisconsin Alzheimer's Institute, the Wisconsin Alzheimer's Disease Research Center, and the Geriatric Research Education and Clinical Center of the William S. Middleton Memorial Veterans Hospital, Madison, WI. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors(s) and do not necessarily reflect the views of the NIH or the Veterans Administration. The authors gratefully acknowledge the WRAP study team who have carefully acquired the longitudinal data and the WRAP participants who make this research possible.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.dadm.2017.11.007.
Supplementary data
References
- 1.Jack C.R., Jr., Knopman D.S., Jagust W.J., Petersen R.C., Weiner M.W., Aisen P.S. Tracking pathophysiological processes in Alzheimer's disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12:207–216. doi: 10.1016/S1474-4422(12)70291-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sager M.A., Hermann B., La Rue A. Middle-aged children of persons with Alzheimer's disease: APOE genotypes and cognitive function in the Wisconsin Registry for Alzheimer's Prevention. J Geriatr Psychiatry Neurol. 2005;18:245–249. doi: 10.1177/0891988705281882. [DOI] [PubMed] [Google Scholar]
- 3.McKhann G., Drachman D., Folstein M., Katzman R., Price D., Stadlan E.M. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 4.Ellis R.J., Jan K., Kawas C., Koller W.C., Lyons K.E., Jeste D.V. Diagnostic validity of the dementia questionnaire for Alzheimer disease. Arch Neurol. 1998;55:360–365. doi: 10.1001/archneur.55.3.360. [DOI] [PubMed] [Google Scholar]
- 5.Kawas C., Segal J., Stewart W.F., Corrada M., Thal L.J. A validation study of the Dementia Questionnaire. Arch Neurol. 1994;51:901–906. doi: 10.1001/archneur.1994.00540210073015. [DOI] [PubMed] [Google Scholar]
- 6.Wechsler D. The Psychological Corporation; San Antonio, TX: 1999. WASI: Wechsler Abbreviated Scale of Intelligence. [Google Scholar]
- 7.Wilkinson G.S. 3rd ed. Jastak Association; Wilmington, DE: 1993. The Wide Range Achievement Test: Manual. [Google Scholar]
- 8.Schmidt M. Western Psychological Services; Los Angeles, CA: 1996. Rey Auditory Verbal Learning Test: A Handbook. [Google Scholar]
- 9.Kaplan E., Goodglass H., Weintraub S. PRO-ED, Inc; Austin, TX: 2001. Boston Naming Test – Second Edition. [Google Scholar]
- 10.Rouleau I., Salmon D.P., Butters N., Kennedy C., McGuire K. Quantitative and qualitative analyses of clock drawings in Alzheimer's and Huntington's disease. Brain Cogn. 1992;18:70–87. doi: 10.1016/0278-2626(92)90112-y. [DOI] [PubMed] [Google Scholar]
- 11.Benton A.L., Hamsher K.S., Sivan A.B. Psychological Assessment Resources; Lutz, FL: 1994. Multilingual Aphasia Examination. [Google Scholar]
- 12.Wechsler D. The Psychological Corporation; San Antonio, TX: 1997. Wechsler Adult Intelligence Scale–III. [Google Scholar]
- 13.Reitan R.M. Validity of the Trail Making Test as an indicator of organic brain damage. Perceptual Mot Skills. 1958;8:271–276. [Google Scholar]
- 14.Trenerry M.R., Crosson B., DeBoe J., Leber W.R. Pychological Assessment Resources, Inc; Odessa, FL: 1989. The Stroop Neuropsychological Screening Test. [Google Scholar]
- 15.Benedict R.H. Psychological Assessment Resources, Inc; Odessa, FL: 1997. Brief Visuospatial Memory Test–Revised. [Google Scholar]
- 16.Wechsler D. Harcourt Brace & Co. for The Psychological Corporation; San Antonio, TX: 1981. Wechsler Adult Intelligence Scale–Revised. [Google Scholar]
- 17.Wechsler D. Harcourt Brace Jovanovich, Inc. for the Psychological Corporation; New York, NY: 1987. Wechsler Memory Scale–Revised. [Google Scholar]
- 18.Folstein M.F., Folstein S.E., McHugh P.R. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 19.Rosen W.G. Verbal fluency in aging and dementia. J Clin Exp Neuropsychol. 1980;2:135–146. [Google Scholar]
- 20.Goodglass H., Kaplan E. Lippincott Williams & Wilkins; Baltimore, MD: 1983. Boston Diagnostic Aphasia Examination–3rd Edition. [Google Scholar]
- 21.Cogstate . Cogstate; Melbourne, Australia: 2011. Cogstate Research Manual, Version 6. [Google Scholar]
- 22.Radloff L.S. The CES-D Scale. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 23.Morris M.C., Tangney C.C., Wang Y., Sacks F.M., Barnes L.L., Bennett D.A. MIND diet slows cognitive decline with aging. Alzheimers Dement. 2015;11:1015–1022. doi: 10.1016/j.jalz.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stewart A.L., Mills K.M., King A.C., Haskell W.L., Gillis D., Ritter P.L. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33:1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Hays R.D., Stewart A.L. Sleep measures. In: Stewart A.L., Ware J.E., editors. Measuring function and well-being. Duke University Press; Durham: 1992. [Google Scholar]
- 26.Johns M.W. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 27.Bastien C.H., Vallières A., Morin C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 28.Schinka J.A., Mcbride A., Vanderploeg R.D., Tennyson K., Borenstein A.R., Mortimer J.A. Florida cognitive activities scale: initial development and validation. J Int Neuropsychol Soc. 2005;11:108–116. doi: 10.1017/S1355617705050125. [DOI] [PubMed] [Google Scholar]
- 29.Galvin J.E. The Quick Dementia Rating System (Qdrs): a rapid dementia staging tool. Alzheimers Dement (Amst) 2015;1:249–259. doi: 10.1016/j.dadm.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morris J.C. Clinical dementia rating: a reliable and valid diagnostic and staging measure for dementia of the Alzheimer type. Int psychogeriatrics. 1997;9:173–176. doi: 10.1017/s1041610297004870. [DOI] [PubMed] [Google Scholar]
- 31.Jorm A., Jacomb P. The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): socio-demographic correlates, reliability, validity and some norms. Psychol Med. 1989;19:1015–1022. doi: 10.1017/s0033291700005742. [DOI] [PubMed] [Google Scholar]
- 32.Lawton M.P., Brody E.M. Assessment of older people: self-maintaining and instrumental activities of daily living. Nurse Res. 1970;19:278. [PubMed] [Google Scholar]
- 33.Berman S.E., Koscik R.L., Clark L.R., Mueller K.D., Bluder L., Galvin J.E. Use of the Quick Dementia Rating System (QDRS) as an initial screening measure in a longitudinal cohort at risk for Alzheimer's disease. JAD Rep. 2017;1:9–13. doi: 10.3233/ADR-170004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Albert M.S., Dekosky S.T., Dickson D., Dubois B., Feldman H.H., Fox N.C. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:270–279. doi: 10.1016/j.jalz.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Edmonds E.C., Delano-Wood L., Clark L.R., Jak A.J., Nation D.A., McDonald C.R. Susceptibility of the conventional criteria for mild cognitive impairment to false-positive diagnostic errors. Alzheimers Dement. 2015;11:415–424. doi: 10.1016/j.jalz.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pedraza O., Lucas J.A., Smith G.E., Petersen R.C., Graff-Radford N.R., Ivnik R.J. Robust and expanded norms for the Dementia Rating Scale. Arch Clin Neuropsychol. 2010;25:347–358. doi: 10.1093/arclin/acq030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sliwinski M., Lipton R.B., Buschke H., Stewart W. The effects of preclinical dementia on estimates of normal cognitive functioning in aging. J Gerontol B Psychol Sci Soc Sci. 1996;51:217–225. doi: 10.1093/geronb/51b.4.p217. [DOI] [PubMed] [Google Scholar]
- 38.De Santi S., Pirraglia E., Barr W., Babb J., Williams S., Rogers K. Robust and conventional neuropsychological norms: diagnosis and prediction of age-related cognitive decline. Neuropsychology. 2008;22:469–484. doi: 10.1037/0894-4105.22.4.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Koscik R.L., La Rue A., Jonaitis E.M., Okonkwo O.C., Johnson S.C., Bendlin B.B. Emergence of mild cognitive impairment in late middle-aged adults in the wisconsin registry for Alzheimer's prevention. Dement Geriatr Cogn Disord. 2014;38:16–30. doi: 10.1159/000355682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Clark L.R., Koscik R.L., Nicholas C.R., Okonkwo O.C., Engelman C.D., Bratzke L.C. Mild cognitive impairment in late middle age in the Wisconsin Registry for Alzheimer's Prevention Study: prevalence and characteristics using robust and standard neuropsychological normative data. Arch Clin Neuropsychol. 2016;31:675–688. doi: 10.1093/arclin/acw024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Koscik R.L., Berman S.E., Clark L.R., Mueller K.D., Okonkwo O.C., Gleason C.E. Intraindividual cognitive variability in middle age predicts cognitive impairment 8-10 years later: results from the Wisconsin Registry for Alzheimer's Prevention. J Int Neuropsychol Soc. 2016;22:1016–1025. doi: 10.1017/S135561771600093X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jack CRJ, Bennett DA, Blennow K, Carrillo MC, Dunn B, Elliott C, et al. NIA-AA research framework: towards a biological definition of Alzheimer's disease. Available at: https://www.alz.org/aaic/nia-aa.asp. Accessed December 22, 2017.
- 43.Bendlin B.B., Carlsson C.M., Johnson S.C., Zetterberg H., Blennow K., Willette A.A. CSF T-Tau/Abeta42 predicts white matter microstructure in healthy adults at risk for Alzheimer's disease. PLoS One. 2012;7:e37720. doi: 10.1371/journal.pone.0037720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Racine A.M., Koscik R.L., Berman S.E., Nicholas C.R., Clark L.R., Okonkwo O.C. Biomarker clusters are differentially associated with longitudinal cognitive decline in late midlife. Brain. 2016;139:2261–2274. doi: 10.1093/brain/aww142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Racine A.M., Koscik R.L., Nicholas C.R., Clark L.R., Okonkwo O.C., Oh J.M. Cerebrospinal fluid ratios with Abeta42 predict preclinical brain beta-amyloid accumulation. Alzheimers Dement (Amst) 2016;2:27–38. doi: 10.1016/j.dadm.2015.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sprecher K.E., Koscik R.L., Carlsson C.M., Zetterberg H., Blennow K., Okonkwo O.C. Poor sleep is associated with CSF biomarkers of amyloid pathology in cognitively normal adults. Neurology. 2017;89:445–453. doi: 10.1212/WNL.0000000000004171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dean D.C., 3rd, Hurley S.A., Kecskemeti S.R., O'Grady J.P., Canda C., Davenport-Sis N.J. Association of amyloid pathology with myelin alteration in preclinical Alzheimer disease. JAMA Neurol. 2017;74:41–49. doi: 10.1001/jamaneurol.2016.3232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hoy A.R., Ly M., Carlsson C.M., Okonkwo O.C., Zetterberg H., Blennow K. Microstructural white matter alterations in preclinical Alzheimer's disease detected using free water elimination diffusion tensor imaging. PLoS One. 2017;12:e0173982. doi: 10.1371/journal.pone.0173982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Almeida R.P., Schultz S.A., Austin B.P., Boots E.A., Dowling N.M., Gleason C.E. Effect of cognitive reserve on age-related changes in cerebrospinal fluid biomarkers of Alzheimer disease. JAMA Neurol. 2015;72:699–706. doi: 10.1001/jamaneurol.2015.0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schultz S.A., Boots E.A., Darst B.F., Zetterberg H., Blennow K., Edwards D.F. Cardiorespiratory fitness alters the influence of a polygenic risk score on biomarkers of AD. Neurology. 2017;88:1650–1658. doi: 10.1212/WNL.0000000000003862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Johnson S.C., Christian B.T., Okonkwo O.C., Oh J.M., Harding S., Xu G. Amyloid burden and neural function in people at risk for Alzheimer's Disease. Neurobiol Aging. 2014;35:576–584. doi: 10.1016/j.neurobiolaging.2013.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lambert J.C., Ibrahim-Verbaas C.A., Harold D., Naj A.C., Sims R., Bellenguez C. Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer's disease. Nat Genet. 2013;45:1452–1458. doi: 10.1038/ng.2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Guerreiro R., Wojtas A., Bras J., Carrasquillo M., Rogaeva E., Majounie E. TREM2 variants in Alzheimer's disease. N Engl J Med. 2013;368:117–127. doi: 10.1056/NEJMoa1211851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jonsson T., Stefansson H., Steinberg S., Jonsdottir I., Jonsson P.V., Snaedal J. Variant of TREM2 associated with the risk of Alzheimer's disease. N Engl J Med. 2013;368:107–116. doi: 10.1056/NEJMoa1211103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cruchaga C., Karch C.M., Jin S.C., Benitez B.A., Cai Y., Guerreiro R. Rare coding variants in the phospholipase D3 gene confer risk for Alzheimer's disease. Nature. 2014;505:550–554. doi: 10.1038/nature12825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Darst B.F., Koscik R.L., Racine A.M., Oh J.M., Krause R.A., Carlsson C.M. Pathway-specific polygenic risk scores as predictors of amyloid-beta deposition and cognitive function in a sample at increased risk for Alzheimer's disease. J Alzheimers Dis. 2017;55:473–484. doi: 10.3233/JAD-160195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dowling N.M., Hermann B., La Rue A., Sager M.A. Latent structure and factorial invariance of a neuropsychological test battery for the study of preclinical Alzheimer's disease. Neuropsychology. 2010;24:742–756. doi: 10.1037/a0020176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mueller K.D., Koscik R.L., Turkstra L.S., Riedeman S.K., LaRue A., Clark L.R. Connected language in late middle-aged adults at risk for Alzheimer's disease. J Alzheimers Dis. 2016;54:1539–1550. doi: 10.3233/JAD-160252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mueller K.D., Koscik R.L., LaRue A., Clark L.R., Hermann B., Johnson S.C. Verbal fluency and early memory decline: results from the Wisconsin Registry for Alzheimer's Prevention. Arch Clin Neuropsychol. 2015;30:448–457. doi: 10.1093/arclin/acv030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bondi M.W., Edmonds E.C., Jak A.J., Clark L.R., Delano-Wood L., McDonald C.R. Neuropsychological criteria for mild cognitive impairment improves diagnostic precision, biomarker associations, and progression rates. J Alzheimers Dis. 2014;42:275–289. doi: 10.3233/JAD-140276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Clark L.R., Delano-Wood L., Libon D.J., McDonald C.R., Nation D.A., Bangen K.J. Are empirically-derived subtypes of mild cognitive impairment consistent with conventional subtypes? J Int Neuropsychol Soc. 2013;19:635–645. doi: 10.1017/S1355617713000313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.La Rue A., Hermann B., Jones J.E., Johnson S., Asthana S., Sager M.A. Effect of parental family history of Alzheimer's disease on serial position profiles. Alzheimers Dement. 2008;4:285–290. doi: 10.1016/j.jalz.2008.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Engelman C.D., Koscik R.L., Jonaitis E.M., Hermann B.P., La Rue A., Sager M.A. Investigation of triggering receptor expressed on myeloid cells 2 variant in the Wisconsin Registry for Alzheimer's Prevention. Neurobiol Aging. 2014;35:1252–1254. doi: 10.1016/j.neurobiolaging.2013.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Engelman C.D., Koscik R.L., Jonaitis E.M., Okonkwo O.C., Hermann B.P., La Rue A. Interaction between two cholesterol metabolism genes influences memory: findings from the Wisconsin Registry for Alzheimer's Prevention. J Alzheimers Dis. 2013;36:749–757. doi: 10.3233/JAD-130482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Boots E.A., Schultz S.A., Clark L.R., Racine A.M., Darst B.F., Koscik R.L. BDNF Val66Met predicts cognitive decline in the Wisconsin Registry for Alzheimer's Prevention. Neurology. 2017;88:2098–2106. doi: 10.1212/WNL.0000000000003980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Laird N.M., Ware J.H. Random-effects models for longitudinal data. Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- 67.Singer J.D. Using SAS PROC MIXED to fit multilevel models, hierarchical models and individual growth models. J Educ Behav Stat. 1998;24:323–355. [Google Scholar]
- 68.Jonaitis E.M., Koscik R.L., La Rue A., Johnson S.C., Hermann B.P., Sager M.A. Aging, practice effects, and genetic risk in the Wisconsin Registry for Alzheimer's Prevention. Clin Neuropsychol. 2015;29:426–441. doi: 10.1080/13854046.2015.1047407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Clark L.R., Berman S.E., Norton D., Koscik R.L., Jonaitis E.M., Blennow K. Age-accelerated cognitive decline in asymptomatic adults with CSF β-amyloid. bioRxiv. 2017 doi: 10.1212/WNL.0000000000005291. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jack C.R., Jr., Bennett D.A., Blennow K., Carrillo M.C., Feldman H.H., Frisoni G.B. A/T/N: an unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology. 2016;87:539–547. doi: 10.1212/WNL.0000000000002923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sperling R.A., Aisen P.S., Beckett L.A., Bennett D.A., Craft S., Fagan A.M. Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:280–292. doi: 10.1016/j.jalz.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Klunk W.E., Engler H., Nordberg A., Wang Y., Blomqvist G., Holt D.P. Imaging brain amyloid in Alzheimer's disease with Pittsburgh Compound-B. Ann Neurol. 2004;55:306–319. doi: 10.1002/ana.20009. [DOI] [PubMed] [Google Scholar]
- 73.Blennow K., Dubois B., Fagan A.M., Lewczuk P., de Leon M.J., Hampel H. Clinical utility of cerebrospinal fluid biomarkers in the diagnosis of early Alzheimer's disease. Alzheimers Dement. 2015;11:58–69. doi: 10.1016/j.jalz.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Johnson S.C., Ries M.L., Hess T.M., Carlsson C.M., Gleason C.E., Alexander A.L. Effect of Alzheimer disease risk on brain function during self-appraisal in healthy middle-aged adults. Arch Gen Psychiatry. 2007;64:1163–1171. doi: 10.1001/archpsyc.64.10.1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Johnson S.C., Schmitz T.W., Trivedi M.A., Ries M.L., Torgerson B.M., Carlsson C.M. The influence of Alzheimer disease family history and apolipoprotein E epsilon4 on mesial temporal lobe activation. J Neurosci. 2006;26:6069–6076. doi: 10.1523/JNEUROSCI.0959-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Xu G., McLaren D.G., Ries M.L., Fitzgerald M.E., Bendlin B.B., Rowley H.A. The influence of parental history of Alzheimer's disease and apolipoprotein E epsilon4 on the BOLD signal during recognition memory. Brain. 2009;132:383–391. doi: 10.1093/brain/awn254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bendlin B.B., Ries M.L., Canu E., Sodhi A., Lazar M., Alexander A.L. White matter is altered with parental family history of Alzheimer's disease. Alzheimers Dement. 2010;6:394–403. doi: 10.1016/j.jalz.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Okonkwo O.C., Xu G., Dowling N.M., Bendlin B.B., Larue A., Hermann B.P. Family history of Alzheimer disease predicts hippocampal atrophy in healthy middle-aged adults. Neurology. 2012;78:1769–1776. doi: 10.1212/WNL.0b013e3182583047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Clark L.R., Racine A.M., Koscik R.L., Okonkwo O.C., Engelman C.D., Carlsson C.M. Beta-amyloid and cognitive decline in late middle age: findings from the Wisconsin Registry for Alzheimer's Prevention study. Alzheimers Dement. 2016;12:805–814. doi: 10.1016/j.jalz.2015.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Boots E.A., Schultz S.A., Almeida R.P., Oh J.M., Koscik R.L., Dowling M.N. Occupational complexity and cognitive reserve in a middle-aged cohort at risk for Alzheimer's disease. Arch Clin Neuropsychol. 2015;30:634–642. doi: 10.1093/arclin/acv041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Schultz S.A., Larson J., Oh J., Koscik R., Dowling M.N., Gallagher C.L. Participation in cognitively-stimulating activities is associated with brain structure and cognitive function in preclinical Alzheimer's disease. Brain Imaging Behav. 2015;9:729–736. doi: 10.1007/s11682-014-9329-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jonaitis E.M., La Rue A., Mueller K.D., Koscik R.L., Hermann B., Sager M.A. Cognitive activities and cognitive performance in middle-aged adults at risk for Alzheimer's disease. Psychol Aging. 2013;28:1004–1014. doi: 10.1037/a0034838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zuelsdorff M.L., Koscik R.L., Okonkwo O.C., Peppard P.E., Hermann B.P., Sager M.A. Reliability of a Novel Social Activity Questionnaire. J Aging Health. 2016 doi: 10.1177/0898264316674812. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zuelsdorff M.L., Engelman C.D., Friedman E.M., Koscik R.L., Jonaitis E.M., Rue A.L. Stressful events, social support, and cognitive function in middle-aged adults with a family history of Alzheimer's disease. J Aging Health. 2013;25:944–959. doi: 10.1177/0898264313498416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sprecher K.E., Bendlin B.B., Racine A.M., Okonkwo O.C., Christian B.T., Koscik R.L. Amyloid burden is associated with self-reported sleep in nondemented late middle-aged adults. Neurobiol Aging. 2015;36:2568–2576. doi: 10.1016/j.neurobiolaging.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ward M.A., Bendlin B.B., McLaren D.G., Hess T.M., Gallagher C.L., Kastman E.K. Low HDL cholesterol is associated with lower gray matter volume in cognitively healthy adults. Front Aging Neurosci. 2010;2 doi: 10.3389/fnagi.2010.00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Willette A.A., Xu G., Johnson S.C., Birdsill A.C., Jonaitis E.M., Sager M.A. Insulin resistance, brain atrophy, and cognitive performance in late middle-aged adults. Diabetes care. 2013;36:443–449. doi: 10.2337/dc12-0922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Birdsill A.C., Carlsson C.M., Willette A.A., Okonkwo O.C., Johnson S.C., Xu G. Low cerebral blood flow is associated with lower memory function in metabolic syndrome. Obesity. 2013;21:1313–1320. doi: 10.1002/oby.20170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Starks E.J., Patrick O'Grady J., Hoscheidt S.M., Racine A.M., Carlsson C.M., Zetterberg H. Insulin resistance is associated with higher cerebrospinal fluid tau levels in asymptomatic APOEvarepsilon4 carriers. J Alzheimers Dis. 2015;46:525–533. doi: 10.3233/JAD-150072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Willette A.A., Bendlin B.B., Starks E.J., Birdsill A.C., Johnson S.C., Christian B.T. Association of insulin resistance with cerebral glucose uptake in late middle-aged adults at risk for Alzheimer disease. JAMA Neurol. 2015;72:1013–1020. doi: 10.1001/jamaneurol.2015.0613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Willette A.A., Johnson S.C., Birdsill A.C., Sager M.A., Christian B., Baker L.D. Insulin resistance predicts brain amyloid deposition in late middle-aged adults. Alzheimers Dement. 2015;11:504–510.e1. doi: 10.1016/j.jalz.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Barnes D.E., Yaffe K. The projected effect of risk factor reduction on Alzheimer's disease prevalence. Lancet Neurol. 2011;10:819–828. doi: 10.1016/S1474-4422(11)70072-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sabia S., Dugravot A., Dartigues J.F., Abell J., Elbaz A., Kivimaki M. Physical activity, cognitive decline, and risk of dementia: 28 year follow-up of Whitehall II cohort study. BMJ. 2017;357:j2709. doi: 10.1136/bmj.j2709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Boots E.A., Schultz S.A., Oh J.M., Larson J., Edwards D., Cook D. Cardiorespiratory fitness is associated with brain structure, cognition, and mood in a middle-aged cohort at risk for Alzheimer's disease. Brain Imaging Behav. 2015;9:639–649. doi: 10.1007/s11682-014-9325-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dougherty R.J., Ellingson L.D., Schultz S.A., Boots E.A., Meyer J.D., Lindheimer J.B. Meeting physical activity recommendations may be protective against temporal lobe atrophy in older adults at risk for Alzheimer's disease. Alzheimers Dement (Amst) 2016;4:14–17. doi: 10.1016/j.dadm.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Okonkwo O.C., Schultz S.A., Oh J.M., Larson J., Edwards D., Cook D. Physical activity attenuates age-related biomarker alterations in preclinical AD. Neurology. 2014;83:1753–1760. doi: 10.1212/WNL.0000000000000964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dougherty R.J., Schultz S.A., Kirby T.K., Boots E.A., Oh J.M., Edwards D. Moderate physical activity is associated with cerebral glucose metabolism in adults at risk for Alzheimer's disease. J Alzheimers Dis. 2017;58:1089–1097. doi: 10.3233/JAD-161067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bilgel M., Koscik R.L., An Y., Prince J.L., Resnick S.M., Johnson S.C. Temporal order of Alzheimer's disease-related cognitive marker changes in BLSA and WRAP longitudinal studies. J Alzheimers Dis. 2017;59:1335–1347. doi: 10.3233/JAD-170448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Neu S.C., Pa J., Kukull W., Beekly D., Kuzma A., Gangadharan P. Apolipoprotein E genotype and sex risk factors for Alzheimer disease: a meta-analysis. JAMA Neurol. 2017;74:1178–1189. doi: 10.1001/jamaneurol.2017.2188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gross A.L., Hassenstab J.J., Johnson S.C., Clark L.R., Resnick S.M., Kitner-Triolo M. A classification algorithm for predicting progression from normal cognition to mild cognitive impairment across five cohorts: the preclinical AD consortium. Alzheimers Dement (Amst) 2017;8:147–155. doi: 10.1016/j.dadm.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.