Abstract
Background:
Three-quarters of patients who undergo total hip replacement (THR) receive postsurgical rehabilitation care in an inpatient rehabilitation facility (IRF), a skilled nursing facility (SNF), or through a home health agency. The objectives of this study are to examine racial differences where THR recipients receive postsurgical rehabilitation care and determine whether discharge destination is associated with hospital readmission.
Methods:
Using the Pennsylvania Health Care Cost Containment Council database, we selected African American (AA) or white adults who underwent THR surgery (n = 68,016). We used multinomial logistic regression models to assess the relationship between race and postsurgical discharge destination. We calculated 90-day hospital readmission as function of discharge destination.
Results:
Among patients <65 years, compared to whites, AAs had a higher risk of discharge to an IRF (adjusted relative risk ratio [aRRR]: 2.56, 95% confidence interval [CI]: 1.77-3.71) and a SNF (aRRR 3.37, 95% CI: 2.07-5.49). Among those ≥65 years, AA patients also had a higher risk of discharge to an IRF (aRRR: 1.96, 95% CI: 1.39-2.76) and a SNF (aRRR: 3.66, 95% CI: 2.29-5.84). Discharge to either IRF or SNF, instead of home with self-care, was significantly associated with higher odds of 90-day hospital readmission (<65 years: adjusted odds ratio [aOR]: 4.06, 95% CI: 3.49-4.74; aOR: 2.05, 95% CI: 1.70-2.46, respectively; ≥65 years: aOR: 4.32, 95% CI: 3.67-5.09, respectively; aOR: 1.74, 95% CI: 1.46-2.07, respectively).
Conclusions:
Compared to whites, AAs who underwent THR were more likely to be discharged to an IRF or SNF. Discharge to either facility was associated with a higher risk of hospital readmission.
Keywords: race, rehabilitation, hip arthroplasty, hip replacement surgery
Introduction
Total hip replacement (THR) surgery has become one of the most successful and frequently performed elective surgeries in the United States. It is the primary treatment for patients with end-stage hip osteoarthritis (OA) who have failed conservative treatment. With the increasing prevalence of OA and the aging of the US population, THR utilization is anticipated to grow. According to the US National Center for Health Statistics, THR among patients who are 45 years or older increased from 138 700 to 310 000 from the years 2000 to 2010.1 By 2030, the demand for THR is expected to grow up to 572 000.2 Technological advancements have also prolonged prosthetic device life expectancy. For instance, implant survivorship is estimated at higher than 80% at 25-year follow-up.3
Numerous studies have reported marked racial/ethnic variation in the utilization of THR in the management of end-stage hip OA.4-8 However, less is known regarding racial/ethnic variations in postsurgical care processes and outcomes. A Medicare claims data analysis found that African Americans (AAs) had greater risk of mortality following primary THR than whites.9 Two separate studies found that racial/ethnic minorities were at an increased risk of a longer hospital stay after THR.10,11 In studies of patients who underwent hip or knee replacement surgery, AAs reported having worse health and OA-related pain and disability than whites preoperatively and postoperatively.12,13
A few studies have examined racial/ethnic variations in rehabilitation destination after THR. However, these studies are also limited by inadequate risk adjustment14 or comparisons were done in patients who underwent total knee replacement with THR surgery in aggregate.15,16 A few other studies found that the patterns of postacute rehabilitation care (PARC) use following lower extremity joint replacement by race varied by state.15-17 Regardless, many patients are discharged home after joint replacement surgery, although about 75% obtain rehabilitation care in an inpatient rehabilitation facility (IRF), in a skilled nursing facility (SNF), or through a home health (HH) agency.18
Finally, there is evidence that discharge destination after lower extremity joint replacement surgery may significantly influence acute care hospital readmission.19-23 More specifically, discharge to a SNF and possibly an IRF appears to increase the risk of readmission.19-23 In 2012, the Centers for Medicare & Medicaid Services (CMS) identified acute care readmission rates after elective total knee replacement or THR as a measure of hospital quality with major financial consequences.24
The primary objectives of this study were to examine whether there are racial variations in discharge destination after THR and to determine whether discharge destination is associated with all-cause 90-day risk of acute care hospital readmission. We hypothesized that racial minority patients will have higher rate of discharge to an IRF or SNF for postsurgical rehabilitation care and consequently will face higher risk of readmission to an acute care hospital within 90 days of discharge.
Methods
Study Sample
The study sample and study variables were previously described.16 Briefly, the Pennsylvania Health Care Cost Containment Council (PHC4) database was used to identify patients who underwent elective primary THR surgery in the state of Pennsylvania from fiscal year (FY) 2002 to 2012. Primary THR surgery cases were identified using the International Classification of Diseases, Ninth Revision (ICD-9) code 81.51. Only adults who identified as AA or white were included in the study. Exclusion criteria were as follows: unknown gender or insurance status, bilateral hip replacement, death on the same day of THR surgery or during hospitalization, transfer to a different acute care hospital or to a nonstudy destination, hip revision or knee replacement/revision during the same hospitalization, >2 previous THR, and negative calculated readmission time from hospital discharge (from likely administrative data set error).
The eligibility criteria for inpatient rehabilitation were revised by CMS in 2004, resulting in significant shifts in rehabilitation utilization.25 The use of IRF decreased and the use of SNF increased between 2004 and 2007. Trends in the use of rehabilitation services stabilized between 2008 and 2012. Hence, we decided to focus our analysis on the cohort of patients who underwent THR surgery between FY2008 and FY2012 (July 1, 2007, to March 31, 2012). The THRs that occurred prior to FY2008 or during the second quarter of FY2012 (90-day readmission for these cases could not be assessed) were excluded.
Study Variables
Outcome measures
The primary study outcome is type of postsurgical rehabilitation care to which the patient was discharged. Options range from home with routine self-care, home with HH care, SNF, or IRF. Hospital readmission within 90 days by type of postsurgical rehabilitation care destination was also determined.
Exposure variable
Primary exposure of interest was patient race (AA or white).
Study covariates
Patient-level variables included sex, age (<45, 45-54, 55-64, 65-74, 75-84, and ≥85 years), and type of medical insurance (private, Medicaid, Medicare, or other government-sponsored health insurance program). The FY during which the patient underwent THR surgery was determined. Clinical variables included postsurgical complications (ie, thromboembolism, postoperative myocardial infarction, prosthetic device complication, and surgical wound infection) that were ascertained using ICD-9 codes. Clinical comorbidities were identified based on coding algorithms developed by Quan and colleagues26 and supplemented with the methodology recommended by the Agency for Healthcare Research and Quality, versions 2.1 and 3.0-3.7 (Supplement 1).27 In contrast to the previously described study protocol,16 a summation of comorbidities was not used in this study, allowing us to take advantage of all the comorbidity information upon analyzing the data.
Facility-level variables included characteristics of the hospital facility in which patients underwent THR. Metro area status was assigned based on the 2013 US Department of Agriculture’s Rural-Urban Continuum Codes.28 Hospital procedure volume was categorized into 3 levels: <100, 100 to 199, and ≥200 THR procedures per year. The study received an exemption from the institutional review board of Philadelphia Veterans Affairs Medical Center’s (Exempt ID: 01409).
Statistical Analysis
Patient-level and facility-level characteristics, along with clinical outcomes, were compared by patient race. Associations between race and the various patient-level, facility-level, and outcome variables were tested using Wald χ2 from unadjusted binary or multinomial logistic regression models. All models considered race as the independent variable and accounted for clustering by hospital facility.
Using similar strategies, patient-level characteristics, facility-level characteristics, and 90-day hospital readmission were compared by postsurgical discharge destination (considered the independent variable). Patient-level and facility-level characteristics, along with postsurgical discharge destination, were also compared by 90-day hospital readmission status (considered the independent variable). Associations were once again tested using Wald χ2 from unadjusted binary or multinomial logistic regression models that also accounted for clustering by hospital facility.
Unadjusted and adjusted relative risk ratios (aRRRs) of being discharged home with HH care, to a SNF, or to an IRF (vs home with self-care) after THR surgery in AAs compared to whites were estimated using multinomial logistic regression models. Multivariable models adjusted for patient-level and facility-level variables were significantly (P < .10) associated with postsurgical discharge destination based on the bivariate analyses conducted (described in the previous paragraph). Unadjusted and adjusted odds ratios (ORs) of hospital readmission at 90 days were estimated using binary logistic regression models. Multivariable models were adjusted for patient-level and facility-level variables that were significantly (P < .10) associated with 90-day hospital readmission (also described in the previous paragraph).
In all models, patients were stratified by age group (<65 years old and ≥65 years old). The age-based stratification accounts for differences in Medicare eligibility. Data management and analyses were conducted using SAS version 9.4 (SAS Institute, Cary, North Carolina) and Stata version 14.1 (StataCorp LP, College Station, Texas).
Results
Study Sample Characteristics
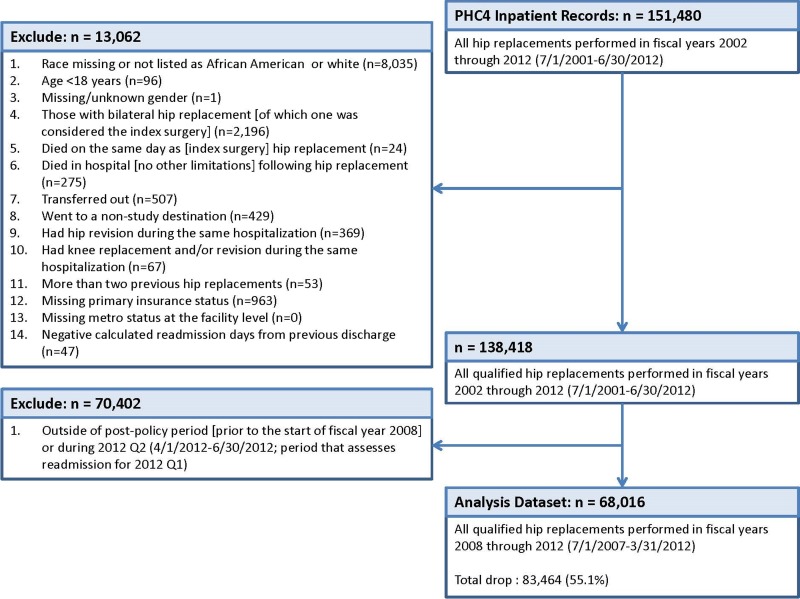
Figure 1 summarizes sample exclusion criteria. Briefly, a total of 151 480 THRs were performed in Pennsylvania between FYs 2002 and 2012. We excluded patients who identified as either non-AA or white and those for whom race identification was missing (n = 8035). We also excluded patients who underwent bilateral hip replacement (n = 2196) and those with unknown medical insurance status (n = 963). Finally, we confined the analysis to those who underwent THR surgery during FYs 2008 and 2012 (n = 68 016).
Figure 1.
Study sample flow diagram.
Table 1 summarizes basic demographic and clinical characteristics of the analytic sample. Among the THR surgery patients analyzed, 63 625 self-identified as white and 4391 self-identified as AA. Among those <65 years, AAs were less likely to have private insurance and more likely to rely on Medicare or Medicaid than whites (P < .001). After age 65, a vast majority (nearly 90%) of both AAs and whites relied on Medicare. AAs were more likely than whites to be admitted into hospitals with ≥200 THR surgeries per year. This was the case for those <65 years (P < .001) as well as among those ≥65 years (P = .019). Complication rates from the procedure were minimal among all patients. Comorbidities such as hypertension, diabetes (uncomplicated), renal failure, and liver disease were more common among AAs than whites (P < .001, all comparisons in both age groups). Other comorbidities including hypothyroidism were more common among white patients compared to AAs (P < .001, both age groups).
Table 1.
Baseline Characteristics and Outcomes by Race and Age Group.a
| <65 Years | ≥65 Years | |||
|---|---|---|---|---|
| WH (n = 28 955) | AA (n = 2937) | WH (n = 34 670) | AA (n = 1454) | |
| Sex, n (%) female | 13 722 (47.4) | 1426 (48.6) | 21 572 (62.2) | 988 (68.0)b |
| Age, n (%)b | ||||
| <45 years | 2858 (9.9) | 521 (17.7) | ||
| 45-54 years | 9304 (32.1) | 1145 (39.0) | ||
| 55-64 years | 16 793 (58.0) | 1271 (43.3) | ||
| 65-74 years | 17 313 (49.9) | 886 (60.9) | ||
| 75-84 years | 14 099 (40.7) | 482 (33.1) | ||
| ≥85 years | 3258 (9.4) | 86 (5.9) | ||
| Insurance type, n (%)b | ||||
| Medicaid | 1707 (5.9) | 795 (27.1) | 46 (0.1) | 18 (1.2) |
| Medicare/government | 3299 (11.4) | 600 (20.4) | 31 066 (89.6) | 1280 (88.0) |
| Private | 23 949 (82.7) | 1542 (52.5) | 3558 (10.3) | 156 (10.7) |
| Metro area (facility level), n (%) | 27 053 (93.4) | 2903 (98.8)b | 31 710 (91.5) | 1447 (99.5)b |
| Fiscal year (FY), n (%) | ||||
| FY2008 (July 01, 2007, to June 30, 2008) | 5315 (18.4) | 533 (18.1) | 6800 (19.6) | 289 (19.9) |
| FY2009 (July 01, 2008, to June 30, 2009) | 5767 (19.9) | 608 (20.7) | 7144 (20.6) | 275 (18.9) |
| FY2010 (July 01, 2009, to June 30, 2010) | 6240 (21.6) | 648 (22.1) | 7565 (21.8) | 298 (20.5) |
| FY2011 (July 01, 2010, to June 30, 2011) | 6455 (22.3) | 656 (22.3) | 7358 (21.2) | 311 (21.4) |
| FY2012 (July 01, 2011, to March 31, 2012) | 5178 (17.9) | 492 (16.8) | 5803 (16.7) | 281 (19.3) |
| Volume of cases (by facility and fiscal year), n (%)d | ||||
| <100/year | 5684 (19.6) | 766 (26.1) | 8655 (25.0) | 366 (25.2) |
| 100 to 199/year | 7725 (26.7) | 434 (14.8) | 10 699 (30.9) | 240 (16.5) |
| 200+/year | 15 546 (53.7) | 1737 (59.1) | 15 316 (44.2) | 848 (58.3) |
| Complications, n (%) | ||||
| Venous thromboembolism | 107 (0.4) | 18 (0.6)c | 215 (0.6) | 20 (1.4)c |
| Postoperative myocardial infarction | 10 (<0.1) | 0 (0.0) | 85 (0.2) | 1 (0.1) |
| Prosthetic device complication | 136 (0.5) | 25 (0.9)c | 441 (1.3) | 8 (0.6)c |
| Surgical wound infection | 57 (0.2) | 6 (0.2) | 79 (0.2) | 6 (0.4) |
| Comorbidities, n (%) | ||||
| Congestive heart failure | 398 (1.4) | 79 (2.7)b | 1595 (4.6) | 99 (6.8)c |
| Cardiac arrhythmias | 1874 (6.5) | 216 (7.4) | 5534 (16.0) | 153 (10.5)b |
| Valvular disease | 672 (2.3) | 47 (1.6)c | 1863 (5.4) | 75 (5.2) |
| Pulmonary circulation disorders | 136 (0.5) | 38 (1.3)b | 438 (1.3) | 27 (1.9)c |
| Peripheral vascular disorders | 267 (0.9) | 25 (0.9) | 1121 (3.2) | 44 (3.0) |
| Hypertension | 13 501 (46.6) | 1632 (55.6)b | 22 020 (63.5) | 1051 (72.3)b |
| Paralysis | 96 (0.3) | 13 (0.4) | 141 (0.4) | 8 (0.6) |
| Other neurological disorders | 813 (2.8) | 80 (2.7) | 1294 (3.7) | 36 (2.5)c |
| Chronic pulmonary disease | 3729 (12.9) | 581 (19.8)b | 5028 (14.5) | 242 (16.6) |
| Diabetes, uncomplicated | 2877 (9.9) | 452 (15.4)b | 5514 (15.9) | 333 (22.9)b |
| Diabetes, complicated | 260 (0.9) | 36 (1.2) | 518 (1.5) | 39 (2.7)b |
| Hypothyroidism | 2868 (9.9) | 97 (3.3)b | 5861 (16.9) | 121 (8.3)b |
| Renal failure | 410 (1.4) | 118 (4.0)b | 1727 (5.0) | 135 (9.3)b |
| Liver disease | 405 (1.4) | 81 (2.8)b | 211 (0.6) | 21 (1.4)b |
| Peptic ulcer disease excluding bleeding | 106 (0.4) | 12 (0.4) | 215 (0.6) | 8 (0.6) |
| AIDS/HIV | 32 (0.1) | 31 (1.1)b | 0 (0.0) | 0 (0.0) |
| Lymphoma | 95 (0.3) | 8 (0.3) | 164 (0.5) | 7 (0.5) |
| Metastatic cancer | 89 (0.3) | 11 (0.4) | 135 (0.4) | 7 (0.5) |
| Solid tumor (without metastasis) | 84 (0.3) | 7 (0.2) | 255 (0.7) | 9 (0.6) |
| Rheumatoid arthritis/collagen vascular | 1006 (3.5) | 174 (5.9)b | 1297 (3.7) | 57 (3.9) |
| Coagulopathy | 439 (1.5) | 51 (1.7) | 737 (2.1) | 30 (2.1) |
| Obesity | 5363 (18.5) | 594 (20.2) | 3483 (10.0) | 192 (13.2)c |
| Weight loss | 82 (0.3) | 11 (0.4) | 226 (0.7) | 9 (0.6) |
| Fluid and electrolyte disorders | 1623 (5.6) | 223 (7.6)c | 3431 (9.9) | 128 (8.8) |
| Blood loss anemia | 416 (1.4) | 56 (1.9) | 665 (1.9) | 27 (1.9) |
| Deficiency anemia | 320 (1.1) | 60 (2.0)b | 671 (1.9) | 52 (3.6)b |
| Alcohol abuse | 649 (2.2) | 82 (2.8) | 227 (0.7) | 12 (0.8) |
| Drug abuse | 268 (0.9) | 119 (4.1)b | 220 (0.6) | 12 (0.8) |
| Psychoses | 104 (0.4) | 34 (1.2)b | 131 (0.4) | 11 (0.8)c |
| Depression | 4120 (14.2) | 315 (10.7)b | 3223 (9.3) | 94 (6.5)c |
| Discharge facility type, n (%)b | ||||
| Inpatient rehab facility (IRF) | 1604 (5.5) | 344 (11.7) | 6161 (17.8) | 210 (14.4) |
| Skilled nursing facility (SNF) | 3449 (11.9) | 830 (28.3) | 11 600 (33.5) | 787 (54.1) |
| Home health care | 17 639 (60.9) | 1397 (47.6) | 13 053 (37.6) | 380 (26.1) |
| Home self-care | 6263 (21.6) | 366 (12.5) | 3856 (11.1) | 77 (5.3) |
| 90-day readmission, n (%) | 2724 (9.4) | 467 (15.9)b | 5439 (15.7) | 289 (19.9)c |
Abbreviations: AA, African American; WH, white.
aVariables were compared by race for each age group (<65 vs ≥65 years) using Wald χ2 test from unadjusted binary or multinomial logistic regression models that account for clustering by facility.
b P < .001.
c P < .05.
db (for <65 years) and c (for ≥65 years).
Most patients who underwent THR were discharged home with HH care. In both age groups, AAs were significantly less likely than whites to be discharged home either with or without HH care (P < .001, comparisons in both age groups). The AAs were more likely than whites to be sent to a SNF (28.3% vs 11.9% among those <65 years old; 54.1% vs 33.5% among those ≥65 years old). Among patients <65 years, AAs were more likely than whites to be sent to an IRF (11.7% vs 5.5%), but the opposite was true among those who were at least 65 years (14.4% vs 17.8%).
Characteristics by Discharge Destination: <65 Years Versus ≥65 Years
Tables 2 and 3 summarizes baseline characteristics by discharge destination. Among patients younger than 65 years, higher proportions of females than males were discharged to IRFs and SNFs. On the other hand, higher proportions of males than females were discharged home (P < .001). Most relied on private medical insurance, especially among those who were discharged home with (84.5%) or without (83.3%) HH care (P < .001). Patients sent home were most likely to have been treated in facilities with ≥200 THR cases per year (P < .001). Surgical complication rates were slightly more common among those discharged to IRFs and SNFs compared to those who were discharged home (P < .001, venous thromboembolism and prosthetic device complication). Comorbidities including hypertension, chronic pulmonary disease, diabetes mellitus, obesity, and depression were more common among those discharged to IRFs and SNFs than among those who were sent home (P < .001, all comparisons).
Table 2.
Characteristics by Discharge Destination of THR Recipients <65 Years.a
| IRF (n = 1948) | SNF (n = 4279) | Home Health Care (n = 19 036) | Home Self-Care (n = 6629) | |
|---|---|---|---|---|
| 90-day readmission, n (%) | 583 (29.9) | 695 (16.2) | 1447 (7.6) | 466 (7.0)b |
| Race, n (%) African American | 344 (17.7) | 830 (19.4) | 1397 (7.3) | 366 (5.5)b |
| Sex, n (%) female | 1102 (56.6) | 2540 (59.4) | 8671 (45.6) | 2835 (42.8)b |
| Age, n (%)b | ||||
| <45 years | 206 (10.6) | 253 (5.9) | 2101 (11.0) | 819 (12.4) |
| 45-54 years | 600 (30.8) | 1172 (27.4) | 6370 (33.5) | 2307 (34.8) |
| 55-64 years | 1142 (58.6) | 2854 (66.7) | 10 565 (55.5) | 3503 (52.8) |
| Insurance type, n (%)b | ||||
| Medicaid | 312 (16.0) | 589 (13.8) | 1098 (5.8) | 503 (7.6) |
| Medicare/government | 563 (28.9) | 880 (20.6) | 1855 (9.7) | 601 (9.1) |
| Private | 1073 (55.1) | 2810 (65.7) | 16 083 (84.5) | 5525 (83.3) |
| Metro area (facility level), n (%) | 1784 (91.6) | 4055 (94.8) | 18 283 (96.0) | 5834 (88.0) |
| Fiscal year (FY), n (%)b | ||||
| FY2008 (July 01, 2007, to June 30, 2008) | 513 (26.3) | 717 (16.8) | 3119 (16.4) | 1499 (22.6) |
| FY2009 (July 01, 2008, to June 30, 2009) | 406 (20.8) | 853 (19.9) | 3849 (20.2) | 1267 (19.1) |
| FY2010 (July 01, 2009, to June 30, 2010) | 389 (20.0) | 962 (22.5) | 4247 (22.3) | 1290 (19.5) |
| FY2011 (July 01, 2010, to June 30, 2011) | 378 (19.4) | 978 (22.9) | 4355 (22.9) | 1400 (21.1) |
| FY2012 (July 01, 2011, to March 31, 2012) | 262 (13.4) | 769 (18.0) | 3466 (18.2) | 1173 (17.7) |
| Volume of cases (by facility and fiscal year), n (%)b | ||||
| <100/year | 693 (35.6) | 1153 (26.9) | 3618 (19.0) | 986 (14.9) |
| 100 to 199/year | 411 (21.1) | 984 (23.0) | 4804 (25.2) | 1960 (29.6) |
| 200+/year | 844 (43.3) | 2142 (50.1) | 10 614 (55.8) | 3683 (55.6) |
| Complications, n (%) | ||||
| Venous thromboembolism | 24 (1.2) | 24 (0.6) | 63 (0.3) | 14 (0.2)b |
| Postoperative myocardial infarction | 3 (0.2) | 1 (<0.1) | 2 (<0.1) | 4 (0.1)c |
| Prosthetic device complication | 23 (1.2) | 43 (1.0) | 74 (0.4) | 21 (0.3)b |
| Surgical wound infection | 7 (0.4) | 16 (0.4) | 31 (0.2) | 9 (0.1)c |
| Comorbidities, n (%) | ||||
| Congestive heart failure | 77 (4.0) | 118 (2.8) | 221 (1.2) | 61 (0.9)b |
| Cardiac arrhythmias | 173 (8.9) | 348 (8.1) | 1220 (6.4) | 349 (5.3)b |
| Valvular disease | 44 (2.3) | 133 (3.1) | 406 (2.1) | 136 (2.1)c |
| Pulmonary circulation disorders | 27 (1.4) | 35 (0.8) | 93 (0.5) | 19 (0.3)b |
| Peripheral vascular disorders | 28 (1.4) | 55 (1.3) | 159 (0.8) | 50 (0.8)c |
| Hypertension | 970 (49.8) | 2255 (52.7) | 8976 (47.2) | 2932 (44.2)b |
| Paralysis | 50 (2.6) | 26 (0.6) | 27 (0.1) | 6 (0.1)b |
| Other neurological disorders | 138 (7.1) | 178 (4.2) | 415 (2.2) | 162 (2.4)b |
| Chronic pulmonary disease | 367 (18.8) | 862 (20.1) | 2330 (12.2) | 751 (11.3)b |
| Diabetes, uncomplicated | 323 (16.6) | 662 (15.5) | 1738 (9.1) | 606 (9.1)b |
| Diabetes, complicated | 55 (2.8) | 64 (1.5) | 127 (0.7) | 50 (0.8)b |
| Hypothyroidism | 223 (11.4) | 492 (11.5) | 1678 (8.8) | 572 (8.6)c |
| Renal failure | 75 (3.9) | 123 (2.9) | 249 (1.3) | 81 (1.2)b |
| Liver disease | 44 (2.3) | 110 (2.6) | 231 (1.2) | 101 (1.5)b |
| Peptic ulcer disease excluding bleeding | 16 (0.8) | 20 (0.5) | 66 (0.3) | 16 (0.2)b |
| AIDS/HIV | 6 (0.3) | 21 (0.5) | 29 (0.2) | 7 (0.1)b |
| Lymphoma | 17 (0.9) | 21 (0.5) | 43 (0.2) | 22 (0.3)b |
| Metastatic cancer | 19 (1.0) | 19 (0.4) | 50 (0.3) | 12 (0.2)b |
| Solid tumor (without metastasis) | 13 (0.7) | 14 (0.3) | 52 (0.3) | 12 (0.2)c |
| Rheumatoid arthritis/collagen vascular | 152 (7.8) | 205 (4.8) | 620 (3.3) | 203 (3.1)b |
| Coagulopathy | 47 (2.4) | 84 (2.0) | 275 (1.4) | 84 (1.3)c |
| Obesity | 508 (26.1) | 1059 (24.7) | 3182 (16.7) | 1208 (18.2)b |
| Weight loss | 23 (1.2) | 28 (0.7) | 35 (0.2) | 7 (0.1)b |
| Fluid and electrolyte disorders | 179 (9.2) | 359 (8.4) | 982 (5.2) | 326 (4.9)b |
| Blood loss anemia | 39 (2.0) | 83 (1.9) | 297 (1.6) | 53 (0.8)b |
| Deficiency anemia | 36 (1.8) | 83 (1.9) | 206 (1.1) | 55 (0.8)b |
| Alcohol abuse | 53 (2.7) | 126 (2.9) | 398 (2.1) | 154 (2.3) |
| Drug abuse | 36 (1.8) | 99 (2.3) | 179 (0.9) | 73 (1.1)c |
| Psychoses | 21 (1.1) | 55 (1.3) | 50 (0.3) | 12 (0.2)b |
| Depression | 366 (18.8) | 799 (18.7) | 2469 (13.0) | 801 (12.1)b |
Abbreviations: IRF, inpatient rehab facility; SNF, skilled nursing facility.
aVariables were compared by discharge destination using Wald χ2 test from unadjusted binary or multinomial logistic regression models that also accounted for clustering by hospital facility.
b P < .001.
c P < .05.
Table 3.
Characteristics by Discharge Destination of THR Recipients ≥65 Years.a
| IRF (n = 6371) | SNF (n = 12 387) | Home Health Care (n = 13 433) | Home Self-Care (n = 3933) | |
|---|---|---|---|---|
| 90-day readmission, n (%) | 2137 (33.5) | 2082 (16.8) | 1166 (8.7) | 343 (8.7)b |
| Race, n (%) African American | 210 (3.3) | 787 (6.4) | 380 (2.8) | 77 (2.0)b |
| Sex, n (%) female | 4372 (68.6) | 8792 (71.0) | 7374 (54.9) | 2022 (51.4)b |
| Age, n (%)b | ||||
| 65-74 years | 2182 (34.2) | 4631 (37.4) | 8775 (65.3) | 2611 (66.4) |
| 75-84 years | 2906 (45.6) | 6132 (49.5) | 4348 (32.4) | 1195 (30.4) |
| ≥85 years | 1283 (20.1) | 1624 (13.1) | 310 (2.3) | 127 (3.2) |
| Insurance type, n (%)b | ||||
| Medicaid | 14 (0.2) | 31 (0.3) | 16 (0.1) | 3 (0.1) |
| Medicare/government | 6000 (94.2) | 11 362 (91.7) | 11 638 (86.6) | 3346 (85.1) |
| Private | 357 (5.6) | 994 (8.0) | 1779 (13.2) | 584 (14.8) |
| Metro area (facility level), n (%) | 5617 (88.2) | 11 497 (92.8) | 12 717 (94.7) | 3326 (84.6)c |
| Fiscal year (FY), n (%)b | ||||
| FY2008 (July 01, 2007, to June 30, 2008) | 1616 (25.4) | 2391 (19.3) | 2260 (16.8) | 822 (20.9) |
| FY2009 (July 01, 2008, to June 30, 2009) | 1400 (22.0) | 2628 (21.2) | 2630 (19.6) | 761 (19.3) |
| FY2010 (July 01, 2009, to June 30, 2010) | 1312 (20.6) | 2737 (22.1) | 3004 (22.4) | 810 (20.6) |
| FY2011 (July 01, 2010, to June 30, 2011) | 1170 (18.4) | 2617 (21.1) | 3087 (23.0) | 795 (20.2) |
| FY2012 (July 01, 2011, to March 31, 2012) | 873 (13.7) | 2014 (16.3) | 2452 (18.3) | 745 (18.9) |
| Volume of cases (by facility and fiscal year), n (%)b | ||||
| <100/year | 2219 (34.8) | 3609 (29.1) | 2659 (19.8) | 534 (13.6) |
| 100 to 199/year | 1932 (30.3) | 3535 (28.5) | 4074 (30.3) | 1398 (35.5) |
| 200+/year | 2220 (34.8) | 5243 (42.3) | 6700 (49.9) | 2001 (50.9) |
| Complications, n (%) | ||||
| Venous thromboembolism | 46 (0.7) | 106 (0.9) | 65 (0.5) | 18 (0.5)c |
| Postoperative myocardial infarction | 26 (0.4) | 35 (0.3) | 15 (0.1) | 10 (0.3)c |
| Prosthetic device complication | 139 (2.2) | 233 (1.9) | 61 (0.5) | 16 (0.4)b |
| Surgical wound infection | 18 (0.3) | 50 (0.4) | 13 (0.1) | 4 (0.1)b |
| Comorbidities, n (%) | ||||
| Congestive heart failure | 424 (6.7) | 843 (6.8) | 332 (2.5) | 95 (2.4)b |
| Cardiac arrhythmias | 1227 (19.3) | 2281 (18.4) | 1681 (12.5) | 498 (12.7)b |
| Valvular disease | 427 (6.7) | 776 (6.3) | 575 (4.3) | 160 (4.1)b |
| Pulmonary circulation disorders | 121 (1.9) | 194 (1.6) | 121 (0.9) | 29 (0.7)b |
| Peripheral vascular disorders | 239 (3.8) | 476 (3.8) | 365 (2.7) | 85 (2.2)b |
| Hypertension | 4067 (63.8) | 7902 (63.8) | 8670 (64.5) | 2432 (61.8) |
| Paralysis | 63 (1.0) | 61 (0.5) | 17 (0.1) | 8 (0.2)b |
| Other neurological disorders | 341 (5.4) | 602 (4.9) | 307 (2.3) | 80 (2.0)b |
| Chronic pulmonary disease | 1019 (16.0) | 2072 (16.7) | 1714 (12.8) | 465 (11.8)b |
| Diabetes, uncomplicated | 1180 (18.5) | 2220 (17.9) | 1898 (14.1) | 549 (14.0)b |
| Diabetes, complicated | 167 (2.6) | 210 (1.7) | 144 (1.1) | 36 (0.9)b |
| Hypothyroidism | 1204 (18.9) | 2275 (18.4) | 1940 (14.4) | 563 (14.3)b |
| Renal failure | 435 (6.8) | 803 (6.5) | 472 (3.5) | 152 (3.9)b |
| Liver disease | 52 (0.8) | 81 (0.7) | 78 (0.6) | 21 (0.5) |
| Peptic ulcer disease excluding bleeding | 44 (0.7) | 80 (0.6) | 76 (0.6) | 23 (0.6) |
| AIDS/HIV | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Lymphoma | 51 (0.8) | 66 (0.5) | 46 (0.3) | 11 (0.3)c |
| Metastatic cancer | 43 (0.7) | 55 (0.4) | 35 (0.3) | 9 (0.2)b |
| Solid tumor (without metastasis) | 63 (1.0) | 104 (0.8) | 79 (0.6) | 18 (0.5)c |
| Rheumatoid arthritis/collagen vascular | 296 (4.6) | 512 (4.1) | 431 (3.2) | 115 (2.9)b |
| Coagulopathy | 160 (2.5) | 297 (2.4) | 235 (1.7) | 75 (1.9)c |
| Obesity | 624 (9.8) | 1264 (10.2) | 1310 (9.8) | 477 (12.1) |
| Weight loss | 50 (0.8) | 136 (1.1) | 37 (0.3) | 12 (0.3)b |
| Fluid and electrolyte disorders | 775 (12.2) | 1558 (12.6) | 921 (6.9) | 305 (7.8)b |
| Blood loss anemia | 147 (2.3) | 281 (2.3) | 226 (1.7) | 38 (1.0)c |
| Deficiency anemia | 157 (2.5) | 333 (2.7) | 173 (1.3) | 60 (1.5)b |
| Alcohol abuse | 53 (0.8) | 82 (0.7) | 78 (0.6) | 26 (0.7) |
| Drug abuse | 58 (0.9) | 119 (1.0) | 44 (0.3) | 11 (0.3)b |
| Psychoses | 39 (0.6) | 81 (0.7) | 15 (0.1) | 7 (0.2)b |
| Depression | 630 (9.9) | 1350 (10.9) | 1048 (7.8) | 289 (7.3)b |
Abbreviations: IRF, inpatient rehab facility; SNF, skilled nursing facility.
aVariables were compared by discharge destination using Wald χ2 test from unadjusted binary or multinomial logistic regression models that also accounted for clustering by hospital facility.
b P < .001.
c P < .05.
For patients who are Medicare eligible (65 or older), significantly higher proportions of females than males were also discharged to IRFs and SNFs (P < .001). More than 85% of these THR recipients had Medicare insurance, but those who were discharged home with (13.2%) or without (14.8%) home care were more likely to have private insurance than those discharged to an IRF (5.6%) or a SNF (8.0%) (P < .001). Complications such as prosthetic device malfunction and comorbidities including cardiac arrhythmias, chronic pulmonary disease, diabetes, hypothyroidism, renal failure, and electrolyte disorders were more commonly seen in patients sent to IRFs and SNFs than in patients who were sent home (P < .001, all comparisons).
Race and Discharge Destination: Unadjusted and Adjusted Analyses
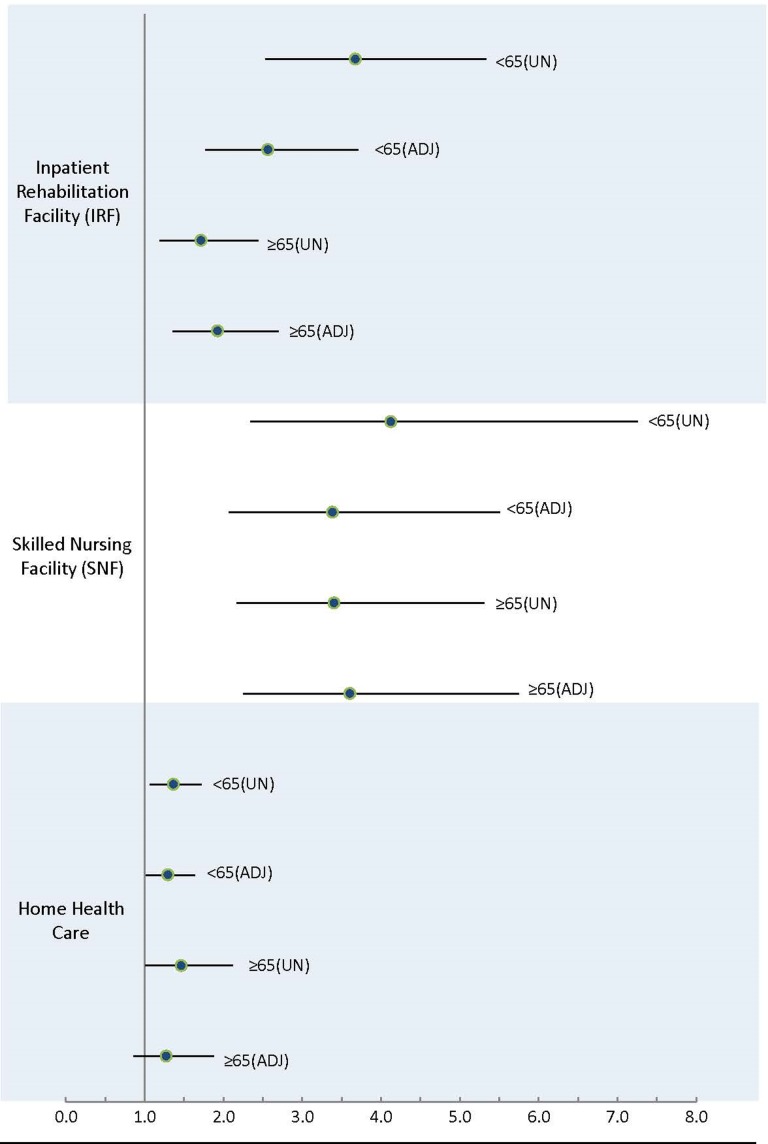
Figure 2 summarizes the adjusted and unadjusted associations between race and discharge destination after THR surgery. Briefly, among patients younger than 65 years, AAs, compared to whites, were more likely to be discharged to an IRF (unadjusted RRR: 3.67, 95% confidence interval [CI]: 2.53-5.33) or to a SNF (unadjusted RRR: 4.12, 95% CI: 2.34-7.26) instead of being sent home with self-care. After adjustment for sex, age, insurance type, facility metropolitan status, FY, volume of cases, complications, and multiple comorbidities, these relationships remained statistically significant (aRRR: 2.56, 95% CI: 1.77-3.71; aRRR: 3.37, 95% CI: 2.07-5.49, respectively).
Figure 2.
Unadjusted (UN) and adjusted (ADJ) relative risk ratios of referral to an inpatient rehabilitation facility (IRF), skilled nursing facility (SNF), and home health care (vs home self-care) in African Americans (vs whites) by age group (<65 and ≥65 years, respectively). In the analysis of total hip replacement (THR) recipients <65 years, the adjusted models include all covariates of interest from Tables 2 and 3 with P < .10. In the analysis of those ≥65 years, the adjusted models include all covariates of interest from Tables 2 and 3 with P < .10.
Among THR recipients ≥65 years, AA race was also significantly associated with being discharged to an IRF (unadjusted RRR: 1.71, 95% CI: 1.19-2.44), a SNF (unadjusted RRR: 3.40, 95% CI: 2.17-5.31), or HH care (unadjusted RRR: 1.46, 95% CI: 1.00-2.12) rather than being discharged home with self-care. After adjustment for multiple sociodemographic and clinical variables (Figure 2), the first 2 of these relationships remained statistically significant (IRF—aRRR: 1.96, 95% CI: 1.39-2.76, respectively; SNF—aRRR: 3.66, 95% CI: 2.29-5.84, respectively). However, after adjustment, there was no longer a statistically significant association between patient race and risk of being sent home with HH care compared to being sent home with self-care (aRRR: 1.29, 95% CI: 0.87-1.92).
Race and Acute Care Hospital Readmissions Within 90 Days of Discharge
Supplement 2 shows the patient-level and facility-level characteristics by 90-day hospital readmission status of both age groups. AA patients, compared to white patients, were more likely to be readmitted to an acute care hospital within 90 days regardless of age group (adjusted OR: 1.13, 95% CI: 1.01-1.28, among those <65 years old; adjusted OR: 1.31, 95% CI: 1.10-1.56, among those ≥65 years old). The odds of readmission to an acute care hospital within 90 days were higher among those discharged to IRFs (<65 years old—adjusted OR: 4.06, 95% CI: 3.49-4.74; ≥65 years old—adjusted OR: 4.32, 95% CI: 3.67-5.09) and SNFs (<65 years old—adjusted OR: 2.05, 95% CI: 1.70-2.46; ≥65 years old—adjusted OR: 1.74, 95% CI: 1.46-2.07) compared to those discharged home with self-care. There were no significant differences in hospital readmission between those discharged home with and without HH care in either age stratification (<65 years old—adjusted OR: 1.09, 95% CI: 0.99-1.21; ≥65 years old—adjusted OR: 1.00, 95% CI: 0.85-1.16).
Discussion
Our study is the first to demonstrate race differences in postacute rehabilitation destination among THR surgery recipients in the state of Pennsylvania. In this large sample of patients, we found that AAs, in comparison to whites, had a significantly higher risk of being discharged to a SNF or IRF rather than being discharged home with self-care. In this study, we also adequately controlled for patient sociodemographic characteristics, clinical comorbidities, surgical complications, and hospital facility characteristics. We found that racial differences in PARC destination persisted even after controlling for these important confounders. We also found that patients discharged to a SNF or IRF have higher risks of readmission to an acute care hospital within 90 days of discharge following THR surgery.
Our findings compare with those from other studies. For example, Ottenbacher et al14 reported that AAs, compared to whites, were more likely to receive inpatient rehabilitation after undergoing lower extremity replacement surgery. Similarly, Freburger et al15 found that racial minorities living in Arizona and New Jersey were more likely to use SNF care relative to whites. In that study, racial minority patients, compared to white patients, were less likely to receive HH care. Finally, a study using data from California hospitals found that among patients who underwent THR surgery, AA patients were more likely to be discharged to a SNF/IRF or to be sent home with HH care than to be sent home without HH.17
Finding a higher risk of hospital readmission after discharge to either an IRF or SNF is also consistent with the literature. For instance, Bini et al29 reported higher risk of 90-day readmission to an acute care hospital among total knee or hip arthroplasty patients who were discharged to a SNF compared to those were discharged home. Several other studies reported a greater risk of 30-day or 90-day hospital readmission among patients discharged to a SNF following joint replacement surgery.19-23 Our own analysis of the PHC4 database showed a higher risk of 30-day readmission to an acute care hospital following knee replacement surgery.16 There is also some evidence that discharge to an IRF instead of home also increases the risk of hospital readmission, albeit the results are conflicting.19-23
There are several reasons that could explain the higher risk of 90-day acute care hospital readmission among patients discharged to a SNF or an IRF.20,21 Debilitated and medically complex patients are more likely to be sent to a SNF or IRF than home. Patients with lower social support or more dysfunctional home setting may also be more likely to be admitted to inpatient rehabilitation facilities (ie, a SNF or IRF). What happens to patients who are admitted to either facility may also influence the odds of acute care hospital readmission. For example, patients are often monitored closely by rehabilitation personnel, thus potentially increasing the odds of identifying reasons for transfer to acute care hospital. The institutional ease of transporting patients back to the hospital from an IRF may also lower the threshold for transfer to an acute care hospital.
There are important limitations to consider in interpreting our findings. First, the study included only THR surgery recipients from the state of Pennsylvania and results may not be generalizable to other states. However, the similarity of our findings to those conducted in other states is reassuring.14,15,17 Second, the data set does not adequately capture other patient variables such as social support, which could vary by race and impact discharge destination decision-making.30-32 Geographical proximity to an IRF or SNF17,33 and patient preference for PARC34 may also influence discharge destination planning but are not available in this data set. Third, although THR for the management of end-stage hip OA is an elective treatment, we have no good data on baseline patient functional status that may potentially vary by race.
In summary, among patients who underwent primary THR surgery in the state of Pennsylvania, AAs, in comparison to white patients, had significantly higher risks of being discharged to a SNF or IRF. These racial differences persisted even after controlling for patient sociodemographic characteristics, clinical comorbidities, surgical complications, and hospital facility characteristics. We also found that patients discharged to a SNF or IRF had a greater chance of being readmitted to an acute care hospital within 90 days following THR surgery. Future studies should evaluate patient-level and health-care system reasons for these variations in postsurgical rehabilitation care.
Supplementary Material
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr Ibrahim is supported in part by the National Institute of Health (NIH)/National Institute of Arthritis and Musculoskeletal and Skin diseases (NIAMS) grant, #K24AR055259. Dr Vina is a recipient of the NIH/NIAMS K23 grant, #K23AR067226.
ORCID iD: Ernest R. Vina, MD, MS http://orcid.org/0000-0001-8135-1731
Supplemental Material: Supplementary material for this article is available online.
References
- 1. Wolford ML, Palso K, Bercovitz A. Hospitalization for total hip replacement among inpatients aged 45 and over: United States, 2000-2010. NCHS Data Brief. 2015;(186):1–8. [PubMed] [Google Scholar]
- 2. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. [DOI] [PubMed] [Google Scholar]
- 3. Pivec R, Johnson AJ, Mears SC, Mont MA. Hip arthroplasty. Lancet. 2012;380(9855):1768–1777. [DOI] [PubMed] [Google Scholar]
- 4. Baron JA, Barrett J, Katz JN, Liang MH. Total hip arthroplasty: use and select complications in the US Medicare population. Am J Public Health. 1996;86(1):70–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hoaglund FT, Oishi CS, Gialamas GG. Extreme variations in racial rates of total hip arthroplasty for primary coxarthrosis: a population-based study in San Francisco. Ann Rheum Dis. 1995;54(2):107–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Escalante A, Espinosa-Morales R, del Rincon I, Arroyo RA, Older SA. Recipients of hip replacement for arthritis are less likely to be Hispanic, independent of access to health care and socioeconomic status. Arthritis Rheum. 2000;43(2):390–399. [DOI] [PubMed] [Google Scholar]
- 7. Bang H, Chiu YL, Memtsoudis SG, et al. Total hip and total knee arthroplasties: trends and disparities revisited. Am J Orthop (Belle Mead NJ). 2010;39(9):E95–E102. [PubMed] [Google Scholar]
- 8. Sharkness CM, Hamburger S, Moore RM, Jr, Kaczmarek RG. Prevalence of artificial hip implants and use of health services by recipients. Public Health Rep. 1993;108(1):70–75. [PMC free article] [PubMed] [Google Scholar]
- 9. Mahomed NN, Barrett JA, Katz JN, et al. Rates and outcomes of primary and revision total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2003;85-A(1):27–32. [DOI] [PubMed] [Google Scholar]
- 10. White RH, McCurdy SA, Marder RA. Early morbidity after total hip replacement: rheumatoid arthritis versus osteoarthritis. J Gen Intern Med. 1990;5(4):304–309. [DOI] [PubMed] [Google Scholar]
- 11. Weaver F, Hynes D, Hopkinson W, et al. Preoperative risks and outcomes of hip and knee arthroplasty in the Veterans Health Administration. J Arthroplasty. 2003;18(6):693–708. [DOI] [PubMed] [Google Scholar]
- 12. Lavernia CJ, Alcerro JC, Rossi MD. Fear in arthroplasty surgery: the role of race. Clin Orthop Relat Res. 2010;468(2):547–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lavernia CJ, Alcerro JC, Contreras JS, Rossi MD. Ethnic and racial factors influencing well-being, perceived pain, and physical function after primary total joint arthroplasty. Clin Orthop Relat Res. 2011;469(7):1838–1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ottenbacher KJ, Smith PM, Illig SB, et al. Disparity in health services and outcomes for persons with hip fracture and lower extremity joint replacement. Med Care. 2003;41(2):232–241. [DOI] [PubMed] [Google Scholar]
- 15. Freburger JK, Holmes GM, Ku LJ, Cutchin MP, Heatwole-Shank K, Edwards LJ. Disparities in post-acute rehabilitation care for joint replacement. Arthritis Care Res (Hoboken). 2011;63(7):1020–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jorgenson ES, Richardson DM, Thomasson AM, Nelson CL, Ibrahim SA. Race, rehabilitation, and 30-day readmission after elective total knee arthroplasty. Geriatr Orthop Surg Rehabil. 2015;6(4):303–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schwarzkopf R, Ho J, Snir N, Mukamel DD. Factors influencing discharge destination after total hip arthroplasty: a California state database analysis. Geriatr Orthop Surg Rehabil. 2015;6(3):215–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tian W, DeJong G, Brown M, Hsieh CH, Zamfirov ZP, Horn SD. Looking upstream: factors shaping the demand for postacute joint replacement rehabilitation. Arch Phys Med Rehabil. 2009;90(8):1260–1268. [DOI] [PubMed] [Google Scholar]
- 19. Riggs RV, Roberts PS, Aronow H, Younan T. Joint replacement and hip fracture readmission rates: impact of discharge destination. PM R. 2010;2(9):806–810. [DOI] [PubMed] [Google Scholar]
- 20. Mesko NW, Bachmann KR, Kovacevic D, LoGrasso ME, O’Rourke C, Froimson MI. Thirty-day readmission following total hip and knee arthroplasty—a preliminary single institution predictive model. J Arthroplasty. 2014;29(8):1532–1538. [DOI] [PubMed] [Google Scholar]
- 21. Zmistowski B, Restrepo C, Hess J, Adibi D, Cangoz S, Parvizi J. Unplanned readmission after total joint arthroplasty: rates, reasons, and risk factors. J Bone Joint Surg Am. 2013;95(20):1869–1876. [DOI] [PubMed] [Google Scholar]
- 22. Schairer WW, Sing DC, Vail TP, Bozic KJ. Causes and frequency of unplanned hospital readmission after total hip arthroplasty. Clin Orthop Relat Res. 2014;472(2):464–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ramos NL, Karia RJ, Hutzler LH, Brandt AM, Slover JD, Bosco JA. The effect of discharge disposition on 30-day readmission rates after total joint arthroplasty. J Arthroplasty. 2014;29(4):674–677. [DOI] [PubMed] [Google Scholar]
- 24. Grosso LM, Curtis JP, Lin Z, et al. Hospital-Level Risk-Standardized Readmission Rate Following Elective Primary Total Hip Arthroplasty (THA) and/or Total Knee Arthroplasty (TKA). Centers for Medicare and Medicaid Services; 2012, https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1228772504368. [Google Scholar]
- 25. Centers for Medicare and Medicaid Services. Final rule Medicare program; changes to the criteria for being classified as an inpatient rehabilitation facility. Fed Regist. 2004;69(89):25752–25776. [PubMed] [Google Scholar]
- 26. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. [DOI] [PubMed] [Google Scholar]
- 27. Agency for Healthcare Research and Quality. Comorbidity Software. 3.7 ed Rockville, MD: Agency for Healthcare Research and Quality; 2016. [Google Scholar]
- 28. Rural-Urban Continuum Codes. United States Department of Agriculture Economic Research Services. 2013. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation.aspx.
- 29. Bini SA, Fithian DC, Paxton LW, Khatod MX, Inacio MC, Namba RS. Does discharge disposition after primary total joint arthroplasty affect readmission rates? J Arthroplasty. 2010;25(1):114–117. [DOI] [PubMed] [Google Scholar]
- 30. Munin MC, Kwoh CK, Glynn N, Crossett L, Rubash HE. Predicting discharge outcome after elective hip and knee arthroplasty. Am J Phys Med Rehabil. 1995;74(4):294–301. [DOI] [PubMed] [Google Scholar]
- 31. de Pablo P, Losina E, Phillips CB, et al. Determinants of discharge destination following elective total hip replacement. Arthritis Rheum. 2004;51(6):1009–1017. [DOI] [PubMed] [Google Scholar]
- 32. Vina ER, Cloonan YK, Ibrahim SA, Hannon MJ, Boudreau RM, Kwoh CK. Race, sex, and total knee replacement consideration: role of social support. Arthritis Care Res (Hoboken). 2013;65(7):1103–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bozic KJ, Wagie A, Naessens JM, Berry DJ, Rubash HE. Predictors of discharge to an inpatient extended care facility after total hip or knee arthroplasty. J Arthroplasty. 2006;21(6 suppl 2):151–156. [DOI] [PubMed] [Google Scholar]
- 34. Mahomed NN, Koo Seen Lin MJ, Levesque J, Lan S, Bogoch ER. Determinants and outcomes of inpatient versus home based rehabilitation following elective hip and knee replacement. J Rheumatol. 2000;27(7):1753–1758. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.