Abstract
Purpose:
Excessive blood loss with hip fracture management has been shown to result in increased rates of complications. Our goal is to compare blood loss and transfusion rates between patients with intracapsular and extracapsular (both intertrochanteric (IT) and subtrochanteric (ST)) hip fractures.
Methods:
472 patients were evaluated over a five-year period. Those who presented to the hospital with a proximal femur fracture (femoral neck, IT or ST) were considered for the study. Exclusion criteria included polytrauma, gunshot injuries, periprosthetic fractures, and non-operative management. Primary endpoint was hemoglobin (Hgb) drop from admission to day of surgery (DOS); secondary endpoint was need for pre-op transfusion and discharge location.
Results:
304 patients were analyzed who sustained a proximal femur fracture. Median IC Hgb drop was 0.6g/dL; median EC Hgb drop was 1.1g/dL from admission to DOS (p = 0.0272). Rate of pre-operative transfusions was higher in EC (36/194 = 18.6%) than IC fractures (5/105 = 4.5%) (p = 0.0006), and overall transfusion rates remained higher throughout hospital stay (55.7% EC vs. 32.7% IC; p = 0.0001). Breakdown of bleeding rate and tranfusion rates between IT and ST fractures were not significant (p = 0.07; p = 0.4483). Extracapsular hip fractures were more likely to be discharged to a skilled nursing facility (SNF) (84.4% EC vs. 73.8% IC; p = 0.027).
Conclusion:
Intracapsular hip fractures have significantly less pre-operative blood loss and fewer pre-operative transfusions than their extracapsular counterparts. These findings can be used to establish appropriate pre-operative resuscitative efforts, ensuring that hip fracture protocols account for the increased likelihood of blood loss in extracapsular fractures.
Keywords: hip fractures, anemia, blood loss, intertrochanteric fracture, femoral neck fracture, subtrochanteric fracture
Introduction
Hip fractures in the elderly are common, with more than 250 000 people sustaining hip fractures annually in the United States. The National Osteoporosis Foundation estimates over 500 000 hip fractures will occur annually by 2040.1 Excessive blood loss after long bone fractures has been shown to result in increased complications,2 but current studies have not addressed the fracture pattern which poses the greatest risk of blood loss anemia following injury. If we were able to better identify which fracture patterns have a greater risk for blood loss, resuscitative efforts may be improved and modified in order to minimize morbidity associated with blood loss.
Intracapsular (IC) hip fractures account for 45% of all acute hip fractures, while intertrochanteric (IT) fractures account for an additional 45%.1 For anatomic reasons, historical belief is that IC fractures tend to have a smaller preoperative hemoglobin (Hgb) drop than extracapsular (EC) fractures. In the clinical setting, it is common to see a patient with a hip fracture present with a low postoperative Hgb level that is largely unexplained by the operative blood loss.3 Most of this blood loss is felt to occur preoperatively,4 and up to 80% of this blood loss may be unaccounted for by medical teams.5 Preoperative anemia is a risk factor for perioperative death4 and need for blood transfusions.5–7 Alternatively, higher postoperative Hgbs have been associated with better overall outcomes3 and shorter hospital stays.8
Whereas traditional teaching is that EC hip fractures have more hidden blood loss preoperatively than IC fractures, this difference, the degree of difference, and transfusion rates have not been well studied in the literature. Our goal is to compare blood loss and transfusion rates between patients with IC and EC (IT and subtrochanteric [ST]) hip fractures and assess patients to accurately identify those at risk of perioperative anemia based on fracture type, medical comorbidities, and time to surgery in an effort to minimize any associated complications.
Methods
A retrospective study was performed at a level 1 trauma center over a 5-year period from January 1, 2010, to December 31, 2014, where 472 patients with hip fractures were evaluated. All adult patients (aged 18-98 without an upper limit) who presented to the hospital with a proximal femur fracture (femoral neck, IT, or ST fracture) were considered for this study. An ST femur fracture was considered any fracture within 5 cm of the lesser trochanter per Arbeitsgemeinschaft für Osteosynthesefragen (AO) guidelines. Patients were identified using the current procedural terminology codes 27235, 27236, 27244, and 27245. Exclusion criteria included patients with polytrauma, any patient who had a concomitant lower extremity or pelvic fracture, gunshot injuries, periprosthetic fractures, pathologic fractures, patients with delayed presentation (>24 hours), and fractures treated nonoperatively. Patients who did not have an available electronic medical record (EMR) or were missing key data points (Hgb values, operative note, etc) were also excluded.
Following application of exclusion criteria, we were able to analyze data from 304 patients who sustained either an IC or EC hip fracture. All patients were followed from the time of admission/injury until time of discharge from orthopedic care. Epidemiological information, as well as mechanism (high vs low energy), fracture type, and fixation type were collected. Hemoglobin values were analyzed from admission complete blood count (CBC) taken at the time of initial presentation and then via daily morning (AM) CBC or hemoglobin & hematocrit (H&H)—all AM labs are drawn at 4 am. Additional labs in the form of prothrombin time (PT), partial thromboplastin time (PTT), and international normalized ratio (INR) were used to assess possible risk factors to increased blood loss. The primary end point for the study was Hgb drop from admission to day of surgery (DOS). Secondary end point was a need for preoperative transfusion.
Statistical analysis was undertaken using both parametric (t test and analysis of variance) and nonparametric (Wilcoxon and Kruskal-Wallis) tests. Chi-square analysis was used for need for transfusion and discharge location. Nonparametric analysis was used for Hgb drops from admission to DOS, time to surgery, and Hgb drop in patients receiving transfusion. Statistical significance was defined as a P value < .05.
Results
Four hundred and seventy-two patients received surgical intervention during this time period, of which 168 were excluded due to polytrauma (80), concomitant lower extremity or pelvic fracture (4), gunshot injuries (29), periprosthetic fractures (12), pathologic fractures (10), delayed presentation (>24 hours) (23), and fractures treated nonoperatively (0). Patients who did not have an available EMR (2) or were missing key data points (Hgb values, operative note, etc) were also excluded (8). Majority of patients missing data points (6/8) were due to transfers from outside hospitals where we did not have access to initial labs, or presurgical Hgb was not drawn (2/8). This left 304 patients for statistical analysis. Of these 304 patients, 110 had IC hip fractures and 194 had EC hip fractures. The EC hip fractures were further divided into 168 IT and 26 ST. Per standard hip fracture protocol, admission labs were drawn prior to IV fluid administration, and patients were all started on IV maintenance fluids at midnight of the first hospital day due to being nil per os (NPO) for surgery (even if not medically cleared at the time). All patients received chemical deep venous thrombosis (DVT) prophylaxis at the time of presentation at our institution (lovenox or heparin—depending on renal function). Comorbidities were tracked in all patients (including but not limited to hypertension, hyperlipidemia, bleeding disorders, congestive heart failure, chronic obstructive pulmonary disease, and diabetes mellitus) without statistically significant differences between the groups. No subgroup analysis was performed between different comorbidities. Refer to Table 1 for complete demographic information.
Table 1.
Patient Demographic Data.a
| No. of patients | 304 |
|---|---|
| Age (years) | 74.0 ± 14.4 |
| Gender | |
| Female | 181 (59.5%) |
| Male | 123 (40.5%) |
| Discharge location | |
| SNF/rehab | 241 (79.3%) |
| Home | 58 (19.1%) |
| Unknown | 5 (1.6%) |
| Injury Statistics | |
| Fracture location | |
| Intracapsular | 110 (36.2%) |
| Extracapsular | 194 (63.8%) |
| Extracapsular fracture breakdown | |
| Intertrochanteric | 168 (86.6%) |
| Subtrochanteric | 26 (13.4%) |
aSummary of patient demographic data including age ranges and gender as well as injury statistics including site of injury and fracture classification.
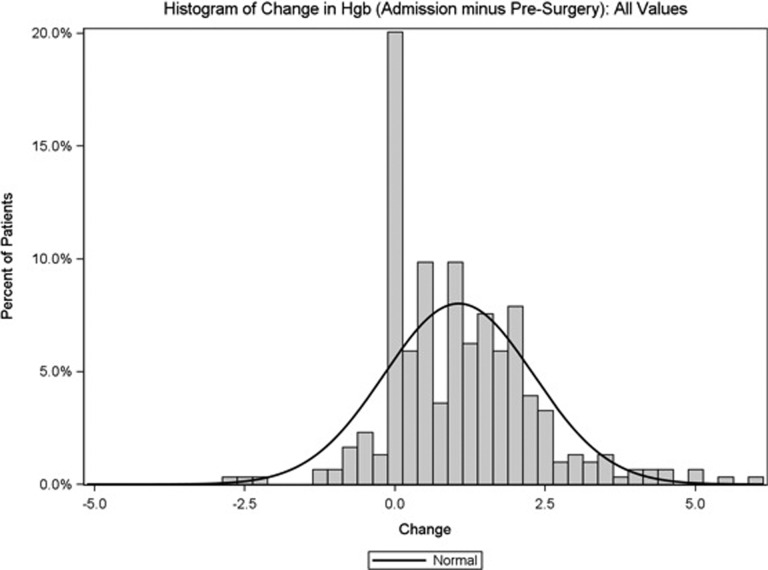
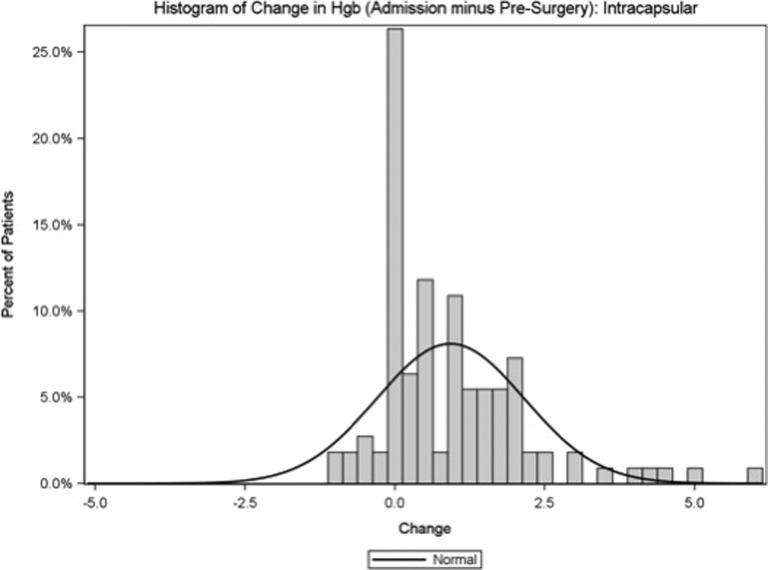
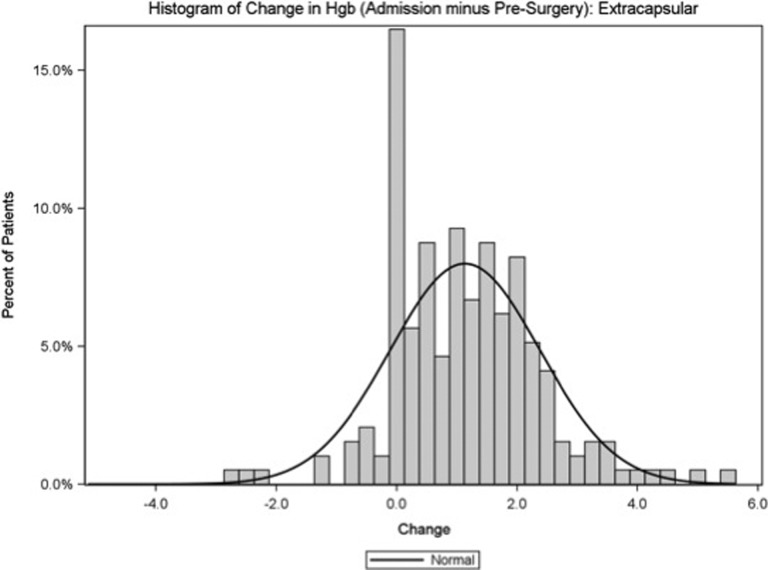
To estimate blood loss, admission Hgb was compared to presurgery Hgb through subtraction of the presurgery Hgb from the admission Hgb. Time to surgery was calculated between the 2 groups and was found to be statistically insignificant (28.8 hours in IC vs 27.5 hours IT and 27.0 hours in ST; P = .716). The Wilcoxon test was used for comparison of the admission Hgb minus the presurgery Hgb for IC vs EC hip fractures. Median IC Hgb drop was 0.6 g/dL, while median EC Hgb drop was 1.1 g/dL from admission to DOS. This was statistically significant with a P value of .0272. This therefore suggests that there is more blood lost from EC hip fractures than IC hip fractures. Further breakdown shows IT Hgb loss (1.12 g/dL) and ST Hgb loss (1.30 g/dL) (P = .07). Refer to Table 2 and Figures 1–3 for complete breakdown of Hgb changes and histogram representation of such changes.
Table 2.
Summary Statistics and Significance Testing for Presurgical Blood Loss for Intracapsular and Extracapsular Fractures.
| Classification Variables | N | Mean | Std Dev | Min | Q1 | Median | Q3 | Max | P Value | Statistical Method |
|---|---|---|---|---|---|---|---|---|---|---|
| Admission Hgb minus presurgery Hgb, by intracapsular | .0238 | Wilcoxon | ||||||||
| Extracapsular | 194 | 1.14 | 1.25 | −2.80 | 0.20 | 1.10 | 1.90 | 5.50 | ||
| Intracapsular | 110 | 0.93 | 1.23 | −1.10 | 0.00 | 0.60 | 1.60 | 5.90 | ||
| Admission Hgb minus presurgery Hgb, by extracapsular | .0709 | Kruskal-Wallis | ||||||||
| IT | 168 | 1.11 | 1.19 | −2.80 | 0.25 | 1.10 | 1.85 | 5.10 | ||
| ST | 26 | 1.30 | 1.59 | −0.50 | 0.00 | 0.80 | 2.00 | 5.50 | ||
| Intracapsular | 110 | 0.93 | 1.23 | −1.10 | 0.00 | 0.60 | 1.60 | 5.90 |
Abbreviations: IT, intertrochanteric; ST, subtrochanteric.
Figure 1.
Histogram representation of the hemoglobin change from admission to date of surgery for all fractures.
Figure 2.
Histogram representation of the hemoglobin change from admission to date of surgery for intracapsular fractures.
Figure 3.
Histogram representation of the hemoglobin change from admission to date of surgery for extracapsular fractures.
The 2 categorical variables (IC and EC) were assessed relative to whether the patient received a blood transfusion preoperatively, and separately throughout their hospital stay. Strict transfusion protocols are adhered to at our institution, and patients are transfused if Hgb <7 mg/dL or <8 mg/dL if symptomatic (tachycardia)—patients are transfused a single unit at a time. There was no change in transfusion practice over the study time frame. Transfusion analysis was conducted using the χ2 test. The rate of preoperative transfusions was significantly higher in EC fractures (36/194 = 18.6%) compared to IC fractures (5/105 = 4.5%) (P = .0006). For the entirety of their hospital stay, 32.7% of patients with IC, (36/110 patients) received a transfusion. In contrast, 55.7% of patients with EC (108/194 patients) received a transfusion (P = .0001). Therefore, we can conclude that not only is the amount of blood loss in EC fractures more significant, but also that the requirement for transfusion is significantly higher in the preoperative period. Further breakdown of transfusion rates in IT (92/168 = 54.8%) and ST fractures (16/26 = 61.5%) was not clinically significant (P = .4483). Refer to Table 3 for a summary of transfusion rate demographics and results.
Table 3.
Demographics, Summary Statistics, and Significance Testing for Transfusion Rates.
| Transfusion Demographics | ||||||
|---|---|---|---|---|---|---|
| Transfusion, n (%) | ||||||
| Yes | 146 (48.0%) | |||||
| No | 158 (52.0%) | |||||
| PRBCs, n (%) | ||||||
| Yes | 144 (47.4%) | |||||
| No | 160 (52.6%) | |||||
| FFP | ||||||
| Yes | 7 (2.3%) | |||||
| No | 297 (97.7%) | |||||
| Platelets | ||||||
| Yes | 4 (1.3%) | |||||
| No | 300 (98.7%) | |||||
| Clinical Significance of Transfusion Rates | ||||||
| Attribute | Transfusion = Yes | Transfusion = No | Total | P Value | Test Method | Significance |
| Preop EC/IC, n (%) | .0006 | Chi-square | Highly significant | |||
| Extracapsular | 36 (18.6%) | 158 (81.4%) | 194 (100.0%) | |||
| Intracapsular | 5 (4.5%) | 105 (95.5%) | 110 (100.0%) | |||
| Total | 41 (13.5%) | 263 (86.5%) | 304 (100.0%) | |||
| Entire hospital stay EC/IC, n (%) | .0001 | Chi-square | Highly significant | |||
| Extracapsular | 108 (55.7%) | 86 (44.3%) | 194 (100.0%) | |||
| Intracapsular | 36 (32.7%) | 74 (67.3%) | 110 (100.0%) | |||
| Total | 144 (47.4%) | 160 (52.6%) | 304 (100.0%) | |||
| IT or ST, n (%) | .4483 | Chi-square | Not significant | |||
| IT | 94 (56.0%) | 74 (44.0%) | 168 (100.0%) | |||
| ST | 16 (61.6%) | 10 (38.4%) | 26 (100.0%) | |||
| Total | 110 (56.7%) | 84 (43.3%) | 194 (100.0%) | |||
Abbreviations: IT, intertrochanteric; ST, subtrochanteric.
Finally, the 2 categorical variables (IC and EC) were assessed for discharge location to determine whether a fracture pattern would be more likely to require further rehab. In all, 84.4% (162/192) of the patients with EC were discharged to a skilled nursing facility (SNF) while only 73.8% (79/107) of the patients with IC were discharged to an SNF (P = .027). Further breakdown of EC fractures shows that 86.7% (144/166) of the patients with IT are discharged to an SNF while only 69.2% (18/26) and 73.8% (79/107) of the ST and patients with IC (respectively) are discharged to an SNF (P = .0096).
Discussion
Hidden blood loss from a fracture after injury and/or following surgery has been a matter of debate. Anemia in the perioperative patient has been shown to produce poorer functional scores and decrease a patient’s ability to walk independently. This, in turn, is theorized to affect their ability to participate in postoperative rehabilitation, further increasing their complications postoperatively.9 A study from Denmark addressing the “hidden” blood loss after hip fracture surgery had unaccounted blood losses anywhere from 547 mL (screws/pins) to 1437 mL (intramedullary hip nail and screw).10 Orthopedic surgeons underestimate the amount of blood loss occurring before and during surgery, and as previously mentioned, up to 80% of this loss may be unaccounted for by medical teams.5 Unfortunately, there are insufficient high-quality studies to inform practitioners in regard to preoperative blood transfusions in IC or EC fractures.11
Studies determining preoperative blood loss between the 2 fracture types are also insufficient to guide clinical practice. Most are extrapolated from studies for different purposes. A study from the UK assessed femoral head blood flow for avascular necrosis between IC and EC hip fractures. They found that a tamponade effect does occur in IC fractures. This was determined by measuring intraosseous pressures in both IC and EC fractures, where it determined an increased intraosseous pressure in the IC fractures was due to the intact capsular tamponade effect.12 This can be extrapolated that this increased intraosseous pressure would also result in a slowing of bleeding and therefore less blood loss. An additional study assessing patients at risk of preoperative blood transfusions in an effort to decrease unnecessary cross matching found pertrochanteric fractures to be an independent risk factor for preoperative transfusions.6
Identifying those patients at risk of excessive bleeding is also important in regard to timing of surgical management. Delays in appropriate resuscitative efforts simply cause a chain reaction in delays further down the line. Up to 44% of delays from 25 to 48 hours after hospitalization to surgery and 42% of delays greater than 48 hours from hospitalization to surgery can be attributed to hematologic abnormalities, most commonly an unacceptable Hgb for surgery. Furthermore, a study by Gdalevich et al showed that delays greater than 48 hours after injury resulted in increased 1-year mortality, mental deterioration, and postoperative mobility.13 However, it is important to note that aggressive transfusion of patients prophylactically or in anticipation of excessive blood loss is also not appropriate. A study by Carson et al examined the outcome differences between transfusing patients at a Hgb <10 vs <8 g/dL, and showed no difference in complication rates, in-hospital mortality, 60-day postoperative mortality or 60-day postoperative rehabilitation outcomes, even in those deemed high cardiovascular risk.14 A study by Nabais et al on patients with acute coronary found that when comparing Hgb drops of <0.8 g/dL to 0.9-1.4 g/dL there was an increase in 6-month mortality rate (8% vs 9.4% P = .014) and 6-month myocardial infarction (MI) rate (12.4% vs 17.0% P = .021). Additionally, they determined that when Hgb was treated as a continuous variable, the hazards ratio for 6-month mortality was 1.16 (95% confidence interval, 1.01-1.32; P = .030) per 1 g/dL increase in Hgb drop.15 Extrapolating that to hip fractures, the Hgb drop experienced by our patients in the EC group (1.1 g/dL) could be deemed significant enough to affect long-term survivability.
With a push for centers to develop geriatric hip fracture programs to better serve patients, information such as this can be invaluable. In recent years, outcomes within geriatric hip fracture protocols have shown vast improvements in complication rates.16 Yet studies have been unable to determine optimal resuscitation protocols due to this gap in blood loss knowledge. Our center feels that a comprehensive and consistent monitoring process is the key to balancing the preoperative Hgb levels. In our experience, drawing H&H labs every 8 hours for the first 48 hours after injury ensures that anemia is caught early and treated promptly, without delaying the operationg room (OR) or transfusing patients unnecessarily. Trends may be followed as well to better understand the hematologic profile of the patient and better anticipate resuscitation demands in the postoperative period. With this new knowledge of the increased risk of blood loss in EC fractures, further research could address the discrepancy in blood loss and how this should shape our resuscitative efforts. Namely, should patients who sustain EC fractures undergo more rigorous monitoring and aggressive resuscitation than their IC counterparts?
There were several limitations to this current study. Due to its retrospective design, data were limited and could only be obtained from what was presented in the medical record. Missing data and inconsistencies could contribute a source of error in data collection. Additionally, since there was some variability in when Hgb blood draws were performed, it is difficult to make a complete comparison. Hemodilution effect is always a concern when using Hgb values as a marker of blood loss. However, our patients all receive a standardized resuscitation protocol (as previously mentioned) through initial maintenance fluids upon admission to the hospital. A study by Grathwohl et al showed that while bolus effects at 1 hour existed, at subsequent 4 and 8 hour Hgb measurements, the hemodilution effect was lost and Hgb values were felt to be a true measure of blood loss. Patients receiving maintenance fluids experienced no hemodilution effect at 1-, 4-, and 8-hour intervals.17 Therefore, it can be assumed that these maintenance fluids had no effect on subsequent lab values. A subgroup analysis was not performed in regard to presence of preinjury blood thinners, and as such these variables may affect results. Aspirin use was included in the blood thinner subset and was accounted for. The number of patients on anticoagulation prior to injury between the two groups was not statistically significant (38.7% EC vs 40.9% IC; P = .6998), therefore unlikely to affect the overall outcomes. Finally, patients who received a transfusion preoperatively were still included in the analysis. Therefore, one could conclude that the blood loss results could be expected to be greater than what is being represented here as artificially elevated posttransfusion, presurgical values were still collected and analyzed.
Conclusion
Our study suggests that IC fractures have significantly less drop in Hgb than EC fractures, which can be correlated to less blood loss. They also are shown to require significantly fewer preoperative blood transfusions than their EC counterparts. These findings should be used to establish appropriate preoperative resuscitative efforts, ensuring that protocols account for the increased likelihood of blood loss in EC fractures. By doing this, we ensure patients are able to undergo surgical fixation in a more appropriate time frame and ensure better outcomes through the postoperative period.
Footnotes
Authors’ Note: Due to the confidential nature of some of the research materials supporting this publication, not all of the data can be made accessible to other researchers. Please contact Katharine D. Harper for more information. All authors listed meet the authorship criteria according to the latest guidelines of the ICMJE and all authors are in agreement with the manuscript.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Saqib Rehman received royalty payments from Jaypee Medical Publishing, was the editor in Elsevier (Orthopaedic Clinics of North America), and speaker of DePuy Synthes. Committee: Orthopaedic Trauma Association.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Bateman L, Vuppala S, Porada P, et al. Medical management in the acute hip fracture patient: a comprehensive review for the internist. Ochsner J. 2012;12(2):101–110. [PMC free article] [PubMed] [Google Scholar]
- 2. Zeideman H, Wray JB, Schneider AJ. Alterations in vascular volume after long bone fracture. Arch Surg. 1963;87:907–911. [DOI] [PubMed] [Google Scholar]
- 3. Kumar D, Mbako AN, Riddick A, Patil S, Williams P. On admission haemoglobin in patients with hip fracture. Injury. 2011;42(2):167–170. doi:10.1016/j.injury.2010.07.239. [DOI] [PubMed] [Google Scholar]
- 4. Smith GH, Tsang J, Molyneux SG, White TO. The hidden blood loss after hip fracture. Injury. 2011;42(2):133–135. doi:10.1016/j.injury.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 5. Zhu XZ, Tao YL, Ma Z. Routine blood tests as predictors of mortality in hip fracture patients. Injury. 2013;44(11):1659. [DOI] [PubMed] [Google Scholar]
- 6. Dillon MF, Collins D, Rice J, Murphy PG, Nicholson P, Mac Elwaine J. Preoperative characteristics identify patients with hip fractures at risk of transfusion. Clin Orthop Relat Res. 2005;439:201–206. doi:00003086-200510000-00035 [pii]. [DOI] [PubMed] [Google Scholar]
- 7. Willems JM, de Craen AJ, Nelissen RG, van Luijt PA, Westendorp RG, Blauw GJ. Haemoglobin predicts length of hospital stay after hip fracture surgery in older patients. Maturitas. 2012;72(3):225–228. doi:10.1016/j.maturitas.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 8. Madsen CM, Jorgensen HL, Norgaard A, et al. Preoperative factors associated with red blood cell transfusion in hip fracture patients. Arch Orthop Trauma Surg. 2014;134(3):375–382. doi:10.1007/s00402-013-1906-3. [DOI] [PubMed] [Google Scholar]
- 9. Foss NB, Kristensen MT, Kehlet H. Anaemia impedes functional mobility after hip fracture surgery. Age and Ageing. 2008;37(2):173–178. doi:10.1093/ageing/afm161. [DOI] [PubMed] [Google Scholar]
- 10. Foss NB, Kehlet H. Hidden blood loss after surgery for hip fracture. J Bone Joint Surg [Br] 2006;88(8):1053–1059. [DOI] [PubMed] [Google Scholar]
- 11. Potter LJ, Doleman B, Moppet IK. A systematic review of pre-operative anemia and blood transfusion in patients with fractured hips. Anaesthesia. 2015;70(4):483–500. [DOI] [PubMed] [Google Scholar]
- 12. Harper WM, Barnes MR, Gregg PJ. Femoral head blood flow in femoral neck fractures: an analysis using intra-osseous pressure measurement. J Bone Joint Surg [Br]. 1991;73(1):73–75. [DOI] [PubMed] [Google Scholar]
- 13. Orosz GM, Hannan EL, Magaziner J, et al. Hip Fracture in the older patient: reasons for delay in hospitalization and timing of surgical repair. J Am Geriatr Soc. 2002;50(8):1336–1340. [DOI] [PubMed] [Google Scholar]
- 14. Gdalevich M, Cohen D, Yosef D, Tauber C. Morbidity and mortality after hip fracture: the impact of operative delay. Arch Orthop Trauma Surg. 2004;124(5):334–340. doi:10.1007/s00402-004-0662-9. [DOI] [PubMed] [Google Scholar]
- 15. Carson JL, Terrin ML, Noveck H, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365(26):2453–2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Grathwohl KW, Bruns BJ, LeBrun CJ, Ohno AK, Dillard TA, Cushner HM. Does hemodilution exist? Effects of saline infusion on hematologic parameters in euvolemic subjects. South Med J. 1996;89(1):51–55. [DOI] [PubMed] [Google Scholar]
- 17. Nabais S, Gaspar A, Costa J, et al. Prognostic impact of hemoglobin drop during hospital stay in patients with acute coronary syndromes. Rev Port Cardiol. 2009;28(4):383–395. [PubMed] [Google Scholar]