Abstract
Background:
Previous research reported the frequency of coronal plane (Hoffa) fractures in high-energy supracondylar femur fractures in a relatively young population. It is the purpose of this study to identify the frequency of coronal plane fractures seen in elderly patients.
Methods:
All patients over the age of 18 years treated for supracondylar femur fractures at 2 level I trauma centers were reviewed over a 4-year period. The patients were stratified (≥60 years and <60 years) and compared to determine differences in injury characteristics and fracture patterns with special attention to the prevalence of coronal plane fractures.
Results:
One hundred ten patients were identified with supracondylar femur fractures (12 Orthopaedic Trauma Association [OTA] 33A; 2 OTA 33B; 96 OTA 33C). Thirty-two of the 96 intercondylar fractures were in patients >60 years of age. The elderly group included a higher percentage of females (81% vs 36%, P = .0001) and was more likely to sustain their injury due to a fall (59% vs 19%, P = .0001). Coronal plane fractures were visualized on computed tomography scans in 56 (58%) of the 96 33C femur fractures. Forty-four percent of elderly patients sustained a coronal plane fracture compared with 66% of the younger cohort (P = .04). The percentage of open fractures (30% elderly vs 46%) was not significantly different between the 2 groups (P = .17).
Conclusions:
The occurrence rate of 44% in this study was higher than expected and is the first to provide this information in the elderly patients on this fracture. It is important that a high index of suspicion be maintained for the Hoffa fracture in all distal femur fractures, regardless of age or mechanism of injury.
Keywords: femur, fracture, elderly, Hoffa, supracondylar
Introduction
First described by Busch in 1869 and later popularized by Albert Hoffa in the first edition of his textbook in 1888, the coronal plane fracture seen in supracondylar femur fractures with intercondylar extension is a unique fracture pattern that requires particular attention.1-4 Coronal plane fractures may be a diagnostic dilemma with routine radiographs. Prior studies have demonstrated that with radiographs alone, only 69% of coronal plane fractures were able to be diagnosed in supracondylar femur fractures.5 Early identification of a Hoffa fragment is critical to choosing the surgical approach and deciding on fixation strategy.
Previous research has reported the frequency of coronal plane (Hoffa) fractures in high-energy supracondylar–intercondylar femur fractures. Nork et al evaluated all patients in a prospective database with an intra-articular distal femur fracture over a 9-year period.5 The authors evaluated 202 supracondylar–intercondylar femur fractures and found 77 (38.1%) had coronal plane fractures after review of radiographs, computed tomography (CT), and operative reports. Only 102 of the knees had CT scans available however, and the study population was relatively young. The fracture patterns may not be similar to elderly patients who may have potentially different bone quality.
It is the purpose of this study to identify the frequency of coronal plane fractures seen in elderly (≥60 years of age) patients. It is our hypothesis that elderly patients will have a significantly lower frequency of Hoffa fractures due to their bone quality combined with a likely different mechanism of injury.
Patients and Methods
After institutional review board approval, all patients over the age of 18 years of age who sustained supracondylar femur fractures were identified at 2 level I trauma centers utilizing institutional diagnostic codes from the period of January 2011 to December 2014. Patients were excluded if they did not have a CT scan of their knee or if they had previous implants to the distal femur. Patient and injury characteristics were extracted from the electronic medical records and archiving system. These included age, gender, mechanism of injury, injury severity score (ISS), and the fracture characteristics including intercondylar extension. The fracture patterns were then classified according to the Orthopaedic Trauma Association (OTA) criteria.6
Next, the CT scans of all the patients were reviewed to verify intercondylar extension and evaluate for either a medial or lateral condyle coronal plane fracture. The patients were then stratified (≥60 years and <60 years) and compared to determine differences in injury characteristics and/or fracture patterns with special attention to the prevalence of coronal plane femoral condyle fractures identified via CT scans.
All patient data were entered into a centralized database (Microsoft Excel, Redmond, Washington). Statistical analysis was performed for the elderly and the younger cohort patient populations. Binary comparisons were made using a Fisher exact test and ordinal or continuous variables were analyzed with Mann-Whitney U test. Significance was set at P < .05.
Results
One hundred ten patients were identified with supracondylar femur fractures (12 OTA 33A, 2 OTA 33B, 96 OTA 33C). The study population included 49 males and 61 females with an average age of 50.7 years (range, 21-92 years). The average age for the younger cohort (<60 years) was 39.3 years (range, 21-59 years) versus 69.3 years (range, 60-88 years) for the elderly cohort. The elderly group included a higher percentage of female (81% vs. 36%, P = .0001) patients.
There were 14 OTA 33-C1 fractures (10 in younger cohort vs 4 in elderly cohort), 32 33-C2 fractures (21 in younger cohort vs 11 in elderly cohort), and 50 33-C3 fractures (33 in younger cohort vs 17 in elderly cohort). Of the 96 supracondylar–intercondylar fractures, 32 (33%) patients were >60 years of age.
The injury characteristics were quite different between the 2 groups. The elderly cohort was more likely to sustain their injury due to a fall (59% vs 19%, P = .0001). Motor vehicle collision was the most common mechanism for the younger population (73% vs 38%, P = .0009; Table 1). The average ISS was similar between the 2 groups (15.2 elderly vs 15.6 younger cohort, P > .05). The percentage of open fractures (30% elderly vs 46%) was not significantly different between the 2 groups (P = .17). Open fractures in the elderly cohort (n = 10) did not have a higher rate of coronal plane fractures when compared with closed injuries (n = 22; P = .71). The classification of the open fractures was not compared.
Table 1.
Patient Demographics and Injury Characteristics.
| Elderly | Young | Significance | |
|---|---|---|---|
| Total patients | 32 | 64 | |
| MOI | |||
| MVC | 12 | 47 | .0009 |
| Fall | 19 | 12 | .0001 |
| GSW | 1 | 3 | 1 |
| Crush | 0 | 2 | .55 |
| Average ISS | 16 | 16 | >.05 |
| Open Fx | 10 | 29 | .27 |
| Coronal plane Fx | 14 (48%) | 42 (66%) | .04 |
| Lateral condyle | 12 (86%) | 25 (60%) | .1 |
Abbreviations: Fx, fracture; GSW, gunshot wound; ISS, injury severity score; MOI, mechanism of injury; MVC, motor vehicle collision.
Italics values specify values <0.05.
Coronal plane condyle fractures were visualized on CT scans in 56 (58%) of the 96 supracondylar–intercondylar 33C femur fractures. There were no coronal plane fractures in OTA 33A fractures and only 2 in the OTA 33B fractures. Forty-four percent of elderly patients sustained a coronal plane fracture compared with 66% of the younger cohort (P = .04; Figure 1). Although elderly patients more commonly had lateral condyle coronal plane fractures (86% vs 60%), this finding was not significant. Eleven percent of the younger cohort had coronal plane fractures involving both the medial and lateral femoral condyle compared with 3% in the elderly cohort (P = .26)
Figure 1.
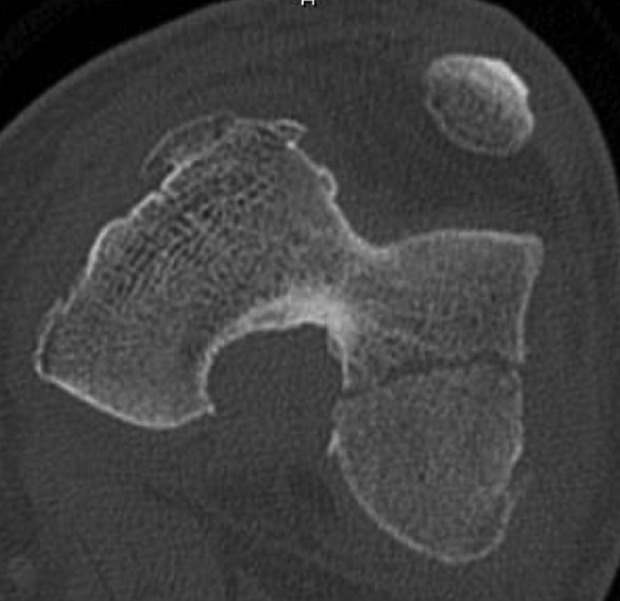
Axial computed tomography (CT) scan with coronal fracture line involving the lateral condyle of a supracondylar femur fracture in an elderly patient.
Discussion
Fractures of the distal femur account for 3% to 6% of all femoral fractures,7-9 with the majority occurring as a low-energy fracture in the elderly patients.9,10 Distal femur fractures are the second most common fragility fracture in elderly patients following those about the hip.7 Several studies have evaluated mortality rates following distal femur fractures in the elderly patients; however, to the best of our knowledge, this is the first study to scrutinize the fracture patterns and specifically look at the rate of Hoffa fractures in an elderly population.11-14
The 58% of supracondylar–intercondylar femur fractures with coronal plane fractures identified in this study population is higher than previously reported. In the landmark study by Nork et al, the authors identified 77 (38.1%) coronal plane fractures of the 202 supracondylar–intercondylar fractures in the study population.5 Their study may underestimate the prevalence of the coronal plane fractures as only 102 of their included patients had CT scans available and the authors commented that biplanar radiographs were only diagnostic in 69% of the knees for a coronal plane fracture. More so, the occurrence rate of Hoffa fractures in the elderly study population of 44% in this study was higher than expected and is the first to provide an occurrence rate in the elderly for supracondylar–intercondylar femur fractures.
We found the elderly patients more commonly sustained their injury as a result of a fall compared with the younger cohort (59% vs 19%, P = .0001). This finding reflects prior research with respect to the mechanism of injury for distal femur fractures in an older population. In a study of 105 patients with distal femur fractures including only patients older than 50 years of age, 95% of the injuries were considered to be low energy.15 Many of these patients may be frail and the distal femur fractures may be devastating injuries. Streubel et al reported the mortality rates of 92 distal femur fractures in patients older than 60 years of age.13 The mortality rates at 30 days, 6 months, and 1 year after surgery were 6%, 18%, and 25% respectively. When only the 48 nonperiprosthetic fractures were evaluated, the mortality rate improved slightly to 2%, 13%, and 23% at the same time intervals. When they compared the rates with hip fractures from the same institution, they found the mortality rates were similar causing some surgeons to question postoperative weight-bearing protocols for these elderly patients often with multiple comorbidities.15
Previous work has cautioned surgeons about early weight bearing after supracondylar femur fractures fixed with locked plating.16 More recent trends have questioned this philosophy, and thus, some studies have attempted to find better implants that would allow for earlier weight bearing. Wahnert et al tested 4 different implants in a biomechanical study using osteoporotic bone models.9 The authors found that intramedullary implants that allowed for distal locking achieved greater axial load and cycles to failure compared with lateral locking plates. The authors did not account for coronal plane fractures however, and after the findings of the current study, these fracture patterns may need to be the focus of future implant designs. Potentially missed coronal plane fractures could lead to early fracture displacement and failure. There is currently a prospective cohort comparison study of early weight bearing in distal femur fractures in patients over 65 years of age, and this question may be answered in the future.17
Several limitations of this study should be considered. This retrospective review only included patients with completed CT scans. We were unable to review the records and determine why some patients with supracondylar fractures did not obtain a CT scan and were thus excluded, possibly overestimating the number of patients with coronal plane fractures. Even so, based on previous research, the accuracy of plane radiographs is limited with respect to Hoffa fractures and we wanted to allow for accurate diagnosis. Secondly, this study only reported on the injury patterns and fracture characteristics. It was beyond the scope of this study to describe how the fracture patterns affected outcomes, but this would certainly be useful information. Detailing the outcomes would offer further guidance as how to best manage the different fracture patterns.
A strength of this study is we included both OTA 33A and OTA 33B type fractures in this analysis. In patients with osteoporotic bone, we wanted to determine whether the Hoffa fracture was noted in these fracture patterns.
In conclusion, this study found that Hoffa fractures occur in up to 44% of supracondylar–intercondylar fractures in patients older than 60 years of age. Although this is less than that occurring in a younger cohort, the prevalence is greater than expected. It is important a high index of suspicion be maintained for the Hoffa fracture in all distal femur fractures, regardless of age or mechanism of injury.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Hübner A. Lehrbuch der Frakturen und Luxationen fur Artzte und Studierende. Ist ed Wurzburg, Germany: Verlag der Stahel’schen Universitats Buch and Kunsthandlung; 1888. [Google Scholar]
- 2. Hübner A. Lerhbuch der Frakturen und Luxationen fur Arzte und Studierend. IVth ed Stuttgart, Germany: Enke; 1904. [Google Scholar]
- 3. Busch F. Mehrere falle seltener knochenverletzungen. Arch Klin Chir. 1869;10:703–719. [Google Scholar]
- 4. Bartonicek J, Rammelt S. History of femoral head fracture and coronal fracture of the femoral condyles. Int Orthop. 2015;39(6):1245–1250. [DOI] [PubMed] [Google Scholar]
- 5. Nork SE, Segina DN, Aflatoon K, et al. The association between supracondylar-intercondylar distal femoral fractures and coronal plane fractures. J Bone Joint Surg Am. 2005;87(3):564–569. [DOI] [PubMed] [Google Scholar]
- 6. Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Tr. 2007;21(10 suppl): S1–S133. [DOI] [PubMed] [Google Scholar]
- 7. Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. [DOI] [PubMed] [Google Scholar]
- 8. Martinet O, Cordey J, Harder Y, Maier A, Buhler M, Barraud GE. The epidemiology of fractures of the distal femur. Injury. 2000;31 suppl 3:C62–C63. [DOI] [PubMed] [Google Scholar]
- 9. Wahnert D, Hoffmeier K, Frober R, Hofmann GO, Muckley T. Distal femur fractures of the elderly—different treatment options in a biomechanical comparison. Injury. 2011;42(7):655–659. [DOI] [PubMed] [Google Scholar]
- 10. Gwathmey FW, Jr, Jones-Quaidoo SM, Kahler D, Hurwitz S, Cui Q. Distal femoral fractures: current concepts. J Am Acad Orthop Surg. 2010;18(10):597–607. [DOI] [PubMed] [Google Scholar]
- 11. Dunlop DG, Brenkel IJ. The supracondylar intramedullary nail in elderly patients with distal femoral fractures. Injury. 1999;30(7):475–484. [DOI] [PubMed] [Google Scholar]
- 12. Butt MS, Krikler SJ, Ali MS. Displaced fractures of the distal femur in elderly patients. Operative versus non-operative treatment. J Bone Joint Surg Br. 1996;78(1):110–114. [PubMed] [Google Scholar]
- 13. Streubel PN, Ricci WM, Wong A, Gardner MJ. Mortality after distal femur fractures in elderly patients. Clin Orthop. 2011;469(4):1188–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kammerlander C, Riedmuller P, Gosch M, et al. Functional outcome and mortality in geriatric distal femoral fractures. Injury. 2012;43(7):1096–1101. [DOI] [PubMed] [Google Scholar]
- 15. Smith JR, Halliday R, Aquilina AL, et al. Distal femoral fractures: the need to review the standard of care. Injury. 2015;46(6):1084–1088. [DOI] [PubMed] [Google Scholar]
- 16. Vallier HA, Hennessey TA, Sontich JK, Patterson BM. Failure of LCP condylar plate fixation in the distal part of the femur. A report of six cases. J Bone Joint Surg Am. 2006;88(4):846–53. doi:10.2106/jbjs.e.00543. [DOI] [PubMed] [Google Scholar]
- 17. Early weightbearing on supracondylar distal femur fractures in elderly patients. ClinicalTrials.gov [Internet] NCT02475941. Bethesda, MD: National Library of Medicine (US); 2015. https://clinicaltrials.gov/ct2/show/NCT02475941. Accessed September 21, 2017. [Google Scholar]


