Abstract
Objective:
This study compared occurrence of falls, cognitive function, and balance profiles across participants in elderly age categories, investigating associations between the 3 aspects in a sample of Singapore’s elderly population.
Method:
Community-dwelling elderly individuals (N = 385) were randomly recruited and grouped into “young-old (65-74 years),” “medium-old (75-84 years),” and “oldest-old (above 85 years)” groups. The Fallproof Health and Activity questionnaire, adapted Mini-Mental State Examination (MMSE), and Berg Balance Scale (BBS) tests were used to survey information related to falls, cognition, and balance profiles.
Results:
Findings revealed significant differences in MMSE and BBS scores across the age groups. Participants with mild cognitive impairment (odds ratio [OR] = 1.87, 95% confidence interval [CI] = 1.08-3.25) and BBS score ≤40 (OR = 0.25, 95% CI = 0.14-0.46) were at the highest risk of falling.
Conclusion:
Community-dwelling elderly individuals with subtle cognitive impairment and BBS scores ≤40 displayed an increased risk of falling.
Keywords: elderly individuals, cognitive functioning, Berg Balance Scale, falls, MMSE
Introduction
Falling is a common public health problem for elderly individuals and is the fifth leading cause of death.1,2 In Singapore, Chan and colleagues3 found that 17.2% (N = 3000) of the elderly population experienced at least 1 fall a year. In 2009, the National University Hospital of Singapore reported that 85.3% of the elderly peoples’ injuries that required help in the emergency department were due to falls.4 Based on data from the Singapore National Trauma Registry, a recent study by Wong et al5 found that more than 88% of elderly patients experienced falls between 2011 and 2013.
Cognitive functioning and balance abilities are 2 primary factors for falls.6 To date, fall risk is closely related to severe cognitive impairment in elderly individuals who have dementia.7 Often, falls management programs and guidelines are directed toward this group of elderly individuals.7 However, it is possible that a subtle decline in cognitive functioning can contribute to postural instability8 and increase the risk of falling.9 The association between cognitive functioning and fall risk arises from the perspective of aging of the frontal cortex and the changes in white matter of the brain.10-12 Subtle changes in cognitive functioning might lead to poor judgments and decision-making13; declines in executive function, attention, and processing speed10,12; and decrements in verbal reasoning and ability,14 which could increase the risk of falling. This may become a particular problem when individuals with mild cognitive impairments may need to engage in dual tasking in everyday life (eg, when talking and climbing up a staircase or navigating an uneven surface on the road). Hence, the early detection of subtle cognitive impairments might help health practitioners to better identify the degree of fall risk in community-dwelling elderly people.
On the other hand, balance impairment has been recognized as a major risk factor for falls in older people.15,16 Research has demonstrated that lack of ability in balance control is associated with a higher risk of falling.15,17,18 Deterioration in biological systems, such as declines in sensory system capacity, neurological functioning, and motor functions and increased reaction time in elderly populations, causes delays in stabilization of control systems, which could contribute to postural instability and falls.19,20 It is also possible that cognition plays a key role in balance regulation in older adults, where the motor and sensory systems are integrated through higher order neurological processes.8 Tangen and colleagues found that a decline in balance ability was associated with increasing severity of cognitive impairment.21 Therefore, we sought to understand whether a similar linear association existed between cognitive function and balance abilities in a community-dwelling elderly population in an Asian community.
Cognitive functioning and balance abilities have been commonly tested by researchers to predict fall risk, especially in elderly people with severe cognitive impairment and neurological conditions such as multiple sclerosis and Alzheimer disease.8,11,22,23 However, studies examining falls, cognitive function, and balance profiles of a community-dwelling elderly population and the association between these 3 aspects are scarce in Asia. This study sought to contribute to the literature by researching the relations between these 3 phenomena in different categories of elderly people in an Asian population. The primary aims of this study were to (1) compare occurrence of falls, cognition, and balance profiles across people in elderly age categories; (2) investigate the association between the 3 aspects; and (3) provide suggestions for the development of simple screening interventions in a sample of Singapore’s elderly population.
Method
Participants
A total of 385 community-dwelling, elderly individuals (65 years and above) were recruited randomly from Singaporean communities. Recruitment e-mails were sent to senior activity centers, government organizations, and social development groups across Singapore. Based on Singapore’s Department of Statistics (2007), the age groups of the elderly people were identified as “young-old (65-74 years),” “medium-old (75-84 years),” and “oldest-old (above 85 years)” in this study.24 Ethics approval was sought from the ethics committee of the Nanyang Technological University, Singapore. Informed consent was obtained from all participants, and procedures used in the study were in accordance with ethical guidelines. Specific inclusion criteria were ability to walk independently, either with or without any assistive device, and freedom from diagnosed cognitive dysfunctions (eg, dementia and Alzheimer disease). Exclusion criteria were history of severe rheumatic arthritis, neuropathy injury, recent stroke events (<18 months), brain injuries, and diagnosed cognitive dysfunctions.
Procedure
A complete testing session included a 20-minute semi-structured interview based on material from the Fallproof Health and Activity questionnaire,18 Mini-Mental State Examination (MMSE) adapted from Folstein et al,25 and Berg Balance Scale (BBS) test.15 For the interviews, each participant was required to complete the questionnaire (Fallproof Health and Activity) either via an informal interview with the researcher or independently. The MMSE test was used to assess cognitive functions as the test is used to quantitatively assess the severity of cognitive impairment and documents cognitive changes occurring over time.26 There were 3 categories of cognitive function levels—no cognitive impairment (>24), mild cognitive impairment (18-23), and severe cognitive impairment (<17).26 The MMSE had a high test–retest level of reliability (r = .83) in assessing cognitive functioning in elderly populations.25 An updated comprehensive review found that the reliability coefficient ranged between 0.64 and 0.97 for the sample populations aged between 58 and 86 years old.26 The cutoff score of <24 showed sensitivity levels of 0.63 and a specificity of 0.96 in predicting the risk of cognitive impairment.27 The BBS is a commonly used subjective assessment tool used globally in predicting falls among elderly people.15,28 The BBS had high reliability (r ≥ .75) in assessing balance abilities in elderly people.15,28,29 The sensitivity and specificity of the BBS test were high in predicting the risk of falls in elderly persons.20,30,31 Lastly, the BBS was administered, a scale consisting of 14 subtests, with each subtest scores ranging from 0 to 4, performed in a standard order (Table 1) to measure functional abilities and balance. The maximum score for this assessment is 56. The categories were low risk of falling (41-56) and increased risk of falling (≤40).31
Table 1.
Berg Balance Scale Items.
| Item | Description |
|---|---|
| 1 | Sitting to standing |
| 2 | Standing unsupported |
| 3 | Sitting unsupported |
| 4 | Standing to sitting |
| 5 | Transfers |
| 6 | Standing with eyes closed |
| 7 | Standing with feet together |
| 8 | Reaching forward with an outstretched arm |
| 9 | Object pick up from floor |
| 10 | Turning to look behind (twisting) |
| 11 | Turning 360° |
| 12 | Placing alternate foot on stool (stepping) |
| 13 | Tandem standing |
| 14 | One leg standing |
All interviews were conducted in accordance with the preferred language (eg, English, Mandarin, Malay, and local dialects) used by the elderly participants to ensure adequate understanding of questions and provision of accurate information. Researchers were competent in speaking each participant’s preferred language. All testing sessions were voice recorded for further analysis and clarification. Two short breaks were provided for participants during the testing session: after the questionnaire interview and after the MMSE test.
Statistical Analysis
The Statistical Program for Social Sciences software version 22.0 was used for statistical analysis. For all outcome measures, between-group differences in mean change were analyzed by using a nonparametric test—Friedman test. Post hoc testing was performed using a Wilcoxon signed-rank test when the Friedman analysis of variance resulted in a statistically significant outcome (α value set at P < .05). Results were reported as means ± standard deviation (SD) for the descriptive data and z score (z) and Wilcoxon (W) for the Mann-Whitney (U) test. Binary logistic regression was used to estimate the odds ratios of risk factors associated with falls. Spearman correlation test was used to identify the correlations between MMSE and BBS scores in the 3 age categories.
Results
Table 2 shows the sociodemographic characteristics, cognitive assessment levels, the risk of falls, and medical conditions in young-old, medium-old, and oldest-old groups. The ethnicity distribution of the 385 participants was as follows: 69.9% were Chinese, 26.2% were Malay, 3.1% were Indian, and 0.8% were others. The distribution was close to the national ethnicity distribution in Singapore: Chinese (74.3%), Malays (13.3%), Indians (9.1%), and others (3.2%).32 Regarding gender distribution, there were 246 females and 139 males for this study; 83.7% (n = 206) of females and 71.9% (n = 100) of males had less than 6 years of education. Nonparametric testing revealed significant differences in weight, BMI, MMSE, and BBS scores across the 3 age groups (P < .05). The males displayed significantly higher scores on both MMSE (U = 13 560.50, W = 43 941.5, Z = −3.379, P < .05) and BBS tests (U = 13 459.5, W = 43 840.5, Z= −3.473, P < .05; Table 3). A higher percentage of fall incidents was observed in the oldest-old group compared to the other 2 groups. It was observed that the proportion of community-dwelling elderly individuals using an assistive device when walking increased with age.
Table 2.
Demographics of the Participants.a
| Characteristics | Young-Old (n = 212) | Medium-Old (n = 146) | Oldest-Old (n =27) | P Value |
|---|---|---|---|---|
| Age, mean (SD) | 69.63 (2.97) | 79.14 (2.95) | 88.22 (2.91) | <.001 |
| Height, m, mean (SD) | 1.56 (0.08) | 1.53 (0.08) | 1.51 (0.07) | >.05 |
| Weight, kg, mean (SD) | 60.56 (11.05) | 54.10 (9.82) | 51.44 (9.58) | <.001 |
| BMI, mean (SD) | 25.17 (4.98) | 23.21 (3.94) | 22.45 (3.65) | <.05 |
| MMSE scores, mean (SD) | 22.51 (5.03) | 21.18 (4.88) | 17.93 (5.04) | <.001 |
| BBS scores, mean (SD) | 47.37 (7.82) | 45.12 (7.72) | 40.74 (6.97) | <.001 |
| Amount of exercise (×days/week), mean (SD) | 2.1 (2.7) | 2.3 (2.7) | 1.3 (2.2) | |
| Gender, n (%) | ||||
| Male | 81 (38.2) | 52 (35.6) | 6 (22.2) | |
| Female | 131 (61.8) | 94 (64.4) | 21 (77.8) | |
| Ethnicity, n (%) | ||||
| Chinese | 132 (62.3) | 112 (76.7) | 25 (92.6) | |
| Malay | 71 (33.5) | 30 (20.5) | 2 (7.4) | |
| Indian | 4 (1.9) | 0 (2.7) | 0 (0) | |
| Others | 5 (2.4) | 4 (0) | 0 (0) | |
| Medical conditions, n (%) | ||||
| Hypertension | 136 (64.2) | 83 (56.8) | 17 (63) | |
| High cholesterol | 102 (48.1) | 73 (50) | 12 (44.4) | |
| Diabetes | 53 (25) | 46 (31.4) | 9 (33.3) | |
| Falls in the past 1 year, n (%) | ||||
| Yes | 58 (27.4) | 40 (27.4) | 9 (33.3) | |
| No | 154 (72.6) | 106 (72.6) | 18 (66.7) | |
| Assistive device used in walking, n (%) | ||||
| Yes | 38 (17.9) | 45 (30.8) | 13 (48.1) | |
| No | 174 (82.1) | 101 (69.2) | 25 (51.9) | |
| Education, n (%) | ||||
| ≤6 years of education | 147 (69.3) | 134 (91.8) | 25 (92.6) | |
| >6 years of education | 65 (30.7) | 12 (8.2) | 2 (7.4) | |
| MMSE categories, n (%) | ||||
| No cognitive impairment (≥24 scores) | 100 (47.2) | 56 (38.4) | 5 (18.5) | |
| Mild cognitive impairment (18-23 scores) | 75 (35.4) | 57 (39.0) | 8 (29.6) | |
| Severe cognitive impairment (≤17 scores) | 37 (17.5) | 33 (22.6) | 14 (51.9) | |
| BBS categories, n (%) | ||||
| Low fall risk (41-56 scores) | 183 (86.3) | 122 (83.6) | 15 (55.6) | |
| Increased fall risk (≤40 scores) | 29 (13.7) | 24 (16.4) | 12 (44.4) |
aN = 385.
Abbreviations: BBS, Berg Balance Scale; BMI, body mass index; MMSE, Mini-Mental State Examination; SD, standard deviation.
Table 3.
Gender Comparisons of MMSE and BBS Scores.
| Overall Gender Comparisons | |||
|---|---|---|---|
| MMSE | BBS | ||
| Male | 23.4 ± 5.1 | 47.5 ± 7.9 | |
| Female | 22.0 ± 4.9a | 45.2 ± 7.8a | |
| MMSE Score According to Age Groups | |||
| Young-Old | Medium-Old | Oldest-Old | |
| Male | 23.4 ± 5.1 | 22.4 ± 4.2 | 18.0 ± 6.8 |
| Female | 22.0 ± 4.9a | 20.5 ± 5.1a | 17.9 ± 4.6 |
| BBS Score According to Age Groups | |||
| Young-Old | Medium-Old | Oldest-Old | |
| Male | 48.5 ± 8.1 | 46.3 ± 7.7 | 44.8 ± 3.8 |
| Female | 46.7 ± 7.6a | 44.5 ± 7.7 | 39.6 ± 7.3 |
Abbreviations: BBS, Berg Balance Scale; MMSE, Mini-Mental State Examination.
a Significant difference from male participants.
Table 4 shows the risk factors for falls and cognitive impairment levels. Risk of falling was significantly higher in those who had mild cognitive impairment and with BBS scores at and below the cutoff of 40.
Table 4.
Independent Risk Factors for Fall and Cognitive Impairment Levels.
| Binary logistic regression: Odds Ratios (OR) and 95% Confidence Intervals (CIs) for Fall | ||||
|---|---|---|---|---|
| Characteristics | B (SE) | OR | 95% CI | P Value |
| MMSE categories | ||||
| No cognitive impairment (≥24 scores) | 1 | Reference | ||
| Mild cognitive impairment (18-23 scores) | 0.63 (0.28) | 1.874 | 1.080-3.250 | <.05 |
| Severe cognitive impairment (≤17 scores) | 0.32 (0.32) | 1.376 | 0.730-2.59 | |
| BBS categories | ||||
| Low fall risk (41-56 scores) | 1 | Reference | ||
| Increased fall risk (≤40 scores) | −1.370 (0.306) | 0.254 | 0.14-0.463 | <.001 |
Abbreviations: BBS, Berg Balance Scale; MMSE, Mini-Mental State Examination; SE, standard error.
Overall, a moderate Spearman ρ correlation value (r = .485, P = .000) was found between MMSE and BBS. A significant moderate relationship was also determined between MMSE and BBS in young-old (r = .467, P = .000) and medium-old (r = .502, P = .000) groups (Figure 1). However, no relationship was found between MMSE and BBS scores in the oldest-old group.
Figure 1.
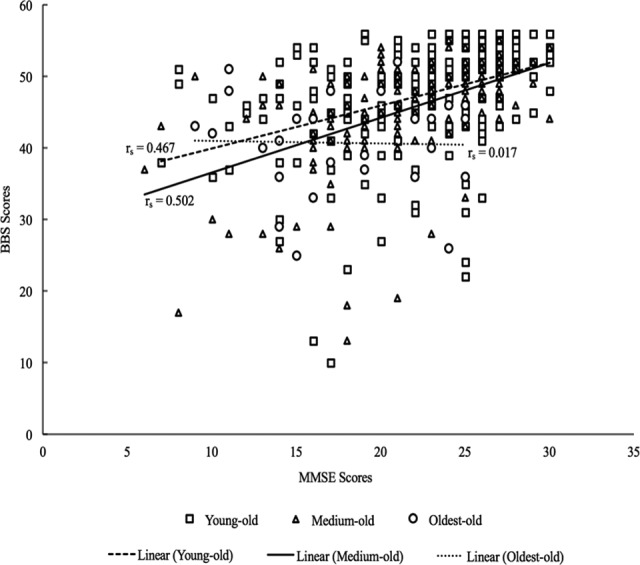
Spearman correlation between MMSE and BBS scores of the 3 age categories—young-old, medium-old, and oldest-old. BBS denotes Berg Balance Scale; MMSE, Mini-Mental State Examination.
Discussion
The aims of this study were to (1) compare occurrence of falls, cognition, and balance (2 primary implicated factors) profiles across elderly age categories; (2) investigate associations between them; and (3) provide suggestions for the development of simple screening interventions in a sample of Singapore’s elderly population. In this screening of Singapore community-dwelling participants, it was observed that elderly individuals had significant declines in cognitive functioning and balance abilities between young-old (65-74 years old) and oldest-old (>85 years old) groups. Mean MMSE scores showed that the level of cognitive function was classified as mild cognitive impairment, for both genders, but especially in females, in all 3 groups. The oldest-old group had a higher percentage of fall incidences, higher risk of cognitive impairment, and increased risk of falls, compared to the younger 2 groups. The risk factor analysis showed that mild cognitive impairment and balance scores ≤40 were associated with falls. Last, we found a moderate correlation between MMSE and BBS scores in the young-old and medium-old age groups.
The findings showed that both cognitive functions and balance abilities significantly declined as people aged. In line with the outcomes of other studies, the current finding also indicates that community-dwelling elderly individuals with mild cognitive impairment9,13,33,34 and balance impairment20,31,34 were most at risk of falling. From the aging perspective, deteriorating speed of cognitive function, a decline in attention and executive function (eg, slow response inhibitions and judgment errors), and declines in sensory systems, due to the aging of the frontal cortex, could be the biggest factors for an increased risk of falling.7,10,18 Furthermore, cognition plays a vital role in the balance regulation in older adults.8 The decline in cognitive function observed might explain the increased risk of falling in this sampled population.
The results of our study have shown that Singapore’s community-dwelling elderly individuals display subtle declines in cognition (mild cognitive impairment), with functional performance below the average scores found in other studies, of similar age groups, conducted in the United States, Japan, Korea, Brazil, China, United Kingdom and Turkey.35 It is plausible that the low education level of the majority of participants in the sampled groups contributed to the subtle decline in cognitive functioning, as education is one of the primary protective mechanisms for cognitive impairment.34 This assumption on the role of education in cognitive impairment is supported by data of Seeman et al,36 who found that highly educated groups were less likely to exhibit cognitive impairment in a group of elderly individuals, aged 70 to 79 years old. Albert37 suggested that low levels of education relate to cognitive declines based on the fact that effects of education on the increment of synaptic density in the brain in the early stages of life could delay the appearance of cognitive declines in old age. Eggenberger et al38 suggested that an intervention exercise that combined cognitive and motor training (eg, interactive cognitive motor video game dancing) improved cognitive function of older adults. Hence, clinicians and health practitioners could consider the alternative solutions/interventions exercises suggested by Eggenberger et al38 to tackle health-related issues on falls, balance, and cognitive deterioration and impairment.
The current findings suggest that the results from the MMSE and BBS tools could be used to predict the risk of falling. The use of the MMSE test tool to predict falls has displayed mixed results.8 Muir et al8 suggested that MMSE scores at and below 26 were strongly associated with the high risk of severe fall-related injury. Mirelman et al7 and Mitchell39 concluded that the MMSE test tool was not strongly associated with fall risk among community-living older adults. In contrast, our results supported the findings of Gleason et al,9 which suggested that a decrease in MMSE scores was associated with elevations in the rate of falls. We found that subtle cognitive deficits can increase the risk of falls. On the other hand, the BBS tool produced the highest sensitivity in predicting falls in independent functioning, community-dwelling elderly individuals.30,31 However, Muir et al16 found that the BBS tool, with the cutoff value at 45, failed to identify people at a high risk of falling (multiple falls). They suggested that the use of a scale cutoff point of 45, suggested by Berg et al,15 was inadequate to predict future falls. Our study adopted a cutoff point of 40 and it seemed to have a predictive value for risk of falls.30,31 Thus, it is suggested that the BBS test tool, with a cutoff point of 40, could be adopted by health practitioners as part of an initial simple screening assessment procedure for the community-dwelling elderly population in Singapore. Further analysis of correlations between MMSE and BBS test scores indicated a moderate relationship in young-old and medium-old groups. This finding suggests that a decline in cognitive ability might have led to a decrease in balance performance, suggesting that clinicians and health practitioners of Singapore could adopt the BBS test as a baseline screening tool to identify potential cognitive impairment in the young-old and medium-old groups.
One limitation of the study was the self-reporting of fall incidences, with a possibility of underreporting by the older participants. The major implication of this study is that health professionals could use the MMSE and BBS tests as predictors for falls in elderly individuals, aged below 85 years. Health professionals might need to explore ways to decelerate deterioration in cognitive function and develop strategies for fall prevention, especially in the oldest group. These strategies could include activities for elderly people to engage the brain and enhance nervous system function. These could include balance and mobility exercise training, use of problem-solving and perceptual awareness activities, cognitive and memory games, and discussion of health education and home safety guidelines. Among elderly individuals, we noted a moderate relationship found between cognitive decline and the risk of falls, and either test could be used as a simple screening tool to incorporate in a routine primary care assessment in Singapore, with further evaluations needed in other South East Asia (SEA) countries.
Conclusion
In conclusion, findings revealed that participants older than 85 years had the highest number of fall incidents, combined with mild impairments displayed in the cognitive and balance assessments. Balance ability and cognitive functioning levels were the biggest risk factors for falls. A significant moderate relationship was determined between MMSE and BBS tests in the young-old (65-74 years old) and medium-old (75-84 years old) groups. This relationship indicates that the MMSE and BBS tools could be incorporated into a routine primary care assessment in Singapore. Future studies could examine and evaluate the use of the MMSE and BBS tests in other SEA countries.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: National Institute of Education(NIE) Academic Research Fund, Singapore (AcRF) x [RI 8/13 CJY].
ORCID iD: Mei Teng Woo, Msc http://orcid.org/0000-0003-1289-9538
References
- 1. Kannus P, Parkkari J, Niemi S, Palvanen M. Fall-induced deaths among elderly people. Am J Public Health. 2005;95(3):422–424. doi:10.2105/AJPH.2004.047779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kannus P, Sievänen H, Palvanen M, Järvinen T, Parkkari J. Prevention of falls and consequent injuries in elderly people. Lancet. 2005;366(9500):1885–1893. doi:10.1016/S0140-6736(05)67604-0. [DOI] [PubMed] [Google Scholar]
- 3. Chan KM, Pang WS, Ee CH, Ding YY, Choo P. Epidemiology of falls among the elderly community dwellers in Singapore. Singapore Med J. 1997;38(10):427–431. [PubMed] [Google Scholar]
- 4. Yeo YY, Lee SK, Lim CY, Quek LS, Ooi SB. A review of elderly injuries seen in a Singapore emergency department. Singapore Med J. 2009;50(3):278–283. [PubMed] [Google Scholar]
- 5. Wong TH, Nguyen HV, Chiu MT, et al. The low fall as a surrogate marker of frailty predicts long-term mortality in older trauma patients. PLoS One. 2015;10(9). doi:10.1371/journal.pone.0137127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Whitney J, Close JCT, Lord SR, Jackson SH. Identification of high risk fallers among older people living in residential care facilities: a simple screen based on easily collectable measures. Arch Gerontol Geriatr. 2012;55(3):690–695. doi:10.1016/j.archger.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 7. Mirelman A, Herman T, Brozgol M, et al. Executive function and falls in older adults: new findings from a five-year prospective study link fall risk to cognition. PLoS One. 2012;7(6):e40297 doi:10.1371/journal.pone.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Muir SW, Gopaul K, Montero Odasso MM. The role of cognitive impairment in fall risk among older adults: a systematic review and meta-analysis. Age Ageing. 2012;41(3):299–308. doi:10.1093/ageing/afs012. [DOI] [PubMed] [Google Scholar]
- 9. Gleason CE, Gangnon RE, Fischer BL, Mahoney JE. Increased risk for falling associated with subtle cognitive impairment: secondary analysis of a randomized clinical trial. Dement Geriatr Cogn Disord. 2009;27(6):557–563. doi:10.1159/000228257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gunning-Dixon FM, Raz N. The cognitive correlates of white matter abnormalities in normal aging. Neuropsychology. 2000;14(2):224–232. [DOI] [PubMed] [Google Scholar]
- 11. Pedroso RV, Coelho FG, Santos-Galduróz RF, Costa JLR, Gobbi S, Stella F. Balance, executive functions and falls in elderly with Alzheimer’s disease (AD): a longitudinal study. Arch Gerontol Geriatr. 2012;54(2):348–351. doi:10.1016/j.archger.2011.05.029. [DOI] [PubMed] [Google Scholar]
- 12. Raz N, Lindenberger U, Rodrigue KM, et al. Regional brain changes in aging healthy adults: general trends, individual differences and modifiers. Cereb Cortex. 2005;15(11):1676–1689. doi:10.1093/cercor/bhi044. [DOI] [PubMed] [Google Scholar]
- 13. Fischer BL, Gleason CE, Gangnon RE, Janczewski J, Shea T, Mahoney JE. Declining cognition and falls: role of risky performance of everyday mobility activities. Phys Ther. 2014;94(3):355–362. doi:10.2522/ptj.20130195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Anstey KJ, Wood J, Kerr G, Caldwell H, Lord SR. Different cognitive profiles for single compared with recurrent fallers without dementia. Neuropsychology. 2009;23(4):500–508. doi:10.1037/a0015389. [DOI] [PubMed] [Google Scholar]
- 15. Berg KO, Maki BE, Williams JI, Holliday PJ, Wood-Dauphinee SL. Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil. 1992;73(11):1073–1080. [PubMed] [Google Scholar]
- 16. Muir SW, Berg K, Chesworth B, Klar N, Speechley M. Balance impairment as a risk factor for falls in community-dwelling older adults who are high functioning: a prospective study. Phys Ther. 2010;90(3):338–347. doi:10.2522/ptj.20090163. [DOI] [PubMed] [Google Scholar]
- 17. Lajoie Y, Gallagher SP. Predicting falls within the elderly community: comparison of postural sway, reaction time, the Berg Balance Scale and the Activities-Specific Balance Confidence (ABC) scale for comparing fallers and non-fallers. Arch Gerontol Geriatr. 2004;38(1):11–26. doi:10.1016/S0167-4943(03)00082-7. [DOI] [PubMed] [Google Scholar]
- 18. Rose DJ. Fallproof!: A Comprehensive Balance and Mobility Training Program. 2nd ed Champaign, IL: Human Kinetics; 2010. [Google Scholar]
- 19. Glorioso C, Sibille E. Between destiny and disease: genetics and molecular pathways of human central nervous system aging. Prog Neurobiol. 2011;93(2):165–181. doi:10.1016/j.pneurobio.2010.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Thorbahn LDB, Newton RA. Use of the berg balance test to predict falls in elderly persons. Phys Ther. 1996;76(6):576–583. doi:10.1093/ptj/76.6.576. [DOI] [PubMed] [Google Scholar]
- 21. Tangen GG, Engedal K, Bergland A, Moger TA, Mengshoel AM. Relationships between balance and cognition in patients with subjective cognitive impairment, mild cognitive impairment, and Alzheimer’s disease. Phys Ther. 2014;94(8):1123–1134. doi:10.2522/ptj.20130298. [DOI] [PubMed] [Google Scholar]
- 22. Graafmans WC, Ooms ME, Hofstee HM, Bezemer PD, Bouter LM, Lips P. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol. 1996;143(11):1129–1136. doi:10.1093/oxfordjournals.aje.a008690. [DOI] [PubMed] [Google Scholar]
- 23. Saverino A, Waller D, Rantell K, Parry R, Moriarty A, Playford ED. The role of cognitive factors in predicting balance and fall risk in a neuro-rehabilitation setting. PLoS One. 2016;11(4):e0153469 doi:10.1371/journal.pone.0153469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Singapore Department of Statistics. National Statistical Standards: Recommendations on Definition and Classification of Age. 2007, https://www.singstat.gov.sg/docs/default-source/default-document-library/methodologies_and_standards/standards_and_classifications/nsa.pdf.
- 25. Folstein ME, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. [DOI] [PubMed] [Google Scholar]
- 26. Tombaugh TN, McIntyre NJ. The Mini-Mental State Examination: a comprehensive review. J Am Geriatr Soc. 1992;40(9):922–935. doi:10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- 27. Kukull WA, Larson EB, Teri L, Bowen J, McCormick W, Pfanschmidt ML. The Mini-Mental State Examination score and the clinical diagnosis of dementia. J Clin Epidemiol. 1994;47(9):1061–1067. doi:10.1016/0895-4356(94)90122-8. [DOI] [PubMed] [Google Scholar]
- 28. Jacome C, Cruz J, Oliveira A, Marques A. Validity, reliability, and ability to identify fall status of the Berg Balance Scale, BESTest, mini-BESTest, and brief-BESTest in patients with COPD. Phys Ther. 2016;96(11):1807–1815. doi:10.2522/ptj.20150391. [DOI] [PubMed] [Google Scholar]
- 29. Berg K. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41(6):304–311. doi:10.3138/ptc.41.6.304. [Google Scholar]
- 30. Shumway-Cook A, Baldwin M, Polissar NL, Gruber W. Predicting the probability for falls in community-dwelling older adults. Phys Ther. 1997;77(8):812–819. doi:10.1093/ptj/77.8.812. [DOI] [PubMed] [Google Scholar]
- 31. Jeon Y, Kim G. Comparison of the Berg Balance Scale and Fullerton Advanced Balance Scale to predict falls in community-dwelling adults. J Phys Ther Sci. 2017;29(2):232–234. doi:10.1589/jpts.29.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Department of Statistics Singapore. Population Trends, 2015; 2015. www.singstat.gov.sg.
- 33. Taylor ME, Delbaere K, Lord SR, Mikolaizak AS, Close JC. Physical impairments in cognitively impaired older people: implications for risk of falls. Int Psychogeriatr. 2013;25(1):148–56. doi:10.1017/S1041610212001184. [DOI] [PubMed] [Google Scholar]
- 34. Härlein J, Halfens RJ, Dassen T, Lahmann NA. Falls in older hospital inpatients and the effect of cognitive impairment: a secondary analysis of prevalence studies. J Clin Nurs. 2011;20(1-2):175–183. doi:10.1111/j.1365-2702.2010.03460.x. [DOI] [PubMed] [Google Scholar]
- 35. Arguvanli S, Akin S, Deniz Safak E, et al. Prevalence of cognitive impairment and related risk factors in community-dwelling elderly in Kayseri, Turkey. Turk J Med Sci. 2015;45(5):1167–1172. doi:10.3906/sag-1406-149. [DOI] [PubMed] [Google Scholar]
- 36. Seeman TE, Huang M, Bretsky P, Crimmins E, Launer L, Guralnik JM. Education and APOE-e4 in longitudinal cognitive decline: Macarthur Studies of Successful Aging. J Gerontol B Psychol Sci Soc Sci. 2005;60(2):74–83. doi:10.1093/geronb/60.2.P74. [DOI] [PubMed] [Google Scholar]
- 37. Albert MS. How does education affect cognitive function?. Ann Epidemiol. 1995;5(1):76–78. doi:10.1016/1047-2797(94)00044-T. [DOI] [PubMed] [Google Scholar]
- 38. Eggenberger P, Wolf M, Schumann M, de Bruin ED. Exergame and balance training modulate prefrontal brain activity during walking and enhance executive function in older adults. Front Aging Neurosci. 2016;8:66 doi:10.3389/fnagi.2016.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mitchell AJ. A meta-analysis of the accuracy of the Mini-Mental State Examination in the detection of dementia and mild cognitive impairment. J Psychiatr Res. 2009;43(4):411–431. doi:10.1016/j.jpsychires.2008.04.014. [DOI] [PubMed] [Google Scholar]


