Abstract
Background: Recent attention has sought to standardize hand surgery training in the United States. This study analyzes the variability in operative hand experience for orthopedic and general surgery residents. Methods: Case logs for orthopedic and general surgery residency graduates were obtained from the American Council of Graduate Medical Education (2006-2007 to 2014-2015). Plastic surgery case logs were not available for comparison. Hand surgery case volumes were compared between specialties with parametric tests. Intraspecialty variation in orthopedic surgery was assessed between the bottom and top 10th percentiles in procedure categories. Results: Case logs for 9605 general surgery residents and 5911 orthopedic surgery residents were analyzed. Orthopedic surgery residents performed a greater number of hand surgery cases than general surgery residents (P < .001). Mean total hand experience ranged from 2.5 ± 4 to 2.8 ± 5 procedures for general surgery residents with no reported cases of soft tissue repairs, vascular repairs, and replants. Significant intraspecialty variation existed in orthopedic surgery for all hand procedure categories (range, 3.3-15.0). Conclusions: As the model for hand surgery training evolves, general surgeons may represent an underutilized talent pool to meet the critical demand for hand surgeon specialists. Future research is needed to determine acceptable levels of training variability in hand surgery.
Keywords: surgery, education, orthopedic, residency, fellowship
Introduction
Hand surgery training in the United States is based on a graduated model of experiential learning that begins in residency and often matures during fellowship.11 Orthopedic, plastic surgery, and general surgery residency graduates apply for hand surgery fellowships in the United States. However, general surgeons represent a minority of hand surgery fellowship applicants.6 While the Accreditation Council for Graduate Medical Education (ACGME) mandates hand surgery training for orthopedic surgery, similar requirements do not exist for general surgery. Furthermore, while orthopedic surgery sponsors more than 60 hand surgery fellowship programs,20 only 1 exists under the auspices of general surgery.7 These differences may be problematic for standardized hand surgery training in the United States.
The current model for hand surgery training is evolving. Some experts have advocated for extended training via integrated hand surgery residency training while others have advocated for additional hand surgery fellowship years.11,22 Elucidation of the number of hand surgery cases performed by surgical residents may inform program directors and governing educational bodies regarding the current state of operative hand surgery training during residency. In addition, a growing need for standardized training exists in today’s litigious environment with renewed focus on quality health care delivery.14 In this study, we determine the interspecialty and intraspecialty variability in operative hand training during surgical residency.
Previous studies have been limited to qualitative studies on the impact of specialty on hand surgery training during residency.18,19 Training discipline affects perceived comfort in performing certain hand surgeries, which can affect case selection during independent practice.2,13 Currently, little is known regarding the state of hand surgery training during general surgery residency. We hypothesized that orthopedic residents would perform more hand surgery cases than general surgery residents and that significant intraspecialty variation would exist within orthopedic surgery residency programs.
Materials and Methods
Approval was obtained from the institutional review board to review ACGME case logs of chief residents in orthopedic and general surgery.1 These data represent the cumulative operative experience during residency. At the time of study, the residency review committee for plastic surgery did not permit public distribution of ACGME case logs. Thus, cumulative operative statistics were only available for general surgery and orthopedic surgery residents (2006-2007 to 2014-2015).
The Tracked Procedures for Specialty by Category document for each specialty was reviewed (Supplemental Tables S1 and S2, available in the online version of the journal). For orthopedic surgery, case volume for “Hand/Fingers” was compared with “Hand” for general surgery. Each procedure category is composed of thematic Current Procedural Terminology (CPT) codes, which are monitored by respective residency review committees and program directors in surgical specialties. For general surgery, the following categories existed: soft tissue repair, tendon repair, nerve repair, vascular repair, replantation, and other. Prior to the 2009-2010 academic year, vascular repair and nerve repair were reported under a single category. In contrast, the following categories existed for orthopedic surgery: incision, excision, intro/removal, repair/revise, trauma, arthrodesis, amputation, and other.
To describe the intraspecialty variation in operative hand experience during orthopedic residency training, fold differences between the 10th and 90th percentiles were calculated. To compare the cumulative operative experience by specialty, the mean number of cases ± standard deviations was compared with an unpaired student t test using Welch correction for unequal variances. Annual trends in case volume were assessed with 1-way analysis of variance (ANOVA) tests. All statistical tests were 2-tailed and performed on GraphPad Prism 6.02 software (GraphPad, La Jolla, California). P values less than .05 were considered significant.
Results
A total of 9605 general surgery residents and 5911 orthopedic surgery residents were included in this study (Table 1). The complement of general surgery residents increased 13.7% from 1004 in 2006-2007 to 1142 in 2014-2015. Similarly, orthopedic surgery residents increased 13.5% from 616 in 2006-2007 to 699 in 2014-2015. Each graduating class of orthopedic surgery residents performed a greater number of hand surgery cases than general surgery residents (P < .001, Figure 1). Over the study period, the mean number of total hand surgery cases was stable for general surgery residents (P > .05) but decreased for orthopedic residents (P < .05).
Table 1.
Number of Orthopedic and General Surgery Residency Programs and Chief Residents.
| Orthopedic surgery |
General surgery |
|||
|---|---|---|---|---|
| Academic year | No. of residency programs | No. of chief residents | No. of residency programs | No. of chief residents |
| 2006-2007 | 149 | 616 | 248 | 1004 |
| 2007-2008 | 148 | 621 | 246 | 1020 |
| 2008-2009 | 148 | 635 | 244 | 1044 |
| 2009-2010 | 147 | 653 | 242 | 1040 |
| 2010-2011 | 148 | 650 | 240 | 1060 |
| 2011-2012 | 149 | 675 | 242 | 1092 |
| 2012-2013 | 150 | 678 | 240 | 1098 |
| 2013-2014 | 151 | 684 | 243 | 1105 |
| 2014-2015 | 151 | 699 | 246 | 1142 |
| Total (%) | — | 5911 (38.1) | — | 9605 (61.9) |
Figure 1.
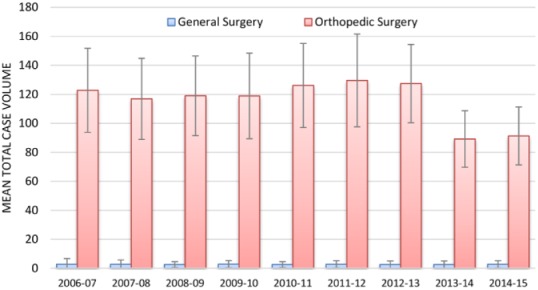
Total operative hand experience for general surgery and orthopedic surgery residents.
Note. Bars represent mean total case volume. Error bars represent standard deviations. During each year, orthopedic surgery residents performed more hand surgery cases (P < .001). There was a decrease in case volume from 2013 to 2014 onward for orthopedic surgery (P < .001), whereas case volume for general surgery remained stable (P > .05).
The distribution of hand surgery cases for general surgery residents was investigated in greater detail (Table 2). There were no soft tissue repairs, vascular repairs, or replants reported and less than 1 case each reported for tendon repair, nerve repair, and other hand procedures. The average total hand experience for general surgery residents ranged from 2.5 ± 4 to 2.8 ± 5 hand surgery cases.
Table 2.
Trends in Operative Hand Experience During General Surgery Residency.
| Mean no. of cases ± SD |
|||||||
|---|---|---|---|---|---|---|---|
| Academic year | Soft tissue repair | Tendon repair | Nerve repair | Vascular repair | Replant | Other | Total |
| 2006-2007 | 0 ± 0 | 0.5 ± 2 | NA | NA | 0 ± 0 | 1.7 ± 5 | 2.7 ± 8 |
| 2007-2008 | 0 ± 0 | 0.5 ± 2 | NA | NA | 0 ± 0 | 1.8 ± 4 | 2.7 ± 6 |
| 2008-2009 | 0 ± 0 | 0.5 ± 1 | NA | NA | 0 ± 0 | 1.6 ± 3 | 2.5 ± 4 |
| 2009-2010 | 0 ± 0 | 0.5 ± 2 | 0.3 ± 1 | 0 ± 0 | 0 ± 0 | 1.9 ± 4 | 2.8 ± 5 |
| 2010-2011 | 0 ± 0 | 0.4 ± 1 | 0.3 ± 1 | 0 ± 0 | 0 ± 0 | 1.8 ± 3 | 2.5 ± 4 |
| 2011-2012 | 0 ± 0 | 0.4 ± 1 | 0.3 ± 1 | 0 ± 0 | 0 ± 0 | 2.0 ± 4 | 2.7 ± 5 |
| 2012-2013 | 0 ± 0 | 0.4 ± 1 | 0.3 ± 1 | 0 ± 0 | 0 ± 0 | 1.8 ± 3 | 2.5 ± 5 |
| 2013-2014 | 0 ± 0 | 0.4 ± 1 | 0.3 ± 1 | 0 ± 0 | 0 ± 0 | 1.8 ± 4 | 2.5 ± 5 |
| 2014-2015 | 0 ± 0 | 0.4 ± 1 | 0.3 ± 1 | 0 ± 0 | 0 ± 0 | 2.0 ± 4 | 2.7 ± 5 |
| P | 1.0 | .151 | 1.0 | 1.0 | 1.0 | .268 | .824 |
The breakdown of hand surgery cases for orthopedic surgery residents is displayed in Table 3. Significant decreases in case volume occurred during 2013-2014 for incision, excision, repair/revise, trauma, arthrodesis, amputation, and other hand procedures (P < .001). Average case volume for intro/removal was stable over time (P > .05).
Table 3.
Trends in Operative Hand Experience During Orthopedic Surgery Residency.
| Mean no. of cases ± SD | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Academic year | Incision | Excision | Intro/removal | Repair/revise | Trauma | Arthrodesis | Amputation | Other | Total |
| 2006-2007 | 27.9 ± 18 | 15.5 ± 9 | 1.4 ± 2 | 32.7 ± 20 | 32.2 ± 21 | 3.9 ± 4 | 7.4 ± 7 | 1.7 ± 3 | 122.8 ± 58 |
| 2007-2008 | 26.2 ± 16 | 15.3 ± 10 | 1.3 ± 2 | 30.7 ± 19 | 31.1 ± 21 | 3.7 ± 3 | 6.7 ± 6 | 1.8 ± 4 | 116.9 ± 56 |
| 2008-2009 | 27.8 ± 16 | 15.2 ± 10 | 1.3 ± 2 | 30.5 ± 18 | 32.1 ± 23 | 3.6 ± 3 | 6.7 ± 6 | 1.8 ± 4 | 119.0 ± 55 |
| 2009-2010 | 27.4 ± 17 | 15.1 ± 10 | 1.2 ± 2 | 29.5 ± 19 | 33.5 ± 27 | 3.8 ± 3 | 6.6 ± 6 | 1.8 ± 4 | 118.9 ± 59 |
| 2010-2011 | 28.6 ± 16 | 15.7 ± 10 | 1.4 ± 2 | 31.6 ± 20 | 36.0 ± 27 | 4.1 ± 4 | 6.9 ± 6 | 1.9 ± 5 | 126.1 ± 58 |
| 2011-2012 | 30.8 ± 19 | 15.8 ± 11 | 1.3 ± 2 | 31.0 ± 20 | 37.7 ± 27 | 4.0 ± 4 | 7.0 ± 6 | 1.9 ± 4 | 129.6 ± 64 |
| 2012-2013 | 30.0 ± 16 | 15.8 ± 10 | 1.5 ± 3 | 30.5 ± 18 | 37.4 ± 26 | 3.9 ± 3 | 6.9 ± 6 | 1.4 ± 3 | 127.4 ± 54 |
| 2013-2014 | 22.6 ± 13 | 13.2 ± 9 | 1.3 ± 3 | 14.9 ± 9 | 28.5 ± 18 | 2.4 ± 2 | 5.3 ± 5 | 1.0 ± 2 | 89.2 ± 39 |
| 2014-2015 | 23.3 ± 14 | 12.7 ± 8 | 1.1 ± 3 | 15.0 ± 9 | 30.6 ± 20 | 2.4 ± 2 | 5.2 ± 5 | 0.9 ± 2 | 91.3 ± 40 |
| P | <.001 | <.001 | .118 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
Fold differences between the 10th and 90th percentiles of orthopedic surgery residents were analyzed (Figure 2). Overall, the fold difference variation appeared stable over time with the exception of amputations, which decreased from 15.0 in 2006-2007 to 10.0 in 2014-2015.
Figure 2.
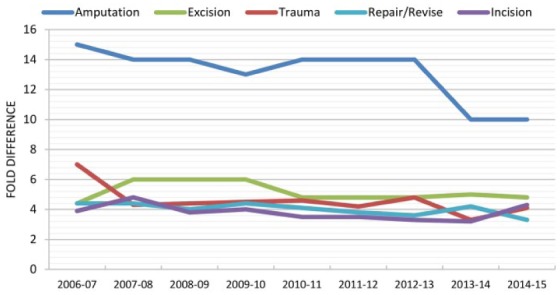
Fold differences between 10th and 90th percentiles by hand procedure category.
Note. Lines were derived from the following algorithm for fold difference: (90th percentile case volume − 10th percentile case volume) / 10th percentile case volume. Trends were not calculated for intro/removal, arthrodesis, and other hand procedure categories because the 10th percentile reported 0 cases.
Discussion
Operative experience is a critical component of surgical residency, which may increase motivation to seek additional subspecialty training. Nonuniform operative experience is an important issue facing prospective residents and the general public.14 Our study revealed significant disparities in operative hand experience for orthopedic and general surgery residents. We confirmed our hypothesis that general surgery residents would underperform in hand surgery cases during residency. Perhaps unsurprisingly, general surgeons comprise a minority of hand surgeons in the United States as evidenced by the number of general surgeons receiving added qualification in hand surgery.5 Over the past 5 years (2011-2015), 372 orthopedic surgeons obtained added qualifications in hand surgery versus 50 general surgeons.3 As previously mentioned, hand surgery is not a core competency of general surgery residency,6 and the few hand surgery cases reported in our study by general surgery residents may stem from a small cohort at unique programs. Because hand surgery is not an ACGME competency during general surgery residency, general surgery residents may receive limited hand surgery experience during burn surgery rotations. Future studies should assess the current state and perceived need for hand surgery rotations during general surgery residency. In the interim, hand surgery fellowship program directors should be aware of the lack of hand surgery experience by incoming general surgery residents.
This study had several limitations which offer future opportunities for research. First, the literature is devoid of evidence suggesting that any of the 3 training disciplines for hand surgery are superior. Thus, greater operative hand surgery experience during residency does equate with greater clinical competency. Second, orthopedic surgery case logs lacked granularity in hand surgery procedure categories, and more specific reporting could facilitate in-depth analyses on the full breadth of hand surgery. Third, plastic surgery was excluded from this study as the ACGME did not make these case logs publicly available.1 Data for plastic surgery were reviewed by the authors, but these data incorporated non–hand surgery cases under hand surgery categories, which would prohibit reasonable comparisons with general surgery and orthopedic data. Fourth, the findings from this study are predicated on accurate reporting by surgical residents, an assumption that has been challenged for both orthopedic and general surgery residents.8,17 And finally, this study focused on operative experience and did not analyze other training experiences in the emergency room or clinic. Arguably, these experiences are critical to developing important skills in case selection and clinical judgment.
General surgery residents may be an underutilized resource to meet the critical demand for hand surgery specialists.16 Greater than 1000 general surgeons graduate each year with little exposure to hand surgery. A look at the content outline for the American Board of Surgery In-Training Examination reveals general surgery residency curricula are devoid of hand surgery knowledge assessment.4 In contrast, orthopedic surgeons are routinely tested on hand surgery knowledge during residency and board examinations.21 To change the status quo, general surgery residents could be afforded greater access to hand surgery rotations starting with elective rotations. The addition of case minimums and regular assessment of hand surgery knowledge would be a critical step toward producing more hand surgeons in general surgery. However, increasing work-hour restrictions and the evolution of general surgery training toward other subspecialties would make this challenging.12 However, as the discussion for the future of hand surgery training evolves,11 general surgery could provide a needed base for future generations of hand surgeon specialists.
Great variability in operative hand surgery experience existed for orthopedic surgery residents. Over the study time period, the variability appeared stable except for amputations. These findings are in contradistinction to a previous study, which found decreasing variability in operative experience for orthopedic surgery residents since 2007.10 A separate study of general surgery residents found increased variability in operative experience after implementation of the 2003 work-hour restrictions.15 National case logs in orthopedic surgery were unavailable before this time period, but it seems plausible that variability would increase in the era of the 80-hour work-week. Programs have responded differently to these reforms, which restrict the operative experience for general surgery residents.9 However, future studies in orthopedic surgery are needed to determine the effects of resident work-hour restrictions on operative variability.
As for the etiology of the operative variability demonstrated in our study, residency programs differ in areas of clinical strength and residents differ in areas of clinical interest. Although these factors likely account for some of the variability in our study, future research is needed to define evidence-based case minimums for competency in hand surgery. Residents at low-volume operative programs may receive suboptimal training and may be underprepared for future fellowship training and independent practice. Ultimately, however, the issue of disparate operative hand experience during residency remains a critical but unanswered question.
In summary, this study demonstrated disparities in the number and types of hand surgery cases performed during orthopedic and general surgery residency. Future efforts should define acceptable limits on operative variability during residency training and define evidence-based case minimums in hand surgery. Additional ACGME reporting on the full breadth of hand surgery training including plastic surgery residency could facilitate future studies. Hand surgery fellowship program directors should be aware of the relative deficiencies in operative hand experience during residency by specialty.
Supplementary Material
Footnotes
Authors’ Note: This article was presented at the American Association for Hand Surgery, Scottsdale, Arizona, January 13-16, 2016.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: Animals or humans were not used for this study.
Statement of Informed Consent: This article did not involve patients.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental material is available in the online version of the article.
References
- 1. Accreditation Council for Graduate Medical Education. Case logs statistical reports, 2011–2015. http://www.acgme.org/Data-Collection-Systems/Case-Logs-Statistical-Reports. Accessed May 1, 2015.
- 2. Aliu O, Chung KC. A role delineation study of hand surgery in the USA: assessing variations in fellowship training and clinical practice. Hand (N Y). 2014;9:58-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. The American Board of Orthopaedic Surgery. Hand subspecialty examination statistics. https://www.abos.org/subspecialties/surgery-of-the-hand/exam-statistics.aspx. Published 2016. Accessed May 1, 2016.
- 4. American Board of Surgery. Content outline for the American Board of Surgery In-Training Examination (ABSITE). https://www.absurgery.org/xfer/GS-ITE.pdf. Published 2016. Accessed on May 1, 2016.
- 5. American Board of Surgery. Hand surgery certifying examination pass rates. http://www.absurgery.org/default.jsp?stathand. Published 2016. Accessed May 1, 2016.
- 6. American Council for Graduate Medical Education. ACGME program requirements for graduate medical education in general surgery. http://www.acgme.org/portals/0/pfassets/programrequirements/440_general_surgery_2016.pdf. Published 2016. Accessed May 1, 2016.
- 7. American Society for Surgery of the Hand. Fellowship directory. https://myaccount.assh.org/FellowshipDirectory. Published 2016. Accessed May 1, 2016.
- 8. Cadish LA, Fung V, Lane FL, et al. Surgical case logging habits and attitudes: a multispecialty survey of residents. J Surg Educ. 2016;73:474-481. [DOI] [PubMed] [Google Scholar]
- 9. Fairfax LM, Christmas AB, Green JM, et al. Operative experience in the era of duty hour restrictions: is broad-based general surgery training coming to an end? Am Surg. 2010;76:578-582. [PubMed] [Google Scholar]
- 10. Gil JA, Daniels AH, Weiss AP. Variability in surgical case volume of orthopaedic surgery residents: 2007 to 2013. J Am Acad Orthop Surg. 2016;24:207-212. [DOI] [PubMed] [Google Scholar]
- 11. Jupiter J. Hand surgery fellowships: time for reconsideration? Tech Hand Up Extrem Surg. 2011;15:197. [DOI] [PubMed] [Google Scholar]
- 12. Mattar SG, Alseidi AA, Jones DB, et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg. 2013;258:440-449. [DOI] [PubMed] [Google Scholar]
- 13. Mehta K, Pierce P, Chiu DT, Thanik V. The effect of residency and fellowship type on hand surgery clinical practice patterns. Plast Reconstr Surg. 2015;135:179-186. [DOI] [PubMed] [Google Scholar]
- 14. Polavarapu HV, Kulaylat AN, Sun S, et al. 100 years of surgical education: the past, present, and future. Bull Am Coll Surg. 2013;98:22-27. [PubMed] [Google Scholar]
- 15. Quillin RC, III, Cortez AR, Pritts TA, et al. Operative variability among residents has increased since implementation of the 80-hour workweek. J Am Coll Surg. 2016;222:1201-1210. [DOI] [PubMed] [Google Scholar]
- 16. Rios-Diaz AJ, Metcalfe D, Singh M, et al. Inequalities in specialist hand surgeon distribution across the United States. Plast Reconstr Surg. 2016;137:1516-1522. [DOI] [PubMed] [Google Scholar]
- 17. Salazar D, Schiff A, Mitchell E, et al. Variability in Accreditation Council for Graduate Medical Education Resident Case Log System practices among orthopaedic surgery residents. J Bone Joint Surg Am. 2014;96:e22. [DOI] [PubMed] [Google Scholar]
- 18. Sears ED, Larson BP, Chung KC. A national survey of program director opinions of core competencies and structure of hand surgery fellowship training. J Hand Surg Am. 2012;37:1971-1977.e7. [DOI] [PubMed] [Google Scholar]
- 19. Sears ED, Larson BP, Chung KC. Program director opinions of core competencies in hand surgery training: analysis of differences between plastic and orthopedic surgery accredited programs. Plast Reconstr Surg. 2013;131:582-590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Silvestre J, Guzman JZ, Abbatematteo JM, et al. Evaluation of content and accessibility of hand fellowship websites. Hand (N Y). 2015;10:516-521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Silvestre J, Lin IC, Chang B, et al. Unique assessment of hand surgery knowledge by specialty. Plast Reconstr Surg. 2016;137:917-924. [DOI] [PubMed] [Google Scholar]
- 22. Szabo RM. What is our identity? What is our destiny? J Hand Surg Am. 2010;35:1925-1937. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


