Abstract
Background: The objective of this study is to determine the time-dependent dissipation of extrinsic wrist ligament tension following the application external fixation with axial distraction of the wrist in a cadaveric model. Methods: Six paired fresh-frozen cadaveric specimens underwent mechanical testing simulating external fixation with 1 arm of each pair osteotomized to simulate a distal radius fracture. The change in tension was then recorded over 24 hours. Results: The rate of stress relaxation decreased with time. The average loss in tension in the control arms and osteotomized arms was 55% and 59%, respectively, over a 24-hour period. There was no statistically significant difference in the stress relaxation behavior between the 2 groups. Conclusion: This study further supports the recommendation that comminuted distal radius fractures treated with an external fixator should have Kirschner wire augmentation or other additional means of fixation to help maintain fracture length and alignment. The results of this study call in to question the efficacy of ligamentotaxis alone through external fixation as the sole means of maintaining reduction of displaced, unstable distal radius fractures.
Keywords: external fixation, distal radius, tension, ligamentotaxis, wrist
Introduction
Treatment of unstable distal radius fractures remains a controversial topic. Over the past 10 years, numerous studies have attempted comparing closed reduction and external fixation and open reduction and internal fixation for these difficult fractures. There is no consensus on the treatment of most displaced unstable distal radius fractures. External fixation remains a reliable treatment option for unstable distal radius fractures.1,3,7,12,15,17,22,24
Treatment of unstable distal radius fractures with external fixation utilizes the principle of ligamentotaxis. Ligamentotaxis is the application of axial tension for reducing and maintaining reduction of distal radius fractures by utilizing the extrinsic ligaments of the wrist. As the distal radius fracture fragment is distracted, tension through the intact dorsal and volar wrist ligament complex provides separation of fracture fragments. In 1952, DePalma8 was the first to describe the use of distraction as a definitive treatment for unstable distal radius fractures. DePalma8 used distraction to achieve reduction and then maintained the reduction by pinning the distal fragment to the intact ulna.
Documented complications of prolonged or excessive distraction across the wrist joint include digital stiffness, complex regional pain syndrome, and decreased grip strength.2,5,6,9,14,18,20,21 Papadonikolakis et al18 showed that increasing distraction across the wrist significantly increased the load required for flexion at the metacarpophalangeal joint. Kaempffe and Walker14 demonstrated that the duration and amount of distraction across the wrist joint negatively correlated with function. However, this has been questioned in a more recent study by Capo et al6 that showed moderately increased distraction of the carpus at the initial fracture reduction correlated with improved clinical outcomes, and the amount and duration of distraction did not have an adverse effect on motion. This study also documented a slight degree of distraction loss over the course of the treatment and was demonstrated by the decreased carpal height ratio (CHR) at time of ex-fix removal as compared with the CHR at application.
Anatomic restoration of palmer tilt is not possible by distraction alone.4 Furthermore, external fixation of unstable distal radius fractures has been shown to have only a 63% success rate for maintaining reduction throughout the treatment period.13 Putnam and Fischer19 proposed a combination of internal fixation with an external fixator as a neutralization device for the treatment of unstable distal radius fractures. Thus, fracture stability could be imparted without the adverse effects of prolonged distraction. We hypothesize that ligamentotaxis alone is unreliable for maintaining tension across unstable fractures of the distal radius. The purpose of this study was to determine the time-dependent dissipation of extrinsic wrist ligament tension following application of wrist external fixation with axial distraction in a cadaveric model.
Materials and Methods
Twelve fresh-frozen cadaveric forearm specimens that were amputated above the elbow joint were obtained. The specimens were then thawed to room temperature in preparation for experimental testing. Eight specimens were female, and 4 were male. The mean age of the specimens were 73 years (age range, 64-88 years). Six randomly chosen fresh-frozen cadaveric specimens (4 female and 2 the male) constituted the control group. The remaining 6 specimens constituted the study group. For each specimen, the base of the metacarpal of the long finger was exposed, and a 3/16-inch Steinman pin was inserted from dorsal to palmer through the base. A traction bow was then secured over the pin. Next, a dorsal approach to the bare area of the distal one-third of the radius was performed in each specimen, and a second 3/16-inch Steinman pin was inserted. A second traction bow was secured over this pin. Sequentially, each cadaveric forearm in the control group was placed in a Model 1101 Instron mechanical testing device (Instron Corporation, Canton, Massachusetts) via removable metal links. Twenty pounds of traction was then applied to each specimen in an attempt to recreate the tension applied to the radiocarpal joint following the application of wrist external fixation with maximum distraction (Figure 1). Using a 100-lb load cell, the following parameters were used for testing: cruise head speed 2 inches/min, hold duration 1440 minutes, and a sampling rate of 5 pts/sec. The change in tension in each cadaver forearm over a 24-hour period was determined by observing the change in applied tension as recorded on the Instron. This recording was made possible as the pins placed in the metacarpal and the radius were kept at a constant distance.
Figure 1.
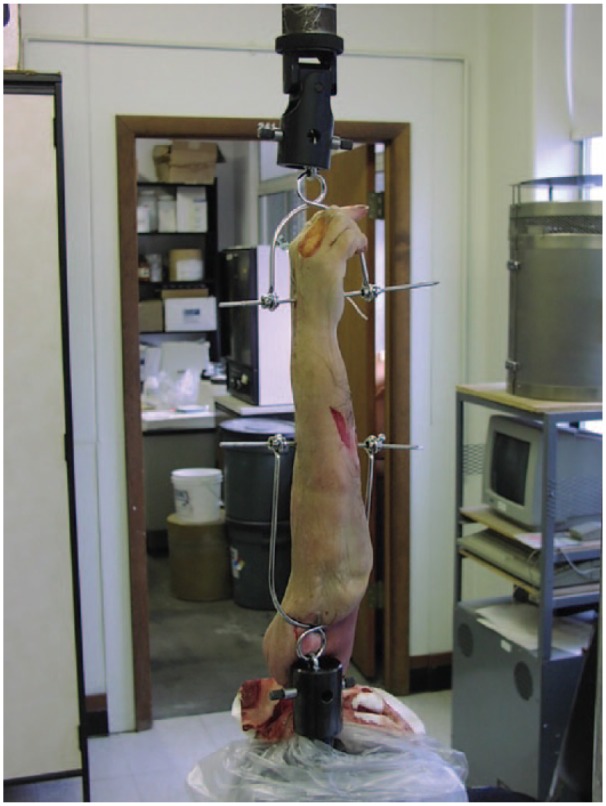
Cadaver specimen attached to Instron device for application of axial loads.
In the remaining 6 specimens, a dorsally based 1-cm wedge of bone was removed 2.5 cm from the radiocarpal joint to simulate an unstable extra-articular distal radius fracture. To accomplish this, a limited posterior approach to the distal radius was made. Using an osteotome, an osteotomy was performed perpendicular to the dorsal cortex, with the distal margin of the osteotomy parallel to the radiocarpal joint, and the proximal margin 40° away from the radiocarpal joint and 1 cm proximal to the distal margin meeting the first cut at the volar cortex. The dorsally based wedge of bone was then removed. The osteotomy was well proximal to the radiocarpal joint, and care was taken to not violate the dorsal radiocarpal ligaments and their attachments on the distal radius. The specimens were then secured into the Instron mechanical testing device and a constant tension of 20 lbs applied. A strain gauge was placed in the radioscaphocapitate ligament of each specimen using the technique previously described. During the ensuing 24-hour period, the resulting tension across the radiocarpal joint of the study specimen was recorded by monitoring tension decay observed on the Instron mechanical testing device. This article does not contain any studies with human or animal subjects.
Results
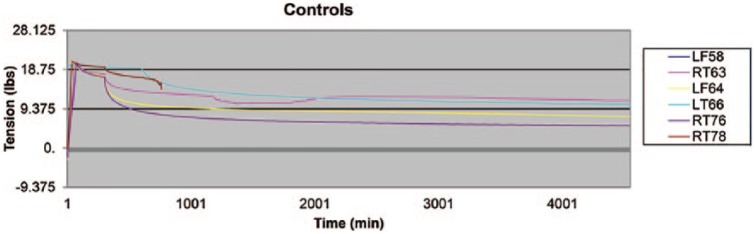
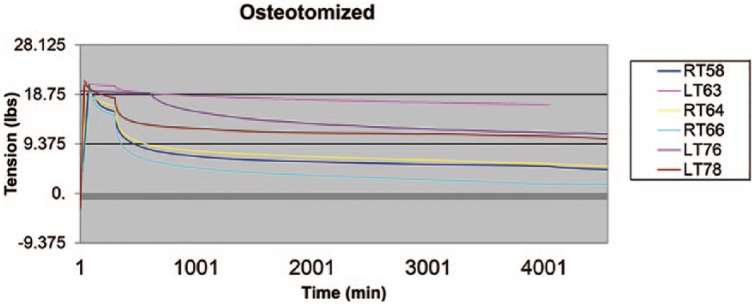
The data from 2 control specimens were incomplete, and therefore, they were deleted from the study. The average loss in tension in the control arms and osteotomized arms was 55% (11 lbs of tension, Figure 2) and 59% (11.8 lbs of tension, Figure 3), respectively, over the 24-hour period. The average decay for all 10 specimens was 57.9%. There was no statistically significant difference in the stress relaxation behavior between wrist ligaments in the control wrists and the osteotomized wrists (Table 1). Fifty percent of the tension decay occurred on average at 70.94 minutes after application of the force for the 10 specimens and did not differ significantly among the control and the study group. Fifty percent of the specimens had ultimate tension decay within the first 180 minutes.
Figure 2.
Tension dissipation as a function of time following the application of axial load to the control specimens.
Figure 3.
Tension dissipation as a function of time following the application of axial load to the distal radius fracture specimens.
Table 1.
Individual Specimen Time-Dependent Tension Measurements in Pounds.
| 30 min | 60 min | 180 min | 360 min | 720 min | 1413 min | |
|---|---|---|---|---|---|---|
| Osteotomy group | ||||||
| Left563 | 19.45 | 19.19 | 18.63 | 18.1 | 17.48 | 16.76 |
| Right566 | 8.49 | 7.19 | 5.26 | 4.13 | 3.08 | 1.71 |
| Left76 | 19.14 | 19.09 | 16.24 | 14.29 | 12.68 | 11.24 |
| Right64 | 11.15 | 10.01 | 8.38 | 7.53 | 6.64 | 5.16 |
| Right58 | 10.41 | 9.21 | 7.4 | 6.44 | 5.73 | 4.51 |
| Controls | ||||||
| Left58 | 19.26 | 19.15 | 14.96 | 12.94 | 11.58 | 10.45 |
| Left64 | 12.1 | 11.11 | 9.85 | 9.2 | 8.64 | 7.53 |
| Right76 | 11.04 | 9.73 | 7.71 | 6.75 | 6.04 | 5.33 |
| Right63 | 14.59 | 13.99 | 13.01 | 10.68 | 12.25 | 11.36 |
| Right78 | 17.75 | 17.28 | 13.95 | |||
| Osteotomy vs controls | P = .67 | P = .69 | P = .81 | P = .95 | P = .88 | P = .82 |
Discussion
Acceptable results for the treatment of unstable fractures of the distal radius have been achieved with both internal fixation with volar plates or with external fixation.15,17,22,24 Ligamentotaxis via external fixation for the treatment of unstable distal radius fractures is well established; however, potentially harmful effects of distraction on the wrist have been reported, and it is unclear how long tension is sustained once applied to the extrinsic ligaments of the wrist.2-6,9,13-15,17,19-22,24
Kaempffe and Walker14 documented an inverse relationship between functional outcomes and the duration of external fixation distraction across the wrist joint. Pain, function, and grip strength were adversely affected in direct proportion to the amount and duration of distraction. A significant finding of that study was an increased incidence of wrist stiffness with increased duration of external fixation.17 Other documented complications of external fixation have included finger clawing, nonunion, malunion, pin loosening, pin tract infection, reflex sympathetic dystrophy, nerve injury, and flexor tendon dysfunction.2,5,6,9,14,18,20,21 Bartosh and Saldan4 have established that ligamentotaxis alone is not a reliable method for recreating palmar tilt beyond a neutral position following comminuted distal radius fractures given that the volar radiocarpal wrist ligaments are less compliant than the dorsal radiocarpal wrist ligaments.
Several studies have reported secondary loss of reduction as a complication of the treatment of unstable distal radius fractures with external fixation.1,3,7 It has been recommend in more recent literature that external fixation be supplemented with Kirschner wire fixation to improve stability of the construct and maintenance of the reduction.11,12,16 However, there are very few studies examining the biomechanical properties of external fixation about the wrist. Winemaker et al23 used strain gauges to measure flexion/extension, rotation, and radioulnar bending forces across an externally fixed comminuted distal radius fracture. The measurements were made from the external fixator directly, and only 4 patients were tested. Additional percutaneous pins were used in some patients, possibly skewing the data. The average force decay in that study was 74% from the initially applied forces. Most of the force decay occurred over the initial 5 minutes following tension application. This was presumed to be due to stress relaxation of the tensioned extrinsic and intrinsic carpal ligaments.23
The ligaments of the wrist are viscoelastic structures, offering biomechanical compliance to applied loads.10 The viscoelastic nature of the wrist extrinsic ligaments allows “creep” as the ligaments accommodate applied longitudinal loads, hence tension decay. Wrist external fixation devices are designed to maintain fracture reduction by creating tension at the fracture site through force transference or ligamentotaxis. To sustain the applied load, the tension can only be maintained within the capacity of the intrinsic and extrinsic radiocarpal ligaments as well as muscle and tendons to sustain the load. Without sustainable tension in the wrist ligaments, it could be difficult to maintain distal radius fracture reduction.
Data from our study showed 55% decay in the wrist ligament tension of the control group over a 24-hour period. The simulated distal radius fracture specimens had a 59% decay in tension over a 24-hour period. The presence of an osteotomy did not significantly affect the decay of longitudinally applied tension across the radiocarpal joint when compared with the control group. Although it was not significant, ultimate tension decay occurred faster in the fracture group. An average of 50% tension decay had occurred just over an hour after tension application for both groups in our study. This is considerably longer than the time of tension decay in the study by Winemaker et al who observed 74% tension decay in 5 minutes following tension application through an external fixation device in vivo.23 The reason for this discrepancy in time is unclear but could be due to the enhanced measurement accuracy provided by the Instron mechanical testing device as opposed to single, isolated strain gauges used in the study by Winemaker et al. It is important to note that 50% of the specimens had ultimate tension decay within the first 180 minutes in our study. Less tension decay was seen in our study (57.9%) after 24 hours than was observed in the in-vivo study by Winemaker et al in 5 minutes (74%).23 This could be due to less soft tissue compliance seen in fresh-frozen cadaver specimens compared with living human tissue.
The limitations of this study include the use of cadaveric forearm specimens, where active muscle forces across the wrist joint could not be simulated. In addition, stiffer, less compliant tissue can be expected in cadaver tissue as compared with living tissue, which could possibly alter results. However, this may have been at least partially offset by the disruption of the dorsal periosteum and other surrounding distal forearm soft tissues following the creation of the distal radius osteotomy. Furthermore, it could be argued that the disruption of the dorsal periosteum at time of osteotomy more accurately reproduced the acute fracture situation. Also, the specimens could only be studied for a 24-hour period due to tissue decomposition, precluding a more prolonged evaluation period to approximate the typical duration of treatment for external fixation of distal radius fractures. Due to the configuration of the Instron mechanical testing device, only 1 Steinman pin was used in both the third metacarpal and the distal radius as opposed to the 2 pins routinely used in clinical practice. We do not believe this affected our results because there was no difficulty maintaining the pins at a constant distance throughout the testing period. This was one of the controls of our study to examine the deterioration in wrist ligament tension. In addition, we did not record simulated fracture displacement data during the testing period, as this was beyond the scope of our study.
The cadaveric specimens examined in this study displayed a soft tissue stress relaxation response to applied longitudinal tension loads. These specimens not only demonstrated marked soft tissue compliance, but they also did so within the first 2 hours following a sustained applied load of 20 lbs. The presence of a disrupted dorsal radial cortex or periosteum, as would be seen in an extra-articular distal radius fracture, had little effect on soft tissue tension decay. We conclude that extrinsic wrist ligament tension is difficult to sustain using wrist external fixation devices applied in a distraction mode. More than 50% of the original tension from an external fixator was applied in this study lost in the first 24 hours after application. It may be advisable to reexamine distal radius fractures treated with external fixation in the first 24 to 48 hours to confirm maintenance of reduction. Wrist external fixation may be best used as a neutralization device, and supplemental fixation should be considered when using external fixation for treatment of distal radius fractures.
Acknowledgments
The authors thank Nakul V. Karkare, MD, and James Thiebaud, MS, for their work on the project and Kelly Viola, MPS, ELS.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained when necessary.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors thank Palmetto Richland Memorial Hospital Research and Education Foundation for financial support.
References
- 1. Abramo A, Kopylov P, Geijer M, et al. Open reduction and internal fixation compared to closed reduction and external fixation in distal radial fractures: a randomized study of 50 patients. Acta Orthop. 2009;80:478-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Aktekin CN, Altay M, Gursoy Z, et al. Comparison between external fixation and cast treatment in the management of distal radius fractures in patients aged 65 years and older. J Hand Surg Am. 2010;35:736-742. [DOI] [PubMed] [Google Scholar]
- 3. Arora J, Malik AC. External fixation in comminuted, displaced intra-articular fractures of the distal radius: is it sufficient? Arch Orthop Trauma Surg. 2005;125:536-540. [DOI] [PubMed] [Google Scholar]
- 4. Bartosh RA, Saldana MJ. Intraarticular fractures of the distal radius: a cadaveric study to determine if ligamentotaxis restores radiopalmar tilt. J Hand Surg Am. 1990;15:18-21. [DOI] [PubMed] [Google Scholar]
- 5. Bini A, Surace MF, Pilato G. Complex articular fractures of the distal radius: the role of closed reduction and external fixation. J Hand Surg Eur Vol. 2008;33:305-310. [DOI] [PubMed] [Google Scholar]
- 6. Capo JT, Rossy W, Henry P, et al. External fixation of distal radius fractures: effect of distraction and duration. J Hand Surg Am. 2009;34:1605-1611. [DOI] [PubMed] [Google Scholar]
- 7. Deepak C, Gopalakrishna G, Ravoof A, et al. Surgical management of distal end radius fractures by ligamentotaxis. Int J Health Sci Res. 2014;4:106-110. [Google Scholar]
- 8. DePalma AF. Comminuted fractures of the distal end of the radius treated by ulnar pinning. J Bone Joint Surg Am. 1952;24:651-662. [PubMed] [Google Scholar]
- 9. Diaz-Garcia RJ, Oda T, Shauver MJ, et al. A systematic review of outcomes and complications of treating unstable distal radius fractures in the elderly. J Hand Surg Am. 2011;36:824-835.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Frank CB. Ligament structure, physiology and function. J Musculoskelet Neuronal Interact. 2004;4:199-201. [PubMed] [Google Scholar]
- 11. Fu YC, Chien SH, Huang PJ, et al. Use of an external fixation combined with the buttress-maintain pinning method in treating comminuted distal radius fractures in osteoporotic patients. J Trauma. 2006;60:330-333. [DOI] [PubMed] [Google Scholar]
- 12. Gradl G, Jupiter JB, Gierer P, et al. Fractures of the distal radius treated with a nonbridging external fixation technique using multiplanar K-wires. J Hand Surg Am. 2005;30:960-968. [DOI] [PubMed] [Google Scholar]
- 13. Hayes AJ, Duffy PJ, McQueen MM. Bridging and non-bridging external fixation in the treatment of unstable fractures of the distal radius: a retrospective study of 588 patients. Acta Orthop. 2008;79:540-547. [DOI] [PubMed] [Google Scholar]
- 14. Kaempffe FA, Walker KM. External fixation for distal radius fractures: effect of distraction on outcome. Clin Orthop Relat Res. 2000;380:220-225. [DOI] [PubMed] [Google Scholar]
- 15. Kumbaraci M, Kucuk L, Karapinar L, et al. Retrospective comparison of external fixation versus volar locking plate in the treatment of unstable intra-articular distal radius fractures. Eur J Orthop Surg Traumatol. 2014;24:173-178. [DOI] [PubMed] [Google Scholar]
- 16. Lin C, Sun JS, Hou SM. External fixation with or without supplementary intramedullary Kirschner wires in the treatment of distal radial fractures. Can J Surg. 2004;47:431-437. [PMC free article] [PubMed] [Google Scholar]
- 17. Margaliot Z, Haase SC, Kotsis SV, et al. A meta-analysis of outcomes of external fixation versus plate osteosynthesis for unstable distal radius fractures. J Hand Surg Am. 2005;30:1185-1199. [DOI] [PubMed] [Google Scholar]
- 18. Papadonikolakis A, Shen J, Garrett JP, et al. The effect of increasing distraction on digital motion after external fixation of the wrist. J Hand Surg Am. 2005;30:773-779. [DOI] [PubMed] [Google Scholar]
- 19. Putnam MD, Fischer MD. Treatment of unstable distal radius fractures: methods and comparison of external distraction and ORIF versus external distraction-ORIF neutralization. J Hand Surg Am. 1997;22:238-251. [DOI] [PubMed] [Google Scholar]
- 20. Raju P, Kini SG. Loss of correction in unstable comminuted distal radius fractures with external fixation and bone grafting—a long term followup study. J Orthop Surg Res. 2011;6:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Richard MJ, Wartinbee DA, Riboh J, et al. Analysis of the complications of palmar plating versus external fixation for fractures of the distal radius. J Hand Surg Am. 2011;36:1614-1620. [DOI] [PubMed] [Google Scholar]
- 22. Wei DH, Poolman RW, Bhandari M, et al. External fixation versus internal fixation for unstable distal radius fractures: a systematic review and meta-analysis of comparative clinical trials. J Orthop Trauma. 2012;26:386-394. [DOI] [PubMed] [Google Scholar]
- 23. Winemaker MJ, Chinchalkar S, Richards RS, et al. Load relaxation and forces with activity in Hoffman external fixators: a clinical study in patients with Colles’ fractures. J Hand Surg Am. 1998;23:926-932. [DOI] [PubMed] [Google Scholar]
- 24. Xie X, Qin H, Shen L, et al. Comparison of internal and external fixation of distal radius fractures. Acta Orthop. 2013;84:286-291. [DOI] [PMC free article] [PubMed] [Google Scholar]