Abstract
Objective
Discrimination is posited to underlie racial disparities in hypertension. Extant literature suggests a possible association between racial discrimination and blood pressure, although inconsistent findings have been reported. The aim of this comprehensive systematic review was to quantitatively evaluate the association between perceived racial discrimination with hypertensive status and systolic, diastolic, and ambulatory blood pressure.
Method
Electronic database search of PubMed and PsycINFO (keywords: blood pressure/hypertension/diastolic/systolic, racism/discrimination/prejudice/unfair treatment) was combined with descendancy and ascendancy approaches. Forty-four articles (N = 32,651) met inclusion criteria. Articles were coded for demographics, hypertensive diagnosis, blood pressure measurement, discrimination measure and constructs, study quality, and effect sizes.
Results
Random effects meta-analytic models were tested based on Fisher’s Z, the derived common effect size metric. Overall, perceived racial discrimination was associated with hypertensive status, Zhypertension = 0.048, 95% CI [.013, .087], but not with resting blood pressure, Zsystolic = 0.011, 95% CI [−.006, .031], Zdiastolic = .016, 95% CI [−.006, .034]. Moderators that strengthened the relation included sex (male), race (Black), age (older), education (lower), and hypertensive status. Perceived discrimination was most strongly associated with nighttime ambulatory blood pressure, especially among Blacks.
Conclusions
Despite methodological limitations in the existing literature, there was a small, significant association between perceived discrimination and hypertension. Future studies should consider ambulatory nighttime blood pressure, which may more accurately capture daily variation attributable to experienced racial discrimination. Perceived discrimination may partly explain racial health disparities.
Keywords: hypertension, blood pressure, racial discrimination, meta-analysis, racial disparities
Hypertension is markedly more prevalent among Blacks than Whites (42% vs. 28.8%), with racial health disparities documented for decades (e.g., Burt et al., 1995; Centers for Disease Control and Prevention, 2011). Among Blacks, hypertension has an earlier age of onset, with greater severity, and is associated with greater pressure related target-organ damage and higher cause-attributable mortality, compared with Whites (American Heart Association, 2005; Ferdinand & Armani, 2007). Blacks typically present with higher risk profiles, including obesity, physical inactivity, cigarette smoking, excess sodium, low socioeconomic status, limited access to quality health care, family history of cardiovascular disease, and stress (Crimmins, Kim, Alley, Karlamangla, & Seeman, 2007). However, these risk factors alone do not adequately account for observed racial differences (Cornoni-Huntley, LaCroix, & Havlik, 1989). Racial discrepancies persist even after controlling for socioeconomic status (Hayward, Crimmins, Miles, & Yang, 2000). Moreover, researchers have failed to demonstrate any risk factors that are biologically unique to Blacks, despite extensive focus on genetics (Hertz, Unger, Cornell, & Saunders, 2005). In fact, the Black–White disparity in hypertension is less consistent when considered internationally (Cooper et al., 2005), which further challenges the role of biological mechanisms as a plausible explanation. Together, these findings have led researchers to consider other psychosocial and environmental factors that may explain the observed hypertension disparities, namely, racial discrimination and racial segregation.
Shifting from biological explanations, researchers have increasingly focused on social aspects of racism, including discrimination and segregation, that may better account for the racial disparities in hypertension observed among industrialized countries (Brondolo, Brady ver Halen, Pencille, Beatty, & Contrada, 2009; Goodman, 2000; Mujahid, Diez Roux, Cooper, Shea, & Williams, 2011; White et al., 2011). Racial discrimination leads to inequitable access to social, educational, and material resources that have both direct and indirect effects on health status (Adler & Rehkopf, 2008; Adler & Snibbe, 2003; Gallo & Matthews, 2003). Racial discrimination has been associated with a range of poorer health outcomes including respiratory conditions, diabetes (Karlsen & Nazroo, 2002), somatic complaints (Bowen-Reid & Harrell, 2002), and chronic health conditions (Finch, Kolody, & Vega, 2000; Gee, Spencer, Chen, & Takeuchi, 2007). Perceived discrimination has been posited to be an underlying determinant of racial disparities in hypertension.
The predominant theoretical explanation linking perceived discrimination and hypertension is conceptually grounded in the cardiovascular reactivity hypothesis (Krantz & Manuck, 1984). Perceptions of racial discrimination are stressful life experiences (Clark, Anderson, Clark, & Williams, 1999) that create emotional distress (Landrine, Klonoff, Corral, Fernandez, & Roesch, 2006) and serve as a potent psychosocial stressor (Brondolo, Gallo, & Myers, 2009). Studies that experimentally simulate exposure to racism (e.g., films depicting racism; harassment by confederates) have found that racist stimuli provoke greater reactivity among Blacks than nonracist stimuli (Fang & Myers, 2001; Guyll, Matthews, & Bromberger, 2001; McNeilly et al., 1995; Sutherland & Harrell, 1986). Blacks who report past experiences with racism also exhibit exaggerated blood pressure reactivity (Clark, 2000). These findings largely support the tenet of reactivity linking racism as a stressor with heightened blood pressure.
Previous literature reviews suggest a plausible relation between discrimination and health. Although several reviews discuss the relation broadly across multiple health outcomes (e.g., physical health; Pascoe & Smart Richman, 2009; Williams & Mohammed, 2009), Brondolo and colleagues focus exclusively on blood pressure and hypertension. In 2003, Brondolo, Rieppi, Kelly, and Gerin (2003) found the extant literature was “mixed and inconsistent” and elucidated methodological limitations that obscure the relation between perceived discrimination and hypertension. More recently, Brondolo, Love, Pencille, Schoenthaler, and Ogedegbe (2011) described the relation as “weak, but small” and suggested findings are more consistent with ambulatory blood pressure and institutional forms of racism. Others have concluded the association is “complex and unclear” (Williams & Mohammed, 2009) or alluded to such (Paradies, 2006). However, these conclusions are predominantly based on pooled findings of hypertensive status and blood pressure measurement. Drawbacks of qualitative reviews include the focus on statistical significance and use of “vote count” methods, in which an entire study is categorized as having a positive, negative, or null relation; rarely is the magnitude of the association considered nor is the contribution of the moderator quantified. Quantitative reviews, or meta-analyses, aim to address these shortcomings by examining the pattern (direction and magnitude) of evidence across studies to derive a cumulative effect, the consistency of effect sizes, and the contribution of moderators. Some previous reviews discussed moderators in the relation between perceived discrimination and hypertension, including coping style or social support (J. P. Harrell, Hall, & Taliaferro, 2003; Pascoe & Smart Richman, 2009); discrimination time frame, type, number of items, or psychometric quality (Paradies, 2006; Pascoe & Smart Richman, 2009); stress (Williams & Mohammed, 2009); obesity and smoking (Brondolo et al., 2011); and socioeconomic status (Brondolo et al., 2003; 2011). However, the extent to which these moderators affect the relation between study features and effect sizes is unknown. In the only quantitative review, Pascoe and Smart Richman (2009) conducted a meta-analysis of perceived discrimination and multiple health outcomes. Although blood pressure was included within the 36 physical health outcome studies, only 12 had blood pressure outcomes, including two that reported redundant results; thus, the review did not systematically include relevant findings from several other blood pressure and hypertension studies. Taken together, a comprehensive, quantitative review of current research remains to be completed.
The aim of the present systematic review was to quantitatively examine the association between racism and hypertension. Specifically, a meta-analysis was conducted to ascertain the size and magnitude of the effect between perceived discrimination with hypertensive status as well as resting systolic and diastolic blood pressure. Further, the roles of individual-level (e.g., age, sex, socioeconomic status, social support, body mass index, smoking status) and methodological (e.g., perceived discrimination measure, hypertensive diagnosis, blood pressure assessment) factors in moderating the associations were evaluated.
Method
Selection of Studies
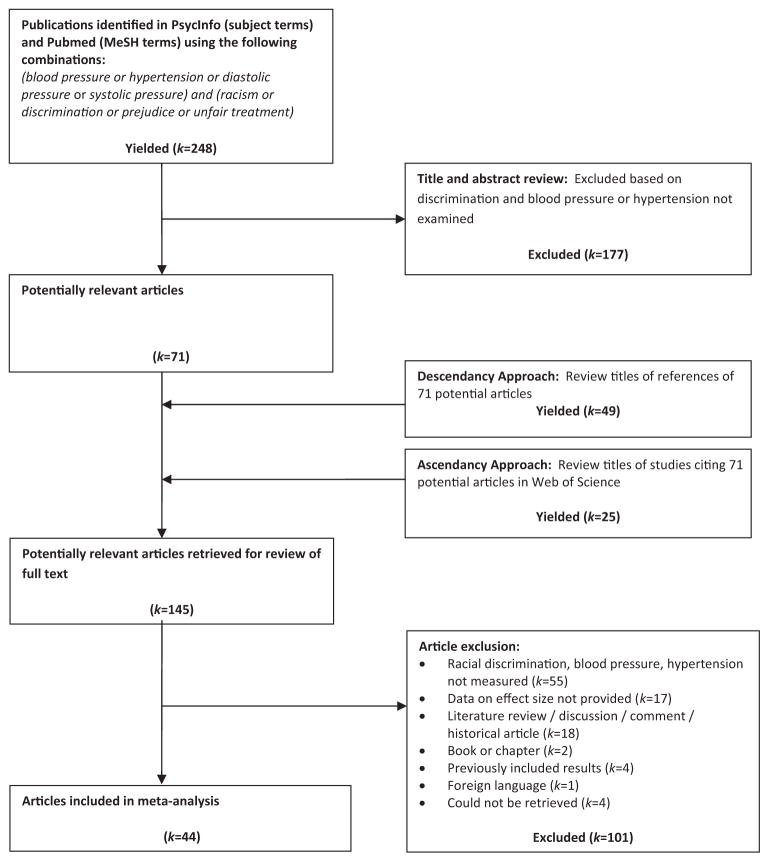
Studies were identified through literature searches of PsycINFO and PubMed electronic databases for the years 1970 to March 2012 (see Figure 1) using keywords (blood pressure/hypertension/diastolic/systolic and racism/discrimination/prejudice/unfair treatment). For the 248 initially identified studies, all titles and abstracts were reviewed; the level of agreement between two independent coders was high (κ = .91); in cases of disagreement, the article was retained for further consideration. Next, ascendancy and descendancy approaches were used to identify additional articles. Finally, letters of solicitation were sent to authors who published two or more articles on the topic, requesting possible data from unpublished manuscripts, including nonsignificant findings. Researchers’ suggestions did not pertain to any nonredundant data. A total of 145 potentially relevant studies were identified for full review. Upon completed review, 44 articles were included in the meta-analysis (see Figure 1 for literature search strategy).
Figure 1.
Flow chart for article identification and inclusion.
Article Coding
Sample size, demographic information (e.g., age, sex, income, education, marital status), physical health characteristics (e.g., smoking), body mass index (BMI), methodology (e.g., recruitment, inclusion/exclusion criteria), blood pressure measurement, hypertensive status definition, discrimination measure, study quality, outcome measures, and effect sizes were coded by a single rater (C.D.). For each study, approximately 50 coding decisions were made. To ensure there was no coding drift, a random sample (10%) of the initially coded studies was blindly recoded after an 18 months delay; intrarater agreement was excellent, ICC = .99, 95% CI [.996, .999]. A second coder (A.H.) independently coded another random sample (10%); interrater agreement was excellent, ICC = .985, 95% CI [.956, .995].
Perceived Discrimination
Measure
Three standardized instruments are commonly used to assess discrimination. The Perceived Racism Scale (McNeilly et al., 1996) measures interpersonal and institutional racism during the past year and lifetime. The Everyday Discrimination Scale (Williams, Yu, Jackson, & Anderson, 1997) measures everyday experiences of interpersonal discrimination and includes an item about the nature of the discrimination. The Experiences of Discrimination (Krieger & Sidney, 1996; Krieger, 1990) measures interpersonal and institutional discrimination across seven domains (e.g., school, work, obtaining housing). “Other Standardized Measures” included less frequently used standardized measures, including the Racism and Life Experiences Scale (S. P. Harrell, 1997; S. P. Harrell, Merchant, & Young, 1997), the Perceived Ethnic Discrimination Questionnaire-Community Version (Brondolo et al., 2005), the Oppression Questionnaire (Victoroff, 2005), and the Nadanolitization Scale (Taylor & Grundy, 1996); these were grouped for comparison purposes. Adaptations of these measures (i.e., reworded questions, changed response options) were coded with the original measure. (See Bond et al., 2007, for psychometric properties of standardized discrimination measures.) Finally, “Researcher-Defined Questions” was coded for singular or limited questions (e.g., “Have you ever felt badly treated because of your race?”).
Constructs
Item analysis of each study’s discrimination measure, to accurately capture nuanced modifications and adaptations in wording, was used to code three underlying constructs: nature, type, and time frame. Nature of the discrimination measure was coded as either “Racism” (items specifically racially oriented) or “Discrimination (nonspecific)” (items more generally about discrimination, not directly attributable to race). Type was coded as either “Interpersonal” (items pertained to interactions between individuals) or “Institutional-setting” (items specifically referred to place or setting; e.g., hospital, workplace). Time frame was coded either as “Past year” or “Lifetime.”
Hypertension
Hypertensive status
Hypertensive status was coded “Physician Diagnosis/Medication” if diagnosis was confirmed by medical chart review, or if participants reported a physician diagnosis or use of prescribed hypertension medications. Self-report of physician diagnosis has been found to be reliable against medical record (Alonso, Beunza, Delgado-Rodríguez, & Martínez-González, 2005). Alternatively, “Measured Blood Pressure” was coded if hypertension was defined as measured values exceeding 40/90 mmHg on a single clinic visit (no study reported taking readings on more than one occasion).
Resting blood pressure
Blood pressure readings taken in a laboratory or clinic, as well as daytime-only ambulatory recordings, were coded for resting blood pressure. Number of readings and assessment method (oscillometric vs. ausculatory) were also coded.
Ambulatory blood pressure
For studies reporting ambulatory data, nighttime only, 24-hour, and nighttime dipping blood pressure were coded. These effect sizes were treated separately and not included in the resting blood pressure analyses.
Effect Size Calculation
Effect size calculations were guided by previously reported procedures (Cooper & Hedges, 1994). Fisher’s Z was designated as the common effect size metric across studies; values range from −∞ to +∞, and it is interpreted similar to a correlation. Fisher’s Z is advantageous as data may be converted from almost any test statistic (Rosenthal, 1991). Bivariate correlations were converted using Fisher’s variance stabilizing transformation (Cooper, 1998). Test statistics (e.g., t test, F statistic) were converted into r and then into Fisher’s Z, using formulas reported elsewhere (Cooper & Hedges, 1994). Unstandardized beta coefficients were converted to t-test statistics; standardized regression coefficients were appropriately weighted (Peterson & Brown, 2005). Zero-order correlations were coded; when partial correlations were coded, the number of covariates was also recorded. Dichotomized outcomes (e.g., odds ratio) were transformed into Cohen’s d, and then converted to Fisher’s Z (Chinn, 2000; Sánchez-Meca, Marín-Martínez, & Chacón-Moscoso, 2003). When test statistic data were not reported, effect sizes were derived from exact p values using distribution tables (Lindley & Scott, 1984). If a comparison was described as “nonsignificant,” an effect size of zero was used as a conservative estimate. Finally, if no statistical values were provided and no information was given regarding significance, the comparison was not included in the analysis.
Data Reduction
Effect sizes were coded for all available and relevant data reported within each article, thus yielding multiple effect sizes per study. Of the 44 articles included, there were a total of 167 effect sizes, for an average of 3.80 effect sizes per study. Stochastic dependencies, which can influence effect size estimates and their precision, are attributable to different effect sizes calculated on the same participants using different measures (e.g., hypertension and resting blood pressure), different samples within the same study (e.g., Blacks, Hispanics, Whites), or several studies reported by the same researchers. Thus, two analytical strategies were employed. First, nonredundant effect sizes were parsed from each study as a conservative approach. If identical participants were incorporated in more than one effect size, the average of the redundant effect sizes was used. Second, because the first strategy has been criticized as being overly conservative and not maximizing power by retaining all available data, analyses were also conducted on the aggregate of all coded effect sizes (see Post Hoc Analyses below).
Analytic Strategy
Random-effects meta-analytic models were used to evaluate the association between perceived racial discrimination and hypertension. Random effects models assume the samples are drawn from populations with different effect sizes. The true effect may differ across studies because of different participant characteristics, measurement of discrimination, or outcome variables (blood pressure vs. hypertensive status). Random-effects models are generally regarded as more accurate than fixed-effects models, which typically yield overly narrow confidence intervals (Schmidt, Oh, & Hayes, 2009).
An analysis of heterogeneity (QT) was conducted for each meta-analysis. This heterogeneity statistic is a measure of variation for included effect sizes; nonsignificant QT indicates the variability is less than expected from sampling error. Distributions found to be heterogeneous (significant QT) generally warrant additional moderator analyses. Separate analyses were conducted for all a priori specified moderator variables, including age, sex, ethnicity, marital status, socioeconomic status (SES), body mass index (BMI), smoking status, hypertensive status, discrimination measure and constructs, and blood pressure assessment. Bootstrap methods (1,000 samples) were used to produce nonparametric estimates of confidence intervals about each effect size. To address concerns about possible publication bias and the file drawer problem, Orwin’s (1983) fail-safe numbers were calculated to determine the number of nonsignificant, unpublished, or missing comparisons that would be needed to make the overall effect negligible or not different than zero. Analyses were conducted using MetaWin (Version 2; Rosenberg, Adams, & Gurevitch, 2000).
Results
Study and Participant Characteristics
Of the 44 included studies, there was an average of 742 participants (SD = 1,125) per study, permitting an adequately powered test of a small effect size. Participants were young adults (38.0 years), 46.7% married, and 32.8% male (see Table 1). Samples across all studies were 62.2% Black, 13.6% White, 11.8% Hispanic, and 12.4% Other (e.g., Aboriginal, Asian, Indian, Pakistani, Mixed). Samples were largely low SES ($26,889), 15.93% high school education or less, overweight (BMIavg = 27.4), and 14.9% smokers. Few participants were hypertensive (24.2%) or used prescribed hypertensive medication (6.6%). Participants were largely recruited from community settings (72%) throughout the United States: Midwest (20%), South (20%), Northeast (15%), or West (10%; data not shown).
Table 1.
Descriptive Characteristics and Frequencies of 44 Studies Included
| Characteristic | k | N | Minimum | Maximum | M (SD) |
|---|---|---|---|---|---|
| Age (years) | 41 | 28,761 | 9.5 | 74.1 | 38.25 (15.22) |
| Sex (% male) | 43 | 30,144 | 0.0 | 100.0 | 32.75% (20.05) |
| Ethnicity (% Black) | 44 | 32,651 | 0.0 | 100.0 | 62.61% (39.86) |
| Marital status (% married) | 14 | 12,725 | 12.0 | 100.0 | 46.69% (23.12) |
| SES | |||||
| Household income ($) | 12 | 3,886 | 7,000.0 | 43,942.0 | 26,889 (13,094) |
| Education (% HS degree or less) | 28 | 23,922 | 0.0 | 58.0 | 15.93% (18.31) |
| BMI kg/m2 | 27 | 18,927 | 22.4 | 30.7 | 27.41 (2.23) |
| Smoking (% smokers) | 16 | 8,898 | 0.0 | 48.6 | 14.85% (12.83) |
| Hypertensive status | |||||
| Hypertensive (% diagnosed) | 32 | 22,414 | 0.0 | 71.0 | 24.21% (24.21) |
| Prescribed medication (% taking) | 22 | 16,346 | 0.0 | 44.4 | 6.60% (11.82) |
| Blood pressure | |||||
| SBP resting mmHg | 27 | 19,754 | 103.6 | 135.3 | 120.71 (9.60) |
| DBP resting mmHg | 27 | 19,754 | 59.0 | 82.9 | 73.05 (7.38) |
| No. laboratory BP readings | 22 | 18,415 | 2.0 | 9.0 | 2.91 (1.60) |
Note. SES = socioeconomic status; HS = high school; BMI = body mass index; SBP = systolic blood pressure; DBP = diastolic blood pressure; BP = blood pressure. Minimum and maximum values reported only for those studies providing the corresponding descriptive statistic.
Resting blood pressure was typically measured using the oscillometric method (32.5%) in a lab or clinic (80%) by a trained nurse or research assistant (35%; data not shown). Average resting blood pressure values largely fell within the normal range (121/73 mmHg). Hypertensive status was typically self-report of physician diagnosis or prescribed medication (65%). Perceived discrimination was assessed using the Perceived Racism Scale (15%), Experiences of Discrimination (15%), Everyday Discrimination Scale (20%), Other Standardized Measures (20%), or Researcher-Defined Questions (20%; data not shown).
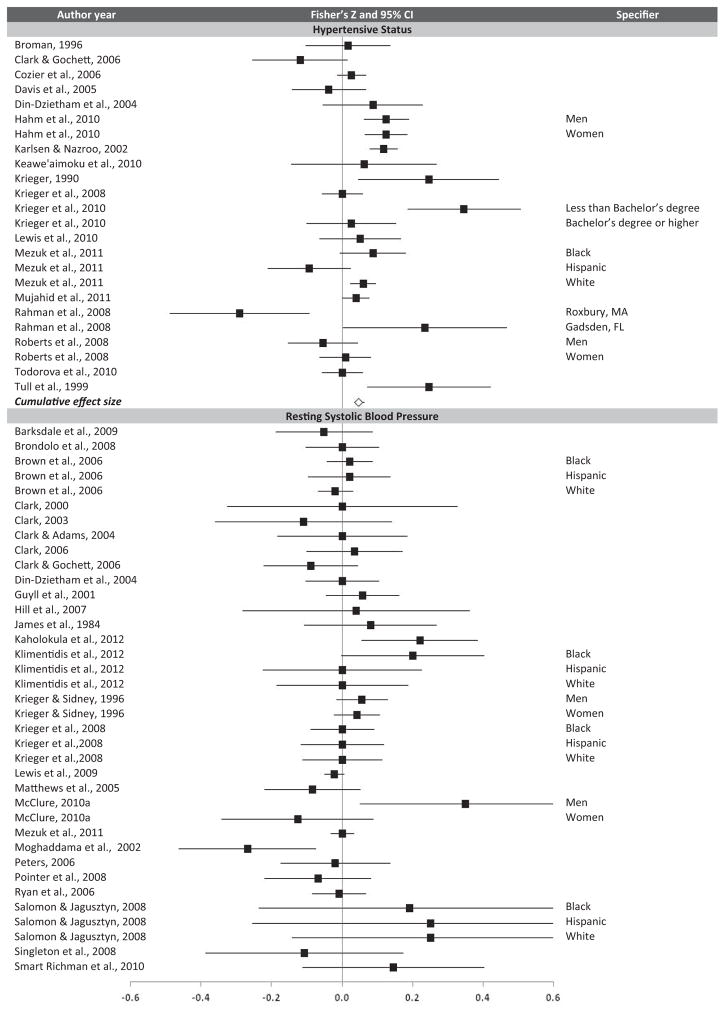
Hypertensive Status and Perceived Racial Discrimination
Hypertensive status and discrimination were reported in 18 studies with 24 nonredundant effect sizes (see Table 2 and Figure 2). The average cumulative effect size indicated a small relation, as greater perceived discrimination was associated with hypertensive status. This cumulative effect size was heterogeneous, warranting further moderator analyses. The observed relation between discrimination and hypertensive status was significant and stronger for effect sizes based on older participants, higher percent males, Blacks only, higher percent Blacks, lower educational attainment, and more hypertensives. Studies using physician diagnosis/medication use, the Everyday Discrimination Scale, and nonspecific nature measures of discrimination also yielded significant, positive cumulative effect sizes. Notably, about half of the heterogeneity statistics for the above analyses were significant, suggesting additional moderators exist.
Table 2.
Hypertensive Status and Discrimination (Random Effects Models)
| Comparison | Effect sizes | N | Fisher Z | Bootstrap 95% CI | QT | Fail-safe n |
|---|---|---|---|---|---|---|
| All studies | 24 | 18,987 | .048 | (.013, .087) | 40.413* | 1132 |
| Moderators | ||||||
| Age | 20 | 15,097 | .053 | (.009, .096) | 34.991* | 1032 |
| Sex (% male) | 23 | 16,480 | .044 | (.008, .085) | 38.004* | 978 |
| Ethnicity | ||||||
| Black only | 13 | 6,312 | .045 | (.002, .102) | 18.605 | 578 |
| Hispanic only | 2 | 1,404 | −.033 | (−.094, .000) | 1.000 | 0 |
| White only | — | — | — | — | — | — |
| % Black | 24 | 18,987 | .048 | (.012, .087) | 40.205* | 1133 |
| Marital status (% married) | 10 | 8,220 | .026 | (−.041, .084) | 11.681 | 249 |
| SES | ||||||
| Household income | 4 | 1,892 | −.018 | (−.078, .049) | 2.328 | 0 |
| Education (% HS degree or less) | 21 | 16,325 | .051 | (.012, .093) | 33.677* | 1041 |
| BMI | 9 | 7,643 | .032 | (−.018, .074) | 13.107 | 278 |
| Smoking (% smokers) | 12 | 7,259 | .053 | (−.014, .130) | 20.337* | 624 |
| Hypertensive status | ||||||
| % hypertensive | 22 | 16,398 | .051 | (.009, .095) | 41.085 | 1100 |
| % taking medication | 6 | 5,317 | .024 | (−.055, .105) | 7.286 | 138 |
| HTN assessment | ||||||
| Physician diagnosis/medication (self-report) | 15 | 10,727 | .072 | (.025, .118) | 23.729* | 1076 |
| Measured blood pressure (>140/90 mmHg) | 9 | 8,260 | .014 | (−.036, .059) | 12.984 | 119 |
| Discrimination assessment | ||||||
| Discrimination measure | ||||||
| Perceived Racism Scale | — | — | — | — | — | — |
| Experiences of Discrimination | 8 | 2,365 | .047 | (−.002, .090) | 9.706 | 369 |
| Everyday Discrimination Scale | 7 | 8,170 | .060 | (.020, .100) | 6.825 | 416 |
| Other standardized measure | 6 | 4,467 | .045 | (−.013, .125) | 7.017 | 266 |
| Researcher-defined questions | 3 | 3,985 | .034 | (−.034, .119) | 1.734 | 98 |
| Nature of discrimination | ||||||
| Racism | 15 | 9,086 | .053 | (−.007, .120) | 25.604* | 786 |
| Discrimination (nonspecific) | 9 | 9,901 | .049 | (.007, .087) | 10.866 | 433 |
| Discrimination type | ||||||
| Interpersonal (nonspecific) | 11 | 10,315 | .041 | (−.003, .083) | 13.809 | 439 |
| Institutional setting | 3 | 1,496 | .055 | (.000, .250) | 2.904 | 164 |
| Discrimination time frame | ||||||
| Lifetime | 16 | 9,796 | .041 | (−.011, .093) | 27.100* | 639 |
| Past year | 5 | 6,549 | .054 | (−.009, .096) | 5.445 | 266 |
| Blacks only | ||||||
| Moderators | ||||||
| Education (% HS degree or less) | 10 | 3,650 | .050 | (.055, .117) | 11.635 | 491 |
| Smoking (% smokers) | 5 | 1,329 | .114 | (.044, .229) | 4.410 | 565 |
| Physician diagnosis/medication (self-report) | 7 | 4,016 | .075 | (.032, .155) | 8.839 | 516 |
| Experiences of discrimination | 3 | 670 | .128 | (.016, .360) | 2.370 | 380 |
| Other standardized measure | 3 | 1,043 | .096 | (.008, .250) | 2.103 | 286 |
| Past year | 3 | 1,294 | .064 | (.016, .087) | 0.868 | 190 |
Note. Significant effects are bolded; effect sizes refers to number of nonredundant effect sizes; fail-safe n using Orwin’s method; cells with a dash = not applicable due to limited number of effect sizes. QT = heterogeneity test statistic; SES = socioeconomic status; HS = high school; BMI = body mass index; HTN = hypertension.
p < .05.
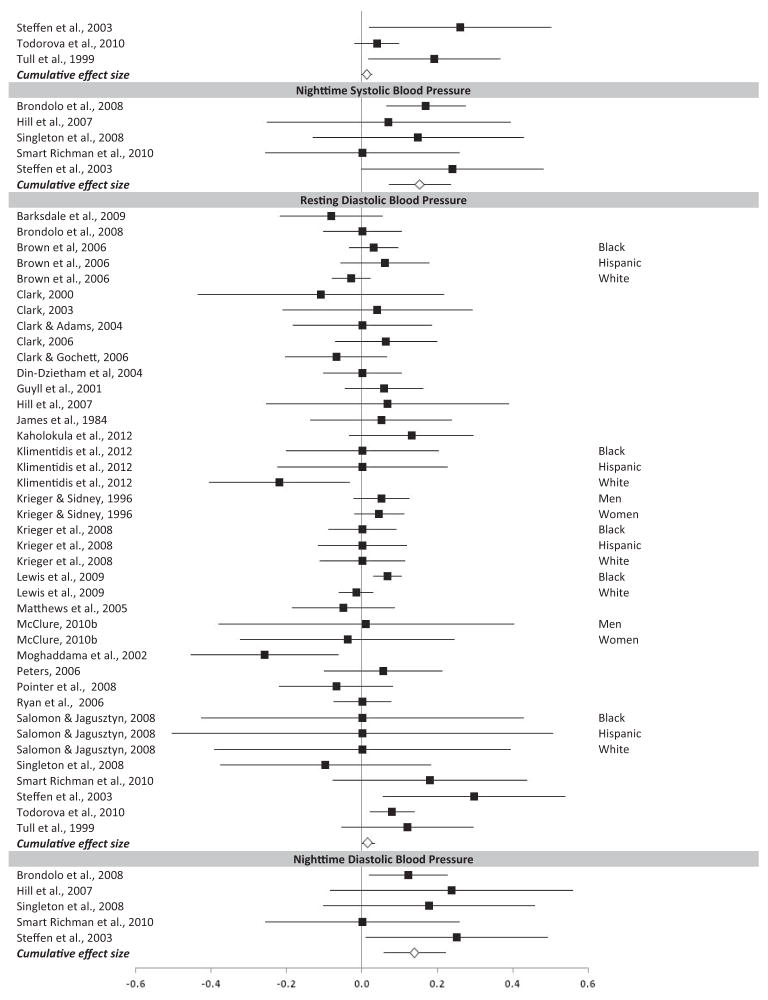
Figure 2.
Forest Plot of Effect Sizes for Perceived Racial Discrimination and Hypertension (Hypertensive Status, Resting Systolic Blood Pressure, Nighttime Systolic Blood Pressure, Resting Diastolic Blood Pressure, Nighttime Diastolic Blood Pressure).
Systolic Blood Pressure and Perceived Racial Discrimination
The relation between resting systolic blood pressure and discrimination was reported in 30 studies and yielded 40 nonredundant effect sizes. The average cumulative effect size did not significantly differ from zero (see Table 3 and Figure 2). A priori moderator analyses revealed that effect sizes based on samples with more smokers and institutional-setting type discrimination measures yielded significant, positive associations between resting blood pressure and discrimination. When ambulatory blood pressure was considered separately (i.e., not included in cumulative analyses), nighttime systolic blood pressure was significantly associated with discrimination; this was the largest effect size observed.
Table 3.
Resting Systolic Blood Pressure and Discrimination (Random Effects Models)
| Comparison | Effect sizes | N | Fisher Z | Bootstrap 95% CI | QT | Fail-safe n |
|---|---|---|---|---|---|---|
| All studies | 40 | 19,449 | .011 | (−.006, .031) | 46.001 | 407 |
| Moderators | ||||||
| Age | 38 | 17,812 | .007 | (−.011, .028) | 43.670 | 244 |
| Sex (% male) | 40 | 19,449 | .011 | (−.006, .032) | 45.474 | 416 |
| Ethnicity | ||||||
| Black only | 20 | 5,139 | .023 | (−.005, .049) | 19.589 | 444 |
| Hispanic only | 7 | 1,922 | .029 | (−.016, .090) | 7.304 | 197 |
| White only | 4 | 1,991 | −.012 | (−.019, .052) | 1.945 | 0 |
| % Black | 40 | 19,449 | .012 | (−.007, .031) | 45.263 | 420 |
| Marital status (% married) | 11 | 8,971 | .007 | (−.024, .037) | 14.608 | 64 |
| SES | ||||||
| Household income | 11 | 3,431 | .006 | (−.029, .032) | 4.324 | 51 |
| Education (% HS degree or less) | 23 | 16,005 | .007 | (−.012, .033) | 30.145 | 144 |
| BMI | 28 | 14,945 | .007 | (−.012, .030) | 33.159 | 130 |
| Smoking (% smokers) | 15 | 7,715 | .012 | (.002, .038) | 9.938 | 160 |
| Hypertensive status | ||||||
| % hypertensive | 30 | 11,953 | .007 | (−.005, .023) | 26.433 | 190 |
| % taking medication | 31 | 15,738 | −.005 | (−.015, .014) | 28.903 | 0 |
| Clinic/laboratory/school | 35 | 18,727 | .013 | (−.004, .036) | 40.549 | 406 |
| No. of readings | 28 | 15,662 | .012 | (−.006, .038) | 28.172 | 270 |
| Ambulatory BP | ||||||
| Daytime | 6 | 791 | .034 | (−.054, .172) | 5.586 | 200 |
| Nighttimea | 5 | 579 | .153 | (.038, .193) | 2.275 | 761 |
| 24 hra | 4 | 561 | .043 | (−.096, .082) | 2.900 | 167 |
| Dippinga | 3 | 517 | −.129 | (−.244, .020) | 2.195 | 0 |
| Discrimination assessment | ||||||
| Discrimination measure | ||||||
| Perceived Racism Scale | 6 | 584 | −.007 | (−.067, .109) | 5.107 | 0 |
| Experiences of Discrimination | 5 | 2,716 | .029 | (.000, .044) | 1.564 | 139 |
| Everyday Discrimination Scale | 16 | 12,683 | −.004 | (−.018, .016) | 15.261 | 0 |
| Other standardized measure | 8 | 1,493 | .034 | (−.018, .106) | 7.656 | 266 |
| Researcher-defined questions | 6 | 2,136 | −.005 | (−.117, .094) | 9.382 | 0 |
| Nature of discrimination | ||||||
| Racism | 29 | 7,268 | .017 | (−.013, .047) | 33.911 | 471 |
| Discrimination (nonspecific) | 11 | 12,181 | −.006 | (−.019, .022) | 10.134 | 0 |
| Discrimination type | ||||||
| Interpersonal (nonspecific) | 19 | 13,170 | .001 | (−.015, .025) | 20.605 | 0 |
| Institutional setting | 4 | 2,871 | .046 | (.040, .060) | 0.275 | 178 |
| Discrimination time frame | ||||||
| Lifetime | 30 | 14,671 | .007 | (−.010, .033) | 32.452 | 190 |
| Past year | 9 | 4,504 | .012 | (−.032, .085) | 9.482 | 140 |
| Blacks only | ||||||
| Moderators | ||||||
| Smoking (% smokers) | 7 | 1,138 | .021 | (.001, .121) | 5.013 | 137 |
| Nighttime ABP | 3 | 161 | .171 | (.070, .245) | 0.759 | 511 |
| Experiences of discrimination | 3 | 2,103 | .037 | (.000, .056) | 0.949 | 107 |
| Institutional setting | 3 | 1,749 | .050 | (.048, .080) | 0.196 | 147 |
Note. Significant effects are bolded; effect sizes refers to number of nonredundant effect sizes; fail-safe n using Orwin’s method. QT = heterogeneity test statistic; SES = socioeconomic status; HS = high school; BMI = body mass index; BP = blood pressure; ABP = ambulatory blood pressure.
p < .05.
Not included in resting blood pressure analyses.
Diastolic Blood Pressure and Perceived Racial Discrimination
The relation between resting diastolic blood pressure and discrimination was reported in 29 studies, with 40 nonredundant effect sizes. The average cumulative effect size did not significantly differ from zero (see Table 4 and Figure 2). A priori moderator analyses revealed that for effect sizes based solely on Blacks and institutional-setting type discrimination measures, there were positive, significant relations between resting diastolic blood pressure and discrimination. There was a negative relation for effect sizes calculated solely on Whites. Select discrimination measures also yielded significant effects. When ambulatory blood pressure was considered separately, nighttime diastolic blood pressure and dipping were significantly associated with discrimination; these were the largest effect sizes observed.
Table 4.
Resting Diastolic Blood Pressure and Discrimination (Random Effects Models)
| Comparison | Effect sizes | N | Fisher Z | Bootstrap 95% CI | QT | Fail-safe n |
|---|---|---|---|---|---|---|
| All studies | 40 | 15,602 | .016 | (−.006, .034) | 37.923 | 597 |
| Moderators | ||||||
| Age | 38 | 13,965 | .013 | (−.011, .034) | 38.014 | 435 |
| Sex (% male) | 40 | 15,602 | .016 | (−.005, .034) | 37.114 | 587 |
| Ethnicity | ||||||
| Black only | 21 | 7,965 | .039 | (.006, .056) | 19.118 | 803 |
| Hispanic only | 7 | 1,869 | .056 | (−.006, .076) | 2.270 | 387 |
| White only | 5 | 3,859 | −.029 | (−.063, −.011) | 4.481 | 0 |
| % Black | 40 | 15,602 | .017 | (−.005, .037) | 39.912 | 622 |
| Marital status (% married) | 10 | 5,177 | .011 | (−.031, .049) | 13.212 | 99 |
| SES | ||||||
| Household income | 11 | 3,378 | .019 | (−.031, .057) | 9.640 | 199 |
| Education (% HS degree or less) | 23 | 12,158 | .018 | (−.007, .043) | 22.221 | 395 |
| BMI | 28 | 11,098 | .015 | (−.010, .047) | 22.858 | 390 |
| Smoking (% smokers) | 14 | 3,921 | .033 | (−.004, .062) | 10.714 | 447 |
| Hypertensive status | ||||||
| % hypertensive | 29 | 8,159 | .012 | (−.014, .041) | 30.570 | 313 |
| % taking medication | 30 | 11,944 | .009 | (−.014, .032) | 28.125 | 237 |
| Clinic/laboratory/school | 33 | 3,200 | .012 | (−.013, .036) | 31.623 | 377 |
| No. of readings | 27 | 11,744 | .019 | (−.010, .047) | 25.379 | 481 |
| Ambulatory BP | ||||||
| Daytime | 6 | 791 | .057 | (−.034, .199) | 5.727 | 337 |
| Nighttimea | 5 | 579 | .138 | (.091, .237) | 2.574 | 687 |
| 24 hra | 4 | 561 | .031 | (−.077, .060) | 2.002 | 119 |
| Dippinga | 3 | 517 | −.139 | (−.266, −.085) | 2.151 | 0 |
| Discrimination assessment | ||||||
| Discrimination measure | ||||||
| Perceived Racism Scale | 6 | 584 | −.009 | (−.088, .121) | 5.292 | 0 |
| Experiences of Discrimination | 6 | 2,878 | .030 | (.005, .046) | 1.618 | 176 |
| Everyday Discrimination Scale | 16 | 8,888 | .010 | (−.021, .039) | 13.166 | 138 |
| Other standardized measure | 7 | 1,331 | .034 | (.004, .082) | 3.275 | 230 |
| Researcher-defined questions | 6 | 2,083 | −.007 | (−.115, .057) | 5.554 | 0 |
| Nature of discrimination | ||||||
| Racism | 29 | 7,215 | .021 | (−.006, .046) | 27.944 | 590 |
| Discrimination (nonspecific) | 11 | 8,387 | .011 | (−.029, .043) | 10.429 | 105 |
| Discrimination type | ||||||
| Interpersonal (nonspecific) | 19 | 9,323 | .009 | (−.021, .039) | 14.875 | 160 |
| Institutional setting | 4 | 2,871 | .060 | (.045, .077) | 0.693 | 236 |
| Discrimination time frame | ||||||
| Lifetime | 31 | 14,671 | .019 | (−.005, .039) | 29.472 | 565 |
| Past year | 8 | 657 | −.070 | (−.131, .002) | 4.408 | 0 |
| Blacks only | ||||||
| Moderators | ||||||
| Sex (% male) | 21 | 7,965 | .039 | (.008, .056) | 18.956 | 788 |
| Nighttime ABP | 3 | 161 | .227 | (.179, .255) | 0.172 | 679 |
| Other standardized measure | 5 | 828 | .032 | (.003, .087) | 1.522 | 152 |
| Institutional setting | 3 | 1,749 | .048 | (.045, .051) | 0.018 | 140 |
| Lifetime | 14 | 7,305 | .041 | (.007, .058) | 13.000 | 555 |
Note. Significant effects are bolded; effect sizes refers to number of nonredundant effect sizes; fail-safe n using Orwin’s method. QT = heterogeneity test statistic; SES = socioeconomic status; HS = high school; BMI = body mass index; BP = blood pressure; ABP = ambulatory blood pressure.
p < .05.
Not included in resting blood pressure analyses.
Post Hoc Analyses
Blacks only
Random effects meta-analytic models were rerun for effect sizes derived from Blacks only (see bottom rows of Tables 2 through 4). There was an overall association for hypertensive status and diastolic blood pressure, based on the cumulative effect sizes. For hypertensive status, moderator analyses revealed the relation was stronger in effect sizes based on samples with lower educational attainment, more smokers, physician diagnosis/medication use, Experiences of Discrimination measure, Other Standardized Measures, and past-year discrimination. For resting systolic blood pressure, significant moderators included smoking, Experiences of Discrimination measure, and institutional-setting type discrimination measures; nighttime ambulatory blood pressure was also significant. For resting diastolic blood pressure, significant moderators included more males, Other Standardized Measures, institutional-setting type discrimination measures, and lifetime time frame discrimination; nighttime ambulatory blood pressure was also significant. All of these QT statistics were nonsignificant, suggesting the cumulative effect sizes were homogenous and do not warrant further parsing. Examination of the fail-safe numbers reveals at least 100 nonsignificant findings are necessary to reduce the observed significant findings to negligible. Across all meta-analytic models, the strongest associations between hypertension and discrimination were observed for nighttime ambulatory blood pressure among Blacks only.
Smoking and socioeconomic status
In addition to testing smoking and education level as moderators at the study sample level, we compared effect sizes that included these as covariates. The overall effect sizes did not differ when socioeconomic status was included as a covariate, for hypertensive status or resting blood pressure, Zcovariate = .033, 95% CI [.014, .068] versus Zzero_order = .024, 95% CI [.002, .051]. When smoking was included as a covariate, resting systolic and diastolic blood pressure were more strongly related to perceived discrimination, Zcovariate = .063, 95% CI [.053, .072] versus Zzero_order = .009 95% CI [−.007, .027]; however, very few studies controlled for smoking. There was no difference when smoking was included as a covariate for hypertensive status.
Study quality
Seven dimensions of study quality were rated dichotomously and summed to yield a quality rating. Dimensions included (a) inclusion/exclusion criteria explicitly described (82%); (b) discrimination measure with established psychometric properties (82%); (c) hypertensive status defined by physician diagnosis/prescription medication use or resting blood pressure assessed by trained professional (68%); (d) sample size greater than 100 participants (77%); (e) statistically controlled for covariates in at least one analysis (70%); (f) test statistic estimates presented (80%); and (g) peer-reviewed journal with impact factor greater than 2 (66%). Effect size was not related to study quality, r = .064, p = .490.
Alternate effect size selection
The aforementioned analyses were based on nonredundant effect sizes, with selection preference for zero-order or bivariate correlations. Largely identical results were obtained when all analyses were rerun with (a) nonredundant effect sizes, selection preference for partial correlations controlling for covariates; (b) redundant effect sizes, including all calculated effect sizes regardless of number contributed per study; and (c) nonredundant effect sizes, averaged to yield only one effect size per study (results not shown for parsimony).
Discussion
Perceived discrimination has been posited to explain observed racial disparities in hypertension. The aim of this comprehensive systematic review was to quantitatively ascertain the strength of the association between perceived racial discrimination and hypertension. There was a significant, albeit small, relation between perceived discrimination and hypertensive status. This relation was stronger among older participants, males, Blacks, lower educational attainment, hypertensives, and physician diagnosis of hypertensive status. The relation was not apparent for resting blood pressure. For resting systolic and diastolic blood pressure, the relation was significant only for institutional-setting type discrimination measures. The largest associations were observed for ambulatory nighttime blood pressure and dipping; this was especially true among Blacks. Overall, there was a small, significant relation between perceived discrimination and hypertensive status, which is more salient among certain subgroups or study features.
Previous narrative reviews also suggest a small and complex relation between racial discrimination and hypertensive status (Brondolo et al., 2011), as determinants at both the individual and contextual levels likely moderate this relation. Individual level differences (e.g., demographics, lifestyle behaviors, social support) have been considered to be important moderators. In the present meta-analysis, age, sex, race, and education moderated at least one association between discrimination and hypertension. With the exception of race, these demographic variables have been underemphasized in prior reviews, with greater attention to other posited moderators. Lifestyle behaviors (e.g., smoking, fitness, alcohol) and weight status (i.e., obesity) have been previously observed as moderators (Brondolo et al., 2011). Smoking was found to moderate the association between perceived discrimination and resting systolic blood pressure only; further, post hoc analyses revealed that in studies that included smoking as a covariate, discrimination was more strongly related to resting blood pressure. Weight status (i.e., BMI) was not found to moderate any association. It was not possible to systematically consider other health behaviors (e.g., fitness, alcohol), due to infrequent and inconsistent reporting in the literature. Prior reviews have primarily considered coping and social support as moderators (e.g., J. P. Harrell et al., 2003; Pascoe & Smart Richman, 2009). The measurement of coping and social support is extremely varied, precluding their inclusion as covariates in the meta-analysis. Marital status, which some consider as a crude proxy of social support, did not moderate the association for any analyses. Finally, contextual-level racial discrimination (e.g., neighborhood racial segregation) has been previously associated with hypertension and blood pressure (e.g., Kershaw et al., 2011; McGrath, Matthews, & Brady, 2006). Few studies report these findings with measures of perceived discrimination, thus limiting neighborhood segregation from being considered as a moderator.
Methodological factors may also moderate the relation between perceived discrimination and hypertension, especially the measurement of these constructs themselves. The conceptualization and measurement of perceived discrimination poses a significant challenge in the study of racial disparities (cf., Brondolo, Gallo, & Myers, 2009; Landrine et al., 2006). Perceived discrimination inherently reflects one’s lifetime burden of discrimination, the occurrence and frequency of everyday and lifetime discrimination, personal attribution and coping resources, as well as the effect of skin color and acculturation. In the present meta-analysis, perceived discrimination was coded based on the measures themselves and three underlying constructs (nature, type, time frame). Although the Everyday Discrimination Scale was used most frequently, its results were inconsistent, as it was associated with hypertensive status but not resting blood pressure. For the nature of discrimination, nonspecific measures were significantly associated with hypertensive status, yet the magnitude of the effect was not meaningfully different than racism measures. For the type of discrimination, institutional-setting measures were significantly associated with both resting blood pressure measures; however, items predominantly inquired about interpersonal discrimination within institutional settings (e.g., “Have you ever been made to feel inferior because of your race or color at work?”), rather than specific policies or procedures of the institution. Finally, time frame of discrimination appeared to only matter for Blacks. Past-year measures were significantly associated with hypertensive status, whereas lifetime measures were significantly associated with resting diastolic blood pressure. Limited psychometric standards in the measurement of perceived discrimination have been previously criticized (cf., Brondolo et al., 2003; 2011). As well, prior reviews considered how measurement of discrimination may moderate observed findings. Others concluded that there is weak evidence linking interpersonal-type discrimination with hypertensive status, and that there is a more consistent relation with ambulatory blood pressure (Brondolo et al., 2011). Institutional-type discrimination has been suggested to be more clearly associated with hypertension incidence in population-based studies using contextual-level indicators of neighborhood segregation (cf., Brondolo et al., 2011). Discrimination time frame findings are inconsistent, with some suggesting that past year may be more sensitive than lifetime (Paradies, 2006), others reporting no differences across chronic, acute, recent, or lifetime, and others observing an association among Blacks alone for chronic, but not acute discrimination (Pascoe & Smart Richman, 2009); however, these findings are limited to general or physical health outcomes. Finally, discrimination measures with more items have been suggested to yield stronger associations with health generally (Paradies, 2006).
Methodological differences in the diagnosis of hypertensive status and measurement of blood pressure also moderated current findings. Discrimination was significantly and more strongly related to hypertensive status that was defined by physician diagnosis or prescription medication, including self-report, compared with clinic or laboratory-measured blood pressure values exceeding 140/90 mmHg. According to the Joint National Committee Blood Pressure Task Force Guidelines (Chobanian et al., 2003; Pickering et al., 2005), having only one to two blood pressure readings on a single day is insufficient to diagnosis hypertension. Physician diagnosis or use of prescribed blood pressure medications are more valid indicators of actual hypertensive status. Most studies use self-report of diagnosis or medication use, and there is evidence that self-report is accurate against medical record (Alonso et al., 2005). Prior reviews have typically drawn conclusions from the combined results of studies with physician diagnosis, self-report of diagnosis, and measured blood pressure as a “proxy for documented diagnosis” (e.g., Brondolo et al., 2003; 2011; Paradies, 2006; Williams & Mohammed, 2009). Resting blood pressure was not associated with perceived discrimination; however, moderators revealed significant associations within subgroups. Consistent with observations of prior reviews (e.g., Brondolo et al., 2011), ambulatory nighttime systolic and diastolic blood pressure were associated with perceived discrimination. Ambulatory dipping was also associated for diastolic blood pressure, and although not significant, a similar magnitude effect was observed for systolic blood pressure. Further, these effect sizes were the largest observed across all meta-analysis associations, accounting for 14% of the variance in the association between perceived discrimination and hypertension. There are plausible reasons why ambulatory measures may yield more accurate measures of blood pressure than clinic-based assessments. First, ambulatory measures are thought to be more ecologically valid, as they capture daily fluctuations of blood pressure in one’s natural living environment. Second, ambulatory measures are more stable from a measurement perspective, as they capture longer time intervals (e.g., 12 to 24 hr), thus reducing measurement error. Ambulatory studies have the potential to yield important insight into contextual level determinants, including neighborhood segregation.
There are current limitations in the extant literature that constrain our comprehensive understanding of the association between perceived discrimination and hypertension. First, sample participants were young, with an average age of 38.25 years. Hypertension prevalence increases with age (e.g., <40 years, 7%; 60+ years, 65%; Ong, Cheung, Man, Lau, & Lam, 2007). The association between perceived discrimination and hypertension may be less apparent, given the young age of participants in most included studies. However, blood pressure levels track over the life course, and the largest effects were observed for hypertensive status rather than resting blood pressure. Second, participants were most typically women (67.25%). Men are more likely to have uncontrolled hypertension as well as greater end-organ damage and mortality than women (American Heart Association, 2005). The strength of the association between perceived discrimination and hypertension was greater in studies with higher percentages of men, which suggests this association may be even more pronounced within men. Third, the findings are based on self-report of perceived racial discrimination. Several additional individual and contextual level factors may explain the observed racial disparities in hypertension, including identification with one’s racial group, level of interacting with members of the racial majority group, perceived group discrimination, coping resources, and neighborhood racial segregation.
The cumulative burden of social and environmental disparities among races has direct implications for racial health disparities (Hicken, Gragg, & Hu, 2011). Hypertension is an established risk factor for other cardiovascular diseases and mortality (O’Donnell et al., 1997). Mortality attributable to hypertension accounts for the largest racial disparity in potential life-years lost (15%), over HIV, diabetes, and homicide (Wong, Shapiro, Boscardin, & Ettner, 2002). Addressing racial disparities in hypertension would contribute greatly to lowering mortality among Blacks. The challenge in developing effective public policy is targeting the intersection of social, behavioral, and environmental determinants that underlie health disparities.
In conclusion, despite methodological limitations, there is a small, significant association between perceived racial discrimination and hypertensive status. Perceived discrimination was most strongly associated with nighttime ambulatory blood pressure, especially among Blacks, which may more accurately capture blood pressure variation in response to racial discrimination. Future research should further examine nighttime blood pressure and contextual-level indicators of institutional-setting discrimination (e.g., neighborhood racial segregation, social cohesion) as possible moderators of the association between perceived racial discrimination and hypertension. Taken together, perceived discrimination may partly explain racial health disparities.
Acknowledgments
This research was made possible through funding support from the Canadian Institutes of Health Research (Cynthia M. Dolezsar – Health Professional Student Research Award; Jennifer J. McGrath – New Investigator Award) and Fonds de Recherche Société et Culture (Alyssa J. M. Herzig – Doctoral Research Grant).
References
References marked with an asterisk indicate studies included in the meta-analysis.
- Adler NE, Rehkopf DH. U.S. disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- Adler NE, Snibbe AC. The role of psychosocial processes in explaining the gradient between socioeconomic status and health. Current Directions in Psychological Science. 2003;12:119–123. doi: 10.1111/1467-8721.01245. [DOI] [Google Scholar]
- Alonso A, Beunza JJ, Delgado-Rodríguez M, Martínez-González MA. Validation of self-reported diagnosis of hypertension in a cohort of university graduates in Spain. BMC Public Health. 2005;5:94–101. doi: 10.1186/1471-2458-5-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Heart Association. Heart Disease and Stroke Statistics –2005 Update. Dallas, TX: Author; 2005. [Google Scholar]
- *.Barksdale DJ, Farrug ER, Harkness K. Racial discrimination and blood pressure: Perceptions, emotions, and behaviors of Black American adults. Issues in Mental Health Nursing. 2009;30:104–111. doi: 10.1080/01612840802597879. [DOI] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, … Roccella E. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Complete Report. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Bowen-Reid TL, Harrell JP. Racist experiences and health outcomes: An examination of spirituality as a buffer. Journal of Black Psychology. 2002;28:18–36. doi: 10.1177/0095798402028001002. [DOI] [Google Scholar]
- *.Broman CL. The health consequences of racial discrimination: A study of African Americans. Ethnicity and Disease. 1996;6:148–153. [PubMed] [Google Scholar]
- Brondolo E, Brady ver Halen N, Pencille M, Beatty D, Contrada R. Coping with racism: A selective review of the literature and a theoretical and methodological critique. Journal of Behavioral Medicine. 2009;32:64–88. doi: 10.1007/s10865-008-9193-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brondolo E, Gallo L, Myers H. Race, racism, and health: Disparities, mechanisms, and interventions. Journal of Behavioral Medicine. 2009;32:1–8. doi: 10.1007/s10865-008-9190-3. [DOI] [PubMed] [Google Scholar]
- Brondolo E, Kelly KP, Coakley V, Gordon T, Thompson S, Levy E, … Contrada R. The perceived ethnic discrimination questionnaire: Development and preliminary validation of a community version. Journal of Applied Social Psychology. 2005;35:335–365. doi: 10.1111/j.1559-1816.2005.tb02124.x. [DOI] [Google Scholar]
- *.Brondolo E, Libby DJ, Denton EG, Thompson S, Beatty DL, Schwartz J, … Gerin W. Racism and ambulatory blood pressure in a community sample. Psychosomatic Medicine. 2008;70:49–56. doi: 10.1097/PSY.0b013e31815ff3bd. [DOI] [PubMed] [Google Scholar]
- Brondolo E, Love EE, Pencille M, Schoenthaler A, Ogedegbe G. Racism and hypertension: A review of the empirical evidence and implications for clinical practice. American Journal of Hypertension. 2011;24:518–529. doi: 10.1038/ajh.2011.9. [DOI] [PubMed] [Google Scholar]
- Brondolo E, Rieppi R, Kelly K, Gerin W. Perceived racism and blood pressure: A review of the literature and conceptual and methodological critique. Annals of Behavioral Medicine. 2003;25:55–65. doi: 10.1207/S15324796ABM2501_08. [DOI] [PubMed] [Google Scholar]
- *.Brown C, Matthews KA, Bromberger JT, Chang Y. The relation between perceived unfair treatment and blood pressure in a racially/ethnically diverse sample of women. American Journal of Epidemiology. 2006;164:257–262. doi: 10.1093/aje/kwj196. [DOI] [PubMed] [Google Scholar]
- Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, … Labarthe D. Prevalence of hypertension in the US adult population. Hypertension. 1995;25:305–313. doi: 10.1161/01.HYP.25.3.305. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. CDC health disparities and inequalities report - United States, 2011. Morbidity and Mortality Weekly Report. Surveillance summaries (Washington, DC: 2002) 2011;60:1–113. [Google Scholar]
- Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Statistics in Medicine. 2000;19:3127–3131. doi: 10.1002/1097-0258(20001130)19:22<3127::AID-SIM784>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, … Roccella E. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Complete Report. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- *.Clark R. Perceptions of interethnic group racism predict increased vascular reactivity to a laboratory challenge in college women. Annals of Behavioral Medicine. 2000;22:214–222. doi: 10.1007/BF02895116. [DOI] [PubMed] [Google Scholar]
- *.Clark R. Self-reported racism and social support predict blood pressure reactivity in Blacks. Annals of Behavioral Medicine. 2003;25:127–136. doi: 10.1207/S15324796ABM2502_09. [DOI] [PubMed] [Google Scholar]
- *.Clark R. Interactive but not direct effects of perceived racism and trait anger predict resting systolic and diastolic blood pressure in black adolescents. Health Psychology. 2006;25:580–585. doi: 10.1037/0278-6133.25.5.580. [DOI] [PubMed] [Google Scholar]
- *.Clark R, Adams JH. Moderating effects of perceived racism on John Henryism and blood pressure reactivity in Black female college students. Annals of Behavioral Medicine. 2004;28:126–131. doi: 10.1207/s15324796abm2802_8. [DOI] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A biopsychosocial model. American Psychologist. 1999;54:805–816. doi: 10.1037/0003-066X.54.10.805. [DOI] [PubMed] [Google Scholar]
- *.Clark R, Gochett P. Interactive effects of perceived racism and coping responses predict a school-based assessment of blood pressure in Black youth. Annals of Behavioral Medicine. 2006;32:1–9. doi: 10.1207/s15324796abm3201_1. [DOI] [PubMed] [Google Scholar]
- Cooper H. Synthesizing research. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Cooper H, Hedges LV. The handbook of research synthesis. New York, NY: Russell Sage Foundation; 1994. [Google Scholar]
- Cooper RS, Wolf-Maier K, Luke A, Adeyemo A, Banegas J, Forrester T, … Thamm M. An international comparison of blood pressure in populations of European vs. African descent. BMC Medicine. 2005;3:2–10. doi: 10.1186/1741-7015-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornoni-Huntley J, LaCroix A, Havlik R. Race and sex differentials in the impact of hypertension in the United States. The National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study. Archives of Internal Medicine. 1989;149:780–788. doi: 10.1001/archinte.1989.00390040022005. [DOI] [PubMed] [Google Scholar]
- *.Cozier Y, Palmer JR, Horton NJ, Fredman L, Wise LA, Rosenberg L. Racial discrimination and the incidence of hypertension in US Black women. Annals of Epidemiology. 2006;16:681–687. doi: 10.1016/j.annepidem.2005.11.008. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. American Journal of Public Health. 2007;97:1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Davis SK, Liu Y, Quarells RC, Din-Dzietham R Metro Atlantic Heart Disease Study Group. Stress-related racial discrimination and hypertension likelihood in a population-based sample of African Americans: The Metro Atlanta Heart Disease Study. Ethnicity and Disease. 2005;15:585–593. [PubMed] [Google Scholar]
- *.Din-Dzietham R, Nembhard WN, Collins R, Davis SK. Perceived stress following race-based discrimination at work is associated with hypertension in African-Americans. The Metro Atlanta Heart Disease Study, 1999–2001. Social Science & Medicine. 2004;58:449–461. doi: 10.1016/S0277-9536(03)00211-9. [DOI] [PubMed] [Google Scholar]
- Fang CY, Myers HF. The effects of racial stressors and hostility on cardiovascular reactivity in African American and Caucasian men. Health Psychology. 2001;20:64–70. doi: 10.1037/0278-6133.20.1.64. [DOI] [PubMed] [Google Scholar]
- Ferdinand KC, Armani AM. The management of hypertension in African Americans. Critical Pathways in Cardiology. 2007;6:67–71. doi: 10.1097/HPC.0b013e318053da59. [DOI] [PubMed] [Google Scholar]
- Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-Origin adults in California. Journal of Health and Social Behavior. 2000;41:295–313. doi: 10.2307/2676322. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- Gee GC, Spencer MS, Chen J, Takeuchi DT. A nationwide study of discrimination and chronic health conditions among Asian Americans. American Journal of Public Health. 2007;97:1275–1282. doi: 10.2105/AJPH.2006.091827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman AH. Why genes don’t count (for racial differences in health) American Journal of Public Health. 2000;90:1699–1702. doi: 10.2105/AJPH.90.11.1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Guyll M, Matthews KA, Bromberger JT. Discrimination and unfair treatment: Relation to cardiovascular reactivity among Afri-can American and European American women. Health Psychology. 2001;20:315–325. doi: 10.1037/0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- *.Hahm HC, Ozonoff A, Gaumond J, Sue S. Perceived discrimination and health outcomes: A gender comparison among Asian-Americans nationwide. Women’s Health Issues. 2010;20:350–358. doi: 10.1016/j.whi.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell JP, Hall S, Taliaferro J. Physiological responses to racism and discrimination: An assessment of the evidence. American Journal of Public Health. 2003;93:243–248. doi: 10.2105/AJPH.93.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell SP. The Racism and Life Experiences Scales (RaLES) California School of Professional Psychology; Los Angeles, CA: 1997. Unpublished manuscript. [Google Scholar]
- Harrell SP, Merchant MA, Young SA. Psychometric properties of the Racism and Life Experience Scales (RaLES). Poster presented at the American Psychological Association convention; Chicago, IL. 1997. [Google Scholar]
- Hayward MD, Crimmins EM, Miles TP, Yang Y. The significance of socioeconomic status in explaining the racial gap in chronic health conditions. American Sociological Review. 2000;65:910–930. doi: 10.2307/2657519. [DOI] [Google Scholar]
- Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Archives of Internal Medicine. 2005;165:2098–2104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- Hicken M, Gragg R, Hu H. How cumulative risks warrant a shift in our approach to racial health disparities: The case of lead, stress, and hypertension. Health Affairs. 2011;30:1895–1901. doi: 10.1377/hlthaff.2010.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Hill LK, Kobayashi I, Hughes JW. Perceived racism and ambulatory blood pressure in African American college students. Journal of Black Psychology. 2007;33:404–421. doi: 10.1177/0095798407307042. [DOI] [Google Scholar]
- *.James SA, LaCroix AZ, Kleinbaum DG, Strogatz DS. John Henryism and blood pressure differences among black men II. Journal of Behavioral Medicine. 1984;7:259–275. doi: 10.1007/BF00845359. [DOI] [PubMed] [Google Scholar]
- *.Kaholokula JK, Grandinetti A, Keller S, Nacapoy A, Kingi T, Mau M. Association between perceived racism and physiological stress indices in Hawaiians. Journal of Behavioral Medicine. 2012;35:27–37. doi: 10.1007/s10865-011-9330-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Kaholokula J, Iwane M, Nacapoy A. Effects of perceived racism and acculturation on hypertension in native Hawaiians. Hawai’i Medical Journal. 2010;69:11–15. [PMC free article] [PubMed] [Google Scholar]
- *.Karlsen S, Nazroo J. Relation between racial discrimination, social class, and health among ethnic minority groups. American Journal of Public Health. 2002;92:624–631. doi: 10.2105/AJPH.92.4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kershaw KN, Diez Roux AV, Burgard SA, Lisabeth LD, Mujahid MS, Schulz AJ. Metropolitan-level racial residential segregation and Black–White disparities in hypertension. American Journal of Epidemiology. 2011;174:537–545. doi: 10.1093/aje/kwr116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Klimentidis YC, Dulin-Keita A, Casazza K, Willig AL, Allison DB, Fernandez JR. Genetic admixture, social-behavioural factors and body composition are associated with blood pressure differently by racial-ethnic group among children. Journal of Human Hypertension. 2012;26:98–107. doi: 10.1038/jhh.2010.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krantz DS, Manuck SB. Acute psychophysiologic reactivity and risk of cardiovascular disease: A review and methodologic critique. Psychological Bulletin. 1984;96:435–464. doi: 10.1037/0033-2909.96.3.435. [DOI] [PubMed] [Google Scholar]
- *.Krieger N. Racial and gender discrimination: Risk factors for high blood pressure? Social Science & Medicine. 1990;30:1273–1281. doi: 10.1016/0277-9536(90)90307-E. [DOI] [PubMed] [Google Scholar]
- *.Krieger N, Carney D, Lancaster K, Waterman P, Kosheleva A, Banaji M. Combining explicit & implicit measures of racial discrimination in research. American Journal of Public Health. 2010;100:1485–1492. doi: 10.2105/AJPH.2009.159517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Krieger N, Chen JT, Waterman PD, Hartman C, Stoddard AM, Quinn MM, … Barbeau E. The inverse hazard law: Blood pressure, sexual harassment, racial discrimination, and occupational exposures in US low-income black, white and Latino workers. Social Science & Medicine. 2008;67:1970–1981. doi: 10.1016/j.socscimed.2008.09.039. [DOI] [PubMed] [Google Scholar]
- *.Krieger N, Sidney S. Racial discrimination and blood pressure: The CARDIA study of young Black and White adults. American Journal of Public Health. 1996;86:1370–1378. doi: 10.2105/AJPH.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrine H, Klonoff EA, Corral I, Fernandez S, Roesch S. Conceptualizing and measuring ethnic discrimination in health research. Journal of Behavioral Medicine. 2006;29:79–94. doi: 10.1007/s10865-005-9029-0. [DOI] [PubMed] [Google Scholar]
- *.Lewis TT, Aiello AE, Leurgans S, Kelly J, Barnes LL. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain, Behavior, and Immunity. 2010;24:438–443. doi: 10.1016/j.bbi.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Lewis TT, Barnes LL, Bienias JL, Lackland DT, Evans DA, Mendes de Leon CF. Perceived discrimination and blood pressure in older African American and White adults. The Journals of Gerontology: Series A: Biological Sciences and Medical Sciences. 2009;64:1002–1008. doi: 10.1093/gerona/glp062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley DV, Scott WF. New Cambridge elementary statistics tables. Cambridge, UK: Cambridge University Press; 1984. [Google Scholar]
- *.Matthews KA, Salomon K, Kenyon K, Zhou F. Unfair treatment, discrimination, and ambulatory blood pressure in Black and White adolescents. Health Psychology. 2005;24:258–265. doi: 10.1037/0278-6133.24.3.258. [DOI] [PubMed] [Google Scholar]
- *.McClure HH, Snodgrass J, Martinez A, Eddy J, Jimenez R, Isiordia L. Discrimination, psychosocial stress, and health among Latin American immigrants in Oregon. American Journal of Human Biology. 2010a;22:421–423. doi: 10.1002/ajhb.21002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.McClure HH, Snodgrass J, Martinez A, Eddy J, Jimenez R, Isiordia L. Discrimination-related stress, blood pressure and Epstein-Barr virus antibodies among Latin American immigrants in Oregon, US. Journal of Biosocial Science. 2010b;42:433–461. doi: 10.1017/S0021932010000039. [DOI] [PubMed] [Google Scholar]
- McGrath JJ, Matthews K, Brady S. Individual vs. neighborhood socioeconomic status & race as predictors of adolescent ambulatory blood pressure & heart rate. Social Science & Medicine. 2006;63:1442–1453. doi: 10.1016/j.socscimed.2006.03.019. [DOI] [PubMed] [Google Scholar]
- McNeilly MD, Robinson EL, Anderson NB, Pieper CF, Shah A, Toth PS, … Gerin W. Effects of racist provocation and social support on cardiovascular reactivity in African American women. International Journal of Behavioral Medicine. 1995;2:321–338. doi: 10.1207/s15327558ijbm0204_3. [DOI] [PubMed] [Google Scholar]
- McNeilly MD, Anderson NB, Armstead CA, Clark R, Corbett M, Robinson EL, … Lepisto EM. The Perceived Racism Scale: A multidimensional assessment of the experience of White racism among African Americans. Ethnicity and Disease. 1996;6:154–166. [PubMed] [Google Scholar]
- *.Mezuk B, Kershaw KN, Hudson D, Lim KA, Ratliff S. Job strain, workplace discrimination, & hypertension among older workers: The Health & Retirement Study. Race and Social Problems. 2011;3:38–50. doi: 10.1007/s12552-011-9041-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Moghaddam F, Taylor D, Ditto B, Jacobs K, Bianchi E. Psychological distress and perceived discrimination: A study of women in India. International Journal of Intercultural Relations. 2002;26:381–390. doi: 10.1016/S0147-1767(02)00012-3. [DOI] [Google Scholar]
- *.Mujahid MS, Diez Roux AV, Cooper RC, Shea S, Williams DR. Neighborhood stressors and race/ethnic differences in hypertension prevalence. American Journal of Hypertension. 2011;24:187–193. doi: 10.1038/ajh.2010.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell CJ, Ridker PM, Glynn RJ, Berger K, Ajani U, Manson JE, Hennekens CH. Hypertension and borderline isolated systolic hypertension increase risks of cardiovascular disease and mortality in male physicians. Circulation. 1997;95:1132–1137. doi: 10.1161/01.CIR.95.5.1132. [DOI] [PubMed] [Google Scholar]
- Ong KL, Cheung BM, Man YB, Lau CP, Lam KSL. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- Orwin RG. A fail-safe N for effect size in meta-analysis. Journal of Educational Statistics. 1983;8:157–159. doi: 10.2307/1164923. [DOI] [Google Scholar]
- Paradies Y. A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology. 2006;35:888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: A meta-analytic review. Psychological Bulletin. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Peters RM. The relationship of racism, chronic stress emotions, and blood pressure. Journal of Nursing Scholarship. 2006;38:234–240. doi: 10.1111/j.1547-5069.2006.00108.x. [DOI] [PubMed] [Google Scholar]
- Peterson RA, Brown S. On the use of beta coefficients in meta-analysis. Journal of Applied Psychology. 2005;90:175–181. doi: 10.1037/0021-9010.90.1.175. [DOI] [PubMed] [Google Scholar]
- Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, … Roccella EJ. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: Blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111:679–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- *.Pointer MA, Livingston JN, Yancey S, McClelland MK, Bukoski RD. Psychosocial factors contribute to resting blood pressure in African Americans. Ethnicity and Disease. 2008;18:289–293. [PMC free article] [PubMed] [Google Scholar]
- *.Rahman S, Hu H, McNeely E, Rahman SM, Krieger N, Waterman P, … Gragg RD. Social and environmental risk factors for hypertension in African Americans. Florida Public Health Review. 2008;5:64–72. doi: 10.1901/jaba.2008.5-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Roberts CB, Vines AI, Kaufman JS, James SA. Cross-sectional association between perceived discrimination and hypertension in African-American men and women: The Pitt County Study. American Journal of Epidemiology. 2008;167:624–632. doi: 10.1093/aje/kwm334. [DOI] [PubMed] [Google Scholar]
- Rosenberg MS, Adams D, Gurevitch J. MetaWin. Statistical Software for Meta-Analysis, Version 2.0. Sunderland, MA: Sinauer Associates; 2000. [Google Scholar]
- Rosenthal R. Meta-analytic procedures for social research. Newbury Park, CA: Sage; 1991. (rev. ed.) [Google Scholar]
- *.Ryan AM, Gee GC, Laflamme DF. The association between self-reported discrimination, physical health, and blood pressure: Findings from African Americans, Black immigrants, and Latino immigrants in New Hampshire. Journal of Health Care for the Poor and Underserved. 2006;17:116–132. doi: 10.1353/hpu.2006.0092. [DOI] [PubMed] [Google Scholar]
- *.Salomon K, Jagusztyn E. Resting cardiovascular levels & reactivity to interpersonal incivility among Black, Latina/o, & White individuals: The moderating role of ethnic discrimination. Health Psychology. 2008;27:473–481. doi: 10.1037/0278-6133.27.4.473. [DOI] [PubMed] [Google Scholar]
- Sánchez-Meca J, Marín-Martínez F, Chacón-Moscoso S. Effect-size indices for dichotomized outcomes in meta-analysis. Psychological Methods. 2003;8:448–467. doi: 10.1037/1082-989X.8.4.448. [DOI] [PubMed] [Google Scholar]
- Schmidt FL, Oh IS, Hayes TL. Fixed-versus random-effects models in meta-analysis: Model properties and an empirical comparison of differences in results. British Journal of Mathematical and Statistical Psychology. 2009;62:97–128. doi: 10.1348/000711007X255327. [DOI] [PubMed] [Google Scholar]
- *.Singleton GJ, Robertson J, Robinson JC, Austin C, Edochie V. Perceived racism and coping: Joint predictors of blood pressure in Black Americans. Negro Educational Review. 2008;59:93–113. [Google Scholar]
- *.Smart Richman L, Pek J, Pascoe E, Bauer DJ. The effects of perceived discrimination on ambulatory blood pressure and affective responses to interpersonal stress modeled over 24 hours. Health Psychology. 2010;29:403–411. doi: 10.1037/a0019045. [DOI] [PubMed] [Google Scholar]
- *.Steffen PR, McNeilly M, Anderson N, Sherwood A. Effects of perceived racism and anger inhibition on ambulatory blood pressure in African Americans. Psychosomatic Medicine. 2003;65:746–750. doi: 10.1097/01.psy.0000079380.95903.78. [DOI] [PubMed] [Google Scholar]
- Sutherland ME, Harrell JP. Individual differences in physiological responses to fearful, racially noxious, and neutral imagery. Imagination, Cognition and Personality. 1986;6:133–150. [Google Scholar]
- Taylor J, Grundy C. Measuring Black internalization of White stereotypes about Blacks: The Nadanolitization Scale. In: Jones RL, editor. Handbook of tests & measurements for Black populations. Hampton, VA: Cobb & Henry; 1996. [Google Scholar]
- *.Todorova ILG, Falcon LM, Lincoln AK, Price LL. Perceived discrimination, psychological distress and health. Sociology of Health & Illness. 2010;32:843–861. doi: 10.1111/j.1467-9566.2010.01257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Tomfohr L, Cooper DC, Mills PJ, Nelesen RA, Dimsdale JE. Everyday discrimination and nocturnal blood pressure dipping in Black and White Americans. Psychosomatic Medicine. 2010;72:266–272. doi: 10.1097/PSY.0b013e3181d0d8b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Tull S, Wickramasuriya T, Taylor J, Smith-Burns J, Brown M, Champagnie G, … Jordan OW. Relationship of internalized racism to abdominal obesity and blood pressure in Afro-Caribbean women. Journal of the National Medical Association. 1999;91:447–452. [PMC free article] [PubMed] [Google Scholar]
- Victoroff J. The Oppression Questionnaire [August 5, 2008] 2005 Retrieved from http://www.humiliationstudies.org/documents/VictoroffOppressionQuestionnaire.pdf.
- White K, Borrell LN, Wong DW, Galea S, Ogedegbe G, Glymour MM. Racial/ethnic residential segregation and self-reported hypertension among US- and foreign-born Blacks in New York City. American Journal of Hypertension. 2011;24:904–910. doi: 10.1038/ajh.2011.69. [DOI] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson J, Anderson N. Racial differences in physical and mental health: Socioeconomic status, stress, and discrimination. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. New England Journal of Medicine. 2002;347:1585–1592. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]