Abstract
Objective
To comprehensively and quantitatively examine the association between subjective socioeconomic status (SES) and health outcomes during adolescence.
Methods
Forty-four studies met criteria for inclusion in the meta-analysis. Information on study quality, demographics, subjective SES, health outcomes, and covariates were extracted from each study. Fisher’s Z was selected as the common effect size metric across studies. Random-effect meta-analytic models were employed and fail-safe numbers were generated to address publication bias.
Results
Overall, subjective SES was associated with health during adolescence (Fisher’s Z = .10). The magnitude of the effect varied by type of health outcome, with larger effects observed for mental health outcomes, self-rated health, and general health symptoms; and nonsignificant effects observed for biomarkers of health and substance-use-related health behaviors. Of the measures of subjective SES employed in the reviewed studies, perception of financial constraints, was most strongly associated with adolescent health outcomes. Analysis of covariates indicated that inclusion of objective SES covariates did not affect the association between subjective SES and health.
Conclusions
This meta-analysis has implications for the measurement of subjective SES in adolescents, for the conceptualization of subjective and objective SES, and for the pathways between SES and health in adolescents.
Keywords: subjective socioeconomic status, health outcomes, adolescence, meta-analysis
Considerable research has linked low socioeconomic status (SES) to poor health outcomes. Prior to the mid-1980s, SES was assumed to be related to health simply below a threshold of poverty, and it was used most often as a control variable (Adler & Ostrove, 1999). The threshold model was challenged most notably by the Whitehall study of mortality (Marmot, Shipley, & Rose, 1984), which demonstrated an increase in risk of mortality as employment grade decreased in British civil servants. Since then, the graded relation between SES and health that occurs at all levels of SES has been well established (Adler et al., 1994) and inverse gradients have been found for many health outcomes, including cardiovascular disease (Kaplan & Keil, 1993), diabetes (Paeratakul, Lovejoy, Ryan, & Bray, 2002), arthritis (Bengtsson et al., 2005), and adverse birth outcomes (Kramer, Séguin, Lydon, & Goulet, 2000). The finding that higher SES is associated with better health at every increment of social status suggests that the association between SES and health is derived not just from basic health needs, but also from social and psychological variables associated with one’s standing in a social hierarchy. In fact, relative standing in the hierarchy may be more important than absolute levels of SES (Wilkinson, 1999). Most studies examining SES gradients in health have used objective indicators, such as income, education, and occupation. These indicators are often used interchangeably, even though they are only moderately correlated with one another (Winkleby, Jatulis, Frank, & Fortmann, 1992). Similar associations with health have been found with each SES indicator, suggesting that a common underlying element of social stratification may influence health (Adler & Ostrove, 1999).
Subjective status has been defined as “a person’s belief about his location in a status order” (Davis, 1956, p. 154). Subjective SES, also called subjective social status (Adler, Epel, Castellazzo, & Ickovics, 2000) and perceived social position (Garbarski, 2010), may be defined as “an individual’s perception of his or her place in the socioeconomic structure” (Singh-Manoux, Adler, & Marmot, 2003, p. 1322). In adults, subjective SES has been found to be more strongly related to health outcomes than objective SES, as measured by a composite of education, income, occupation (Adler et al., 2000), education or income (Operario, Adler, & Williams, 2004), or employment grade (Singh-Manoux, Marmot, & Adler, 2005). Subjective SES may be strongly linked to health outcomes through a number of mechanisms (Singh-Manoux et al., 2005). First, subjective SES may reflect a person’s relative social position within the social hierarchy, rather than his or her absolute position. Wilkinson (1999) has suggested that perception of relative position mediates the association between income inequality and population health. Experimental research in animals also points to the link between position in the social hierarchy and health outcomes (Sapolsky, 2005). Second, subjective SES may be a more precise measure of social position, as it represents the cognitive average of various markers of SES (Singh-Manoux et al., 2003), takes into account past and future prospects, and offers a more nuanced judgment of objective indicators. Third, the association between subjective SES and health may be reciprocal, such that subjective rating of SES is affected by health status or that both subjective status and health ratings are affected by a third, underlying variable. Garbarski (2010) found evidence for reciprocal associations between subjective SES and health; however, these associations differed across health outcomes and subjective SES measures. In contrast, negative affect was found not to uniquely confound the relation between subjective SES and health (Operario et al., 2004), and associations between subjective SES and health did not change with an experimental mood induction (Kraus, Adler, & Chen, 2013). Finally, longitudinal associations have been observed between subjective SES and change in self-rated health over time (Singh-Manoux et al., 2005), which provides preliminary support for the direction of this association.
The inverse, graded relation between SES and health has been well established in infants (e.g., Kramer et al., 2000), children (e.g., Chen, Matthews, & Boyce, 2002), and adults (e.g., Adler & Ostrove, 1999). However, inequalities in adolescent health are understudied (Currie et al., 2008), and studies have shown that the SES gradient in health may be present inconsistently during adolescence. For instance, some studies have demonstrated inverse gradients between SES and global health measures (parent rating of health, activity limitations, school limitations), acute conditions (injuries, respiratory conditions; Chen, Martin, & Matthews, 2006), and health behaviors (cigarette smoking, sedentary lifestyle; Lowry, Kann, Collins, & Kolbe, 1996), while other studies found little evidence of SES gradients in self-rated health, acute illness, nonfatal injuries, and mental health (West, 1997). Some studies have shown associations with certain health outcomes (self-rated health, depression, obesity), but not with others (asthma, suicide attempts, sexually transmitted diseases; Goodman, 1999). Studying adolescent health is important because health-related behaviors (e.g., tobacco and alcohol use, physical inactivity) and health outcomes (e.g., obesity, mental disorders, injuries) during adolescence track over time and can have a sustained effect on future health (Sawyer et al., 2012).
There are multiple explanations for differing relations between SES and health in childhood, adolescence, and adulthood, including a nonconstant, dynamic relation between SES and physical health across the life span or different patterns across age according to health outcomes. In adolescence, the association between SES and health may be weaker due to equalization from school and peer influences (West, 1997) or stronger due to the accumulation of SES influences that contribute to health (Chen et al., 2002). The SES–health association may also differ across age depending on the health outcome of interest (Chen et al., 2006). However, inconsistencies in SES gradients in some adolescent health outcomes may also be partly explained by measurement issues. Adolescent SES is usually derived from parental education, parental occupation, family income, or family wealth, with information collected from parents or from adolescents themselves. Using parental or family SES as a proxy for adolescent SES may be problematic (Glendinning, Love, Hendry, & Shucksmith, 1992), since adolescents may develop a sense of their own social status during this time of transition between childhood (status primarily determined by family) and adulthood (status primarily self-determined).
Having adolescents report their subjective SES, in addition to using objective measures of SES, may help to address some of the issues associated with the measurement of SES in adolescents. Subjective ratings of social status provide insight into how perceptions of relative rank within social hierarchies affect health in this age group. A number of studies have examined the association between subjective SES and a variety of health outcomes in adolescents, including smoking, obesity, depression, and self-rated health. A systematic, narrative review of nine studies that examined this association was completed previously (Ritterman, 2007). Since then, there has been expansion in the number of studies completed in this area. Due to the broad range of health outcomes measured and variety of measures of subjective socioeconomic status employed, it is difficult to qualitatively describe the overall results from these studies. To our knowledge, no systematic, quantitative review of this literature has been completed. Therefore, a meta-analytic review of the studies examining the association between subjective SES and health in adolescents is valuable in terms of synthesizing the research in this area, and makes both theoretical and methodological contributions.
The purpose of this paper is to comprehensively and quantitatively examine the association between subjective SES and health outcomes during adolescence. This meta-analysis examines the overall magnitude of the association, as well potential moderators of the association.
Method
Literature Search Strategy
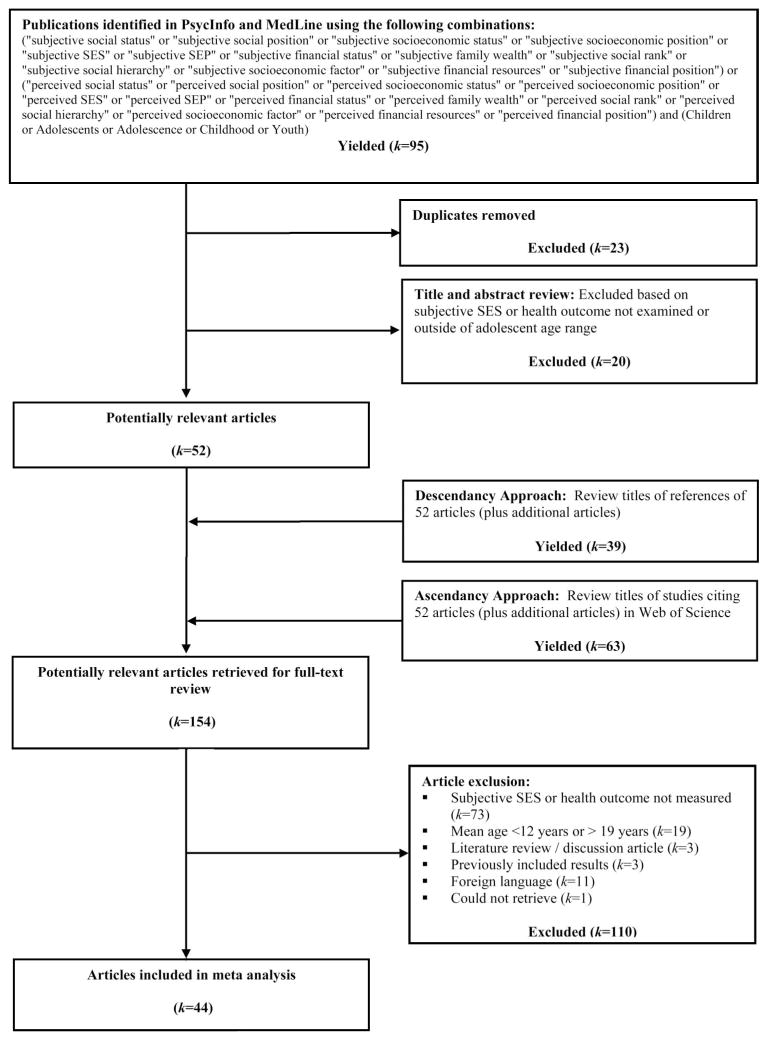
A literature search was conducted in PsycInfo and MedLine electronic databases from 1970 to May, 2012. Searches included the words subjective or perceived, variations on the words social status, socioeconomic position, and adolescence and related terms. Next, ascendancy and descendency approaches were used to identify additional articles. Finally, letters of solicitation were sent to authors who had published two or more articles on the topic requesting available data from unpublished manuscripts, including nonsignificant findings. Researchers’ suggestions did not pertain to any nonredundant data. A total of 154 potentially relevant studies were identified for full review, and were located and retrieved (see Figure 1 for full description of literature search strategy).
Figure 1.
Flowchart for article identification and inclusion in meta-analysis.
Study Inclusion Criteria and Selection
Each study selected for inclusion examined the association between subjective SES and a health outcome or health behavior in the adolescent age range (12–19 years). Additional inclusion criteria were: study results published in English and not previously published in another included study. Thus, 44 studies were included in the meta-analysis.
Data Extraction
Data were extracted by a single rater (EQ), who coded all studies in consultation with another rater (JM). Discrepancies were resolved to reach consensus. Ten percent of studies were blindly recoded after a period of 4 months, with excellent intrarater agreement (ICC = .997). Sample size, demographic information (e.g., % female, age, country), and participation rate were extracted from each study. Information on extraction of subjective SES measures, health outcome measures, and main covariates is provided in the subsequent sections.
Measures
Subjective SES
Subjective SES was operationally defined as the adolescents’ perception of their or their family’s socioeconomic, financial, or social status. Four types of subjective SES measures were coded depending on the type of measure used and content of comparison: society ladder, school ladder, Likert scale, and financial constraints. Society ladder assesses familial placement in society, while school ladder assesses personal placement in the school community, by asking participants to indicate their ranking on a 10-point ladder (see Goodman et al., 2001 for full description of the original scales). Variations of these ladders were accepted, including using a 7-point society ladder (Åslund, Leppert, Starrin, & Nilsson, 2009), examining placement within community (Ritterman et al., 2009; Ritterman, 2010), and examining several types of school status (West, Sweeting, Young, & Kelly, 2010). Likert scale assesses perception of family’s socioeconomic status based on questions such as, “How well off do you think your family is? How would you rate your family’s socioeconomic status? How would you describe your family’s financial situation?” Responses were rated on 3-, 4-, or 5-point ordinal scales, such as low, middle-low, middle, middle-high, high; short of money, in the middle, well off, very well off. Financial constraints assesses adolescents’ perception of economic constraints in the family using several methods, including a single item (“financial difficulties in the family”) and multi-item scales that assessed perception of inadequate money for various needs and wants.
Health outcomes
Outcome variables were defined as: self-rated health, mental health, physical health, and health behaviors. Self-rated health included adolescents’ ratings of their general or overall health on a single item using a 3-, 4- or 5-point Likert scales, such as poor, fair, good, very good, excellent or not healthy, healthy, very healthy. Mental health outcomes included the following subcategories: psychological well-being (e.g., life satisfaction, quality of life, psychological well-being, and psychological distress), psychological variables (e.g., self-esteem, optimism, aggression, hostility, mastery), depression, and stress. Physical health outcomes included the following subcategories: obesity (e.g., body mass index, overweight, obesity), biomarkers (e.g., cortisol, blood pressure, cardiovascular indicators), general symptoms (e.g., headaches, back pain, stomachaches), and injuries. Health behaviors included the following subcategories: substance use (e.g., alcohol, cigarettes, illicit drugs, marijuana), other health behaviors (e.g., diet, exercise), and sexual health.
Covariates
We coded whether each of these variables of interest were included as covariates for each subjective SES-health association: age, sex, race, family structure (e.g., two-parent vs. single-parent home) and school achievement (e.g., type of academic program; marks). We also coded whether the following objective SES covariates were controlled for: household income, parent education, parent occupation, parent employment status, family wealth (Family Affluence Scale; Currie et al., 2008), an objective SES index score, receipt of government aid/welfare, and family savings.
Study quality
The quality of the study was determined on the basis of eight study characteristics: (i) population-representative, (ii) N greater than 1,000, (iii) participation rate greater than 80%, (iv) statistical control for confounders, (v) statistical control for objective SES, (vi) objective SES measured by two or more indicators and parent-reported, (vii) majority of outcomes used validated measures (standardized questionnaires or objectively measured variables), (viii) appropriate statistics used. Intrarater reliability by the first coder (EQ) after a 4-month delay and interrater reliability by an independent coder (DK) for study quality were both excellent (ICC = .990 and .964, respectively).
Statistical Analysis
Effect size calculation
Effect size calculations were guided by previously reported procedures (Cooper & Hedges, 1994). Fisher’s Z was selected as the common effect size metric across studies, as results were predominantly reported as correlations between subjective SES and a health outcome. Fisher’s Z ranges from −∞ to +∞ and is interpreted similar to that of a correlation. It is advantageous as data may be converted from almost any form and summary data are not required; however, it is slightly biased by low sample sizes (Rosenthal, 1991). Bivariate correlations (r) were converted using Fisher’s variance stabilizing transformation. Test statistics, including unstandardized beta coefficients, t test and F-statistic, were converted into r and then into Fisher’s Z (Cooper & Hedges, 1994; Rosenberg, Adams, & Gurevitch, 2000). Dichotimized outcomes (e.g., odds ratio) were transformed into Cohen’s d, and then converted to Fisher’s Z (Chinn, 2000). Means and standard deviations, and χ2 were transformed into Hedges’ g, and then converted to Fisher’s Z (Durlak, 2009). When no test statistic data were reported, effect sizes were derived from reported p values (Rosenberg et al., 2000), and results described as “nonsignificant” were assigned an effect size of zero. The direction of the Fisher Z was coded uniformly, to ensure that positive values reflected better health outcomes (e.g., less obesity, higher self-rated health, lower depression scores) as a function of higher subjective SES.
Selection of effect sizes
Effect sizes were coded for all available and relevant data reported within each article, thus yielding multiple effect sizes per study. There were several reasons why multiple effect sizes were reported and we selected effect sizes accordingly. 1) When multiple results were reported for the same effect size due to employment of several analytic strategies in the original article, we followed a hierarchy to determine which statistic to use and only included one effect size. 2) When different subjective SES measures were employed, different health outcomes were measured, or different group of participants were included, we treated each effect size as nonredundant because a separate subjective SES–health relation was examined. 3) When identical participants were incorporated in more than one subjective SES–health relation due to inclusion of different covariates, we employed two approaches to deal with redundancy (aggregation to create a mean effect size vs. retention of redundant effect sizes); thus, results were analyzed in two ways, depending on the selection of effect sizes. A conservative approach included aggregated effect sizes, so that each subjective SES–health relation was examined only once in each sample (134 nonredundant effect sizes; M = 3.04 effects per study). A less conservative approach included redundant effect sizes to maximize power and to examine the effect of inclusion of covariates (262 redundant effect sizes; M = 5.95 effects per study).
Analytic strategy
Random-effect meta-analytic models were used to evaluate the association between subjective SES and health during adolescence. Random-effects models assume that the samples are drawn from populations with different effect sizes and allows for both random variance and variance due to true differences between the populations. Random-effects models are preferred to fixed-effects models, which typically yield overly narrow confidence intervals (Schmidt, Oh, & Hayes, 2009).
An analysis of the heterogeneity statistic (QT), which measures the variation for the included effect sizes, was conducted for each meta-analytic model. A nonsignificant QT statistic indicates a homogeneous distribution, such that the variability of the effect sizes is less than would be expected from sampling error. A significant QT statistic indicates heterogeneous distribution, and may warrant additional moderator analyses. Separate analyses were conducted for all a priori specified moderator variables, including type of health outcome, geographical region, type of subjective SES measure, study quality, and inclusion of age, sex, race, family type, school achievement, household income, parent education, parent occupation, and family health as covariates. We conducted categorical summary analyses for moderators. As with variance in ANOVA, the total heterogeneity (QT) can be partitioned into the variation explained by the model (QM) and the residual error variance (QR). For all moderator analyses, we tested for differences between groups. We also used continuous summary analyses (regression) to test for an association between sample characteristics (mean age, female proportion) and effect size. Bootstrap methods (1,000 samples) were used to produce robust nonparametric estimates of confidence intervals about each effect size (Rosenberg et al., 2000).
To address concerns about possible publication bias and the file-drawer problem, Orwin’s (1983) fail-safe numbers were calculated to determine the number of nonsignificant, unpublished, or missing comparisons that would be needed to make the overall effect negligible or not different from zero. Analyses were performed using MetaWin 2 (Rosenberg et al., 2000).
Results
Study and Participant Characteristics
Study and sample characteristics are presented in Table 1. The mean number of participants per study was 7,293 (SD = 16,568), which permits adequately powerful tests of a small effect size.
Table 1.
Descriptive Characteristics and Frequencies of 45 Studies Included
| Characteristic | K | N | M (SD) |
|---|---|---|---|
| Sample size | 44 | 320,872 | 7,292.55 (16,567.61) |
| Age (range) | 36 | 303,435 | 12.52 (2.10)–17.32 (2.79) |
| Age (mean) | 27 | 135,517 | 15.32 (1.62) |
| Sex (% female) | 42 | 318,906 | 52.97 (9.10) |
| Objective SES | |||
| Parental education—Low | 16 | 164,982 | 18.90% (15.14) |
| Parental education—High | 18 | 171,428 | 25.15% (13.56) |
| Unemployment | 8 | 20,907 | 13.56% (9.89) |
| Subjective SES | |||
| Society ladder | 12 | 31,467 | 6.51 (0.76) |
| School ladder | 9 | 28,853 | 6.80 (1.12) |
| Likert scale—Low | 22 | 277,135 | 11.41% (9.87) |
| Likert scale—High | 17 | 257,939 | 15.15% (11.80) |
| Financial constraints | 6 | 11,448 | |
| Region | |||
| North America | 19 | 48,739 | |
| Western Europe | 6 | 34,794 | |
| Eastern Europe | 12 | 26,324 | |
| Asia | 5 | 208,590 | |
| Australia | 1 | 97 | |
| Study Quality | 44 | 320,872 | 4.46 (1.38) |
| Population-representative | 10 | 74,698 | |
| N > 1,000 | 33 | 306,405 | |
| Participation rate > 80% | 25 | 265,473 | |
| Control for potential confounders | 37 | 303,204 | |
| Control for objective SES | 29 | 209,604 | |
| Objective SES = two measures, parent-reported | 6 | 19,352 | |
| Validated measures for > 50% outcomes | 19 | 34,739 | |
| Appropriate statistics, presented adequately | 39 | 308,893 | |
Note. K = number of studies reporting this information; N = total number of participants; M = Mean; SD = standard deviation.
Overall Effects
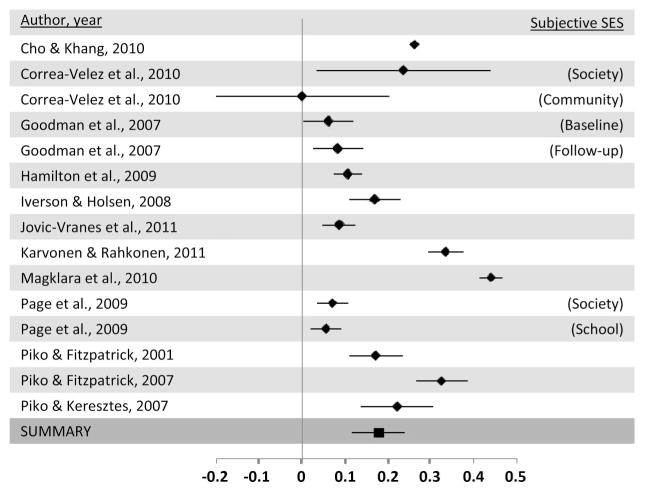
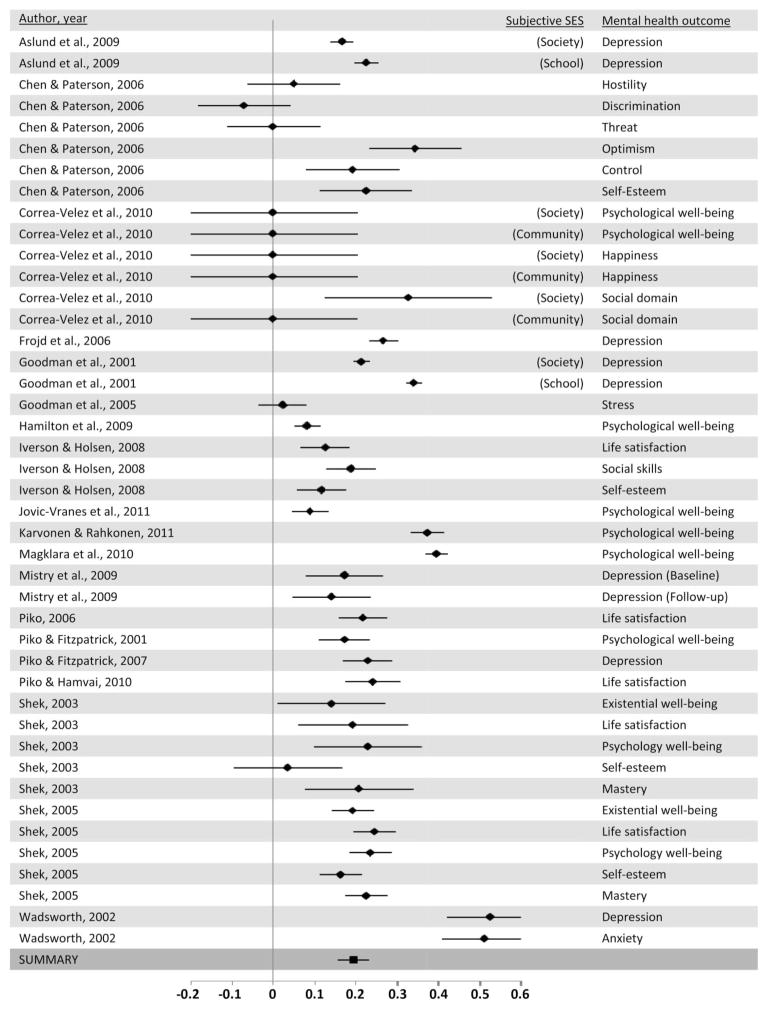
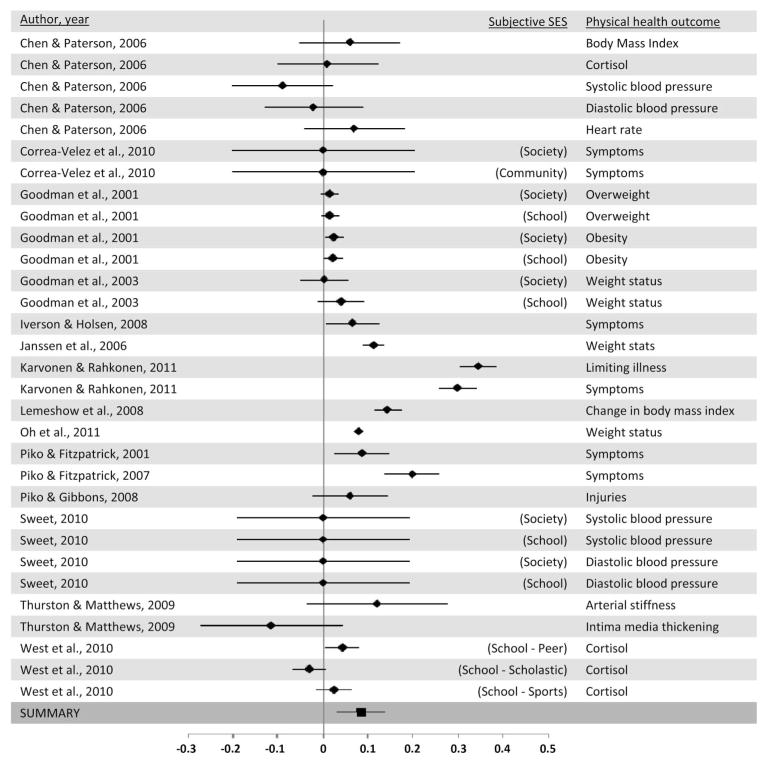
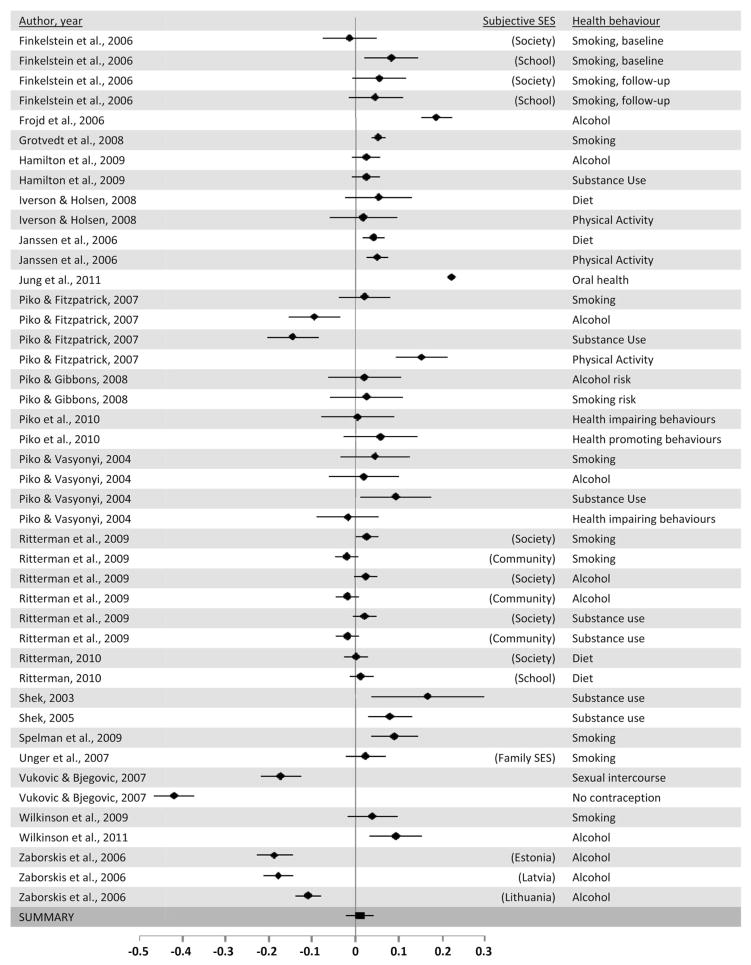
The average cumulative effect size indicated a positive relation such that higher subjective SES was associated with better health outcomes (Fisher’s Z = .095, nonredundant effect sizes; Z = .113, redundant effect sizes). Results suggest that the effect sizes were homogeneous for nonredundant effect sizes and heterogeneous for redundant effect sizes. Effect sizes and confidence intervals are provided for each nonredundant effect size by type of health outcome (see Figures 2, 3, 4, and 5).
Figure 2.
Forest plot for self-rated health.
Figure 3.
Forest plot for mental health outcomes.
Figure 4.
Forest plot for physical health outcomes.
Figure 5.
Forest plot for health behaviors.
Moderator Analyses
Sufficient data and variability existed for the examination of moderators, including health outcome, subjective SES measure, study quality, and geographical region within nonredundant effects (see Table 2), and inclusion of covariates: age, sex, race, family type, school achievement, parent education, parent occupation, household income, and family wealth within redundant effects (see Table 3).
Table 2.
Effect Sizes by Health Outcome, Subjective SES Measure, Study Quality, and Region
| Comparison | Effect sizes1 | N | Fisher Z | Bootstrap 95% CI | QT | Fail-safe N2 |
|---|---|---|---|---|---|---|
| All studies | 133 | 5,105,372 | .095 | (.071, .117) | 138.04 | 12,462 |
| Health outcome | QM = 56.56 (3, 129) p < .001* | |||||
| Self-rated health | 15 | 98,837 | .178 | (.118, .246) | 10.50 | 2,649 |
| Mental health | 43 | 72,182 | .189 | (.154, .227) | 53.54 | 8,086 |
| Depression | 9 | 38,122 | .249 | (.193, .324) | 14.07 | 2,232 |
| Psychological well-being | 16 | 24,407 | .192 | (.140, .240) | 9.20 | 3,047 |
| Psychological variables | 17 | 8,444 | .154 | (.086, .230) | 22.68 | 2,612 |
| Physical health | 31 | 137,726 | .064 | (.029, .102) | 44.58* | 1,957 |
| BMI/Obesity | 10 | 118,442 | .052 | (.021, .085) | 9.45 | 508 |
| Biomarkers | 13 | 10,486 | .006 | (−.025, .033) | 10.66 | 66 |
| General symptoms | 7 | 8,238 | .162 | (.067, .259) | 76.26 | 1,125 |
| Health behaviors | 44 | 196,627 | .010 | (−.025, .040) | 45.10 | 380 |
| Substance use | 33 | 91,363 | .011 | (−.016, .039) | 32.95 | 321 |
| Other | 9 | 101,700 | .068 | (.028, .122) | 4.49 | 604 |
| Subjective SES measure | QM = 28.95 (3, 128) p = .001* | |||||
| Likert scale | 48 | 306,816 | .062 | (.023, .100) | 50.07 | 2,945 |
| Society ladder | 44 | 85,011 | .093 | (.047, .142) | 40.41 | 4,032 |
| School ladder | 21 | 83,657 | .058 | (.024, .103) | 10.03 | 1,202 |
| Financial constraints | 20 | 29,888 | .240 | (.182, .293) | 18.88 | 4,770 |
| Study quality | QM = 0.08 (1, 131) p = .78 | |||||
| Low (0–4) | 64 | 133,012 | .093 | (.055, .125) | 40.51 | 5,717 |
| High (5–7) | 69 | 372,360 | .098 | (.066, .130) | 83.27 | 6,676 |
| Region | QM = 29.76 (4, 132) p = .001* | |||||
| North America | 56 | 172,540 | .071 | (.044, .104) | 68.48 | 3,919 |
| United States | 41 | 91,342 | .088 | (.052, .133) | 42.35 | 3,569 |
| Canada | 7 | 36,364 | .063 | (.038, .088) | 6.05 | 433 |
| Mexico | 8 | 44,834 | .003 | (−.010, .016) | 6.94 | 16 |
| Western Europe | 21 | 69,126 | .185 | (.129, .244) | 16.78 | 3,857 |
| Eastern Europe | 31 | 45,503 | .042 | (−.016, .095) | 26.72 | 1,270 |
| Asia | 15 | 217,233 | .181 | (.146, .213) | 8.21 | 2,700 |
| Australia | 10 | 970 | .056 | (.000, .136) | 9.00 | 551 |
Note.
Number of nonredundant effect sizes,
Fail-safe n using Orwin’s method;
N = total number of participants; QT = heterogeneity test statistic; QM = test of between-group differences.
p < .05.
Table 3.
Effect Sizes by Type of Covariates Included in Original Analysis
| Comparison | Effect sizes1 | N | Fisher Z | Bootstrap 95% CI | QT | Fail-safe N2 |
|---|---|---|---|---|---|---|
| All studies | 262 | 1,672,597 | .113 | (.095, .131) | 364.10* | 29,436 |
| Any Covariates | QM = 8.55 (1, 260) p = .02* | |||||
| No covariates | 89 | 188,463 | .145 | (.115, .178) | 83.08 | 12,824 |
| One or more covariates | 173 | 1,484,134 | .097 | (.077, .119) | 237.78* | 16,655 |
| Age | QM = 8.69 (1, 260) p = .01* | |||||
| Did not include as covariate | 134 | 303,149 | .135 | (.109, .164) | 123.85 | 18,013 |
| Included as covariate | 128 | 1,339,448 | .090 | (.069, .116) | 153.30 | 11,414 |
| Sex | QM = 6.89 (1, 260) p = .03* | |||||
| Did not include as covariate | 153 | 709,387 | .131 | (.106, .153) | 191.31 | 19,892 |
| Included as covariate | 109 | 963,210 | .089 | (.062, .115) | 142.55 | 9,588 |
| Race | QM = 0.19 (1, 260) p = .71 | |||||
| Did not include as covariate | 224 | 1,457,806 | .113 | (.094, .132) | 367.56 | 24,987 |
| Included as covariate | 38 | 214,791 | .119 | (.075, .177) | 24.22 | 4,501 |
| Family type | QM = 0.53 (1, 260) p = .53 | |||||
| Did not include as covariate | 201 | 749,688 | .110 | (.090, .129) | 229.93 | 21,907 |
| Included as covariate | 61 | 922,909 | .123 | (.082, .162) | 112.84 | 7,461 |
| School achievement | QM = 15.93 (1, 260) p = .006* | |||||
| Did not include as covariate | 220 | 765,767 | .099 | (.080, .118) | 173.00 | 21,565 |
| Included as covariate | 42 | 906,830 | .183 | (.141, .227) | 115.68 | 7,651 |
| Objective SES covariates | QM = 0.02 (1, 260) p = .89 | |||||
| No objective SES covariates | 142 | 846,659 | .114 | (.090, .138) | 205.78* | 16,112 |
| One or more objective SES covariates | 120 | 825,938 | .112 | (.086, .138) | 145.45* | 13,313 |
| Education | QM = 1.67 (1, 260) p = .28 | |||||
| Did not include as covariate | 175 | 1,352,057 | .106 | (.084, .128) | 307.84* | 18,408 |
| Included as covariate | 87 | 320,540 | .127 | (.097, .159) | 57.63 | 10,941 |
| Occupation | QM = 3.09 (1, 260) p = .13 | |||||
| Did not include as covariate | 243 | 1,631,999 | .117 | (.098, .135) | 328.83* | 28,229 |
| Included as covariate | 19 | 40,598 | .060 | (−.023, .139) | 12.09 | 1,121 |
| Income | QM = 2.07 (1, 260) p = .22 | |||||
| Did not include as covariate | 253 | 1,649,759 | .116 | (.096, .134) | 350.01 | 28,972 |
| Included as covariate | 9 | 22,838 | .055 | (.029, .088) | 4.62 | 482 |
| Family wealth | QM = 0.04 (1, 260) p = .62 | |||||
| Did not include as covariate | 251 | 1,230,679 | .114 | (.096, .133) | 280.13 | 28,400 |
| Included as covariate | 11 | 441,918 | .093 | (.050, .138) | 13.44 | 1,107 |
Note.
Number of redundant effect sizes,
Fail-safe n using Orwin’s method;
N = total number of participants; QT = heterogeneity test statistic; QM = test of between-group differences.
p < .05.
Health outcome
Categorical summary analyses indicated significant between-groups differences for the type of health outcome. The association between subjective SES and self-reported health was reported in 12 studies (15 nonredundant effect sizes). The average cumulative effect size was homogeneous and indicated a positive relation such that higher subjective SES was associated with better self-reported health (Fisher’s Z = .178). The association between subjective SES and mental health was reported in 19 studies (43 nonredundant effect sizes). The average cumulative effect size was homogeneous and indicated a positive relation, such that high subjective SES was associated with better mental health (Fisher’s Z = .189). Further examination of mental health outcomes showed that this association was present for depression, psychological well-being, and psychological variables (e.g., self-esteem). The association between subjective SES and physical health was reported in 15 studies (31 nonredundant effect sizes). The average cumulative effect size was heterogeneous and indicated a positive relation, such that high subjective SES was associated with better physical health (Fisher’s Z = .064). Further examination of physical health outcomes showed that this association was present for general physical symptoms (e.g., headaches), but not for biomarkers (e.g., cortisol). The association between subjective SES and health behaviors was reported in 20 studies (44 nonredundant effect sizes). The average cumulative effect size was homogeneous and indicated a lack of association between subjective SES and health behaviors (Fisher’s Z = .010). Further examination showed that this association was not present for substance-related health behaviors; however, a small, but significant effect was present for other health behaviors (e.g., diet, physical activity).
Subjective SES measure
Categorical summary analyses indicated significant between-groups differences for type of subjective SES measure employed. Specifically, although all types of measures were associated with a significant positive association with health, financial constraints was associated with the largest effect (Fisher’s Z = .240), while Likert scale, society ladder, and school ladder were associated with smaller mean effect sizes (Fisher’s Z = .062, .093, .058, respectively). As a post hoc analysis, we ran all analyses without the financial constraints measure and patterns of results remained largely identical. Results are not presented for parsimony.
Objective SES
Categorical summary analyses indicated no significant difference between effects that controlled for objective SES compared to those that did not control for objective SES (Fisher’s Z = .114 vs. .112). Therefore, the inclusion of objective SES covariates did not influence the magnitude of the association between subjective SES and health. Likewise, QM was nonsignificant for the inclusion of parent education, parent occupation, household income, and family wealth as covariates.
Covariates
Categorical summary analyses indicated that inclusion of one or more covariates was associated with a significantly smaller effect size compared to examining the subjective SES–health relation alone (Fisher’s Z = .097 vs. .145). Effects that included age or sex covariates had significantly smaller mean effect size compared to effects that did not control for these covariates. Continuous summary analyses showed that mean age of the sample (B = −0.009, SE = 0.011, p = .26), age range of the sample (minimum age B = −0.002, SE = 0.007, p = .46; maximum age B = 0.001, SE = 0.005, p = .51), and female proportion of the sample (B = 0.001; SE = 0.002; p = .60) were not significantly associated with effect size. The inclusion of race or family structure as covariates did not appear to alter the association between subjective SES and health. Controlling for school achievement was associated with a larger mean effect size than not controlling for school achievement.
Study quality
There was no difference between studies that were coded to be of high compared to low quality (Fisher’s Z = .093 and .098, respectively) in categorical summary analyses. In addition, when study quality was retained as a continuous variable, the slope of the regression line between study quality and effect size was nonsignificant (B = −0.002, SE = 0.008, p = .36).
Geographical region
Categorical summary analyses indicated significant between-groups differences for geographical region of the study. Specifically, studies conducted in Western Europe, Asia, North America, and Australia had significant positive mean effect sizes (Fisher’s Z = .185, .181, .071, .056, respectively) while studies conducted in Eastern Europe did not (Fisher’s Z = .042). Because of heterogeneity between studies from North America, each country was examined separately. These analyses indicated significant associations in Canada and the United States, but not in Mexico.
Discussion
The present meta-analysis examined the association between subjective SES and health outcomes during adolescence across 44 studies. Overall, results demonstrated a positive association such that higher subjective SES was associated with better health outcomes. The magnitude of the associations were similar to those observed in studies that have examined the subjective SES-health association in adults (e.g., Singh-Manoux et al., 2005) and in studies that have examined the objective SES–health association in youth (e.g., Chen et al., 2006). Several moderating variables were examined to further explain this association.
We examined four different types of subjective SES measures: society ladder, school ladder, Likert scale, and financial constraints. Results indicated that measuring subjective SES using the society ladder, school ladder, or Likert scale yielded similar effect sizes. These findings suggest that the association between subjective SES and health in adolescents is robust, and is not altered significantly by measuring slightly different constructs. Namely, the society ladder references income, education, and jobs compared to others in society and clearly reflects “socioeconomic status,” as do some of the Likert scales employed in the included studies. Other Likert scales are worded in such a way that the ratings are more closely tied to income, financial status, or wealth. School ladder may be theoretically more consistent with “sociometric status,” a form of social status that represents the respect and admiration individuals have in their face-to-face groups (Anderson, John, Keltner, & Kring, 2001). Despite these conceptual differences, as well as a variety of measurement (own status vs. family’s status; school vs. society vs. neighborhood comparison groups; Likert scale vs. 10-point ladder) and analytical differences (categorical vs. continuous), overall associations were largely similar between these three measures of subjective SES. One measure of subjective SES yielded stronger associations with health outcomes than the others: perception of financial constraints. It is possible that perception of financial constraints reflects a different construct than the other measures of subjective SES. Adolescents who perceive financial constraints or difficulties in their households may be those at the very bottom of the socioeconomic gradient. This measure may detect adolescents living in poverty, who experience material deprivation in addition to low social status, which may put them at greater risk for experiencing stress and other negative health outcomes.
In terms of health outcomes, subjective SES showed the largest effect sizes for mental health outcomes, followed by self-rated health, and physical health outcomes, all of which were positively associated with subjective SES. Within mental health outcomes, depression was most strongly linked to subjective SES, followed by general psychological well-being and other psychological variables. Perception of socioeconomic rank is thought to influence health outcomes through psychological processes (Operario et al., 2004; Wilkinson, 1999), and associated biological processes and harmful coping behaviors. The present results corroborate the idea that subjective SES is closely tied to psychological processes and outcomes. The finding that subjective SES is robustly associated with global self-rated health is important because self-rated health is considered to be a strong indicator of physical health status and predictor of future mortality (Idler & Benyamini, 1997; Singh-Manoux et al., 2006). In addition, these results mirror those in the adult literature (e.g., Singh-Manoux et al., 2005), which indicates that the relation between subjective SES and health may be similar in adolescents and adults. Results varied depending on the type of physical health outcome measured. For instance, subjective SES was strongly associated with general physical health symptoms, while the effect size of the association between SES and obesity was much smaller, and biomarkers of physical health were not associated with subjective SES. It is possible that general symptoms, such as headaches and stomachaches may be psychosomatic, and thus, are more strongly and immediately associated with psychological processes. In contrast, changes in biomarkers of health may take longer to emerge, which may explain why few associations were observed in these “healthy” community samples of adolescents. It will be important to examine associations between subjective SES and biomarkers of physical health in population-representative samples that would include unhealthy and at-risk youth.
The current pattern of results across health outcomes may also be linked to the measurement of these outcomes: subjective SES was more strongly associated with self-reported measures of health (e.g., self-rated health, general symptoms, psychological well-being) than measured health outcomes (e.g., height/weight, blood pressure). This could be due to shared variance across self-reports (i.e., mono-informant bias), reverse causation, or a confounding third variable. Garbarski (2010) examined whether subjective SES and health are reciprocally associated with one another in a sample of adults. Results indicated that subjective SES had an effect on self-rated health that was stronger than the reverse association; however, relations between subjective SES and health status were reciprocal, and depressive symptoms affected subjective ratings of SES. In contrast, other studies have demonstrated that chronic negative affect (Operario et al., 2004) and other psychosocial variables (e.g., self-esteem, mastery, trust; Lundberg & Kristenson, 2008) do not uniquely confound the association between subjective SES and self-rated health. Moreover, experimentally induced shifts in negative mood did not affect subjective SES ratings or the association between subjective SES and self-rated health (Kraus et al., 2013). To date, there has been little examination of third variables or reciprocal relations between subjective SES and health in adolescents. Longitudinal associations between low subjective SES and subsequent poor self-rated health (Goodman, Huang, Schafer-Kalkhoff, & Adler, 2007) suggest that this relation is not merely a measurement artifact in this age group. However, more research is needed to measure and test potential confounds of the association between subjective SES and self-reported health outcomes in adolescence.
Present results showed a lack of association between subjective SES and substance-use-related health behaviors. The cost of purchasing alcohol, cigarettes, or illicit drugs may be protective against initiation or maintenance of these behaviors in adolescents. Other health behaviors, including diet and physical activity, showed a significant positive association. Finally, sexual health behaviors were inversely related to subjective SES, such that high status was associated with more risky sexual health behaviors in the one study that measured this outcome. Health behaviors are thought to be established in youth and extend into adulthood, and contribute greatly to morbidity and mortality from cardiovascular disease, cancer, and other conditions (Kolbe, Kann, & Collins, 1993). However, this review suggests a lack of association between subjective SES and substance-related behaviors during adolescence.
Geographic region of the study was examined as a potential moderator. Results showed the largest effects of subjective SES and adolescent health in Western Europe (U.K., Finland, Sweden) and Asia (China, South Korea). Slightly smaller effect sizes were observed in the United States, Canada, and Australia, with no association observed in Eastern Europe (Hungary, Serbia) and Mexico. Cross-country differences may be related to economic variables (e.g., gross domestic product, societal income inequality), sociocultural variables (e.g., collectivism vs. individualism, capitalism vs. socialism vs. communism), or study methodology (e.g., subjective SES measure, health outcomes). Income inequality is of particular interest, since more unequal distribution of income in society is thought to accentuate relative SES differences (Wilkinson, 1999). Examination of the hypothesis that subjective SES–health association was stronger in more unequal countries could not be examined due to the potential confound of study variables. For instance, no associations were observed in the studies conducted in Mexico (a highly unequal society); however, it is unclear whether these findings were associated with income inequality or sociocultural variables, or the fact that these studies examined substance-related health behaviors. Future studies that use more similar subjective SES measures and examine similar health outcomes may help to elucidate the specific moderating role of economic, cultural, and political influences on the subjective SES-health association.
We examined the influence of inclusion of a variety of covariates on the association between subjective SES and health. Results indicated that larger effect sizes were found in studies that did not control for covariates, which is an expected finding. Specifically, studies that controlled for age and sex had lower mean effect sizes than studies that did not. However, the association between subjective SES and health did not differ as age of the sample increased or in studies with a greater proportion of female adolescents. Inclusion of race as a covariate did not moderate the association. A lack of reporting of race outside of the United States precluded further examination of this variable. Future research in this area should report racial breakdown to examine how race may affect the subjective SES–health association, especially since racial differences have been observed in this area (Goodman et al., 2003). It is interesting to note that larger effect sizes were observed when school achievement (e.g., marks at school, future academic goals) was entered as a covariate. School achievement may be conceptualized as an adolescent-specific objective indicator of SES, as it is indicative of future educational attainment. Future objective SES may have a suppressive effect on subjective SES, since controlling for this measure strengthened the relation between subjective SES and health. Thus, it may be important to control for adolescent-specific objective SES indicators, including school achievement, current employment, and pocket money, when examining the association between subjective SES and health.
We found no difference in the magnitude of the association between effects that controlled for objective SES and effects did not control for objective SES. These results suggest that the influence of subjective SES on health is independent of objective SES, which is supportive of the idea that subjective SES reflects a person’s relative social position, while objective SES is reflective of absolute position. Less than half of the effect sizes controlled for objective SES, with most of these using parental education as the objective SES indicator. More studies that measure both objective and subjective SES are required to tease apart these associations across health outcomes.
The graded association between SES and health is well established (Adler et al., 1994); however, precise mechanisms of how SES “gets under the skin” to affect health remain unclear. Several mechanisms have been proposed and examined (see Adler & Stewart, 2010 for a review), including material conditions (differential access to health care, environmental exposure to hazards; Lynch, Davey Smith, Kaplan, & House, 2000), psychosocial factors (stress, social support), and health behaviors. The importance of relative rank and social comparison has also been emphasized (Wilkinson, 1999). Rank is thought to be a fundamental process of social life, both in humans and in animals. Humans place themselves into hierarchies based on numerous dimensions. Research in nonhuman primates has demonstrated the importance of subordinate rank on physical and psychological stress (Sapolsky, 2005). The importance of measuring subjective SES emerged from these lines of research.
Socioeconomic status is posited to be shaped by two related, but relatively independent processes: material resources (education, wealth, occupation) and subjective perception of social rank (Kraus, Piff, Mendoza-Denton, Rheinschmidt, & Keltner, 2012). Material resources help to determine access to goods and services, while rank shapes perception of one’s standing. Based on this conceptualization, objective and subjective SES may be differentially associated with different health outcomes. Indeed, in the present study, we found that subjective SES was most strongly linked to health outcomes that are closely tied to psychological processes, including self-rated health, depression, psychological well-being, and general physical health symptoms. Over time, low subjective SES and associated psychological processes may predict worsened physical health outcomes. However, further evidence is necessary to support this hypothesis.
In addition to these theoretical implications, the findings from the current study also have implications for ongoing research in this field. Previously, Braveman et al. (2005) recommended that researchers take an outcome-specific and socioeconomic-group-specific approach to measuring SES. Based on current findings, we suggest that future research measure as much relevant socioeconomic information as possible, including subjective SES, traditional measures of objective SES, and area or neighborhood SES, when investigating the role of SES on adolescent health. It is also critical to clearly specify the precise SES factors measured and why these were chosen, and to provide adequate analytical information to understand the unique influence of each indicator. It is also recommended that researchers designing surveys of child and adolescent health begin to include measures of subjective SES in addition to measures of objective and area SES. These ratings are quick and easy to complete, and we have shown that subjective SES may be an independent construct from objective SES in adolescents. Results appear largely similar when the society ladders, school ladders, and Likert scales measuring perceived family SES are employed. However, it is recommended that the Subjective Social Status Scale–Youth Version be employed across studies and across countries for increased consistency and comparability of results. This scale may be used flexibly across different cultural contexts, since explanations of social status and reference points may be modified.
Future research in this area should build on the results of this review to understand how subjective and objective SES affect specific health outcomes, especially biomarkers of health and health behaviors. In addition, research is required to better understand the relations between subjective and objective measures of SES, as well as to uncover mediating and moderating factors between these measures of SES and health outcomes. Finally, additional research is needed to understand how subjective and objective SES affects health across countries, with different health policies, income inequality, and sociocultural influences.
This review and meta-analysis provides an important contribution to the growing literature on subjective SES and health. There is evidence of an association between subjective SES and adolescent health outcomes. Future research should incorporate both subjective and objective measures of SES to help understand pathways to health disparities. This knowledge, together with social policy action, may help to reduce disparities in health across the life span. As this field continues to expand, it is important for researchers to consider the measurement of subjective SES on the observed results and to streamline the number of subjective SES measures used by researchers. Theoretically, examining the overall association between subjective SES and health in adolescents contributes to the limited literature on the SES gradient in health in this age group. Moreover, it provides insight into the role of subjective status in the pathway from social inequalities to disparities in health outcomes.
Acknowledgments
This research was made possible through funding support from the Canadian Institutes of Health Research Canada Graduate Scholarships Award (Elizabeth C. Quon CGM 89256) and New Investigator Award (Jennifer J. McGrath MSH95353), and the Quebec Inter-University Centre for Social Statistics. We thank Danielle Kingdon for her help with reliability coding.
References
References marked with an asterisk indicate studies included in the meta-analysis.
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn R, Syme SL. Socioeconomic status and health: The challenge of the gradient. American Psychologist. 1994;49:15–24. doi: 10.1037/0003-066X.49.1.15. [DOI] [PubMed] [Google Scholar]
- Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy White women. Health Psychology. 2000;19:586–592. doi: 10.1037/0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- Adler NE, Ostrove JM. Socioeconomic status and health: What we know and what we don’t. Annals of the New York Academy of Sciences. 1999;896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- Adler NE, Stewart J. Health disparities across the lifespan: Meaning, methods, and mechanisms. Annals of the New York Academy of Sciences. 2010;1186:5–23. doi: 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- Anderson C, John OP, Keltner D, Kring AM. Who attains social status? Effects of personality and physical attractiveness in social groups. Journal of Personality and Social Psychology. 2001;81:116–132. doi: 10.1037/0022-3514.81.1.116. [DOI] [PubMed] [Google Scholar]
- *.Åslund C, Leppert J, Starrin B, Nilsson KW. Subjective social status and shaming experiences in relation to adolescent depression. Archives of Pediatrics & Adolescent Medicine. 2009;163:55–60. doi: 10.1001/archpedi.163.1.55. [DOI] [PubMed] [Google Scholar]
- Bengtsson C, Nordmark B, Klareskog L, Lundberg I, Alfredsson L the EIRA Study Group. Socioeconomic status and the risk of developing rheumatoid arthritis: Results from the Swedish EIRA study. Annals of the Rheumatic Diseases. 2005;64:1588–1594. doi: 10.1136/ard.2004.031666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Marchi KS, Metzler M, Posner S. Socioeconomic status in health research: One size does not fit all. JAMA: Journal of the American Medical Association. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Chen E, Martin AD, Matthews KA. Socioeconomic status and health: Do gradients differ within childhood and adolescence? Social Science & Medicine. 2006;62:2161–2170. doi: 10.1016/j.socscimed.2005.08.054. [DOI] [PubMed] [Google Scholar]
- Chen E, Matthews KA, Boyce WT. Socioeconomic differences in children’s health: How and why do these relationships change with age? Psychological Bulletin. 2002;128:295–329. doi: 10.1037/0033-2909.128.2.295. [DOI] [PubMed] [Google Scholar]
- *.Chen E, Paterson LQ. Neighborhood, family, and subjective socioeconomic status: How do they relate to adolescent health? Health Psychology. 2006;25:704–714. doi: 10.1037/0278-6133.25.6.704. [DOI] [PubMed] [Google Scholar]
- Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Statistics in Medicine. 2000;19:3127–3131. doi: 10.1002/1097-0258(20001130)19:22<3127::AID-SIM784>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- *.Cho HJ, Khang YH. Family Affluence Scale, other socioeconomic position indicators, and self-rated health among South Korean adolescents: Findings from the Korea Youth Risk Behavior Web-based Survey (KYRBWS) Journal of Public Health. 2010;18:169–178. doi: 10.1007/s10389-009-0299-9. [DOI] [Google Scholar]
- Cooper H, Hedges LV. The handbook of research synthesis. New York, NY: Robert Sage Foundation; 1994. [Google Scholar]
- *.Correa-Velez I, Gifford SM, Barnett AG. Longing to belong: Social inclusion and wellbeing among youth with refugee backgrounds in the first three years in Melbourne, Australia. Social Science & Medicine. 2010;71:1399–1408. doi: 10.1016/j.socscimed.2010.07.018. [DOI] [PubMed] [Google Scholar]
- Currie C, Molcho M, Boyce W, Holstein B, Torsheim T, Richter M. Researching health inequalities in adolescents: The development of the Health Behaviour in School-Aged Children (HBSC) family affluence scale. Social Science & Medicine. 2008;66:1429–1436. doi: 10.1016/j.socscimed.2007.11.024. [DOI] [PubMed] [Google Scholar]
- Davis JA. Status symbols and the measurement of status perception. Sociometry. 1956;19:154–165. doi: 10.2307/2785629. [DOI] [Google Scholar]
- Durlak JA. How to select, calculate, and interpret effect sizes. Journal of Pediatric Psychology. 2009;34:917–928. doi: 10.1093/jpepsy/jsp004. [DOI] [PubMed] [Google Scholar]
- *.Finkelstein DM, Kubzansky LD, Goodman E. Social status, stress, and adolescent smoking. Journal of Adolescent Health. 2006;39:678–685. doi: 10.1016/j.jadohealth.2006.04.011. [DOI] [PubMed] [Google Scholar]
- *.Fröjd S, Marttunen M, Pelkonen M, von der Pahlen B, Kaltiala-Heino R. Perceived financial difficulties and maladjustment outcomes in adolescence. European Journal of Public Health. 2006;16:542– 548. doi: 10.1093/eurpub/ckl012. [DOI] [PubMed] [Google Scholar]
- Garbarski D. Perceived social position and health: Is there a reciprocal relationship. Social Science & Medicine. 2010;70:692–699. doi: 10.1016/j.socscimed.2009.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glendinning A, Love JG, Hendry LB, Shucksmith J. Adolescence and health inequalities: Extensions to Macintyre and West. Social Science & Medicine. 1992;35:679– 687. doi: 10.1016/0277-9536(92)90006-C. [DOI] [PubMed] [Google Scholar]
- Goodman E. The role of socioeconomic status gradients in explaining differences in US adolescents’ health. American Journal of Public Health. 1999;89:1522–1528. doi: 10.2105/AJPH.89.10.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Goodman E, Adler NE, Daniels SR, Morrison JA, Slap GB, Dolan LM. Impact of objective and subjective social status on obesity in a biracial cohort of adolescents. Obesity Research. 2003;11:1018–1026. doi: 10.1038/oby.2003.140. [DOI] [PubMed] [Google Scholar]
- *.Goodman E, Adler NE, Kawachi I, Frazier AL, Huang B, Colditz GA. Adolescents’ perceptions of social status: Development and evaluation of a new indicator. Pediatrics. 2001;108(2):e31. doi: 10.1542/peds.108.2.e31. [DOI] [PubMed] [Google Scholar]
- *.Goodman E, Huang B, Schafer-Kalkhoff T, Adler N. Perceived socioeconomic status: A new type of identity which influences adolescents’ self-rated health. Journal of Adolescent Health. 2007;41:479–487. doi: 10.1016/j.jadohealth.2007.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Goodman E, McEwen BS, Dolan LM, Schafer-Kalkhoff T, Adler NE. Social disadvantage and adolescent stress. Journal of Adolescent Health. 2005;37:484–492. doi: 10.1016/j.jadohealth.2004.11.126. [DOI] [PubMed] [Google Scholar]
- *.Grotvedt L, Stigum H, Hovengen R, Graff-Iversen S. Social differences in smoking and snuff use among Norwegian adolescents: A population-based survey. BMC Public Health. 2008;8:322. doi: 10.1186/1471-2458-8-322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Hamilton HA, Noh S, Adlaf EM. Perceived financial status, health, and maladjustment in adolescence. Social Science & Medicine. 2009;68:1527–1534. doi: 10.1016/j.socscimed.2009.01.037. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- *.Iversen AC, Holsen I. Inequality in health, psychosocial resources and health behavior in early adolescence: The influence of different indicators of socioeconomic position. Child Indicators Research. 2008;1:291–302. doi: 10.1007/s12187-008-9015-5. [DOI] [Google Scholar]
- *.Janssen I, Boyce WF, Simpson K, Pickett W. Influence of individual- and area-level measures of socioeconomic status on obesity, unhealthy eating, and physical inactivity in Canadian adolescents. American Journal of Clinical Nutrition. 2006;83:139–145. doi: 10.1093/ajcn/83.1.139. [DOI] [PubMed] [Google Scholar]
- *.Jovic-Vranes A, Jankovic J, Vasic V, Jankovic S. Self-perceived health and psychological well-being among Serbian school-children and adolescents: Data from National Health Survey. Central European Journal of Medicine. 2011;6:400–406. doi: 10.2478/s11536-011-0035-z. [DOI] [Google Scholar]
- *.Jung SH, Watt RG, Sheiham A, Ryu JI, Tsakos G. Exploring pathways for socio-economic inequalities in self-reported oral symptoms among Korean adolescents. Community Dentistry and Oral Epidemiology. 2011;39:221–229. doi: 10.1111/j.1600-0528.2010.00595.x. [DOI] [PubMed] [Google Scholar]
- Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: A review of the literature. Circulation. 1993;88:1973–1998. doi: 10.1161/01.CIR.88.4.1973. [DOI] [PubMed] [Google Scholar]
- *.Karvonen S, Rahkonen O. Subjective social status and health in young people. Sociology of Health & Illness. 2011;33:372–383. doi: 10.1111/j.1467-9566.2010.01285.x. [DOI] [PubMed] [Google Scholar]
- Kolbe LJ, Kann L, Collins JL. Overview of the Youth Risk Behavior Surveillance System. Public Health Reports. 1993;108(Suppl 1):2–10. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1403301/ [PMC free article] [PubMed] [Google Scholar]
- Kramer MS, Séguin L, Lydon J, Goulet L. Socio-economic disparities in pregnancy outcome: Why do the poor fare so poorly? Paediatric and Perinatal Epidemiology. 2000;14:194–210. doi: 10.1046/j.1365-3016.2000.00266.x. [DOI] [PubMed] [Google Scholar]
- Kraus MW, Adler N, Chen TWD. Is the association of subjective SES and self-rated health confounded by negative mood? An experimental approach. Health Psychology. 2013;32:138–145. doi: 10.1037/a0027343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraus MW, Piff PK, Mendoza-Denton R, Rheinschmidt ML, Keltner D. Social class, solipsism, and contextualism: How the rich are different from the poor. Psychological Review. 2012;119:546–572. doi: 10.1037/a0028756. [DOI] [PubMed] [Google Scholar]
- *.Lemeshow AR, Fisher L, Goodman E, Kawachi I, Berkey CS, Colditz GA. Subjective social status in the school and change in adiposity in female adolescents. Archives of Pediatric Adolescent Medicine. 2008;162:23–28. doi: 10.1001/archpediatrics.2007.11. [DOI] [PubMed] [Google Scholar]
- Lowry R, Kann L, Collins JL, Kolbe LJ. The effect of socioeconomic status on chronic disease risk behaviors among US adolescents. JAMA: Journal of the American Medical Association. 1996;276:792–797. doi: 10.1001/jama.1996.03540100036025. [DOI] [PubMed] [Google Scholar]
- Lundberg J, Kristenson M. Is subjective status influenced by psychosocial factors? Social Indicators Research. 2008;89:375–390. doi: 10.1007/s11205-008-9238-3. [DOI] [Google Scholar]
- Lynch JW, Davey Smith G, Kaplan GA, House JS. Income inequality and mortality: Importance to health of individual income, psychosocial environment, or material conditions. British Medical Journal. 2000;320:1200. doi: 10.1136/bmj.320.7243.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Magklara K, Skapinakis P, Niakas D, Bellos S, Zissi A, Stylianidis S, Mavreas V. Socioeconomic inequalities in general and psychological health among adolescents: A cross-sectional study in senior high schools in Greece. International Journal for Equity in Health. 2010;9:3. doi: 10.1186/1475-9276-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot MG, Shipley MJ, Rose G. Inequalities in death: Specific explanations of a general pattern? The Lancet. 1984;323:1003–1006. doi: 10.1016/S0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- *.Mistry RS, Benner AD, Tan CS, Kim SY. Family economic stress and academic well-being among Chinese-American youth: The influence of adolescents’ perceptions of economic strain. Journal of Family Psychology. 2009;23:279–290. doi: 10.1037/a0015403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Oh IH, Cho Y, Park SY, Oh C, Choe BK, Choi JM, Yoon TY. Relationship between socioeconomic variables and obesity in Korean adolescents. Journal of Epidemiology. 2011;21:263–270. doi: 10.2188/jea.JE20100099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Operario D, Adler NE, Williams DR. Subjective social status: Reliability and predictive utility for global health. Psychology & Health. 2004;19:237–246. doi: 10.1080/08870440310001638098. [DOI] [Google Scholar]
- Orwin RG. A fail-safe N for effect size in meta-analysis. Journal of Educational Statistics. 1983;8:157–159. doi: 10.2307/1164923. [DOI] [Google Scholar]
- Paeratakul S, Lovejoy J, Ryan D, Bray G. The relation of gender, race and socioeconomic status to obesity and obesity comorbidities in a sample of US adults. International Journal of Obesity and Related Metabolic Disorders. 2002;26:1205–1210. doi: 10.1038/sj.ijo.0802026. [DOI] [PubMed] [Google Scholar]
- *.Page RM, Simonek J, Ihász F, Hantiu I, Uvacsek M, Kalabiska I, Klarova R. Self-rated health, psychosocial functioning, and other dimensions of adolescent health in Central and Eastern European adolescents. The European Journal of Psychiatry. 2009;23:101–114. doi: 10.4321/S0213-61632009000200004. [DOI] [Google Scholar]
- *.Piko BF. Satisfaction with life, psychosocial health and materialism among Hungarian youth. Journal of Health Psychology. 2006;11:827–831. doi: 10.1177/1359105306069072. [DOI] [PubMed] [Google Scholar]
- *.Piko B, Fitzpatrick KM. Does class matter? SES and psychosocial health among Hungarian adolescents. Social Science & Medicine. 2001;53:817–830. doi: 10.1016/S0277-9536(00)00379-8. [DOI] [PubMed] [Google Scholar]
- *.Piko BF, Fitzpatrick KM. Socioeconomic status, psychosocial health and health behaviours among Hungarian adolescents. European Journal of Public Health. 2007;17:353–360. doi: 10.1093/eurpub/ckl257. [DOI] [PubMed] [Google Scholar]
- *.Piko BF, Gibbons FX. Behavioral and psychosocial influences of risk perception among Hungarian adolescents. International Journal of Public Health. 2008;53:131–138. doi: 10.1007/s000-00-7054-9. [DOI] [PubMed] [Google Scholar]
- *.Piko BF, Hamvai C. Parent, school and peer-related correlates of adolescents’ life satisfaction. Children and Youth Services Review. 2010;32:1479–1482. doi: 10.1016/j.childyouth.2010.07.007. [DOI] [Google Scholar]
- *.Piko BF, Keresztes N. Self-perceived health among early adolescents: Role of psychosocial factors. Pediatrics International. 2007;49:577–583. doi: 10.1111/j.1442-200X.2007.02430.x. [DOI] [PubMed] [Google Scholar]
- *.Piko BF, Skultéti D, Luszczynska A, Gibbons FX. Social orientations and adolescent health behaviours in Hungary. International Journal of Psychology. 2010;45:12–20. doi: 10.1080/00207590903030279. [DOI] [PubMed] [Google Scholar]
- *.Piko BF, Vazsonyi AT. Leisure activities and problem behaviours among Hungarian youth. Journal of Adolescence. 2004;27:717– 730. doi: 10.1016/j.adolescence.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Ritterman ML. Perceived social status and adolescent health and risk behaviors: A systematic review. Berkeley, CA: Institute for the Study of Societal Issues, UC Berkeley; 2007. (ISSC Working Paper Series 2006–2007, 24) Retrieved from http://escholarship.org/uc/item/01s0w5m9. [Google Scholar]
- *.Ritterman ML. Doctoral dissertation. 2010. Social hierarchy and health among adolescents: The role of perceived class identity. Retrieved from ProQuest® Dissertations & Theses (Publication no. 3413551) [Google Scholar]
- *.Ritterman ML, Fernald LC, Ozer EJ, Adler NE, Gutierrez JP, Syme SL. Objective and subjective social class gradients for substance use among Mexican adolescents. Social Science & Medicine. 2009;68:1843–1851. doi: 10.1016/j.socscimed.2009.02.048. [DOI] [PubMed] [Google Scholar]
- Rosenberg MS, Adams D, Gurevitch J. Statistical software for meta-analysis (version 2.0) Sunderland, MA: Sinauer Associates; 2000. MetaWin. [Google Scholar]
- Rosenthal R. Meta-analytic procedures for social research. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- Sapolsky RM. The influence of social hierarchy on primate health. Science. 2005;308:648–652. doi: 10.1126/science.1106477. [DOI] [PubMed] [Google Scholar]
- Sawyer SM, Afifi RA, Beringer LH, Blakemore SJ, Dick B, Ezeh AC, Patton GC. Adolescence: A foundation for future health. Lancet. 2012;379:1630–1640. doi: 10.1016/S0140-6736(12)600172-5. [DOI] [PubMed] [Google Scholar]
- Schmidt FL, Oh IS, Hayes TL. Fixed-versus random-effects models in meta-analysis: Model properties and an empirical comparison of differences in results. British Journal of Mathematical & Statistical Psychology. 2009;62:97–128. doi: 10.1348/000711007X255327. [DOI] [PubMed] [Google Scholar]
- *.Shek DTL. Economic stress, psychological well-being and problem behavior in Chinese adolescents with economic disadvantage. Journal of Youth and Adolescence. 2003;32:259–266. doi: 10.1023/A:1023080826557. [DOI] [Google Scholar]
- *.Shek DTL. Economic stress, emotional quality of life, and problem behavior in Chinese adolescents with and without economic disadvantage. Social Indicators Research. 2005;71:363–383. doi: 10.1007/s11205-004-8028-9. [DOI] [Google Scholar]
- Singh-Manoux A, Adler NE, Marmot MG. Subjective social status: Its determinants and its association with measures of ill-health in the Whitehall II study. Social Science & Medicine. 2003;56:1321–1333. doi: 10.1016/S0277-9536(02)00131-4. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Marmot MG, Adler NE. Does subjective social status predict health and change in health status better than objective status? Psychosomatic Medicine. 2005;67:855–861. doi: 10.1097/01.psy.0000188434.52941.a0. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Martikainen P, Ferrie J, Zins M, Marmot M, Goldberg M. What does self rated health measure? Results from the British Whitehall II and French Gazel cohort studies. Journal of Epidemiology and Community Health. 2006;60:364–372. doi: 10.1136/jech.2005.039883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Spelman AR, Spitz MR, Kelder SH, Prokhorov AV, Bondy ML, Frankowski RF, Wilkinson AV. Cognitive susceptibility to smoking: Two paths to experimenting among Mexican origin youth. Cancer Epidemiology, Biomarkers & Prevention. 2009;18:3459–3467. doi: 10.1158/1055-9965.EPI-09-0765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Sweet E. “If your shoes are raggedy you get talked about”: Symbolic and material dimensions of adolescent social status and health. Social Science & Medicine. 2010;70:2029–2035. doi: 10.1016/j.socscimed.2010.02.032. [DOI] [PubMed] [Google Scholar]
- *.Thurston RC, Matthews KA. Racial and socioeconomic disparities in arterial stiffness and intima media thickness among adolescents. Social Science & Medicine. 2009;68:807– 813. doi: 10.1016/j.socscimed.2008.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Unger JB, Sun P, Johnson CA. Socioeconomic correlates of smoking among an ethnically diverse sample of 8th grade adolescents in Southern California. Preventive Medicine. 2007;44:323–327. doi: 10.1016/j.ypmed.2006.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Vukovic DS, Bjegovic VM. Brief report: Risky sexual behavior of adolescents in Belgrade: Association with socioeconomic status and family structure. Journal of Adolescence. 2007;30:869–877. doi: 10.1016/j.adolescence.2007.06.005. [DOI] [PubMed] [Google Scholar]
- *.Wadsworth M, Compas B. Coping with family conflict and economic strain: The adolescent perspective. Journal of Research on Adolescence. 2002;12:243–274. doi: 10.1111/1532-7795.00033. [DOI] [Google Scholar]
- West P. Health inequalities in the early years: Is there equalisation in youth? Social Science & Medicine. 1997;44:833–858. doi: 10.1016/S0277-9536(96)00188-8. [DOI] [PubMed] [Google Scholar]
- *.West P, Sweeting H, Young R, Kelly S. The relative importance of family socioeconomic status and school-based peer hierarchies for morning cortisol in youth: An exploratory study. Social Science & Medicine. 2010;70:1246–1253. doi: 10.1016/j.socscimed.2009.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Wilkinson AV, Shete S, Spitz MR, Swann AC. Sensation seeking, risk behaviors, and alcohol consumption among Mexican origin youth. Journal of Adolescent Health. 2011;48:65–72. doi: 10.1016/j.jadohealth.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Wilkinson AV, Shete S, Vasudevan V, Prokhorov AV, Bondy ML, Spitz MR. Influence of subjective social status on the relationship between positive outcome expectations and experimentation with cigarettes. Journal of Adolescent Health. 2009;44:342–348. doi: 10.1016/j.jadohealth.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson RG. Health, hierarchy, and social anxiety. Annals of the New York Academy of Sciences. 1999;896:48–63. doi: 10.1111/j.1749-6632.1999.tb08104.x. [DOI] [PubMed] [Google Scholar]
- Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: How education, income, and occupation contribute to risk factors for cardiovascular disease. American Journal of Public Health. 1992;82:816–820. doi: 10.2105/AJPH.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Zaborskis A, Sumskas L, Maser M, Pudule I. Trends in drinking habits among adolescents in the Baltic countries for the period of transition: HBSC survey results, 1993–2002. BMC Public Health. 2006;6(67) doi: 10.1186/1471-2458-6-67. [DOI] [PMC free article] [PubMed] [Google Scholar]