Abstract
Objective
This study examined the effects of childhood ADHD symptoms, both inattention and hyperactivity impulsivity, on the development of smoking in male and female adolescents.
Method
Twin difference methods controlled for shared genetic and environmental confounders in three population-based, same-sex twin samples (N=3762; 64% monozygotic). One cohort oversampled female adolescents with ADHD, beginning in childhood. Regressions of childhood inattentive and hyperactive-impulsive symptoms were conducted to predict smoking outcomes by age 17. ADHD effects were divided into those shared between twins in the pair and non-shared, or different within pairs.
Results
Adolescents with more severe ADHD as children were more likely to initiate smoking and to start smoking younger. ADHD symptoms in females were associated to a greater degree with daily smoking, more cigarettes per day, and dependence than were ADHD symptoms in males. Monozygotic female twins with greater attentional problems than their co-twins had greater nicotine involvement, consistent with possible causal influence. These effects remained when co-occurring externalizing behaviors and stimulant medication were considered. Hyperactivity-impulsivity, while also more strongly related to smoking for female adolescents, appeared primarily non-causal.
Conclusions
Smoking initiation and escalation are affected differentially by ADHD subtype and gender. The association of inattention to smoking for female adolescents may be causal, whereas hyperactivity-impulsivity appears to act indirectly, through shared propensities for both ADHD and smoking.
INTRODUCTION
Cigarette use among U.S. adolescents has declined markedly [1], reflecting successful policy changes and health initiatives. Nevertheless, it remains a persistent problem, with 38% of 12-graders having smoked tobacco cigarettes [2] and the rising popularity of e-cigarettes prompting a new warning from the Surgeon General[3]. Because nicotine is the substance most consistently linked to attention- deficit hyperactivity disorder (ADHD)[4], clarifying precisely how ADHD contributes to smoking is imperative. Toward this objective, prospective clinical samples have established that adolescents with ADHD are more likely to initiate smoking early [5] and escalate to daily smoking[6]. Prevention of these earlier stages of smoking, which mediate associations between genetic risk and nicotine dependence [7], is essential.
Yet evidence for whether female adolescents with ADHD are at heightened risk for substance problems relative to controls, as males are, has been inconsistent[8–10]. With these few exceptions, most prospective clinical samples of children with ADHD including substance outcomes are largely or exclusively male[11]. ADHD was long considered to occur much more frequently in males than females, and males were more likely to be referred for treatment by teachers[12]. Inclusion of a predominantly inattentive subtype in DSM-IV identified more females, with DSM-5 estimates of a 2:1 male-to-female ADHD ratio in the general population. Accordingly, population-based samples are well-suited for studying both genders. However, they often struggle to recruit enough females with clinically significant ADHD, leaving unresolved whether male and female adolescents bear similar risk.
Moreover, although childhood ADHD typically begins prior to smoking initiation, we cannot assume that it causes smoking. The association might result instead from overlapping risks increasing the likelihood of both ADHD and smoking. For example, some prospective research casts doubt on whether ADHD confers a specific risk apart from co-occurring conduct (CD) and oppositional defiant disorders (ODD) or suggests its contribution may be limited to a specific symptom subtype[13]. Other prospective research has found that although CD reduced its effects, hyperactivity-impulsivity was still associated with increased likelihood of initiating smoking and developing dependence[14], although this independent association may be stronger for females[15]. There is also evidence that inattention and nicotine dependence may be particularly related[14, 16].
While a study of cousins, full- and half-siblings discordant for ADHD suggested ADHD-drug disorder associations appeared partially due to causal influence[17], monozygotic (MZ) twin pairs who differ in ADHD might provide more definitive evidence of causality. Because MZ twins share essentially the same genetic sequence and rearing environment, differences within MZ pairs can only be due to unique, non-genetic influences[18]. If differences within dizgotic (DZ) but not MZ pairs are found, this suggests genetic factors influence both ADHD and smoking, as DZ pairs share only 50% of their segregating genetic material. Familial environment is an important confound if within-pair differences are absent, since both twin types share factors in the rearing environment, including socioeconomic status (SES) and prenatal nicotine exposure.
In the current study, prospective and twin difference designs were combined to explore the etiology of adolescent smoking in twins discordant for ADHD. Whether differences within pairs in number and type of ADHD symptoms might lead to differences in smoking was examined, along with gender moderation of effects. This quasi-experimental, causally informative design integrates genetic and social science perspectives and provides critical information for public health initiatives[19]. Because its sensitivity decreases when twin correlations on the putative causal factor are high[20], combining multiple datasets helps ensure adequate statistical power for detecting significant within-pair differences in MZ pairs, particularly when testing whether effects are moderated by gender.
We hypothesized two mechanisms through which ADHD might accelerate nicotine involvement: 1) a shared externalizing propensity, represented primarily by hyperactivity-impulsivity, increases the likelihood of both ADHD and smoking, and 2) a non-shared, specific influence of inattention increases smoking. We hypothesized that this specific influence may be more salient for female adolescents. Because females typically have more inattentive than hyperactive-impulsive symptoms and experience greater impairment from inattention in academics and peer relationships during childhood [21], we examined whether risks from inattention extended to adolescent smoking. We also determined whether effects persisted after taking into account non-shared exposures predating ADHD (e.g., birth weight differences), co-occurring externalizing disorders (i.e., CD/ODD) and stimulant medication use. By combining datasets, including a cohort oversampling affected females, and using dimensional measures and multiple informants, we enhanced power to identify within-pair differences and gender moderation.
METHOD
Participants
A total of 3762 individuals (52% female) visited with parents at baseline, comprising 1881 like- sex twin pairs (64% MZ) from three community-ascertained cohorts in the Minnesota Twin Family Study (MTFS), a longitudinal investigation of the development of substance abuse. Twin pairs born in Minnesota identified from birth records were eligible if they lived within a day’s drive of the University of Minnesota and had no physical/psychological disability that would preclude completing the assessment.
One cohort was assessed at age 17; two were assessed at age 11 and followed to age 17. In one 11-year-old cohort, pairs were randomly allocated to screened or non-screened samples. The non-screened sample was recruited using the criteria above. In the screened cohort, the parent was interviewed to enrich the sample with twins showing academic disengagement and externalizing disorder symptoms. The family was recruited if at least one twin exceeded an empirically validated threshold that maximized sensitivity and specificity for identifying cases of externalizing disorders[22]. A higher allocation of females to the screened sample ensured participation of more affected females. After a complete description of the study was given, written informed consent was obtained from the parents, and written assents were obtained from the twins. Based on information obtained prior to recruitment, there were no significant differences between participating and non-participating families on parent-reported mental health or SES. Thus, the combined sample was representative of the Minnesota population for the target birth years (e.g., 9–8% were White; for further detail, see[22, 23]).
Assessments for all cohorts overlapped at age 17, with age 17 data available for 92.5% of the combined sample. Retention in the two cohorts followed prospectively was excellent, with no selective loss of those with more ADHD symptoms at baseline. Assessment of the cohort assessed only at age 17 was cross-sectional. Figure SF1 describes the sample, data utilized at each wave, and years during which cohorts were assessed.
Measures and Procedures
Non-shared exposures were indexed via birth weight from birth certificates; neurological injuries from parental report. A composite measure of SES represented the mean of four standardized scores: highest parental occupation status, mother’s and father’s highest degree, and household income.
Each parent and child was interviewed by a different interviewer, each of whom had a degree in psychology (or related field) and extensive training. Primary caregiver reports of twins, including lifetime ADHD prior to age 12 (consistent with DSM-5 onset) and DSM-IV nicotine dependence by age 17, were obtained with the Diagnostic Interview for Children and Adolescents-Revised (DICA–R;[24], modified to include DSM-IV. Twin reports of ADHD prior to age 12 (e.g., asking “When you were younger…”) were obtained with a parallel version of the DICA-R, CD and ODD were also assessed lifetime at baseline with the DICA-R. Self-reported nicotine dependence was assessed in twins at age 17 via a modified, expanded Substance Abuse Module (SAM) from the Composite International Diagnostic Interview[25].
Symptoms were assigned by consensus of two individuals with advanced clinical training (supervised by a Ph.D. clinical psychologist). A symptom was considered present if reported by parent or child and if frequency and severity met pre-established guidelines. Combining informants is recommended for etiological investigations involving ADHD, with inclusion of twin self-ratings essential for detecting differences within pairs [26]. Because different diagnostic systems were in place when each cohort was assessed, symptom counts were harmonized with DSM-IV (e.g., the inattentive count was prorated by multiplying by 1.5 for earlier cohorts assessed on only six of nine DSM-IV inattentive symptoms). Although analyses were based on symptom counts rather than diagnoses, many adolescents had clinically-relevant ADHD: 337 males and 201 females had ≥ 5 symptoms of either the predominantly inattentive or hyperactive-impulsive subtype, or both (Combined), including impairment.
Three composites reflecting highest level of smoking by age 17 were derived from items added to the SAM and a self- administered computerized measure: earliest age of initiation reported across assessments; progression to daily smoking (0 = none; 1 = initiated, never daily; 2 = daily smoker since age 16 only; 3 = daily smoker before age 16); and cigarettes per day (CPD) during heaviest use, adjusted for non-daily use (0 = none; 1 = < −CPD; 2 = −CPD; 3 = 1/2 pack; 4 = 1+ packs). When applicable, equivalent use of chewing tobacco was incorporated.
Statistical Analyses
Because none of the correlations between birth weight or neurological problems and either inattentive or hyperactive-impulsive symptoms in MZ or DZ pairs significantly differed from zero, these were not considered further. Choice of regression models was based on each outcome’s distribution. Age of initiation was explored via survival models implemented in the COXPH package in the R statistical program. Data were censored for those whose initiation status was still unknown by age 17. We used a gamma between-within model recommended for co-twin survival analysis [27], which uses a Wald test of β=0, distributed as χ2 with 1 degree of freedom. For progression to daily smoking, ordinal regression with proportional odds models was implemented in the MIXOR package in R. For CPD and nicotine dependence, linear mixed models with maximum likelihood estimation were implemented in SAS PROC MIXED; nicotine symptoms were log-transformed prior to analysis.
Individual-level models were fit using either the inattentive or hyperactivity-impulsivity symptom count as the predictor of each of four smoking outcomes. Individual-level models treated twins as individuals, yet accounted for correlations within pairs and generated appropriate standard errors [28] through random intercepts at the cluster (pair) level or shared frailty terms (for survival models[27]). Next, twin difference models divided significant individual-level effects of inattention or hyperactivity-impulsivity into those shared by twins in a pair (twin-pair average) and non-shared (within-pair difference). The within-pair effect represents the unique effect of ADHD after controlling for all shared confounders, measured or unmeasured. Models were conducted separately by gender if gender moderation was significant at the individual-level. If the within-pair effect was significant, whether this differed for MZ and DZ pairs was assessed. Models were repeated with MZ or DZ pairs only to obtain separate estimates for each. Power was estimated at 80% for detecting MZ-within-pair effects accounting for .7% of the variance in smoking outcomes and for detecting gender differences between male and female MZ-within-pair estimates accounting for 1.2% of the variance (see Appendix SA1).
RESULTS
Descriptive data regarding highest levels of smoking in the combined sample were consistent with aggregated trends for U.S. adolescents from 1990-present [1], including significantly greater smoking among male than female adolescents (Table 1). Consequently, ADHD effects on smoking were adjusted to remove confounding from specific demographic covariates, including gender, cohort, SES, and age at assessment. Although adjusting overall (i.e., individual-level) effects of ADHD for shared covariates reduced their size, all were highly significant (p <.0001).
Table 1.
Descriptive Statistics for Lifetime Smoking Involvement and DSM-IV Nicotine Dependence Symptoms by Age 17 in Three Combined Cohorts by Gender
| Combined Cohorts (N=345–647)a |
All Males (N=166–747) |
All Females (N=181–900) |
Male Versus Female Comparison | Gender Effect Sizec | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Measure of Nicotine Involvement (% and N) | % | N | % | N | % | N | χ2 | p | OR | 95% CI |
|
| ||||||||||
| Ever used tobacco | 59.9 | 2185 | 67.4 | 1178 | 53.0 | 1007 | 78.91 | <0.001 | 1.83 | 1.60, 2.10 |
| Ever smoked dailyb | 25.4 | 883 | 28.6 | 475 | 22.5 | 408 | 17.29 | <0.001 | 1.38 | 1.18, 1.61 |
| Ever used ≥10 cigarettes/chews per day | 14.4 | 498 | 17.5 | 289 | 11.6 | 209 | 24.85 | <0.001 | 1.62 | 1.34,1.97 |
| Combined Cohorts (N=345–647)a |
AH Males (N=166–747) |
AH Females (N=181–900) |
Male Versus Female Comparison | Gender Effect Sizec | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Measure of Nicotine Involvement (M and SD) | Mean | SD | Mean | SD | Mean | SD | t | p | d | 95% CI |
|
| ||||||||||
| Age of smoking initiation | 13.5 | 2.5 | 13.2 | 2.7 | 13.9 | 2.3 | 6.16 | <0.001 | 0.27 | 018,035 |
| DSM-IV Nicotine Dependence symptom countd | .64 | 1.4 | .73 | 1.4 | .56 | 1.3 | 3.79 | <0.001 | 0.13 | 006,020 |
N – 3457 (cigarettes per day), 3478 (daily smoking; dependence), 3629 (initiation age), and 3647 (ever used), or 92 – 97% of baseline sample.
Higher levels of smoking were combined into clinically meaningful categories above, though continuous or ordinal measures were used in regression analyses.
Effect sizes are expressed as odds ratios (OR) for categorical outcomes or Cohen’s d for quantitative outcomes. ORs significantly greater than 1 indicate a higher level of involvement for males than females (e.g., 1.38 = a 38% increase in the likelihood for males). For Cohen’s d, .2 corresponds to a small effect, with male gender associated with earlier initiation; males and females were reverse-coded for this comparison.
This raw nicotine dependence symptom count was log-transformed in regression analyses to mitigate positive skew.
Adjusted effects are shown for inattention (top of Table 2) and hyperactivity-impulsivity (bottom of Table 2). Estimates are provided separately by gender when gender moderation was significant. Effects on initiation are given as hazard ratios (HR), reflecting increased likelihood of initiating smoking during any specific year; effects on progression to daily smoking are given as odds ratios (OR). Both reflect increases associated with a 1 symptom increase in inattention or hyperactivity-impulsivity and are shown in bold if significantly different from 1. For CPD and dependence, ADHD, CPD, and nicotine symptoms were converted to standardized scores (mean=0, SD=1) based on the entire sample. Regression estimates for these models reflect the smoking increase associated with a 1 SD increase in inattention or hyperactivity-impulsivity and are in bold if significantly different from zero.
Table 2.
Results of Individual-Level and Twin Difference Analysesa of Baseline ADHD Symptoms on Smoking Initiation, Progression to Daily Smoking, Cigarettes Per Day, and DSM-IV Nicotine Dependence Symptoms by Age 17
| ADHD Inattentive Symptoms (raw- or z-score)
| |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Gender Moderation?b | Individual-Level Analysisc | Within-Pair Twin Difference Analysis (in complete pairs only) | |||||||
|
| |||||||||
| Smoking Involvement by Age 17 | All Twins N=3629 |
Dizygotic Pairs N=652 |
Monozygotic Pairs N=1154 |
||||||
| Initiation of Use – age in years | No | Hazard Ratiod | 95% CI | Hazard Ratio | 95% CI | p | Hazard Ratio | 95% CI | p |
|
| |||||||||
| 1.16 | 1.13, 1.20 | 1.06 | 1.01, 1.11 | 0.023 | 1.08 | 1.02, 1.14 | <0.010 | ||
|
| |||||||||
| Progression to Daily Smoking | Yes; Female>Male | All Twins N=3478 |
Dizygotic Pairs N=617 (321 female;296 male) |
Monozygotic Pairs N=1092 (570 female;522 male) |
|||||
|
| |||||||||
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | p | Odds Ratio | 95% CI | p | ||
|
|
|||||||||
| 0 = none | Female | Female | Female | Female | Female | Female | Female | Female | |
| 1 = initiated, never daily | 1.27 | 1.17, 1.37 | 1.12 | 0.99, 1.26 | 0.063 | 1.19 | 1.01, 1.40 | 0.041 | |
| 2 = smoking daily starting since age 16 | Male | Male | Male | Male | Male | Male | Male | Male | |
| 3 = smoking daily before age 16 | 1.19 | 1.11, 1.27 | 1.03 | 0.92, 1.14 | 0.609 | 1.06 | 0.92, 1.22 | 0.392 | |
|
| |||||||||
| Maximum Cigarettes Per Day(z)e | Yes; Female>Male | All Twins N=3457 |
Dizygotic Pairs N=609 (318 female;291 male) |
Monozygotic Pairs N=1085 (568 female;517 male) |
|||||
|
| |||||||||
| β | 95% CI | β | 95% CI | p | β | 95% CI | p | ||
|
|
|||||||||
| Female | Female | Female | Female | Female | Female | Female | Female | ||
| .17 | .13, .21 | .10 | .01, .18 | 0.030 | .17 | .10, .24 | <0.0001 | ||
| Male | Male | Male | Male | Male | Male | Male | Male | ||
| .07 | .03, .11 | −.04 | −.12, .05 | 0.421 | .01 | −.06, .08 | 0.749 | ||
|
| |||||||||
| Symptoms of Nicotine Dependence(z)e | Yes; Female>Male | All Twins N=3478 |
Dizygotic Pairs N=617 (321 female;296 male) |
Monozygotic Pairs N=1092 (570 female;522 male) |
|||||
|
| |||||||||
| β | 95% CI | β | 95% CI | p | β | 95% CI | p | ||
|
|
|||||||||
| Female | Female | Female | Female | Female | Female | Female | Female | ||
| .17 | .12, 21 | .10 | .01, .18 | 0.047 | .17 | .09, .25 | <0.0001 | ||
| Male | Male | Male | Male | Male | Male | Male | Male | ||
| .09 | .05, .14 | −.01 | −.09, .07 | 0.799 | .04 | −.03, .12 | 0.258 | ||
|
| |||||||||
| ADHD Hyperactive-Impulsive Symptoms (raw- or z-score) | |||||||||
|
| |||||||||
| Gender Moderation?b | Individual-Level Analysisc | Within-Pair Twin Difference Analysis (in complete pairs only) | |||||||
|
| |||||||||
| Smoking Involvement by Age 17 | All Twins N=3629 |
Dizygotic Pairs N=652 pairs |
Monozygotic Pairs N=1154 pairs |
||||||
|
| |||||||||
| Initiation of Use – age in years | No | Hazard Ratiod | 95% CI | Hazard Ratio | 95% CI | p | Hazard Ratio | 95% CI | p |
|
| |||||||||
| 1.24 | 1.20, 1.29 | 1.07 | 1.01, 1.14 | 0.029 | 1.06 | 0.98, 1.14 | 0.150 | ||
|
| |||||||||
| Progression to Daily Smokinge | Yes; Female>Male | All Twins N=3478 |
Dizygotic Pairs N=617 (321 female; 296 male) |
Monozygotic Pairs N=1092 (570 female; 522 male) |
|||||
|
| |||||||||
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | p | Odds Ratio | 95% CI | p | ||
|
|
|||||||||
| 0 = none | Female | Female | Female | Female | Female | Female | Female | Female | |
| 1 = initiated, never daily | 1.45 | 1.32, 1.59 | 1.31 | 1.14, 1.52 | <0.001 | 1.20 | 0.98, 1.45 | 0.073 | |
| 2 = smoking daily starting since age 16 | Male | Male | Male | Male | Male | Male | Male | Male | |
| 3 = smoking daily before age 16 | 1.24 | 1.15, 1.34 | 1.03 | 0.84, 1.26 | 0.773 | 0.98 | 0.88, 1.08 | 0.643 | |
|
| |||||||||
| Maximum Cigarettes Per Day (z)e | Yes; Female>Male | All Twins N=3457 |
Dizygotic Pairs N=609 (318 female; 291 male) |
Monozygotic Pairs N=1085 (568 female; 517 male) |
|||||
|
| |||||||||
| β | 95% CI | β | 95% CI | p | β | 95% CI | p | ||
|
|
|||||||||
| Female | Female | Female | Female | Female | Female | Female | Female | ||
| .21 | .16, .25 | .20 | .11, .29 | <0.0001 | .13 | .04, .21 | 0.003 | ||
| Male | Male | Male | Male | Male | Male | Male | Male | ||
| .10 | .06, .14 | −.03 | −.12, .06 | 0.547 | −.03 | −.11, .05 | 0.432 | ||
|
| |||||||||
| Symptoms of Nicotine Dependence(z)e | Yes; Female>Male | All Twins N=3478 |
Dizygotic Pairs N=617 (321 female;296 male) |
Monozygotic Pairs N=1092 (570 female;522 male) |
|||||
|
| |||||||||
| β | 95% CI | β | 95% CI | p | β | 95% CI | p | ||
|
|
|||||||||
| Female | Female | Female | Female | Female | Female | Female | Female | ||
| .20 | .15, .24 | .22 | .12, .31 | <0.0001 DZ>MZf |
.06 | −.03, .16 | 0.175 | ||
| Male | Male | Male | Male | Male | Male | Male | Male | ||
| .11 | .06, .15 | −.06 | −.14, .04 | 0.205 | .02 | −.08, .11 | 0.738 | ||
Individual-level analyses include all adolescents; twin difference analyses include pairs in which both twins have data. Significant effects are in bold. Because all individual-level effects of ADHD were significant (all ps <.0001), specific significance levels are given only for within-pair effects.
Gender moderation test statistics and significance levels are given in the text.
Individual-level estimates were covariate-adjusted for age at assessment (except for initiation), cohort, parental SES, and gender (except when presented separately by gender). Within-pair estimates are not affected by adjusting for shared covariates.
Effects for initiation are given as hazard ratios; effects for progression to daily smoking are given as odds ratios. Those significantly greater than 1.0 correspond to the increased likelihood of initiating at each age (ages 8–18) or progressing a level toward daily smoking (e.g., from 1 to 2), respectively, associated with a 1 symptom increase in ADHD. Within-pair estimates reflect differential likelihood of initiating or progressing in frequency associated with a twin having 1 more ADHD symptom than his or her cotwin.
Effects for CPD and nicotine dependence are given as standardized beta coefficients (β), because ADHD symptoms, CPD, and log-transformed nicotine dependence symptoms were all converted to standardized (z) scores, with a mean of 0 and SD of 1. Individual-level estimates thereby reflect the increase in CPD or symptoms (in SD units) associated with a 1 SD increase in ADHD; within-pair estimates reflect the difference (in SD units) associated with a twin being 1 SD higher in ADHD than his or her cotwin.
DZ>MZ indicates that the within-pair effect was significantly greater for DZs than MZs (p<.05).
Adolescents with more inattentive or hyperactive-impulsive symptoms were more likely to initiate smoking (and earlier), without significant gender moderation. HRs associated with individual- level effects on initiation were 1.16 and 1.24, indicating rate of initiation increased 16% for each inattentive and 24% for each hyperactivity-impulsivity symptom. However, for female relative to male adolescents, ADHD was associated with faster progression to daily smoking (i.e., Inattention X Gender: z statistic = 2.01, p <.05; Hyperactivity-impulsivity X Gender: z = 3.19, p<.002), higher CPD [Inattention X Gender: F (1, 1689) = 12.09, p <.001; Hyperactivity-impulsivity X Gender: F = 11.00, p <.001] and more nicotine dependence symptoms [Inattention X Gender: F (1, 1704) = 7.04, p <.02; Hyperactivity- impulsivity X Gender: F = 5.78; p <.02]. For instance, a 27% increase in the odds of progressing one level toward daily smoking was observed for each inattentive symptom in female adolescents (19% for males) or 45% for each hyperactive-impulsive symptom (24% for males).
Twin difference effects are presented separately within DZ and MZ pairs in Table 2 to identify the source of observed differences, as their combined estimates were always significant for female adolescents (Table ST1). For both genders, MZ and DZ within-pair differences in inattention were significantly associated with initiation, consistent with partial causal influence. Rate of initiation increased 8% with each additional inattentive symptom a MZ twin had compared to his/her co-twin. However, all MZ- and DZ-within-pair estimates for inattention were significantly associated with daily smoking, CPD, and nicotine dependence for female pairs only (except one for female DZs, at p=.06), with no significant within-pair estimates for males, consistent with causal influence for female adolescents and full confounding by indirect genetic and environmental influences for males. By contrast, for hyperactivity-impulsivity, no MZ-within-pair estimates were significant (except for CPD in females), whereas all were significant for DZs (for initiation) or female DZs (for other outcomes). That the female DZ-within-pair estimate for hyperactivity-impulsivity was significantly greater than the MZ for nicotine dependence (DZ>MZ; Table 2) implies genetic differences primarily accounted for female adolescents’ increased smoking risk from hyperactivity-impulsivity.
Because potentially causal effects of inattention might be mediated by CD, ODD, or treatment with stimulant medications, individual-level analyses of inattention predicting all four smoking outcomes were repeated, adding either (1) log-transformed CD/ODD symptoms at baseline or (2) ever used prescription stimulants (yes/no) as a covariate. Although CD/ODD effects on smoking partially overlapped those of inattention, they did not affect significant gender moderation effects, nor did stimulants. Whether the possible causal association of attentional differences on smoking in females was due instead to greater likelihood of CD/ODD (or stimulants) in the more inattentive twin was also evaluated (see Appendix SA1). All significant MZ-within-pair effects remained, however, except for progression to daily smoking (e.g., OR declined from 1.19 to 1.17; p=.08, when CD/ODD were added).
Figure 1 illustrates an example of this consistent pattern for inattention, with nicotine dependence as the outcome. Adjusting for CD/ODD lowered the magnitude of the overall effect attributable to inattention so it remained significant for female adolescents only; significant female MZ- within-pair differences in inattention were minimally affected. Figure 2 demonstrates the practical significance of twin discordance in ADHD on maximum amount smoked (CPD), the only outcome with significant MZ-within-pair differences for both symptom subtypes. As may be seen, with shared genes and environment completely controlled, a potentially causal influence of moderate-to-large effect was evident for female pairs only.
Figure 1. Overall and Within Pair Difference Effects of Inattentive Symptoms on DSM-IV Nicotine Dependence Symptoms By Gendera, Before and After Adjusting for Conduct and Oppositional Defiant Disorder (CD/ODD).
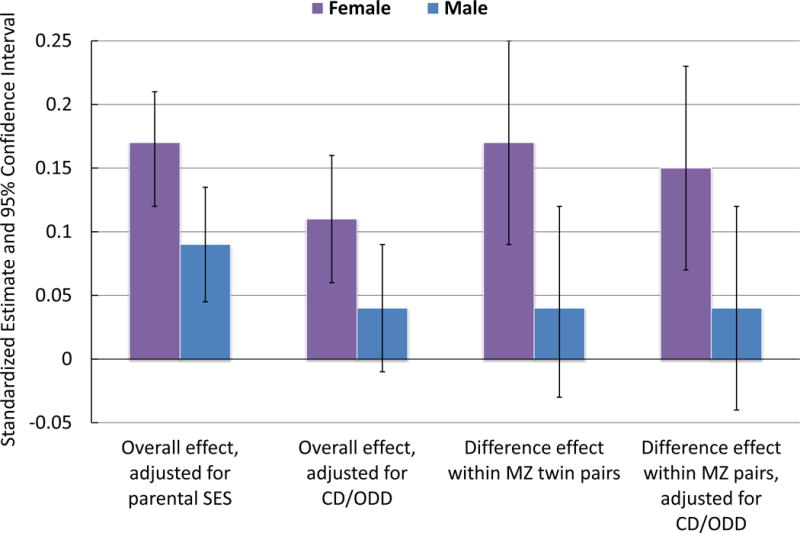
aOverall effect included N-3457 individuals; difference effect within monozygotic (MZ) pairs included N-568 female; 517 male pairs.
Figure 2. Monozygotic (MZ) Twin Discordance in Maximum Amount Smoked Per Day by Age 17 As a Function of Discordance in ADHD and Gender.
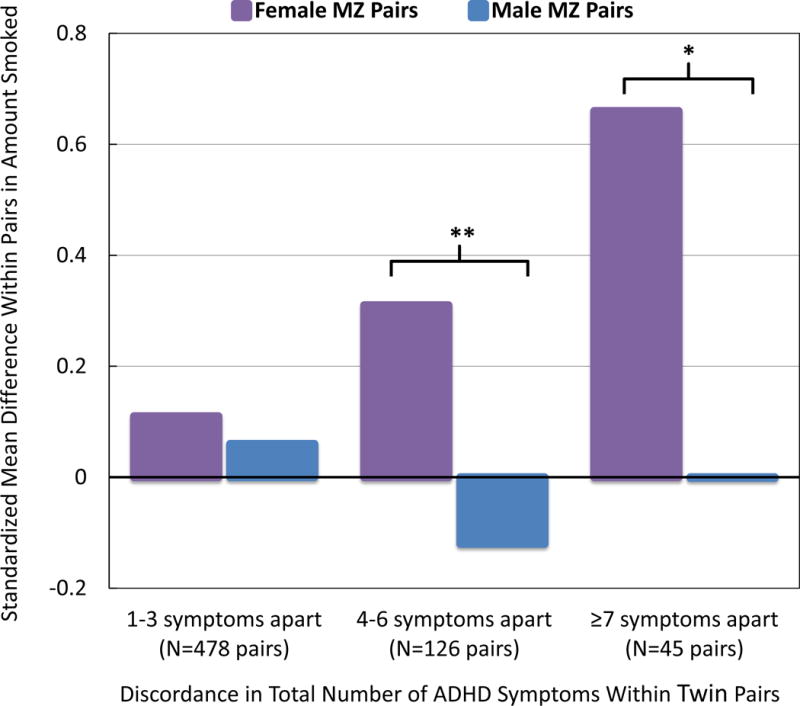
Note: MZ female twins with more ADHD symptoms than their co-twins escalated in amount smoked relative to the co-twin by age 17, reaching ~.7 SD apart in the most discordant pairs. For instance, more affected female twins smoked roughly 1/2 pack of cigarettes per day more than co-twins with 7 fewer symptoms. This effect was not evident in males. Differences between male and female MZ pairs were significant for pairs discordant by 4–6 (t = −2.79, df = 124) and ≥7 symptoms (t = −2.03, df = 43). *p < 0.05; **p < 0.01
DISCUSSION
In a combined analysis of three population-based cohorts with a significant number of females affected by ADHD, whether the association of childhood ADHD with smoking is consistent with a possible causal influence was evaluated using a twin difference design. To our knowledge, this is the first twin difference study to address effects of inattention and hyperactivity-impulsivity on progression of smoking during adolescence. Consistent with previous research [5, 6], adolescents with more ADHD symptoms were more prone to initiate smoking early and to progress to heavier, frequent smoking and nicotine dependence by age 17. However, ADHD was reliably associated with a higher level of these smoking risks for female than for male adolescents.
Our findings were also consistent with a causal influence of inattention on smoking initiation in both genders, or on increased smoking involvement in female adolescents only. Attentional differences within MZ female pairs were significantly related to differential progression to daily smoking, CPD, and nicotine dependence. While effect sizes corresponding to each symptom were modest, these effects became consequential for smoking among more discordant pairs (Figure 2; see SF2 for another example) and were unaffected by co-occurring externalizing disorders (Figure 1) or stimulant medication. Conversely, for male adolescents, within-pair differences were absent, suggesting familial factors (e.g., lower SES or parental smoking) play a greater role than inattention specifically. Hyperactivity-impulsivity effects in both genders were almost fully confounded by influences common to hyperactivity-impulsivity and smoking, with the exception of CPD. Thus, consistent with our hypotheses, both causal and non-causal mechanisms may be important in explaining the increased vulnerability of females with ADHD to smoking.
Mechanisms of Gender Moderation
Support for causality bolsters the plausibility that nicotine may be used to self-medicate inattention[13], consistent with findings of a placebo-controlled study that smokers with ADHD experience nicotine-related reductions in symptoms[29]. Furthermore, while nicotine withdrawal is generally associated with negative affect, smokers with ADHD report more severe withdrawal [30] and concentration difficulties [6] than those without ADHD. Although prescription stimulants for ADHD have been associated with reduced smoking [31], in the current study, they were associated with neither increased nor decreased smoking or nicotine dependence (similar to [32]) and did not ameliorate attentional effects for females.
Even if inattention is causal, there are likely to be mediators of its effects on smoking in female adolescents. The increased vulnerability of females to peer and academic consequences of inattention [21] might contribute to greater depression and anxiety among inattentive females relative to inattentive males [33], increasing their receptivity to nicotine’s effects on attention and mood. Gender differences in the interaction of ovarian hormones with nicotine and dopaminergic reward-processing systems [34] might further increase the susceptibility of female adolescents to self-medicate.
Shared propensities primarily explain the relationship of hyperactivity-impulsivity to smoking for both genders. Even when familial resemblance is genetic, adverse environments among those with ADHD may be increased through gene-environment interplay[35]. For example, adolescents with externalizing propensities are prone to selecting deviant peers, and increased exposure to such peers is associated with subsequent nicotine dependence[36]. That the hyperactivity/impulsivity-smoking relationship might be stronger for female than male adolescents was unexpected, yet consistent with evidence that greater risk accumulation may be required for females to develop ADHD[37].
Could Smoking Cause Inattention Instead?
Apparently causal effects in a twin difference design are sometimes due to “reverse causation”[18]. Thus, smoking might also cause inattention. In the Netherlands Twin Registry (NTR)[38], MZ twins who smoked showed a larger subsequent increase in attention problems from adolescence to adulthood compared to non-smoking co-twins. We examined whether reverse causation represents a plausible alternative interpretation of our results by re-running inattention models using only data from the two prospectively-assessed cohorts with ADHD measured at age 11. Although the MZ-within-pair effect became marginally significant for initiation (p = .05), attentional differences within MZ pairs were still significantly related to CPD, daily smoking, and dependence for females by age 17, suggesting reverse causation does not account for the results. Discrepancies between our findings and those from adults in the NTR may be due to etiological differences between childhood and adult ADHD. Childhood inattention might contribute to increased smoking; however, considering the deleterious cognitive effects of adolescent nicotine exposure [3], nicotine might contribute to increased inattention later on.
Strengths, Limitations, and Implications
Childhood ADHD appears relatively early in development, and non-shared experiences predating it appeared unlikely alternatives to a causal role of inattention for smoking. However, because observational data were used, causality cannot be conclusively proven, and it is possible that an unmeasured, non-shared experience leading to attentional differences in females might partially account for this association[18] (e.g., early maltreatment of one twin). Conversely, because MZ-within- pair estimates are disproportionately reduced by compounding of measurement error, the MZ-within- pair association of hyperactivity-impulsivity to CPD suggests there may be partially causal effects of hyperactivity-impulsivity for female adolescents that we did not have the power to detect. Additionally, although e-cigarettes were not in common use when these data were collected, e-cigarette users are more likely to initiate smoking of conventional cigarettes[3], and both are nicotine-based. Finally, while our sample was representative of Minnesota, replication among a more diverse sample is needed. The study has many strengths as well. The cohort sequential design ensures results are not specific to adolescents from one era, and assessment of multiple smoking outcomes with structured interviews and computer measures increases reliability and provides internal replication.
This study confirms that specific relationships between inattention and smoking observed in previous research may arise partially from causal effects, which has implications for intervention[16]. Diminishing inattention should reduce initiation and progression to heavy smoking, particularly for females. Preventing nicotine exposure among females with ADHD is critical, as adolescent females may be more susceptible to nicotine’s neurotoxic effects[39]. Focusing on coping with inattention and its associated impairments is consistent with findings that psychosocial therapies may produce greater reductions in ADHD-related impairment than medication[40].
Supplementary Material
Acknowledgments
Financial Support: This work was supported by National Institute on Drug Abuse grants R01DA038065 to Irene Elkins, R37DA005147 and R01DA013240 to William Iacono; and National Institute on Alcohol Abuse and Alcoholism grant R01AA009367 to Matt McGue. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest: The authors report no financial relationships with commercial interests.
References
- 1.Johnston ID, et al. Monitoring the Future national survey results on drug use, 1975–2015: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan; 2016. [Google Scholar]
- 2.Kann L, et al. Youth Risk Behavior Surveillance – United States, 2015. 6. Vol. 65. Centers for Disease Control and Prevention, MMWR Surveill Summ; 2016. [DOI] [PubMed] [Google Scholar]
- 3.A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2016. E-Cigarette Use Among Youth and Young Adults. [Google Scholar]
- 4.Nigg JT. Attention-deficit/hyperactivity disorder and adverse health outcomes. Clin Psychol Rev. 2013;33(2):215–28. doi: 10.1016/j.cpr.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Molina BS, Pelham WE., Jr Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. J Abnorm Psychol. 2003;112(3):497–507. doi: 10.1037/0021-843x.112.3.497. [DOI] [PubMed] [Google Scholar]
- 6.Rhodes JD, et al. Cigarette smoking and ADHD: An examination of prognostically relevant smoking behaviors among adolescents and young adults. Psychology of Addictive Behaviors. 2016;30(5):588–600. doi: 10.1037/adb0000188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belsky DW, et al. Polygenic risk and the developmental progression to heavy, persistent smoking and nicotine dependence: evidence from a 4-decade longitudinal study. JAMA Psychiatry. 2013;70(5):534–42. doi: 10.1001/jamapsychiatry.2013.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Biederman J, et al. Adult psychiatric outcomes of girls with attention deficit hyperactivity disorder: 11-year follow-up in a longitudinal case-control study. Am J Psychiatry. 2010;167(4):409–17. doi: 10.1176/appi.ajp.2009.09050736. [DOI] [PubMed] [Google Scholar]
- 9.Babinski DE, et al. Late adolescent and young adult outcomes of girls diagnosed with ADHD in childhood: an exploratory investigation. J Atten Disord. 2011;15(3):204–14. doi: 10.1177/1087054710361586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hinshaw SP, et al. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into adolescence: Evidence for continuing cross-domain impairment. J Consult Clin Psychol. 2006;74(3):489–99. doi: 10.1037/0022-006X.74.3.489. [DOI] [PubMed] [Google Scholar]
- 11.Lee SS, et al. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clin Psychol Rev. 2011;31(3):328–41. doi: 10.1016/j.cpr.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Derks EM, Hudziak JJ, Boomsma DI. Why more boys than girls with ADHD receive treatment: a study of Dutch twins. Twin Res Hum Genet. 2007;10(5):765–70. doi: 10.1375/twin.10.5.765. [DOI] [PubMed] [Google Scholar]
- 13.Looby A. Childhood attention deficit hyperactivity disorder and the development of substance use disorders: valid concern or exaggeration? Addict Behav. 2008;33(3):451–63. doi: 10.1016/j.addbeh.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 14.Elkins IJ, McGue M, Iacono WG. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Arch Gen Psychiatry. 2007;64(10):1145–52. doi: 10.1001/archpsyc.64.10.1145. [DOI] [PubMed] [Google Scholar]
- 15.Galera C, et al. Childhood hyperactivity-inattention symptoms and smoking in adolescence. Drug Alcohol Depend. 2005;78(1):101–8. doi: 10.1016/j.drugalcdep.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Pingault JB, et al. Childhood trajectories of inattention, hyperactivity and oppositional behaviors and prediction of substance abuse/dependence: a 15-year longitudinal population-based study. Mol Psychiatry. 2013;18(7):806–12. doi: 10.1038/mp.2012.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sundquist J, et al. Attention-deficit/hyperactivity disorder and risk for drug use disorder: a population-based follow-up and co-relative study. Psychol Med. 2015;45(5):977–83. doi: 10.1017/S0033291714001986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McGue M, Osler M, Christensen K. Causal inference and observational research: The utility of twins. Perspectives on Psychological Science. 2010;5(5):546–556. doi: 10.1177/1745691610383511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.D’Onofrio BM, et al. Critical need for family-based, quasi-experimental designs in integrating genetic and social science research. Am J Public Health. 2013;103(Suppl 1):S46–55. doi: 10.2105/AJPH.2013.301252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frisell T, et al. Sibling Comparison Designs Bias From Non-Shared Confounders and Measurement Error. Epidemiology. 2012;23(5):713–720. doi: 10.1097/EDE.0b013e31825fa230. [DOI] [PubMed] [Google Scholar]
- 21.Elkins IJ, et al. The impact of attention-deficit/hyperactivity disorder on preadolescent adjustment may be greater for girls than for boys. J Clin Child Adolesc Psychol. 2011;40(4):532–45. doi: 10.1080/15374416.2011.581621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keyes MA, et al. The enrichment study of the Minnesota twin family study: increasing the yield of twin families at high risk for externalizing psychopathology. Twin Res Hum Genet. 2009;12(5):489–501. doi: 10.1375/twin.12.5.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iacono WG, McGue M. Minnesota Twin Family Study. Twin Res. 2002;5(5):482–7. doi: 10.1375/136905202320906327. [DOI] [PubMed] [Google Scholar]
- 24.Reich W. Diagnostic interview for children and adolescents (DICA) Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:59–66. doi: 10.1097/00004583-200001000-00017. [DOI] [PubMed] [Google Scholar]
- 25.Robins LN, et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of General Psychiatry. 1988;45(12):1069–77. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- 26.Merwood A, et al. Different heritabilities but shared etiological influences for parent, teacher and self-ratings of ADHD symptoms: an adolescent twin study. Psychol Med. 2013;43(9):1973–84. doi: 10.1017/S0033291712002978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sjolander A, et al. Between-within models for survival analysis. Stat Med. 2013;32(18):3067–76. doi: 10.1002/sim.5767. [DOI] [PubMed] [Google Scholar]
- 28.Carlin JB, et al. Regression models for twin studies: a critical review. Int J Epidemiol. 2005;34(5):1089–99. doi: 10.1093/ije/dyi153. [DOI] [PubMed] [Google Scholar]
- 29.Gehricke JG, et al. The reinforcing effects of nicotine and stimulant medication in the everyday lives of adult smokers with ADHD: A preliminary examination. Nicotine Tob Res. 2006;8(1):37–47. doi: 10.1080/14622200500431619. [DOI] [PubMed] [Google Scholar]
- 30.Kollins SH, et al. Effects of smoking abstinence on smoking-reinforced responding, withdrawal, and cognition in adults with and without attention deficit hyperactivity disorder. Psychopharmacology (Berl) 2013;227(1):19–30. doi: 10.1007/s00213-012-2937-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schoenfelder EN, Faraone SV, Kollins SH. Stimulant treatment of ADHD and cigarette smoking: a meta-analysis. Pediatrics. 2014;133(6):1070–80. doi: 10.1542/peds.2014-0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Humphreys KL, Eng T, Lee SS. Stimulant medication and substance use outcomes: a meta-analysis. JAMA Psychiatry. 2013;70(7):740–9. doi: 10.1001/jamapsychiatry.2013.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Becker SP, et al. Negative social preference in relation to internalizing symptoms among children with ADHD predominantly inattentive type: girls fare worse than boys. J Clin Child Adolesc Psychol. 2013;42(6):784–95. doi: 10.1080/15374416.2013.828298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pauly JR. Gender differences in tobacco smoking dynamics and the neuropharmacological actions of nicotine. Front Biosci. 2008;13:505–16. doi: 10.2741/2696. [DOI] [PubMed] [Google Scholar]
- 35.Thapar A, et al. What have we learnt about the causes of ADHD? J Child Psychol Psychiatry. 2013;54(1):3–6. doi: 10.1111/j.1469-7610.2012.02611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Samek DR, et al. Antisocial peer affiliation and externalizing disorders in the transition from adolescence to young adulthood: Selection versus socialization effects. Dev Psychol. 2016;52(5):813–23. doi: 10.1037/dev0000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Taylor MJ, et al. Is There a Female Protective Effect Against Attention-Deficit/Hyperactivity Disorder? Evidence From Two Representative Twin Samples. J Am Acad Child Adolesc Psychiatry. 2016;55(6):504–512 e2. doi: 10.1016/j.jaac.2016.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Treur JL, et al. Smoking During Adolescence as a Risk Factor for Attention Problems. Biol Psychiatry. 2015;78(9):656–63. doi: 10.1016/j.biopsych.2014.06.019. [DOI] [PubMed] [Google Scholar]
- 39.Abreu-Villaca Y, et al. Nicotine is a neurotoxin in the adolescent brain: critical periods, patterns of exposure, regional selectivity, and dose thresholds for macromolecular alterations. Brain Res. 2003;979(1–2):114–28. doi: 10.1016/s0006-8993(03)02885-3. [DOI] [PubMed] [Google Scholar]
- 40.Sibley MH, et al. Pharmacological and psychosocial treatments for adolescents with ADHD: an updated systematic review of the literature. Clin Psychol Rev. 2014;34(3):218–32. doi: 10.1016/j.cpr.2014.02.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


