Abstract
Objective
To examine the impact of health literacy on hospitalizations and death in a population of patients with heart failure (HF).
Patients and Methods
Residents from the 11-county region in southeast Minnesota with a first-ever International Classification of Diseases, Ninth Revision code 428 or Tenth Revision code 150 (n=5121) from January 1, 2013, through December 31, 2015, were identified and prospectively surveyed to measure health literacy using established screening questions. A total of 2647 patients returned the survey (response rate, 52%); 2487 patients with complete health literacy data were retained for analysis. Health literacy, measured as a composite score on three 5-point scales, was categorized as adequate (≥8) or low (<8). Cox proportional hazards regression and Andersen-Gill models were used to examine the association of health literacy with mortality and hospitalization.
Results
Of 2487 patients (mean age, 73.5 years; 53.6% male [n=1333]), 10.5% (n= 261) had low health literacy. After mean ± SD follow-up of 15.5±7.2 months, 250 deaths and 1584 hospitalizations occurred. Low health literacy was associated with increased mortality and hospitalizations. After adjusting for age, sex, comorbidity, education, and marital status, the hazard ratios for death and hospitalizations in patients with low health literacy were 1.91 (95% CI, 1.38–2.65; P<.001) and 1.30 (95% CI, 1.02–1.66; P=.03), respectively, compared with patients with adequate health literacy.
Conclusion
Low health literacy is associated with increased risks of hospitalization and death in patients with HF. The clinical evaluation of health literacy could help design interventions individualized for patients with low health literacy.
Heart failure (HF) is a public health burden.1,2 In the United States, there are an estimated 5.7 million people living with HF, with total annual medical costs of $31 billion.1,3,4 These numbers are expected to grow to more than 8 million people and $70 billion in cost by 2030.4 Although diagnosis and treatment have improved, mortality has not changed,2–5 and hospitalizations are still common, most often due to comorbidities.6–9 Because the management of HF is complex and requires multiple skills, to prevent poor outcomes, it is crucial for patients to be engaged in good self-care.10,11
Health literacy is described by the Institute of Medicine as “the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions.”12 Patients with limited health literacy have insufficient drug adherence and inadequate self-care behavior.13,14 Thus, these patients may use more health care services such as hospital or emergency department visits15 and, as a consequence, incur higher medical costs.16 In HF, associations between poor health literacy and mortality,17,18 hospitalization,19,20 and recurrence of HF21 have been reported. However, these results were generated in smaller convenience samples, chiefly of hospitalized patients, relying on composite end points (death and hospitalizations combined). Hence, to our knowledge, health literacy remains to be studied in a large population-based community, a design essential to comprehensively capture outcomes and afford separate analyses for death and hospitalizations, which have vastly different clinical implications.
To address this gap in knowledge, we investigated the association between health literacy and death and hospitalizations in a large population-based study of patients with HF in southeast Minnesota.
METHODS
Study Setting and Design
This study was conducted in 11 counties in southeast Minnesota: Dodge, Fillmore, Free-born, Goodhue, Houston, Mower, Olmsted, Rice, Steele, Wabasha, and Winona (approximate population of 491,684 according to the 2010 US Census), incorporating data from Mayo Clinic, Mayo Clinic Health System, and Olmsted Medical Center and their affiliated clinics. This study used the medical records linkage system of the Rochester Epidemiology Project (REP), which allows retrieval of health care utilization and outcomes of the residents in this region.22–24 The study was approved by the Mayo Clinic and Olmsted Medical Center institutional review boards.
Case Identification
Using the resources of the REP, residents 18 years or older from the 11-county area in southeast Minnesota with a first-ever International Classification of Diseases, Ninth Revision code 428 or Tenth Revision code I50 for HF from January 1, 2013, through December 31, 2015, were identified. These patients were asked to complete a survey to measure health literacy and other sociobehavioral measures. A mixed-mode design was used to improve the response rate. Patients were mailed a survey packet containing the survey, an introductory letter, and a Health Insurance Portability and Accountability Act of 1996 form. Patients who did not want to complete the survey through the mail were given the opportunity to complete the survey over the telephone by requesting a telephone call. The survey packet was resent to nonresponders approximately 1 month after the first mailing. A telephone interview was attempted approximately 1 month after the second mailing for the remaining nonresponders.
Health Literacy
Health literacy was measured using 3 established screening questions: (1) How confident are you filling out forms by yourself? (2) How often do you have someone (such as a family member, friend, hospital/clinic worker, or caregiver) help you read hospital materials? (3) How often do you have problems learning about your medical condition because of difficulty reading hospital materials?25,26 Each question is scored on a 5-point scale. The sum of the 3 question scores can range from 3 to 15 points, with a lower score indicating lower health literacy. These 3 questions have been validated against longer and more comprehensive measures of health literacy.26–28 The Cronbach α, a measure of internal consistency reliability, for the 3 questions was 0.80 in this study, which supports scoring and reporting them as a single measure. Patients were categorized as having low health literacy if they scored less than 8 and adequate health literacy if they scored 8 or greater.
Other Patient Characteristics
Educational level and marital status were obtained from the patient survey. The comorbidities included in the Charlson Comorbidity Index were retrieved using the electronic REP record linkage system, and the score was calculated for each participant.29,30
Outcomes
Participants were followed for death and hospitalization from enrollment through December 31, 2016 (range of follow up, 9–21 months). Death information was retrieved from the REP, which obtains death certificate data from Minnesota. Hospitalizations were collected through the REP, which, as described previously herein, collects information for nearly all hospitalizations for residents in the 11 counties included in this study. In-hospital transfers were counted as a single event.
Statistical Analyses
Participant characteristics, overall and by health literacy category, are presented as frequencies or mean ± SD. Differences between individuals with low vs adequate health literacy were compared using 2-sample t tests for continuous variables and χ2 tests for categorical variables. Mortality was assessed using the Kaplan-Meier method according to health literacy categories and compared with the log-rank test. Cox proportional hazards regression was used to estimate the associations of health literacy with death in unadjusted, age- and sex-adjusted, and fully adjusted models that also included the Charlson Comorbidity Index, education, and marital status.
The cumulative mean numbers of hospitalizations during follow-up by health literacy category were plotted using a nonparametric estimator described by Nelson.31 Andersen-Gill modeling, which allows for modeling of multiple outcome events, was used to examine associations between health literacy categories and hospitalizations in unadjusted, age- and sex-adjusted, and fully adjusted models that also included the Charlson Comorbidity Index, education, and marital status. In ancillary analyses, health literacy was categorized into tertiles to examine a dose-response relationship between health literacy and outcomes.
The proportional hazards assumption was tested using scaled Schoenfeld residuals and found to be valid. A P<.05 was used as the level of statistical significance. Statistical analyses were performed using SAS software, version 9.4 (SAS Institute Inc).
RESULTS
Of 5866 patients identified with HF and sent a survey, 256 died without completing the survey, 23 were lost to follow-up, 405 were physically or mentally unable to complete the survey, and 61 had a language barrier. Of the remaining 5121 patients, 2647 returned the survey (response rate 52%). Patients who returned a survey were similar regarding sex to patients who did not return a survey (P=.98). Responders were slightly older than nonresponders (mean age, 72.5 vs 71.3 years; P=.002) and had a slightly higher Charlson Comorbidity Index (mean index, 2.02 vs 1.88; P=.03). Patients who completed the health literacy screener were retained for the analysis (n=2487; mean age, 73.5 years; 53.6% male [n=1333]). The median time from HF diagnosis to completion of the survey was 365 days (25th–75th percentile, 298–470 days). Approximately 10.5% of patients (n=261) had low health literacy (range among the 11 counties, 6.9%–17.1%). These patients were, on average, older, less likely to be married, and had lower educational attainment than those with adequate health literacy (Table 1). Patients with low health literacy had a higher Charlson Comorbidity Index and specifically had a higher proportion of peripheral vascular and cerebrovascular disease, renal disease, and diabetes. Moreover, patients with inadequate health literacy were more likely to complete the survey via telephone.
TABLE 1.
Baseline Characteristics
| Characteristic | Total cohort (N=2487) | Adequate health literacy (n=2226) | Low health literacy (n= 261) | P value |
|---|---|---|---|---|
| Age (y), mean ± SD | 73.5 (12.5) | 73.3±12.3 | 75.0±14.6 | .04 |
|
| ||||
| Male sex (No. [%]) | 1333 (53.6) | 1193 (53.6) | 140 (53.6) | .99 |
|
| ||||
| Education (No. [%])a | <.001 | |||
| Non–high school graduate | 289 (11.8) | 210 (9.6) | 79 (30.3) | |
| High school graduate | 872 (35.5) | 757 (34.5) | 115 (44.1) | |
| Some college/college degree | 1017 (41.4) | 957 (43.6) | 60 (23.0) | |
| Graduate school | 277 (11.3) | 270 (12.3) | 7 (2.7) | |
|
| ||||
| Married (No. [%])b | 1455 (58.9) | 1333 (60.4) | 122 (46.7) | <.001 |
|
| ||||
| Survey completed by mail (No. [%]) | 1549 (62.3) | 1435 (64.5) | 114 (43.7) | <.001 |
|
| ||||
| Charlson Comorbidity Index (No. [%]) | <.001 | |||
| 0 | 213 (8.6) | 201 (9.0) | 12 (4.6) | |
| 1–2 | 978 (39.3) | 894 (40.2) | 84 (32.2) | |
| ≥3 | 1296 (52.1) | 1131 (50.8) | 165 (63.2) | |
|
| ||||
| Myocardial infarction (No. [%]) | 406 (16.3) | 361 (16.2) | 45 (17.2) | .67 |
|
| ||||
| Peripheral vascular disease (No. [%]) | 896 (36.0) | 780 (35.0) | 116 (44.4) | .003 |
|
| ||||
| Cerebrovascular disease (No. [%]) | 357 (14.4) | 302 (13.6) | 55 (21.1) | .001 |
|
| ||||
| Chronic pulmonary disease (No. [%]) | 788 (31.7) | 694 (31.2) | 94 (36.0) | .11 |
|
| ||||
| Moderate/severe renal disease (No. [%]) | 580 (23.3) | 499 (22.4) | 81 (31.3) | .002 |
|
| ||||
| Diabetes (No. [%]) | 846 (34.0) | 723 (32.5) | 123 (47.1) | <.001 |
|
| ||||
| Cancer (No. [%]) | 399 (16.0) | 364 (16.4) | 35 (13.4) | .22 |
Education status missing for 32 patients.
Marital status missing for 19 patients.
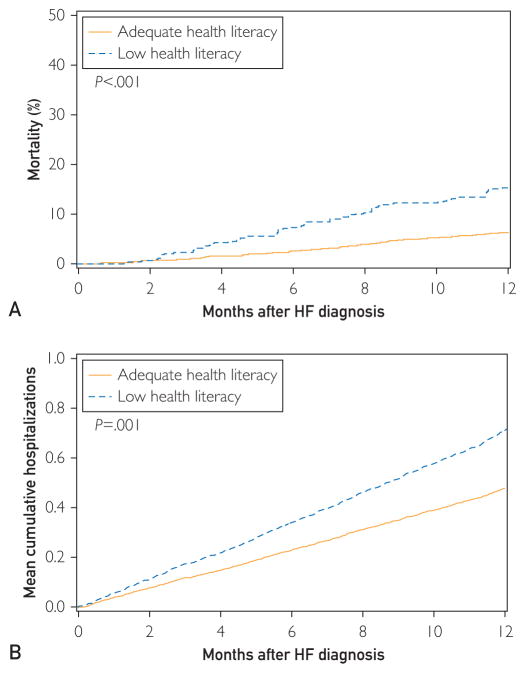
After mean ± SD follow-up of 15.5±7.2 months, 250 deaths occurred. Poor health literacy was associated with an increased risk of death (Figure A). Patients with low health literacy had more than a 2-fold increased risk of death compared with those with adequate literacy (hazard ratio [HR]=2.30; 95% CI, 1.69–3.15; P<.001) (Table 2). Adjustment for age, sex, education, marital status, and comorbidity slightly attenuated this association (HR=1.91; 95% CI, 1.38–2.65; P<.001). Further adjustment for mode of survey completion did not materially change the results.
FIGURE.
Mortality (A) and mean cumulative number of hospitalizations (B) after heart failure (HF) diagnosis by health literacy category.
TABLE 2.
Death and Hospitalizations for Low vs Adequate Health Literacy
| Factor | Hazard ratios (95% CIs) | P value | |
|---|---|---|---|
|
| |||
| Adequate health literacy (n=2226) | Low health literacy (n=261) | ||
| All-cause death (250 events) | |||
| Unadjusted model | 1.00 | 2.30 (1.69–3.15) | <.001 |
| Age and sex adjusted | 1.00 | 2.09 (1.53–2.87) | <.001 |
| Fully adjusteda | 1.00 | 1.91 (1.38–2.65) | <.001 |
|
| |||
| All-cause hospitalizations (1584 events) | |||
| Unadjusted model | 1.00 | 1.48 (1.17–1.88) | .001 |
| Age and sex adjusted | 1.00 | 1.48 (1.17–1.88) | .001 |
| Fully adjusteda | 1.00 | 1.30 (1.02–1.66) | .03 |
Adjusted for age, sex, education, marital status, and Charlson Comorbidity Index.
A total of 1584 hospitalizations occurred during follow-up. Poor health literacy was associated with a higher mean cumulative number of hospitalizations (Figure B). Patients with inadequate health literacy had almost a 50% increased risk of hospitalizations compared with those with adequate health literacy (HR=1.48; 95% CI, 1.17–1.86; P=.001) (Table 2). After adjustment for age, sex, education, marital status, and comorbidity, the association was attenuated but remained strong and significant (HR=1.30; 95% CI, 1.02–1.66; P=.03). Additional adjustment for mode of survey completion did not change the strength of the association.
In ancillary analyses, we categorized the health literacy score into tertiles: high, 14 to 15 points; intermediate, 11 to 13 points; and low, 10 points or less. Patients in the intermediate tertile did not have an increased risk of death (HR=1.09; 95% CI, 0.78–1.53) after adjustment for age, sex, education, marital status, and comorbidity compared with patients in the high tertile, whereas patients in the low tertile had a nearly 2-fold increased risk of death (HR=1.87; 95% CI, 1.34–2.62; Ptrend<.001). Furthermore, patients in the intermediate and low tertiles had a nearly 20% and 30% increased risk of hospitalization, respectively, compared with the high tertile after adjustment for age, sex, education, marital status, and comorbidity (intermediate tertile: HR=1.17; 95% CI, 0.96–1.43; and low tertile: HR=1.32; 95% CI, 1.05–1.65; Ptrend=.02).
DISCUSSION
In a large population-based cohort study, we found that patients with poor health literacy had nearly a 2-fold increased risk of mortality and a 30% increased risk of hospitalization compared with patients with adequate health literacy.
Measuring Health Literacy
We evaluated health literacy using an established 3-question brief screener.25,26 Compared with alternative methods used in previous studies for health literacy evaluation, such as the Short Test of Functional Health Literacy in Adults (S-TOFHLA),19,20 the brief screener is less time-consuming and easier to implement in clinical practice.17 Whereas the S-TOFHLA is an objective evaluation that requires an interviewer, the brief screener is a subjective measure that can be self-administered.
Health Literacy in HF
In the present cohort, the prevalence of low health literacy was 10.5% (n=261), which is lower than that in other studies using the same questionnaire,15,17,18 with reported prevalences of low health literacy of 17.5%17 to 33.7%15 in patients with HF. However, these studies pertained to hospitalized patients15,17,18 and, thus, are not directly comparable with the present community study whereby patients with HF were surveyed in the outpatient setting. Moreover, in the present study, the prevalence of low health literacy was quite heterogeneous among the different counties, ranging from 6.9% to 17.1%. Olmsted County, which has a high level of health literacy, is the county that contributes most of the patients with HF, thereby driving the average prevalence.
Herein, a low level of health literacy was associated with a large increase in the risk of death and hospitalizations independently of age, sex, education, marital status, and comorbidities, demonstrating that the 3-question brief screener has strong prognostic value. These results extend and augment previous reports that evaluated the association between poor health literacy and mortality, but the present finding is in contrast with previous reports in that they did not detect an association with hospitalizations.17,18 This is important because the present results highlight the impact that low health literacy has on 1 key indicator of health care utilization. The present data, in turn, underscore the need to assess health literacy in clinical practice and use the results to individualize interventions.
We chose to categorize literacy scores less than 8 as having low health literacy, which is mathematically equivalent to a cutoff score of 10 points in a reversed score,17 but, as shown by other authors,18 health literacy is not a dichotomous construct. By categorizing the scores into tertiles and examining the association with all-cause death and hospitalization, we identified a dose-response relationship between health literacy and risk of hospitalization, with the risk increasing as health literacy decreases. These findings are important because the dose-response relationship supports causality, and any suboptimal level of literacy will lead to an increase in adverse outcomes.
The mechanisms whereby low health literacy leads to poor outcomes are only partially understood and likely involve access and health care utilization, the interaction between provider and patient, and self-care.32 In particular, patients with adequate health literacy, which is associated with better knowledge of disease,33 are more likely to engage in more effective interaction with physicians. Furthermore, health literacy is influenced by socioeconomic and demographic factors and by education and mental abilities.32 All these factors could lead patients with limited health literacy to have worse self-care behavior,14,34 which is critical in the long-term management of HF. Self-care for HF is complex and requires not only a high level of medication adherence but also weight monitoring, a sodium-controlled diet, and regular exercise and, for many patients, weight loss. Moreover, inadequate medication adherence in patients with limited health literacy13 seems to play an important role in their higher risk of HF reoccurrence.21 Last, owing to the lower knowledge of their disease,35,36 they are less likely to recognize signs and symptoms of exacerbation,32 making hospitalization and death more likely.
Clinical Implications
The brief screener is a simple, efficient, and reliable tool to evaluate health literacy. This screener could be implemented in clinical practice to identify patients at higher risk for poor outcomes and to design interventions to support their individual informational and self-care needs. Because screening for low health literacy can be stigmatizing, it should be done only if effective interventions are readily available to address the needs of the vulnerable populations of patients identified through the screening.32 Some interventions focusing on patients with low health literacy can improve knowledge of HF, health behaviors,37 and outcomes.38–41 Indeed, developing or strengthening specific skills required for effective self-management, such as how to use diuretics and monitor body weight daily,42 may increase health literacy and improve outcomes. Screening for low health literacy can help to ensure that the resources required for successful interventions are dedicated to those most in need.
Limitations and Strengths
As in any survey study, we could have incurred nonresponder bias; specifically, those with lower health literacy could have been less likely to respond, although we demonstrated that responders differ slightly only in age and comorbidity index and are similar to non-responders regarding sex. Considering the high response rate (52%) and the nonresponder analysis, we believe that our cohort is representative of the HF population in southeast Minnesota. Finally, to achieve a higher response rate, we used a mixed mode (mail and telephone) to collect data on those who prefer to complete the survey by telephone. The present study was conducted in a population of mostly non-Hispanic white race/ethnicity with higher-than-average education. Thus, it needs replication in other populations. Finally, as in any observational study, we cannot rule out the effect of residual confounding due to unmeasured variables.
The present study has several distinct strengths. This is a population-based cohort study that used the REP.22–24 This allowed us to achieve a comprehensive ascertainment of comorbidities, death, and hospitalizations in a large area of southeastern Minnesota. Furthermore, we prospectively surveyed patients using a validated and reliable method to screen health literacy.26
CONCLUSION
In this population-based study of 11 counties in southeast Minnesota, we demonstrated that low health literacy is associated with higher mortality and hospitalization rates. Further studies should be conducted to evaluate how to address this risk factor and improve morbidity and mortality in patients with HF.
Acknowledgments
We thank Ellen Koepsell, RN, and Deborah Strain for their study support.
The funding sources played no role in the design, conduct, or reporting of this study. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Grant Support: This study was made possible by the Rochester Epidemiology Project (grant number R01-AG034676; Principal Investigators: Walter A. Rocca, MD, MPH, and Jennifer L. St Sauver, PhD). This work was supported by grants R01 HL120859 Principal Investigator: Véronique L. Roger, MD, MPH from the National Heart, Lung, and Blood Institute, and grant CDRN-1501-26638 Principal Investigator: Véronique L. Roger, MD, MPH from the Patient-Centered Outcomes Research Institute.
Abbreviations and Acronyms
- HF
heart failure
- HR
hazard ratio
- REP
Rochester Epidemiology Project
- S-TOFHLA
Short Test of Functional Health Literacy in Adults
Footnotes
Potential Competing Interests: Dr Boyd receives royalties for being a coauthor of a chapter on multimorbidity for Up-to-Date.
References
- 1.Roger VL. Epidemiology of heart failure. Circ Res. 2013;113(6):646–659. doi: 10.1161/CIRCRESAHA.113.300268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gerber Y, Weston SA, Redfield MM, et al. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern Med. 2015;175(6):996–1004. doi: 10.1001/jamainternmed.2015.0924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Writing Group Members. Mozaffarian D, Benjamin EJ, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 4.Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gerber Y, Weston SA, Enriquez-Sarano M, et al. Mortality associated with heart failure after myocardial infarction: a contemporary community perspective. Circ Heart Fail. 2016;9(1):e002460. doi: 10.1161/CIRCHEARTFAILURE.115.002460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunlay SM, Redfield MM, Weston SA, et al. Hospitalizations after heart failure diagnosis: a community perspective. J Am Coll Cardiol. 2009;54(18):1695–1702. doi: 10.1016/j.jacc.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Desai AS, Stevenson LW. Rehospitalization for heart failure: predict or prevent? Circulation. 2012;126(4):501–506. doi: 10.1161/CIRCULATIONAHA.112.125435. [DOI] [PubMed] [Google Scholar]
- 8.Hall MJ, Levant S, DeFrances CJ. Hospitalization for congestive heart failure: United States, 2000–2010. NCHS Data Brief. 2012;(108):1–8. [PubMed] [Google Scholar]
- 9.Manemann SM, Chamberlain AM, Boyd CM, et al. Skilled nursing facility use and hospitalizations in heart failure: a community linkage study. Mayo Clin Proc. 2017;92(4):490–499. doi: 10.1016/j.mayocp.2017.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riegel B, Moser DK, Anker SD, et al. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120(12):1141–1163. doi: 10.1161/CIRCULATIONAHA.109.192628. [DOI] [PubMed] [Google Scholar]
- 11.Arena R, Lavie CJ. Preventing bad and expensive things from happening by taking the healthy living polypill: everyone needs this medicine [published online March 13, 2017] Mayo Clin Proc. doi: 10.1016/j.mayocp.2017.02.005. https://doi.org/10.1016/j.mayocp.2017.02.005. [DOI] [PubMed]
- 12.Institute of Medicine (US) Committee on Health Literacy. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004. p. 4. [PubMed] [Google Scholar]
- 13.Noureldin M, Plake KS, Morrow DG, Tu W, Wu J, Murray MD. Effect of health literacy on drug adherence in patients with heart failure. Pharmacotherapy. 2012;32(9):819–826. doi: 10.1002/j.1875-9114.2012.01109.x. [DOI] [PubMed] [Google Scholar]
- 14.Macabasco-O’Connell A, DeWalt DA, Broucksou KA, et al. Relationship between literacy, knowledge, self-care behaviors, and heart failure-related quality of life among patients with heart failure. J Gen Intern Med. 2011;26(9):979–986. doi: 10.1007/s11606-011-1668-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cox SR, Liebl MG, McComb MN, et al. Association between health literacy and 30-day healthcare use after hospital discharge in the heart failure population. Res Social Adm Pharm. 2017;13(4):754–758. doi: 10.1016/j.sapharm.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 16.Howard DH, Gazmararian J, Parker RM. The impact of low health literacy on the medical costs of Medicare managed care enrollees. Am J Med. 2005;118(4):371–377. doi: 10.1016/j.amjmed.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 17.Peterson PN, Shetterly SM, Clarke CL, et al. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305(16):1695–1701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McNaughton CD, Cawthon C, Kripalani S, Liu D, Storrow AB, Roumie CL. Health literacy and mortality: a cohort study of patients hospitalized for acute heart failure. J Am Heart Assoc. 2015;4(5) doi: 10.1161/JAHA.115.001799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moser DK, Robinson S, Biddle MJ, et al. Health literacy predicts morbidity and mortality in rural patients with heart failure. J Card Fail. 2015;21(8):612–618. doi: 10.1016/j.cardfail.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu JR, Holmes GM, DeWalt DA, et al. Low literacy is associated with increased risk of hospitalization and death among individuals with heart failure. J Gen Intern Med. 2013;28(9):1174–1180. doi: 10.1007/s11606-013-2394-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McNaughton CD, Collins SP, Kripalani S, et al. Low numeracy is associated with increased odds of 30-day emergency department or hospital recidivism for patients with acute heart failure. Circ Heart Fail. 2013;6(1):40–46. doi: 10.1161/CIRCHEARTFAILURE.112.969477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ., III History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87(12):1202–1213. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, III, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(2):151–160. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.St Sauver JL, Grossardt BR, Yawn BP, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41(6):1614–1624. doi: 10.1093/ije/dys195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–594. [PubMed] [Google Scholar]
- 26.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23(5):561–566. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wallace LS, Rogers ES, Roskos SE, Holiday DB, Weiss BD. Screening items to identify patients with limited health literacy skills. J Gen Intern Med. 2006;21(8):874–877. doi: 10.1111/j.1525-1497.2006.00532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wallace LS, Cassada DC, Rogers ES, et al. Can screening items identify surgery patients at risk of limited health literacy? J Surg Res. 2007;140(2):208–213. doi: 10.1016/j.jss.2007.01.029. [DOI] [PubMed] [Google Scholar]
- 29.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 30.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 31.Nelson W. Recurrent Events, Data Analysis for Product Repairs, Disease Recurrences, and Other Applications. Philadelphia, PA: Society for Industrial and Applied Mathematics; 2003. ASA-SIAM Series on Statistics and Applied Probability. [Google Scholar]
- 32.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(suppl 1):S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 33.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease: a study of patients with hypertension and diabetes. Arch Intern Med. 1998;158(2):166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 34.Matsuoka S, Tsuchihashi-Makaya M, Kayane T, et al. Health literacy is independently associated with self-care behavior in patients with heart failure. Patient Educ Couns. 2016;99(6):1026–1032. doi: 10.1016/j.pec.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 35.Hawkins MA, Dolansky MA, Levin JB, et al. Cognitive function and health literacy are independently associated with heart failure knowledge. Heart Lung. 2016;45(5):386–391. doi: 10.1016/j.hrtlng.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen AM, Yehle KS, Albert NM, et al. Relationships between health literacy and heart failure knowledge, self-efficacy, and self-care adherence. Res Social Adm Pharm. 2014;10(2):378–386. doi: 10.1016/j.sapharm.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baker DW, Dewalt DA, Schillinger D, et al. The effect of progressive, reinforcing telephone education and counseling versus brief educational intervention on knowledge, self-care behaviors and heart failure symptoms. J Card Fail. 2011;17(10):789–796. doi: 10.1016/j.cardfail.2011.06.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.DeWalt DA, Malone RM, Bryant ME, et al. A heart failure self-management program for patients of all literacy levels: a randomized, controlled trial [ISRCTN11535170] BMC Health Serv Res. 2006;6:30. doi: 10.1186/1472-6963-6-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.DeWalt DA, Schillinger D, Ruo B, et al. Multisite randomized trial of a single-session versus multisession literacy-sensitive self-care intervention for patients with heart failure. Circulation. 2012;125(23):2854–2862. doi: 10.1161/CIRCULATIONAHA.111.081745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Di Palo KE, Patel K, Assafin M, Pina IL. Implementation of a patient navigator program to reduce 30-day heart failure readmission rate. Prog Cardiovasc Dis. 2017;60(2):259–266. doi: 10.1016/j.pcad.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 41.Ziaeian B, Fonarow GC. The prevention of hospital readmissions in heart failure. Prog Cardiovasc Dis. 2016;58(4):379–385. doi: 10.1016/j.pcad.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baker DW, DeWalt DA, Schillinger D, et al. “Teach to goal”: theory and design principles of an intervention to improve heart failure self-management skills of patients with low health literacy. J Health Commun. 2011;16(suppl):373–388. doi: 10.1080/10810730.2011.604379. [DOI] [PMC free article] [PubMed] [Google Scholar]