Abstract
Objective
Sexual abuse experienced in childhood and adolescence is associated with severity of posttraumatic stress disorder (PTSD), depressive symptoms, and emotion regulation difficulties. The current study examined the relationships among these factors in a sample of adolescents with sexual abuse-related PTSD. It was hypothesized that: 1) self-perceived emotion regulation difficulties would predict severity of PTSD and depressive symptoms, and that 2) depressive symptoms would mediate the relationship between emotion regulation difficulties and PTSD.
Method
Ninety treatment-seeking female adolescents with a history of sexual abuse were evaluated using the Child PTSD Symptom Scale - Interview and completed the Negative Mood Regulation Questionnaire and the Beck Depression Inventory as part of a baseline evaluation.
Results
Greater emotion regulation difficulties were associated with greater severity of PTSD and depressive symptoms. Additionally, the relationship between emotion regulation difficulties and PTSD severity was mediated by depressive symptoms. However, the reverse was also true: the relationship between emotion regulation difficulties and depressive symptoms was mediated by PTSD symptoms.
Conclusions
Mediation analyses showed that emotion regulation difficulties were associated with both PTSD and depressive symptoms rather than fitting a unidirectional model. These findings are consistent with and extend previous research and highlight the importance of emotion regulation in adolescent survivors of sexual abuse.
Keywords: posttraumatic stress disorder, depression, emotion regulation, sexual abuse, adolescence
Internationally, it is estimated that 19.7% of women have experienced sexual abuse prior to the age of eighteen (Pereda, Guilera, Forns, & Goméz-Benito, 2009a; 2009b). Childhood sexual abuse is defined as any forced or coerced sexual activity with a minor and may include oral, vaginal, and/or anal penetration with a penis, digits, or foreign objects, as well as forced sexual touching. After experiencing childhood sexual abuse, survivors are at increased risk for developing psychopathology even after controlling for other childhood adversities (Molnar, Buka, & Kessler, 2001; Whiffen & MacIntosh, 2005). One of the psychiatric disorders most frequently linked to childhood sexual abuse is posttraumatic stress disorder (PTSD; Foa, Chrestman, & Gilboa-Schechtman, 2009; McLean, Morris, Conklin, Jayaeickreme, & Foa, 2014; Simon, Feiring, & Kobielski McElroy, 2010). Among adolescents sexually abused as children, the rate of PTSD has been estimated to be 38.5% in nonclinical samples (Perkonigg, Kessler, Storz, & Wittchen, 2000) and as high as 88% in clinical samples (Carey, Walker, Rossouw, Seedat, & Stein, 2008).
The role of emotion regulation in those with PTSD has received increasing attention. Emotion regulation is broadly defined as the “ability to act effectively in the context of emotionally salient events” (Gratz & Roemer, 2004). Emotion regulation strategies can be adaptive, such as acceptance, problem solving, and positive refocusing, whereas other strategies are considered maladaptive, such as rumination, catastrophizing, and self-blame (Garnefski, Kraaij, & Spinhoven, 2001). One important dimension of emotion regulation is one's self-perceived ability for regulating negative moods. Multiple studies demonstrate that self-perceived emotion regulation abilities are important predictors of affect, cognition, and behavior (e.g., Shepherd-McMullen, Mearns, Stokes, & Mechanic, 2015). Self-perceived emotion regulation may be especially important in PTSD, where traumatized individuals may maintain dysfunctional beliefs about their ability to cope with the aftermath (e.g., “I should be able to get over this”).
The association between emotion regulation difficulties and PTSD in survivors of childhood sexual abuse is well-established (e.g., Ehring & Quack, 2010; Messman-Moore, Walsch, & DiLillo, 2010; Ullman, Peter-Hagene, & Relyea, 2014). One study found that survivors who had experienced early-onset, chronic interpersonal trauma including childhood sexual abuse reported significantly higher scores on all measures of emotion regulation difficulties compared to survivors of late onset, non-interpersonal and/or non-chronic traumas (Ehring & Quack, 2010). Furthermore, survey data from university undergraduates demonstrated that trauma frequency was associated with PTSD symptoms via emotion regulation difficulties, but only for those who experienced traumas involving physical, sexual, or emotional abuse perpetrated by someone to whom the victim was close, such as a parent (Goldsmith, Chesney, Heath, & Barlow, 2013). Similarly, among survivors of childhood abuse, difficulties with emotion regulation mediated the link between frequency of abuse and PTSD (Stevens et al., 2013). Overall, these studies suggest that childhood sexual abuse may disrupt normative emotion regulation processes and result in greater PTSD severity.
Research indicates that emotion regulation difficulties are also associated with depressive symptomatology in individuals who experienced child abuse (e.g., Kim & Cichetti, 2010). Survivors of childhood sexual abuse report especially high levels of depressive symptoms (Silverman, Reinherz, & Giaconia, 1996; Feiring, Taska, & Lewis, 1999). Previous studies have shown that depressive symptoms are associated with more frequent use of negative emotion regulation strategies, such as rumination, thought suppression, and catastrophizing, and less frequent use of positive emotion regulation strategies, such as reappraisal and self-disclosure (Campbell-Sills, Barlow, Brown, & Hofmann, 2006; Garnefski & Kraaij, 2006; Gross & John, 2003). Together, this literature suggests that the greater emotion regulation difficulties associated with childhood sexual abuse may be closely tied to increased depressive symptoms.
Despite the findings that emotion regulation difficulties, PTSD, and depressive symptoms are closely related, few studies have attempted to relate these constructs in a single, cohesive model. One study that came close to this goal found that the association between low emotion regulation ability and PTSD in survivors of motor vehicle accidents was mediated by rumination (Ehring & Ehlers, 2014). This study suggests that difficulties in regulating emotions may influence depressive rumination, which in turn contributes to the maintenance of PTSD. While not identical, rumination is an emotion regulation strategy that is closely related to depression. Rumination has been demonstrated to worsen depressed mood (Campbell-Sills et al., 2006; Garnefski & Kraaij, 2006; Gross & John, 2003; Nolen-Hoeksema, Parker, & Larson, 1994) and to result in greater depressive symptoms (Just & Alloy, 1997; Kuehner & Weber, 1999). To date, no studies have examined the relationship between emotion regulation difficulties, PTSD, and depressive symptoms, specifically. It is possible that the relationship between emotion regulation difficulties and greater PTSD symptoms may be exacerbated by depressive symptoms, which would suggest that treating depressive symptoms could improve PTSD symptoms. This may be especially important given research showing that those with PTSD are at a significantly increased risk for major depressive disorder compared to non-trauma exposed individuals (Breslau, Davis, Peterson, & Schultz, 2000).
Taken together, the literature suggests that emotion regulation difficulties are associated with both PTSD and depressive symptoms; however, few studies have investigated how these symptom domains impact one another in adolescents with sexual abuse-related PTSD. Moreover, few studies on emotion regulation in adolescent survivors of sexual abuse have examined self-perceived ability to regulate negative emotions, despite existing literature highlighting the importance of perceived self-efficacy and emotional competence in children's ability to cope with trauma resulting from childhood sexual abuse (Diehl & Prout, 2002). To address this gap, the current study examined the association between self-perceived emotion regulation difficulties and PTSD in female adolescent survivors of childhood sexual abuse and to test whether depressive symptoms mediate this relationship. Based on previous research, we hypothesized that greater emotion regulation difficulties would be associated with greater severity of PTSD and greater depressive symptoms. We also hypothesized that depressive symptoms would mediate the relationship between emotion regulation difficulties and PTSD. To test the specificity of the direction of our effects, we also explored whether PTSD would mediate the relationship between emotion regulation and depressive symptoms.
Methods
Participants
Participants were 90 adolescent females seeking treatment for childhood sexual abuse-related PTSD at Women Organized Against Rape (WOAR), an inner-city community-based rape-crisis center in Philadelphia, PA that provides mental health services to survivors of sexual abuse. This clinic serves a diverse population with many underrepresented patients. Inclusion criteria were primary diagnosis of chronic or sub-threshold PTSD (≥ 1 re-experiencing symptom, ≥ 2 avoidance symptoms, ≥ 2 arousal symptoms, and ≥ 14 on the Child Posttraumatic Stress Scale-Interview) resulting from childhood sexual abuse that had occurred at least 3 months prior to screening. Adolescents were excluded if they started psychotropic medication within the previous 12 weeks, exhibited active suicidal ideation with intent, were diagnosed with a pervasive developmental disorder, had a disorder that was primary relative to PTSD, demonstrated alcohol or substance dependence, or were receiving concurrent trauma-focused psychotherapy.
Participants were 14-17 years old (M = 15; SD = 1.56). All participants identified as female on a self-report demographic measure. Fifty-six percent of the sample identified as African American (n = 50), 24% Caucasian (n = 22), 13% Hispanic (n = 12), 6% Biracial (n = 5), and 1% Native American (n = 1). In terms of comorbid diagnoses, 47.3% met criteria for major depressive disorder (n = 43), 11.0% for obsessive-compulsive disorder (n = 10), 12.1% for generalized anxiety disorder (n = 11), 9.9% for specific phobia (n = 9), 6.6% for social anxiety disorder (n = 6), 5.5% for oppositional defiant disorder (n = 5), 5.5% for attention-deficit/hyperactivity disorder (n = 5), and 1.1% met criteria for panic disorder (n = 1). Additional attributes of the sample are described in McLean et al. (2014).
Procedure
This study used baseline data collected as part of a previously reported clinical trial (Foa et al., 2013). Full study details are described in Foa et al. (2013). Participants were recruited from the following sources: 1) direct referrals to WOAR; 2) referrals to WOAR from their outreach efforts within the Philadelphia School District; and 3) referrals from mental health providers in the Philadelphia area. Potential participants contacted WOAR through the organization's 24-hour hotline and completed an initial screening with a WOAR counselor who assessed for sexual abuse and length of time since trauma. Eligible adolescents and a non-offending primary guardian were invited to complete a pre-treatment assessment with a doctoral level clinical psychologist. During the pre-treatment baseline assessment, participants and their guardian signed minor assent and parental consent and completed a 2-3 hour baseline evaluation consisting of a clinical interview and self-report measures. This study received approval from the University of Pennsylvania institutional review board and the executive board of WOAR.
Measures
The Child PTSD Severity Scale – Interview (CPSS-I; Foa, Johnson, Feeny, & Treadwell, 2001; Gillihan, Aderka, Conklin, Capaldi, & Foa, 2013) assesses PTSD diagnosis and symptom severity in children ages 8 to 18 years of age. The scale consists of 17 items that correspond to DSM-IV-TR symptoms (responses scored as: 0 = not at all; 1 = once a week or less/once in a while; 2 = 2 to 4 times a week/half the time; and 3 = 5 or more times a week/almost always). Total scores range from 0 to 51, with higher scores indicating more severe symptoms. In addition to a total PTSD score, the scale yields three subscale scores: re-experiencing symptoms (5 items), avoidance symptoms (7 items), and hyperarousal symptoms (5 items). This measure has demonstrated excellent psychometric properties including good interrater reliability (.87) and convergent validity with other PTSD measures (Gillihan et al., 2013). The CPSS-I demonstrated acceptable internal consistency in the current sample (Cronbach's alpha = 0.73).
The Negative Mood Regulation Questionnaire (NMR; Catanzaro & Mearns, 1990) is a 30-item self-report questionnaire that assesses beliefs in the efficacy of mood regulatory strategies (scale: 1 = strongly disagree to 5 = strongly agree; range = 30-150). The emotion regulation construct is defined as “the expectancy that some behavior or cognition will alleviate a negative mood state” (Catanzaro & Mearns, 1990). Higher scores on the NMR correspond to greater emotion regulation skills. The items of the NMR can be grouped into three classes: general (i.e., beliefs that negative moods can or cannot be alleviated), cognitive (i.e., thought processes that might influence negative moods), and behavioral (i.e., actions that influence mood when alone or with others). This measure has shown good test-retest reliability over 4 and 8 weeks (r = 0.67; r = 0.78) and acceptable temporal stability as well as discriminant validity from social desirability, locus of control, and depression (Catanzaro & Mearns, 1990). The NMR has been negatively associated with anxiety and depression and positively related to active coping strategies (Catanzaro, 1993; Catanzaro & Horlock, 1996; Mearns, 1991). The NMR demonstrated good internal consistency in our sample (Cronbach's alpha = 0.88). For ease of interpretation, we reversed the NMR scores so that higher scores would correspond to greater self-perceived emotion regulation difficulty.
The Beck Depression Inventory (BDI; Beck, Steer, & Garbin, 1988) is a 21-item self-report measure of cognitive, affective, and somatic symptoms of depression (e.g., sleep disturbance and anhedonia) that has been used in a variety of populations, including trauma survivors (Foa, Rothbaum, Riggs, & Murdock, 1991). Total scores range from 0-63. Split half-reliability has been shown previously to be .93, and this measure has shown high correlations with clinician ratings of depression, ranging from .62 to .65 (Beck, Ward, Mendelson, & Erbaugh, 1961). The BDI showed good internal consistency in the current sample (Cronbach's alpha = 0.86).
Data Analysis
First, we calculated correlations between all variables of interest to verify that the variables were related to each other in the expected directions. Correlations were corrected for multiple comparisons using the false discovery rate (FDR) correction to control for the possibility of inflated Type I errors (Benjamini & Hochberg, 1995). Next, we investigated whether depressive symptom severity mediated the effect of emotion regulation on PTSD severity. Mediation analyses were conducted as specified by Preacher and Hayes (2004) using IBM SPSS Statistics 23. Specifically, we examined the total effect of emotion regulation difficulties on PTSD severity (c path in Figure 1a), the relationship between emotion regulation and depressive symptom severity (a path), the effect of depressive symptom severity on PTSD severity (b path), and the direct effect of emotion regulation on PTSD severity after adding depression as a mediator to the model (c' path). The indirect effect of emotion regulation on PTSD severity through the mediator was tested using bootstrapping procedures, which make fewer assumptions about the sampling distribution. This procedure involves computing unstandardized indirect effects for each of 10,000 bootstrapped samples and calculating the 95% confidence interval (Shrout & Bolger, 2002). In order to test the specificity of the direction of our effects, we also tested the reverse mediation model with PTSD as the mediator and depression severity as the dependent variable, using the same procedures.
Figure 1.
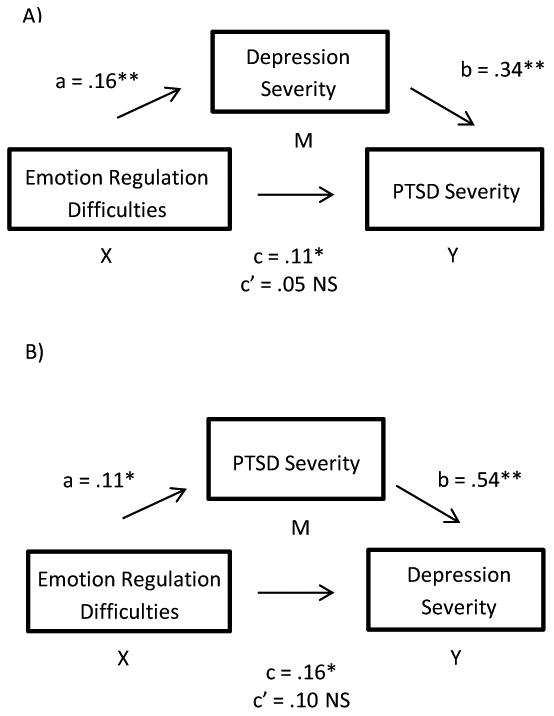
A) The relationship between emotion regulation and PTSD was mediated by depression severity. When controlling for depression severity, the relationship between emotion regulation and PTSD severity becomes non-significant (c'). B) PTSD severity mediated the relationship between emotion regulation and depression. All mediation results show the unstandardized regression coefficients.
Results
Correlation analyses
All correlations reported are FDR corrected for multiple comparisons. Table 1 presents Pearson correlations (two-tailed), means, standard deviations, ranges, and normality estimates for the study variables (NMR, CPSS-I, BDI). As can be seen in Table 1, self-perceived emotion regulation difficulties were positively associated with PTSD and depressive symptoms.
Table 1. Correlations, Means, Standard Deviations, Ranges, and Normality Estimates for Study Variables.
| 1 | 2 | 3 | ||
|---|---|---|---|---|
| 1 | Emotion regulation | – | ||
| 2 | PTSD severity | .26* | – | |
| 3 | Depression severity | .30** | .51** | – |
|
| ||||
| M (SD) | 91.33 (17.20) | 27.91 (7.67) | 21.67 (9.83) | |
| Range | 48-129 | 14-42 | 2-48 | |
| Skewness (SE) | .52 (.26) | .14 (.25) | .59 (.26) | |
| Kurtosis (SE) | .21 (.51) | -.87 (.50) | -.07 (.51) | |
FDR-corrected correlation is significant at the 0.05 level (2-tailed)
FDR-corrected correlation is significant at the 0.01 level (2-tailed).
Mediation analyses
Regression analyses were used to investigate the hypothesis that depression severity mediates the effect of emotion regulation difficulties on PTSD severity. First, we demonstrated that emotion regulation difficulties significantly predicted PTSD severity (b = 0.11, SE = 0.05, t(83) = 2.35, p = .021). Results also indicated that emotion regulation difficulties were a significant predictor of depression severity (b = 0.16, SE = 0.06, t(83) = 2.80, p = .006), and that depression severity was a significant predictor of PTSD severity (b = 0.34, SE = 0.08, t(83) = 4.23, p < .001). Emotion regulation difficulties were no longer a significant predictor of PTSD severity after adding depression as a mediator (b = 0.05, SE = 0.04, t(82) = 1.21, p = .228), consistent with significant mediation (see Figure 1a). Approximately 23% of the variance in PTSD severity was accounted for by the predictors (R2 = .233). The indirect effect tested using a bootstrap estimation approach with 10,000 samples was significant (b = 0.06, SE = 0.03, 95% CI = 0.02, 0.12). The reverse mediation model with PTSD as the mediator and depression severity as the dependent variable was also significant (b = 0.06, SE = 0.03, 95% CI = 0.01, 0.13; See Figure 1b). In this model, the predictors accounted for approximately 25% of the variance in depression severity (R2 = .252).
Discussion
The current study examined the associations between self-perceived emotion regulation difficulties, depressive symptoms, and PTSD severity in a sample of adolescents with sexual abuse-related PTSD. As hypothesized, greater emotion regulation difficulties were associated with greater severity of PTSD symptoms. This finding is consistent with previous findings showing that emotion regulation difficulties are related to PTSD symptoms in trauma survivors, particularly in survivors of childhood sexual abuse (e.g., Ehring & Quack, 2010; Moore, Zoellner, & Mollenholt, 2008; Tull, Barrett, McMillan, & Roemer, 2007). Whereas these earlier studies examined emotion regulation strategies, the current study extends previous work by using a measure of self-perceived ability to regulate emotion. Cognitive theories of emotion suggest that individual's beliefs about their ability to regulate negative emotions have important implications for the development and treatment of psychiatric disorders (Catanzaro & Mearns, 1990). The results of this study provide evidence for the importance of self-perceived emotion regulation abilities in adolescents with PTSD related to childhood sexual abuse.
Emotion regulation difficulties were also associated with depressive symptoms in the current study. This is consistent with the notion that emotion regulation difficulties may make it difficult to inhibit thinking about negative content (Joorman & Gotlib, 2010) and may lead survivors to engage in rumination to cope with these difficulties (Nolen-Hoeksema, Wisco, & Lyobomirsky, 2008). Rumination, or repeatedly focusing on negative thinking, often occurs in the context of depression. For example, research has shown that emotion regulation difficulties, such as disengagement (e.g., denial) or involuntary engagement (e.g., rumination), were related to higher levels of depressive symptoms (Silk, Steinberg, & Morris, 2003). The current results extend this work by demonstrating an association between greater self-perceived emotion regulation difficulties and greater depressive symptoms in adolescent females with sexual abuse-related PTSD. While theory suggests that rumination may be an important maladaptive emotion regulation strategy associated with depression, additional research is needed to identify whether other types of emotion regulation strategies, such as catastrophizing or self-blame, predict depressive severity.
The results of the current study also demonstrated that depressive symptom severity may contribute to the relationship between emotion regulation difficulties and PTSD severity. This finding is similar to the results of a previous study showing that rumination mediated the association between emotion regulation and PTSD (Ehring & Ehlers, 2014). The Ehring and Ehlers (2014) study suggested that difficulty regulating negative emotions after trauma may promote rumination, which in turn increases PTSD severity. While rumination is not identical to depressive symptoms, it is closely related to depression. The current study showed that self-perceived emotion regulation difficulties (e.g., “I won't be able to put it out of my mind”) may lead to increased depressive symptoms, thus exacerbating an individual's PTSD symptoms. This finding suggests that depressive symptoms, beyond simply rumination, are important to understanding the established link between emotion regulation difficulties and PTSD severity.
However, our results showed that the reverse was also supported: the relationship between emotion regulation difficulties and depression severity was mediated by PTSD severity. This implies that having greater emotion regulation difficulties may lead to greater PTSD symptoms which, in turn, may lead to greater depressive symptoms. But, as mentioned previously, it is also equally likely that greater emotion regulation difficulties may lead to greater depressive symptoms, which may lead to greater PTSD symptoms in the event of a trauma. The results of the current study cannot rule out one or the other possibility, as both mediation models explained a similar amount of variance in the dependent variable. This suggests that emotion regulation difficulties are related to both PTSD and depressive symptoms, rather than fitting a unidirectional causal model.
Conceptually, both outcomes (depression leading to greater PTSD and PTSD leading to greater depression) are likely to be true in different circumstances. Pre-existing major depressive disorder has been shown to result in a threefold greater risk for developing PTSD after a trauma (Breslau et al., 2000), suggesting that someone with depressive tendencies may be vulnerable to developing PTSD in the event of a traumatic event. Conversely, the same study showed that those with a diagnosis of PTSD were at significantly greater risk for developing major depression than non-traumatized individuals, while trauma-exposed individuals without PTSD were no more likely to develop depression than non-traumatized individuals (Breslau et al., 2000). This suggests that experiencing a traumatic event is not necessarily the catalyst that leads to greater depressive symptoms. It may be that the debilitating effects of having PTSD (daily distress and impairment in functioning) may lead an individual to subsequently become depressed. Or the depression and PTSD may occur in parallel but unrelated trajectories. Overall, it is likely that the relationship between emotion regulation difficulties, depressive symptoms, and PTSD results from a combination of these possibilities, which interact in complex ways. Future studies should examine symptom onset (which came first, depressive symptoms or PTSD symptoms) since preexisting symptoms may influence the direction of this effect.
Moreover, there may be additional factors, such as resilience or some other adaptive emotion regulation strategy that protect the trauma-exposed individuals without PTSD from developing either PTSD or major depressive disorder. Or there may exist specific maladaptive emotion regulation strategies that are particularly germane to the development of depressive and PTSD symptoms. Future research on the relationship between emotion regulation, depressive symptoms, and PTSD should examine specific facets of emotion regulation, such as lack of acceptance of emotional response, ability to engage in goal-directed behaviors, poor impulse control, lack of emotional awareness, lack of accessibility to effective emotion regulation strategies, and lack of emotional clarity (Gratz & Roemer, 2004). The systematic study of various dimensions of emotion regulation may provide information on which aspects of emotion regulation are most relevant to the development of depression and PTSD.
Additionally, although the current study was conducted using the DSM-IV-TR PTSD criteria, the new DSM-5 criteria warrants discussion. The reorganization of the PTSD criteria under the DSM-5 led to the inclusion of the “negative alterations in cognitions and mood” cluster which consists of depressive symptoms (decreased interest in activities, feeling isolated, difficulty experiencing positive affect) and negative cognitions (overly negative thoughts and assumptions about oneself or the world; distorted blame of self or others). The endorsement of dysfunctional cognitions represents one type of maladaptive emotion regulation strategy that has been studied widely in relation to PTSD (Foa & Rothbaum, 2001). The recognition that depressive symptoms and maladaptive emotion regulation strategies are an integral part of PTSD symptoms provides conceptual support for the proposed relationship between emotion regulation difficulties, depressive symptoms, and PTSD symptoms.
It is important to note several methodological limitations to the current study. First, whether PTSD symptoms predict depressive symptoms or depressive symptoms predict PTSD symptoms cannot be definitively tested in the current cross-sectional sample due to a lack of temporal precedence in data collected at a single time point. Future work would benefit from exploration of the causal relationship between emotion regulation difficulties, PTSD, and depressive symptoms in a longitudinal or prospective design. Furthermore, participants in this study were female adolescents seeking treatment for sexual abuse-related PTSD; therefore, the results may not generalize to adolescents with PTSD related to other types of traumas. This study also did not assess gender identity or gender role, which may be important attributes to assess in future studies given research showing that youth in the top decile of childhood gender nonconformity report elevated exposure to childhood physical, psychological, and sexual abuse (Roberts, Rosario, Corliss, Koenen, & Austin, 2012). Lastly, this study did not collect information on whether the sexual abuse involved penetration, which has been shown previously to be related to increased clinical symptoms (Molnar, Buka, & Kessler, 2001). We assessed the number of trauma incidents, but this was not found to be related to the variables in the current study. This may be due to lack of variability since most participants in this study reported multiple incidences of sexual abuse. Future studies on sexual abuse should measure both the severity and frequency of the abuse.
Despite these limitations, the current study has some notable strengths. The use of an ethnically diverse, community-based sample where the majority of participants reported multiple incidences of sexual abuse may be more generalizable to clinics serving underrepresented inner-city patients. Furthermore, the use of an adolescent sample mitigates common criticisms of many studies on childhood sexual abuse involving adults or children as participants. Studies involving adult participants require retrospective recall of abuse that occurred many years if not decades before the study, which may be prone to recall bias or error (Fergusson, Horwood, & Woodward, 2000), while studies involving children face the issue that most abused children do not reveal abuse during childhood (London, Bruck, Ceci, & Shuman, 2007). Although an adolescent sample is not immune to recall bias or non-disclosure, the use of adolescents may help to lessen the likelihood of some of these concerns. Additionally, adolescence is a critical period for the development of emotion regulation abilities and is a time when depressive symptoms increase. For example, a 14-year longitudinal study conducted by Roza et al. (2003) reported that mood disorders increase sharply in adolescence and young adulthood, especially in females. This is likely due to a number of factors including hormonal changes during puberty as well as a combination of psychosocial factors including changing relationships with peers, lower self-esteem, and body-image issues (Sowislo & Orth, 2013; Stice, Hayward, Cameron, Killen, & Barr Taylor, 2000).
Future work could also benefit from collecting information on income, medical insurance coverage (e.g., Medicaid vs. private insurance), and Child Protective Services investigations or legal proceedings, to help determine the level of severity and functional impairment of the sample. Additionally, given that recent research has found that current distress and history of sexual abuse among parents can contribute to some dimensions of preschoolers' emotion, such as displays of underregulation of emotion (e.g., Langevin et al., 2016), future studies on adolescent sexual abuse should also examine how these parental factors impact adolescents' self-perceived emotion regulation abilities. Since our sample consisted of many inner-city adolescents in a community-based sample, it is likely that there was a sizable portion of parents with histories of sexual abuse themselves.
Lastly, the results of the current study have implications for clinical settings. Interventions that target emotion regulation strategies may be useful for adolescents with sexual abuse-related PTSD. As our results show, emotion regulation abilities may have important effects on both depressive and PTSD symptoms. Based on the view that early trauma may predispose individuals to have emotion regulation difficulties, a number of authors have advocated for treatments that bolster adaptive emotion regulation strategies (Cloitre, Koenen, Cohen, & Han, 2002; Ehring & Ehlers, 2014; Wolfsdorf & Zlotnick, 2001). This may be especially important in adolescence, which is a crucial developmental period in which individuals learn to regulate affect in adaptive ways with increasing independence (Steinberg & Avenevoli, 2000; Steinberg et al., 2006). Addressing emotion regulation difficulties may increase the effectiveness of evidence-based treatment interventions for depression and PTSD symptoms. In conclusion, the findings of the current study build upon the existing body of knowledge that emotion regulation may be an important dimension of sexual abuse survivors' experiences and may inform our understanding of psychopathology in adolescents with PTSD related to childhood sexual abuse.
Acknowledgments
This research was supported in part by a grant from the National Institute of Mental Health (NIMH) awarded to Edna B. Foa. Trial registration: clinicaltrials.gov, identifier: NCT00417300.
References
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8(1):77–100. doi: 10.1016/0272-7358(88)90050-5. [DOI] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4(6):561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society Series B (Methodological) 1995;57(1):289–300. doi: 10.2307/2346101. [DOI] [Google Scholar]
- Breslau N, Davis GC, Peterson EL, Schultz LR. A second look at comorbidity in victims of trauma: The posttraumatic stress disorder—major depression connection. Society of Biological Psychiatry. 2000;48(9):902–909. doi: 10.1016/S0006-3223(00)00933-1. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Barlow D, Brown T, Hofmann S. Acceptability and suppression of negative emotion in anxiety and mood disorders. Emotion. 2006;6(4):587–595. doi: 10.1037/1528-3542.6.4.587. [DOI] [PubMed] [Google Scholar]
- Carey PD, Walker JL, Rossouw W, Seedat S, Stein DJ. Risk indicators and psychopathology in traumatised children and adolescents with a history of sexual abuse. European Child & Adolescent Psychiatry. 2008;17(2):93–98. doi: 10.1007/s00787-007-0641-0. [DOI] [PubMed] [Google Scholar]
- Catanzaro SJ. Mood regulation expectancies, anxiety sensitivity, and emotional distress. Journal of Abnormal Psychology. 1993;102(2):327–330. doi: 10.1037//0021-843x.102.2.327. http://dx.doi.org/10.1037/0021-843X.102.2.327. [DOI] [PubMed] [Google Scholar]
- Catanzaro SJ, Horlock BA. Mood regulation expectancies predict situational coping responses, but not changes in depression. Proceedings and Abstracts of the Annual Meeting of the American Psychological Society. 1996 Jul;8:111. [Summary] [Google Scholar]
- Catanzaro SJ, Mearns J. Measuring generalized expectancies for negative mood regulation: Initial scale development and implications. Journal of Personality Assessment. 1990;54:546–563. doi: 10.1080/00223891.1990.9674019. http://dx.doi.org/10.1080/00223891.1990.9674019. [DOI] [PubMed] [Google Scholar]
- Diehl AS, Prout MF. Effects of posttraumatic stress disorder and child sexual abuse on self-efficacy development. American Journal of Orthopsychiatry. 2002;72(2):262–5. doi: 10.1037/0002-9432.72.2.262. [DOI] [PubMed] [Google Scholar]
- Ehring T, Ehlers A. Does rumination mediate the relationship between emotion regulation ability and posttraumatic stress disorder? European Journal Of Psychotraumatology. 2014;5 doi: 10.3402/ejpt.v5.23547. http://dx.doi.org/10.3402/ejpt.v5.23547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehring T, Quack D. Emotion Regulation Difficulties in Trauma Survivors: The Role of Trauma Type and PTSD Symptom Severity. Behavior Therapy. 2010;41(4):587–598. doi: 10.1016/j.beth.2010.04.004. [DOI] [PubMed] [Google Scholar]
- Feiring C, Taska L, Lewis M. Adjustment following sexual abuse discovery: The role of shame and attributional style. Developmental Psychology. 2002;38:79–92. doi: 10.1037//0012-1649.38.1.79. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Woodward LJ. The stability of child abuse reports: A longitudinal study of young adults. Psychological Medicine. 2000;30(3):529–544. doi: 10.1017/S0033291799002111. [DOI] [PubMed] [Google Scholar]
- Foa EB, Chrestman KR, Gilboa-Schechtman E. Prolonged exposure therapy for adolescents with PTSD: Emotional processing of traumatic experience (Therapist guide) New York, NY: Oxford University Press; 2009. [Google Scholar]
- Foa EB, Rothbaum BO. Treating the trauma of rape: Cognitive-behavioral therapy for PTSD. New York: Guilford Press; 2001. [Google Scholar]
- Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59(5):715–723. doi: 10.1037/0022-006X.59.5.715. [DOI] [PubMed] [Google Scholar]
- Foa EB, McLean CP, Capaldi S, Rosenfield D. Prolonged exposure vs supportive counseling for sexual abuse–related PTSD in adolescent girls: A randomized clinical trial. Journal of the American Medical Association. 2013;310(35):2650–2657. doi: 10.1001/jama.2013.282829. [DOI] [PubMed] [Google Scholar]
- Foa EB, Johnson KM, Feeny NC, Treadwell KR. The Child PTSD Symptom Scale: A preliminary examination of its psychometric properties. Journal of Clinical Child Psychology. 2001;30(3):376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- Garnefski N, Kraaij V, Spinhoven P. Negative life events, cognitive emotion regulation and emotional problems. Personality and Individual Differences. 1999;30(8):1311–1327. doi: 10.1016/S0191-8869(00)00113-6. [DOI] [Google Scholar]
- Garnefski N, Kraaij V. Relationships between cognitive emotion-regulation strategies and depressive symptoms: A comparative study of five specific samples. Personality and Individual Differences. 2006;40(8):1659–1669. http://dx.doi.org/10.1016/j.paid.2005.12.009. [Google Scholar]
- Gillihan SJ, Aderka IM, Conklin P, Capaldi S, Foa EB. The Child PTSD Symptom Scale: Psychometric properties in female adolescent sexual assault survivors. Psychological Assessment. 2013;25:23–31. doi: 10.1037/a0029553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith RE, Chesney SA, Heath NM, Barlow MR. Emotion regulation difficulties mediate associations between betrayal trauma and symptoms of posttraumatic stress, depression, and anxiety. Journal of Traumatic Stress. 2013;26(3):376–384. doi: 10.1002/jts.21819. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–55. doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology. 2003;85(2):348–362. doi: 10.1037/0022-3514.85.2.348. http://dx.doi.org/10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Joorman J, Gotlib IH. Emotion regulation in depression: Relation to cognitive inhibition. Cognition & Emotion. 2010;24(2):281–298. doi: 10.1080/02699930903407948. http://doi.org/10.1080/02699930903407948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Just N, Alloy LB. The response styles theory of depression: Tests and an extension of the theory. Journal of Abnormal Psychology. 1997;106(2):221–229. doi: 10.1037//0021-843x.106.2.221. http://dx.doi.org/10.1037/0021-843X.106.2.221. [DOI] [PubMed] [Google Scholar]
- Kuehner C, Weber I. Responses to depression in unipolar depressed patients: An investigation of Nolen-Hoeksema's response styles theory. Psychological Medicine. 1999;29(6):1323–1333. doi: 10.1017/S0033291799001282. [DOI] [PubMed] [Google Scholar]
- Langevin R, Hébert M, Allard-Dansereau C, Bernard-Bonnin A. Emotion regulation in sexually abused preschoolers: The contribution of parental factors. Journal of Traumatic Stress. 2016;29(2):180–184. doi: 10.1002/jts.22082. [DOI] [PubMed] [Google Scholar]
- London K, Bruck M, Ceci SJ, Shuman DW. Disclosure of child sexual abuse: What does the research tell us about the ways that children tell? Psychology, Public Policy, & Law. 2005;11(1):194–226. doi: 10.1037/1076-8971.11.1.194. [DOI] [Google Scholar]
- Mearns J. Coping with a breakup: Negative mood regulation expectancies and depression following the end of a romantic relationship. Journal of Personality and Social Psychology. 1991;60(2):327–334. doi: 10.1037//0022-3514.60.2.327. http://dx.doi.org/10.1037/0022-3514.60.2.327. [DOI] [PubMed] [Google Scholar]
- McLean CP, Morris SH, Conklin P, Jayaeickreme N, Foa EB. Trauma characteristics and posttraumatic stress disorder among adolescent survivors of childhood sexual abuse. Journal of Family Violence. 2014;29(5):559–566. doi: 10.1007/s10896-014-9613-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messman-Moore TL, Walsh KL, DiLillo D. Emotion regulation and risky sexual behavior in revictimization. Child Abuse and Neglect. 2010;34(12):967–976. doi: 10.1016/j.chiabu.2010.06.004. [DOI] [PubMed] [Google Scholar]
- Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: Results from the National Comorbidity Survey. American Journal of Public Health. 2001;91(5):753–760. doi: 10.2105/ajph.91.5.753. http://dx.doi.org/10.2105/AJPH.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore LA, Zoellner LA, Mollenholt N. Are expressive suppression and cognitive reappraisal associated with stress-related symptoms? Behaviour Research and Therapy. 2008;46(9):993–1000. doi: 10.1016/j.brat.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Parker LE, Larson J. Ruminative coping with depressed mood following loss. Journal of Personality and Social Psychology. 1994;67(1):92–104. doi: 10.1037//0022-3514.67.1.92. http://dx.doi.org/10.1037/0022-3514.67.1.92. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspectives in Psychological Sciences. 2008;3:400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Pereda N, Guilera G, Forns M, Gómez-Benito J. The international epidemiology of child sexual abuse: a continuation of Finkelhor (1994) Child Abuse & Neglect. 2009a;33(6):331–42. doi: 10.1016/j.chiabu.2008.07.007. http://doi.org/10.1016/j.chiabu.2008.07.007. [DOI] [PubMed] [Google Scholar]
- Pereda N, Guilera G, Forns M, Gómez-Benito J. The prevalence of child sexual abuse in community and student samples: A meta-analysis. Clinical Psychology Review. 2009b;29(4):328–38. doi: 10.1016/j.cpr.2009.02.007. http://doi.org/10.1016/j.cpr.2009.02.007. [DOI] [PubMed] [Google Scholar]
- Perkonigg A, Kessler RC, Storz S, Wittchen HU. Traumatic events and post-traumatic stress disorder in the community: Prevalence, risk factors and comorbidity. Acta Psychiatrica Scandinavica. 2000;101(1):46–59. doi: 10.1034/j.1600-0447.2000.101001046.x. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, and Computers. 2004;36(4):717–731. doi: 10.3758/BF03206553. [DOI] [PubMed] [Google Scholar]
- Roberts AL, Rosario M, Corliss HL, Koenen KC, Austin B. Childhood gender nonconformity: A risk indicator for childhood abuse and posttraumatic stress in youth. Pediatrics. 2012;129(3):410–417. doi: 10.1542/peds.2011-1804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roza SJ, Hofstra MB, van der Ende J, Verhulst FC. Stable prediction of mood and anxiety disorders based on behavioral and emotional problems in childhood: A 14-year follow-up during childhood, adolescence, and young adulthood. American Journal of Psychiatry. 2003;160(12):2116–2121. doi: 10.1176/appi.ajp.160.12.2116. http://dx.doi.org/10.1176/appi.ajp.160.12.2116. [DOI] [PubMed] [Google Scholar]
- Shepherd-McMullen C, Mearns J, Stokes J, Mechanic M. Negative mood regulation expectancies moderate the relationship between psychological abuse and avoidant coping. Journal of Interpersonal Violence. 2015;30(9):1553–1566. doi: 10.1177/0886260514540805. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7(4):422–445. doi: 10.1037//1082-989X.7.4.422. [DOI] [PubMed] [Google Scholar]
- Silverman AB, Reinherz HZ, Giaconia RM. The long-term sequelae of child and adolescent abuse: A longitudinal community study. Child Abuse and Neglect. 1996;20(8):709–723. doi: 10.1016/0145-2134(96)00059-2. [DOI] [PubMed] [Google Scholar]
- Simon VA, Feiring C, Kobielski McElroy S. Making meaning of traumatic events: Youths' strategies for processing childhood sexual abuse are associated with psychosocial adjustment. Child Maltreatment. 2010;15(3):229–241. doi: 10.1177/1077559510370365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowislo JF, Orth U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychological Bulletin. 2013;139(1):213–240. doi: 10.1037/a0028931. [DOI] [PubMed] [Google Scholar]
- Stevens NR, Gerhart J, Goldsmith RE, Heath NM, Chesney SA, Hobfoll SE. Emotion regulation difficulties, low social support, and interpersonal violence mediate the link between childhood abuse and posttraumatic stress symptoms. Behavior Therapy. 2013;44(1):152–61. doi: 10.1016/j.beth.2012.09.003. [DOI] [PubMed] [Google Scholar]
- Silk JS, Steinberg L, Morris AS. Adolescents' emotion regulation in daily life: Links to depressive symptoms and problem behavior. Child Development. 2003;74(6):1869–1880. doi: 10.1046/j.1467-8624.2003.00643.x. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Avenevoli S. The role of context in the development of psychopathology: A conceptual framework and some speculative propositions. Child Development. 2000;71(1):66–74. doi: 10.1111/1467-8624.00119. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Blatt-Eisengart I, Cauffman E. Patterns of competence and adjustment among adolescents from authoritative, authoritarian, indulgent, and neglectful homes: A replication in a sample of serious juvenile offenders. Journal of Research on Adolescence. 2006;16(1):47–58. doi: 10.1111/j.1532-7795.2006.00119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Hayward C, Cameron RP, Killen JD, Barr Taylor C. Body-image and eating disturbances predict onset of depression among female adolescents: A longitudinal study. Journal of Abnormal Psychology. 2000;109(3):438–444. doi: 10.1037/0021-843X.109.3.438. [DOI] [PubMed] [Google Scholar]
- Tull MT, Barrett HM, McMillan ES, Roemer L. A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy. 2007;38(3):303–313. doi: 10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Peter-Hagene LC, Relyea M. Coping, emotion regulation, and self-blame as mediators of sexual abuse and psychological symptoms in adult sexual assault. Journal of Child Sexual Abuse. 2014;23(1):74–93. doi: 10.1080/10538712.2014.864747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfsdorf BA, Zlotnick C. Affect management in group therapy for women with posttraumatic stress disorder and histories of childhood sexual abuse. Journal of Clinical Psychology. 2001;57(2):169–181. 2–0. doi: 10.1002/1097-4679(200102)57:2<169∷AID-JCLP4>3.0.CO. [DOI] [PubMed] [Google Scholar]
- Whiffen VE, MacIntosh HB. Mediators of the link between childhood sexual abuse and emotional distress: A review. Trauma, Violence and Abuse. 2005;6(1):24–39. doi: 10.1177/1524838004272543. http://dx.doi.org/10.1177/1524838004272543. [DOI] [PubMed] [Google Scholar]


