Abstract
Purpose
This study was conducted to (1) compare diet quality among depressed and non-depressed overweight and obese rural-dwelling adults; and (2) determine whether body mass index (BMI) category moderates the relationship between depressive symptoms and overall diet quality.
Methods
Rural adults in Kentucky (n = 907) completed the 9-item Patient Health Questionnaire (PHQ-9) that assessed depressive symptoms and a food frequency questionnaire that generated 2005 Healthy Eating Index (HEI) scores. Participants were grouped into overweight (BMI 25–29.9kg/m2) and obese (≥30kg/m2) and non-depressed (PHQ-9 < 10) and depressed (PHQ-9 ≥ 10) groups. Bootstrapped ANCOVAs were used to compare diet quality among the 4 groups. Ordinary least squares regression using PROCESS was used to determine whether BMI category (overweight vs obese) moderated the association between depressive symptoms and overall diet quality.
Results
Overall diet quality was poorer in the obese depressed group than in the obese non-depressed group. Intake of fruit and dark green/orange vegetables and legumes was lower in the obese depressed group than in the overweight non-depressed group. Depressive symptoms predicted poor overall diet quality (B = −0.287, P < .001) and the relationship was moderated by BMI category (coefficient of BMI category*depressive symptom interaction term = 0.355, P < .049). A significant inverse relationship between depressive symptoms and overall diet quality was observed in the overweight group but not in the obese group.
Conclusion
Components of diet quality vary according to BMI category and depressive symptom status. The relationship between depressive symptoms and diet quality is influenced by BMI category.
Keywords: body mass index, depressive symptoms, diet quality, obesity, rural adults
Despite significant interest in rural health and factors underlying rural-urban disparities in the United States,1,2 rural residents remain disproportionately burdened by certain lifestyle-related chronic diseases.3 Lifestyle-related chronic diseases including heart disease, stroke, and diabetes have contributed to higher rural mortality rates and lower life expectancies—both of which have worsened over the past 40 years—compared to urban areas.4,5 This disparity has led some researchers to describe a “nonmetropolitan mortality penalty” whereby higher mortality rates are observed in rural/nonmetropolitan areas than in urban/metropolitan areas.6,7
Depressive symptoms and diet quality are 2 interrelated modifiable chronic disease risk factors that may underlie rural-urban health disparities. Depression prevalence is greater in rural compared to urban areas,8 and negative associations between depressive symptoms and diet quality have been reported in various populations.9–13 Depressive symptoms may be related to rural residents being less likely than urban residents to consume recommended daily amounts of fruits and vegetables,14 which decreases the risk for chronic conditions including stroke15 and coronary heart disease.16 Fewer than 2% of rural residents have healthy diets defined as a Healthy Eating Index score above 80.17,18 Although a variety of diet quality measures have been used, evidence links higher diet quality scores to favorable health outcomes including better physical functioning19 and lower risk for type II diabetes, cardiovascular disease (CVD), cancer, and mortality.20
Rural residents are more likely to be obese than urban residents,21,22 and consequently they are at greater risk for weight-related chronic conditions. Obese rural adults may be at high risk for experiencing depressive symptoms given evidence of a U-shaped association between BMI and depressive symptoms,23–25 which suggests that those who are overweight may experience a lower depressive symptom burden than those with greater obesity severity. While both overweight and obese rural adults are at risk for weight-related chronic conditions, those who are obese and depressed may be more likely to consume a low-quality diet that further increases chronic disease risk. Determining differences in diet quality between overweight and obese rural adults by depressive symptom status may inform future efforts to improve specific aspects of diet quality where known deficits exist and potentially reduce the risk for chronic conditions in this high-risk population.
Obesity severity has been proposed to moderate the association between depression and obesity, with researchers advocating for studies that adopt moderator/mediator frameworks to further understand these complex relationships.26 Determining whether BMI category moderates the relationship between depressive symptoms and diet quality in high-risk overweight and obese rural-dwelling adults could provide insight about whether the magnitude or direction of this relationship varies by weight status. Such insight may be beneficial for researchers and health care providers when assessing overweight and obese rural adults who may be at risk for having both poor diet quality and depressive symptoms. Therefore, the aims of this study were to (1) compare diet quality among depressed and non-depressed overweight and obese rural-dwelling adults and (2) determine whether BMI category moderates the relationship between depressive symptoms and overall diet quality in this high-risk population.
Methods
Design
This was a secondary analysis using data from the RICH Heart Program Data Bank, which included baseline data from a subsample of overweight and obese adults participating in the Heart Health in Rural Kentucky study. Details of the study have been published elsewhere.27 In brief, the Heart Health study was a 2-phased community-based study designed to improve self-management of CVD risk factors in rural Kentucky adults. The first phase was a randomized, controlled, wait-list intervention conducted in a rural eastern Kentucky, and the second phase was a larger pre- and post-test intervention conducted in 3 other rural areas in Kentucky. Both studies incorporated a “whole health” approach encouraging behavioral changes to improve eating habits, physical activity, medication adherence, and psychological health.
Sample and Setting
Adults living in rural areas were eligible to participate in the study if they met any of the following inclusion criteria: diagnosed with CVD, had 2 or more CVD risk factors, and/or had genetic or congenital heart disease. Risk factors for CVD included age >44 in men or >55 in women; self-reported psychosocial stressors including depression, anxiety, or chronic stress; family history of CVD; history of hypertension or current treatment; abnormal lipids or current treatment; diabetes or gestational diabetes; current smoker; overweight or obese; sedentary lifestyle; and having a diet high in saturated fat, total fat, or low fruit and vegetable intake. Exclusion criteria included taking medications that interfere with lipid metabolism; cognitive impairment; non-English speaking; chronic drug abuse; end-stage renal, liver, or pulmonary disease; active cancer other than skin cancer; gastrointestinal conditions requiring special diets; and conditions severely limiting mobility.
Participants were recruited from 4 sites in eastern and central Kentucky. Recruitment sites were located within non-metropolitan (ie, rural) counties as defined by the United States Department of Agriculture, Economic Research Service’s Rural-Urban Continuum Codes (RUCC).28 Rural-Urban Continuum Codes range from 1–9 with higher scores indicating greater rurality. Metropolitan (ie, urban) counties are classified according to the size of their metropolitan areas, while non-metropolitan counties are classified by degrees of urbanization and adjacency to metropolitan areas. For this study, we used Rural-Urban Continuum Codes 4–9 to designate rural counties.28
Measures
Healthy Eating Index Scores
The VioScreen™ online food-frequency questionnaire (FFQ; Viocare Inc., Princeton, New Jersey) was used to collect data on dietary patterns that were used to generate HEI-2005 scores. This FFQ incorporates food images to assist participants when estimating portion sizes and prompts participants for additional details as responses are being recorded. Food and nutrition information from the Nutrition Coordinating Center Food and Nutrient Database is used to generate the dietary analysis, and HEI scores are automatically calculated.29 This FFQ has been shown to reliably measure energy-adjusted macronutrient intake when compared with 6, 24-hour dietary recalls conducted over 90 days and performs as well as paper-based FFQs.30 For energy-adjusted macronutrient intake, the FFQ underestimates fat (5%) and protein (4%), and overestimates carbohydrates (4%).
The HEI-2005 is a measure of diet quality developed by the United States Department of Agriculture’s (USDA) Center for Nutrition Policy and Promotion to monitor adherence to 2005 national dietary recommendations. The HEI-2005 contains 9 adequacy and 3 moderation components that include all the MyPyramid major food groups and recommendations from the 2005 Dietary Guidelines and MyPyramid (eg, whole grains to reflect that half of consumed grains should be whole).31 The 9 adequacy components include total fruit (5 points), whole fruit (5 points), total vegetables (5 points), dark green and orange vegetables and legumes (5 points), total grains (5 points), whole grains (5 points), milk (10 points), meat and beans (10 points), and oils (10 points). The 3 moderation components include saturated fat (10 points), sodium (10 points), and calories from solid fats, alcoholic beverages, and added sugars (20 points). Standards for components were based upon participant data from the 2001–2002 National Health and Nutrition Examination Survey (NHANES), which provided one 24-hour dietary recall.31 Recommended amounts of food consumption were based on the USDA’s 12 MyPyramid food patterns, adequate intakes, and tolerable upper intake levels. These recommended amounts were then converted to densities and expressed in amounts per 1,000 calories. Higher scores for each HEI component represents an intake closer to the standard, and maximum points are awarded for meeting the standard. Moderation components are reverse scored (ie, greater intake corresponds with a lower score) due to the need to consume less of these items. The HEI-2005 total score is calculated by summing the component scores and can range from 0–100 with higher scores indicating better diet quality. Guenther and colleagues32 reported that HEI-2005 scores were high for menus developed by nutrition experts and that 9 of the 12 component scores were lower in smokers compared to nonsmokers. Further, low correlations among component scores with total energy were observed, suggesting that the HEI-2005 captures diet quality independent of energy intake. These findings support the validity of using the HEI-2005 as a measure of diet quality.32
Depressive Symptoms
Depressive symptoms were measured using the validated 9-item Patient Health Questionnaire (PHQ-9).33 The frequency of experiencing each of the 9 items is assessed over a 2-week period with responses ranging from “0; Not at all” to “3; Nearly every day.” The total score ranges from 0–27 with higher scores indicating higher levels of depressive symptoms. A total score of 0–4 represents minimal depressive symptoms, 5–9 mild, 10–14 moderate, 15–19 moderately severe, and 20–27 severe. We used the established PHQ-9 cut point of ≥1033 to categorize participants as being depressed.
Body Mass Index
Trained research staff measured each participant’s height and weight using a portable stadiometer and professional-grade digital scale. Height was measured without shoes to the nearest 0.1cm, and weight was measured to the nearest 0.1lb with participants wearing only light clothing without shoes. Body mass index (BMI) was calculated as the weight in kilograms divided by height in meters squared. We categorized participants into 2 groups using a single binary variable (0 = overweight, 1 = obese) using a standard BMI cutpoint of 25–29.9 kg/m2 for overweight and ≥30 kg/m2 for obese.34
Other Variables of Interest
To characterize the sample, the following data were also obtained using a self-reported questionnaire: age, sex, race, marital status, education level, financial status, employment status, and when blood pressure and blood glucose had been checked by a health care provider. The Charlson Comorbidity Index35 was used to assess participant comorbidities.
Procedure
Institutional Review Board approvals were obtained prior to recruitment and all participants provided signed informed consent. Participants were recruited from Centers of Rural Health, primary care offices, and community settings including churches, employment settings, and health fairs. Once enrolled, participants completed baseline questionnaires and underwent a brief physical exam during which trained research staff measured height and weight.
Data Analysis
Frequency distributions and descriptive statistics were examined on all variables to assess for outliers and violations of normality. Bonferroni corrected one-way ANOVAs and Chi-square tests of association were used to compare differences in sociodemographic characteristics, BMI, and depressive symptoms between the overweight and obese groups by depressed/non-depressed status.
To address Aim 1, we conducted Bonferroni corrected ANCOVAs controlling for age and sex to compare the HEI-2005 total score and component scores between overweight and obese rural-dwelling adults who were depressed and non-depressed. We used simple sampling bootstrapping of 1000 samples at a 95% bias-corrected and accelerated confidence interval to compare mean differences in HEI total and component scores due to the data being non-normally distributed and the high frequency of maximum scores within each component.
To address Aim 2, we used Andrew F. Hayes’ PROCESS macro for SPSS36 (IBM Corp, Armonk, New York) to test whether BMI category moderated the relationship between depressive symptoms as a continuous variable and overall diet quality. We controlled for age, sex, and education due to their influence on diet quality.37,38 PROCESS uses ordinary least squares regression in creating moderation models and offers several advantages to performing moderation analyses over standard regression procedures. PROCESS centers predictor variables and automatically computes the interaction term between the predictor and moderator variable. PROCESS also performs simple slopes analyses to determine the relationship between the predictor and outcome at levels of the moderating variable.
As a sensitivity analysis, we examined whether BMI category moderated the relationship between depressive symptoms and diet quality in participants with and without hypertension and diabetes to better assess how these risk factors affected our relationship of interest. Data analyses were conducted using SPSS version 24. An alpha level < 0.05 was deemed statistically significant.
Results
Sample Characteristics
Table 1 shows the sample characteristics. On average, the obese depressed group was younger and obtained fewer years of formal education than the overweight non-depressed group. The overweight depressed group also obtained fewer years of formal education than the overweight non-depressed group. A greater proportion of adults in the obese depressed group reported not having enough money to make ends meet and a lower proportion retired for reasons other than illness compared to the non-depressed groups. A greater proportion of adults in the obese depressed group had retired due to illness compared to the overweight non-depressed group, and both obese groups had a greater proportion of adults with diabetes and hypertension compared to the overweight non-depressed group. The obese depressed group had a higher average BMI compared to the obese non-depressed group. There were no group differences in the proportion of adults having their blood pressure or blood glucose checked by a health care provider within the past year.
Table 1.
Sample Characteristics (n = 907)
| BMI Category and Depressive Symptom Status | ||||
|---|---|---|---|---|
| Variable | Overweight and Non-Depressed (n=261) Mean (SD) or n (%) |
Overweight and Depressed (n = 39) Mean (SD) or n (%) |
Obese and Non-Depressed (n = 476) Mean (SD) or n (%) |
Obese and Depressed (n=131) Mean (SD) or n (%) |
| Age | 54.1 ± 15.5 | 53.0 ± 14.7 | 52.6 ± 14.3 | 49.7 ± 12.9* |
| Sex | ||||
| Female | 178 (68.2%) | 31 (79.5%) | 348 (73.1%) | 101 ((77.1%) |
| Male | 83 (31.8%) | 8 (20.5%) | 128 (26.9%) | 30 (22.9%) |
| Race/Ethnicity | ||||
| Caucasian/White | 251 (96.2%) | 37 (94.9%) | 458 (96.2%) | 126 (96.2%) |
| Other | 10 (3.8%) | 2 (5.1%) | 18 (3.8%) | 5 (3.8%) |
| Marital Status | ||||
| Single | 28 (10.7%) | 4 (10.3%) | 47 (9.9%) | 14 (10.7%) |
| Married or Cohabitating | 185 (70.9%) | 23 (59%) | 337 (70.8%) | 84 (64.1%) |
| Divorced/Separated | 24 (9.2%) | 7 (17.9%) | 43 (9%) | 24 (18.3%) |
| Widowed | 24 (9.2%) | 5 (12.8%) | 49 (10.3%) | 9 (6.9%) |
| Education Level (yrs) | 14.5 ± 3.0 | 13.0 ± 3.7* | 14.1 ± 3.1 | 13.5 ± 2.8* |
| Financial Status | ||||
| Enough or more than enough to make ends meet | 241 (92.3%) | 33 (84.6%) | 451 (94.7%) | 103 (78.6%) |
| Not enough to make ends meet | 20 (7.7%) | 6 (15.4%) | 25 (5.3%) | 28 (21.4%)b |
| Comorbidities | ||||
| Myocardial Infarction | 11 (4.2%) | 5 (12.8%) | 25 (5.3%) | 4 (3.1%) |
| Diabetes | 18 (6.9%) | 6 (15.4%) | 89 (18.7%)* | 36 (27.5%)* |
| Hypertension | 110 (42.1%) | 18 (46.2%) | 253 (53.2%)* | 79 (60.3%)* |
| Blood Pressure Checked | ||||
| Within past year | 235 (90.0% | 39 (100%) | 428 (89.9%) | 120 (91.6%) |
| Never or more than 1 year | 26 (10.0%) | 0 (0%) | 48 (10.1%) | 11 (8.4%) |
| Blood Glucose Checked | ||||
| Within past year | 168 (64.4%) | 28 (71.8%) | 330 (69.3%) | 92 (70.2%) |
| Never or more than 1 year | 93 (35.6%) | 11 (28.2%) | 146 (30.7%) | 39 (29.8%) |
| Employment Status | ||||
| Employed full- or part-time | 187 (71.6%) | 26 (66.7%) | 335 (70.4%) | 90 (68.7%) |
| Homemaker | 13 (5%) | 4 (10.3%) | 27 (5.7%) | 6 (4.6%) |
| Retired not due to illness | 49 (18.8%) | 5 (12.8%) | 80 (16.8%) | 9 (6.9%) b |
| Retired due to illness | 4 (1.5%) | 1 (2.6%) | 16 (3.4%) | 9 (6.9%)* |
| Other | 8 (3.1%) | 3 (7.7%) | 18 (3.8%) | 17 (13%) b |
| Body Mass Index (kg/m2) | 27.6 ± 1.4 | 27.7 ± 1.6 | 36.9 ± 6.1a | 39.2 ± 8.4a |
| Depressive Symptom Score | 3.5 ± 2.7 | 12.7 ± 2.8b | 3.9 ± 2.5c | 13.5 ± 3.5b |
P < .05 compared to overweight non-depressed group
P <. 05 compared to every other group
P < 0.05 compared to overweight non-depressed and obese non-depressed groups
P < 0.05 compared to the overweight depressed and obese depressed groups
Differences in Diet Quality by BMI Category Stratified by Presence of Depressive Symptoms
Table 2 shows the differences in diet quality among overweight and obese rural adults who were depressed and non-depressed. The obese depressed group had a lower HEI total score compared to the obese non-depressed group (60.7 vs 63.1, P = .024). The obese depressed group had lower HEI component scores for total fruit and whole fruit consumption compared to the overweight non-depressed group (2.2 vs. 2.7, P = .009 and 2.7 vs. 3.1, P = .023 respectively). The obese depressed group also had a lower HEI component score for dark green vegetables, orange vegetables, and legumes compared to the non-depressed overweight and obese groups (2.3 vs 2.7, P = .024 and 2.7, P = .008, respectively). Both obese groups had a higher HEI oil score than the overweight non-depressed group. The obese non-depressed group had a lower HEI sodium score compared to the overweight non-depressed group (2.3 vs. 2.8 P = .006,) and the overweight depressed group (2.3 vs 3.2, P = .034) There were no other differences in diet quality among groups.
Table 2.
Total HEI-2005 Diet Quality Scores and Component Scores by Body Mass Index Category and Depressive Symptom Status
| BMI Category and Depressive Symptom Status | |||||
|---|---|---|---|---|---|
|
| |||||
| Variable | Maximum Score | Overweight and Non-Depressed (n=261) |
Overweight and Depressed (n=39) |
Obese and Non-Depressed (n=476) |
Obese and Depressed (n=131) |
| Total Score | 100 | 62.8 (61.4, 64.4) | 62.6 (59.4, 66.2) | 63.1 (62.0, 64.1) | 60.7 (58.9, 62.6)a |
| Adequacy Components† | |||||
| Total Fruit | 5 | 2.7 (2.5, 2.9) | 2.4 (2.0, 2.9) | 2.5 (2.3, 2.6) | 2.2 (2.0, 2.5)* |
| Whole Fruit | 5 | 3.1 (2.9, 3.3) | 2.9 (2.4, 3.4) | 3.0 (2.8, 3.1) | 2.7 (2.4, 3.0)* |
| Total Vegetables | 5 | 4.1 (4.0, 4.2) | 3.8 (3.4, 4.2) | 4.1 (4.0, 4.2) | 3.9 (3.8, 4.1) |
| Dark Green and Orange | 5 | 2.7 (2.5, 3.0) | 2.6 (2.1, 3.0) | 2.7 (2.6, 2.9) | 2.3 (2.1, 2.6)*a |
| Vegetables, and Legumes | |||||
| Total Grains | 5 | 4.0 (3.9, 4.2) | 4.1 (3.8, 4.4) | 4.2 (4.1, 4.2) | 4.1 (3.9, 4.3) |
| Whole Grains | 5 | 1.9 (1.7, 2.0) | 1.8 (1.4, 2.2) | 1.8 (1.6, 1.9) | 1.7 (1.4, 1.9) |
| Milk | 10 | 6.9 (6.6, 7.3) | 7.3 (6.5, 8.1) | 7.0 (6.8, 7.3) | 6.9 (6.4, 7.3) |
| Meat and Beans | 10 | 8.8 (8.6, 9.1) | 9.0 (8.5, 9.4) | 9.1 (8.9, 9.2) | 9.1 (8.8, 9.3) |
| Oils | 10 | 8.5 (8.2, 8.8) | 9.0 (8.4, 9.5) | 8.8 (8.7, 9.0)* | 9.0 (8.6, 9.3)* |
| Moderation Components‡ | |||||
| Saturated Fat | 10 | 5.0 (4.5, 5.4) | 4.3 (3.3, 5.3) | 4.7 (4.3, 5.0) | 4.3 (3.8, 4.9) |
| Sodium | 10 | 2.8 (2.5, 3.1) | 3.2 (2.4, 4.0) | 2.3 (2.1, 2.5)b | 2.4 (2.0, 2.8) |
| Calories from SFAAS | 20 | 12.3 (11.6, 12.9) | 12.2 (10.4, 14.1) | 13.0 (12.5, 13.4) | 12.1 (11.1, 13.1) |
Note: SFAAS=Solid fats, alcoholic beverages, and added sugars; scores adjusted for age and sex; estimated marginal means with 95% bias corrected and accelerated confidence intervals reported.
Higher scores indicate greater consumption
Higher scores indicate less consumption
P < .05 compared to overweight non-depressed group
P < .05 compared to obese non-depressed group
P < .05 compared to the overweight groups
BMI Category as a Moderator of Depressive Symptoms and Overall Diet Quality
Table 3 shows the analysis testing whether BMI category moderates the relationship between depressive symptoms and overall diet quality. The interaction term of BMI category*depressive symptoms was significant (b = 0.355, P = .049), indicating that BMI category moderated the association between depressive symptoms and overall diet quality. The main effect of depressive symptoms was also significant (b = −0.287, P < .001), indicating that greater depressive symptom burden is associated with poorer diet quality. Increasing age, being female, and having a higher education were associated with having a better quality diet.
Table 3.
Assessment of Whether Body Mass Index Category Moderates the Relationship Between Depressive Symptoms and Overall Diet Quality (n = 907)
| Variable | Coefficient (95% CI) | P-value |
|---|---|---|
| Age | 0.261 (0.209–0.313) | < .001 |
| Sex | 3.20 (1.543–4.857) | < .001 |
| Education | 0.261 (0.019–0.504) | .035 |
| BMI Category | 0.369 (−1.212–1.951) | .647 |
| Depressive symptoms | −0.287 (−0.447 to −0.127) | < .001 |
| BMI Category*depressive symptoms | 0.355 (0.002–0.707) | .049 |
|
| ||
| Model R2 | 0.14 | < .001 |
BMI = Body Mass Index
Figure 1 shows the simple slopes analysis of the association between depressive symptoms and diet quality by BMI category. For the overweight group, there was a significant negative relationship between depressive symptoms and diet quality (b = −0.524, P < .001). The negative relationship between depressive symptoms and diet quality in the obese group was not statistically significant (b = −0.170, P = .065).
Figure 1.
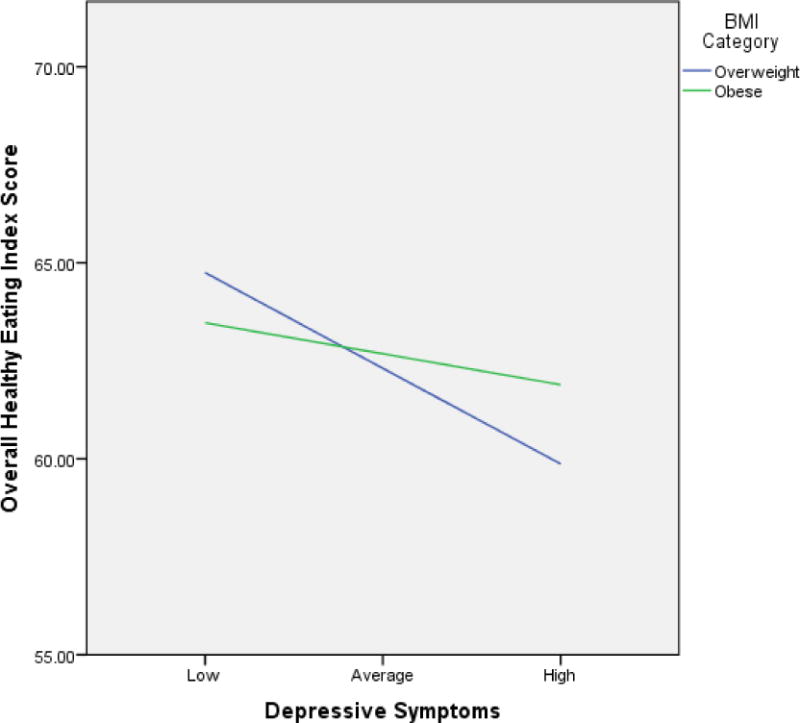
Body Mass Index Category as a Moderator of Depressive Symptoms and Diet Quality in Rural-Dwelling Adults
The sensitivity analyses testing whether BMI category moderated the relationship between depressive symptoms and diet quality in those with and without hypertension and diabetes are shown in Table 4. A BMI moderation effect was observed only in those without these conditions as shown by the interaction between BMI category and depressive symptoms. Among those without hypertension, there was an inverse association between depressive symptoms and diet quality in those who were overweight (b = −0.855, P < .001) but not obese (b = −0.062, P = .670). Among those without diabetes, the inverse association was significant in those who were overweight (b = −0.581, P < .001) but not obese (b = −0.167, P = .123).
Table 4.
Sensitivity Analyses to Determine Whether Body Mass Index Category Moderates the Relationship Between Depressive Symptoms and Overall Diet Quality by Cardiovascular Disease Risk Factors
| Hypertensive (n = 460) | Non-hypertensive (n = 447) | Diabetic (n = 149) | Non-Diabetic (n = 758) | |||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Variable | Coefficient (95% CI) |
P | Coefficient (95% CI) |
P | Coefficient (95% CI) |
P | Coefficient (95% CI) |
P |
| Age | 0.282 (0.207–0.357) | < .001 | 0.247 (0.172–0.323) | < .001 | 0.233 (0.073–0.393) | .005 | 0.249 (0.193–0.305) | < .001 |
| Sex | 4.296 (2.024–6.568) | < .001 | 2.167 (−0.118–4.452) | .063 | 2.429 (−1.512–6.37) | .225 | 3.553 (1.780–5.325) | < .001 |
| Education | 0.171 (−0.157–0.499) | .307 | 0.374 (0.011–0.737) | .043 | −0.150 (−0.690–0.390 | .584 | 0.418 (0.140–0.697) | .003 |
| BMI Category | 0.003 (−2.241–2.248) | .998 | 0.658 (−1.50–2.816) | .549 | −0.825 (−5.759–4.109) | .742 | 0.266 (−1.383–1.915) | .752 |
| Depressive symptoms | −0.219 (−0.435 to −0.003) | .047 | −0.367 (−0.608 to −0.126) | .003 | −0.327 (−0.675–0.020) | .064 | −0.318 (−0.501 to −0.135) | .001 |
| BMI Category*depressive symptoms | −0.142 (−0.638–0.353) | .573 | 0.793 (0.286–1.30) | .002 | 0.065 (−0.810–0.939) | .884 | 0.414 (0.025–0.803) | .037 |
|
| ||||||||
| Model R2 | 0.15 | < .001 | 0.13 | < .001 | 0.13 | .004 | 0.14 | <.001 |
Discussion
Depressive symptoms and poor diet quality are interrelated factors that increase risk for chronic diseases and are modifiable targets for improving the health of rural-dwelling adults. There are 2 primary findings from this study that have important rural health implications. First, overall diet quality was lower in rural-dwelling adults who were both obese and depressed compared to those who were obese and non-depressed. Those who were obese and depressed also consumed a lower quality diet with respect to fruit and certain vegetables compared to those who were overweight and non-depressed. Second, depressive symptoms were associated with poor overall diet quality in rural-dwelling adults and the negative relationship between depressive symptoms and overall diet quality was only significant for the overweight group, not for the obese group. These findings may have potential implications for screening and managing depressive symptoms in overweight and obese rural adults as part of efforts to improve diet quality and reduce rural health disparities.
Several studies have provided evidence of poor diet quality in rural-dwelling US adults.17,18,39 However, little is known about how specific conditions such as depressive symptoms affect diet quality in overweight or obese rural adults who are at high risk for multiple chronic conditions. We found that the obese depressed group had a poorer overall diet compared to the obese non-depressed group, but there were no differences between the overweight and obese groups. Vitolins and colleagues reported that older rural adults with no chronic conditions consumed more fruits and vegetables compared to those with one or more conditions.39 In our study, obese depressed adults had a lower quality diet with respect to total fruit, whole fruit, dark green vegetables, orange vegetables, and legumes than overweight non-depressed adults. Obese depressed adults also had a lower quality diet with respect to dark green vegetables, orange vegetables, and legumes compared to obese non-depressed adults. Rural adults who are both obese and depressed may be at high risk for diet-related comorbidities due to inadequate consumption of fruits and certain vegetables. This is consistent with Lutfiyya and colleagues’ findings that rural adults are less likely than urban adults to consume recommended amounts of fruits and vegetables, and that non-obese rural adults are more likely than obese rural adults to meet these recommendations.14
Our finding of a negative relationship between depressive symptoms and diet quality is in concordance with several existing studies.9–13 However, as noted in 2 recent systematic reviews, there is inconsistent evidence regarding the association between diet quality and depression.40,41 Explanations for conflicting findings include heterogeneity in depression assessment, measurement of diet quality, and covariate selection. For example, Rahe and colleagues reported no association between scores on the Center for Epidemiologic Studies Depression Scale (CES-D) and diet quality after adjusting for multiple covariates including BMI.42 They also found no interaction by BMI. This conflicts with our finding of a moderation effect by BMI category and may be due to our highly specific sample of rural-dwelling overweight and obese adults at high risk for CVD. Greater depression severity has been associated with poorer diet quality among obese participants with major depression,43 providing some evidence that the relationship is strongest among those with excess body weight. Other studies using samples at high risk for CVD support an association between depressive symptoms and diet quality. Depressive symptoms have been associated with poor diet quality among hypertensive men and women with metabolic syndrome44 and among men at high risk for CVD.45 These findings highlight how the relationship between depressive symptoms and diet quality may vary according to various methodological considerations and individual characteristics.
We anticipated the relationship between depressive symptoms and diet quality would be strongest in the obese group given evidence that the association between depression and obesity is strongest among the most severely obese.46 Surprisingly, the negative relationship between depressive symptoms and diet quality was observed only among those who were overweight. There are a couple of possible explanations for this finding. Jacka and colleagues reported that people with a past history of depression who received treatment prior to participating in their study had higher prudent dietary scores even after controlling for current depression.47 Citing evidence that health care providers infrequently provide dietary counseling, they suggest people may modify their diets to improve depressive symptoms. This suggestion has some empirical support with one study reporting 17% of non-St. John Wort users and 43% of St. John Wort users changing their diet as a strategy for depression, stress, or worries.48 Therefore, obese participants may have made favorable dietary changes to self-manage their symptoms and thus diminished the association between depressive symptoms and diet quality in this group. With low quality and poor access to clinical care being barriers to achieving optimal health among rural residents,49,50 obese rural-dwelling adults experiencing high depressive symptom burden may attempt behavioral self-management strategies such as adopting favorable dietary changes to improve their symptoms. Future research is needed to test this hypothesis.
Our sensitivity analyses confirmed that the negative relationship between depressive symptoms and diet quality existed only in rural-dwelling adults who were overweight and not in those who were obese. Interestingly, BMI category moderated the relationship between depressive symptoms and diet quality only in those not having hypertension or diabetes compared to having these comorbidities. Given there were no group differences in having blood pressure or blood glucose assessed by a health care provider within the past year, differential access to health care services is an unlikely explanation for this finding. However, overweight and obese rural adults having these risk factors may be receiving dietary counseling and making dietary changes that affect relationships among BMI, depressive symptoms, and diet quality. Although several unmeasured factors are likely involved, clinicians should consider assessing depressive symptoms and diet quality in overweight rural adults without diabetes and hypertension as part of efforts to reduce chronic disease risk in this population.
Despite our sample being at high risk for CVD and living in rural environments with barriers to healthy eating,51 the overall diet quality in our sample was comparable with national estimates. The average HEI-2005 total scores in our sample of rural-dwelling adults ranged from 60.7 in the obese and depressed group to 63.1 in the obese and non-depressed group. In comparison, the average HEI-2005 total score was 57.0 among participants 40–59 years of age in the 2003–2004 National Health and Nutrition Examination Survey (NHANES) and 63.8 among those 60 years and older.52 Using data from the 2001–2002 NHANES survey, Rehm and colleagues reported that the average HEI-2005 total score was 58.5, with scores increasing with age.53 Further, they reported that HEI-2005 scores were lowest in non-Hispanic black adults compared to other racial/ethnic groups and lower among those with less formal education. However, there were a few notable differences with respect to component scores. In comparison to the total NHANES sample,52 the groups in our sample generally consumed more sodium and saturated fat and fewer calories from solid fats, alcoholic beverages, and added sugars. They also consumed more whole grains, milk, oils, and dark green and orange vegetables and legumes.55 While these findings suggest that rural residents engage in some healthy dietary behaviors, improvements are needed in certain areas such as decreasing intake of sodium and saturated fat.
Multiple strategies have been proposed to improve dietary behaviors as part of efforts to improve health outcomes. Population-level recommendations for improving diet quality include modifying laws, regulations, and tax policies that promote healthy eating, as well as increasing public awareness of the link between diet quality and mental health.54–56 However, there is recognition that accessing healthy foods is particularly challenging for people living in remote and disadvantaged areas.54 Despite overall diet quality scores being similar between those living in food secure versus food insecure areas after adjusting for demographic variables, residents in food insecure areas consume fewer vegetables than those living in food secure areas.38 Therefore, interventions to improve the diet quality of rural adults should be tailored to address known deficits in specific dietary behaviors such as low fruit and vegetable consumption.14
Limitations
Several limitations of this study should be noted. Given our sample included only overweight and obese rural-dwelling adults from Kentucky, findings may not be generalizable to other rural populations having different sociodemographic characteristics and access to different amenities. We were also unable to determine temporal relationships between depressive symptoms and diet quality that may be suggestive of a causal association. However, the primary purpose of the study was to examine diet quality by overweight and obese BMI category and depressive symptom status rather than provide evidence of causal associations. Underreporting of dietary intake may also be a limitation due to several factors including social desirability, participant weight status, and depressive symptoms.57 Finally, our results should be interpreted with caution due to other potential factors that could affect the relationship between depressive symptoms and diet quality in overweight and obese rural-dwelling adults. Although we did not adjust for CVD risk factors in our group comparisons due to concerns of shared variance confounding group effects on diet quality,58 our sensitivity analyses suggest that the moderation effect of BMI category on the relationship between depressive symptoms and diet quality occurs in those without hypertension and diabetes compared to those with these conditions. This study potentially offers valuable insight on relationships between depressive symptoms and diet quality that may be useful for rural stakeholders in addressing rural health outcomes.
Conclusion
In conclusion, specific components of diet quality vary according to BMI category and depressive symptom status. Rural adults who were both obese and depressed had lower diet quality in several areas relative to those who were overweight and non-depressed. The relationship between depressive symptoms and overall diet quality in overweight and obese rural-dwelling adults was moderated by BMI category. The inverse relationship between depressive symptoms and diet quality was significant only for rural adults who were overweight. Interventions to reduce depressive symptoms in rural populations may be a viable strategy to improve diet quality and thus reduce risk for chronic conditions that disproportionately affect rural residents.
Acknowledgments
Funding: This research was funded in part by awards D1ARH16062 and D1ARH20134 from the Health Resources and Services Administration. Drs. Moser and Chung are supported by NIH NINR R01 #NR016824-01.
Footnotes
Disclosures: The authors report no financial or other conflicts of interest.
References
- 1.Gamm L, Hutchison L, Bellamy G, Dabney BJ. Rural healthy people 2010: identifying rural health priorities and models for practice. J Rural Health. 2002;18(1):9–14. doi: 10.1111/j.1748-0361.2002.tb00869.x. [DOI] [PubMed] [Google Scholar]
- 2.Bolin JN, Bellamy GR, Ferdinand AO, et al. Rural Healthy People 2020: New Decade, Same Challenges. J Rural Health. 2015;31(3):326–333. doi: 10.1111/jrh.12116. [DOI] [PubMed] [Google Scholar]
- 3.O’Connor A, Wellenius G. Rural-urban disparities in the prevalence of diabetes and coronary heart disease. Public Health. 2012;126(10):813–820. doi: 10.1016/j.puhe.2012.05.029. [DOI] [PubMed] [Google Scholar]
- 4.Singh GK, Siahpush M. Widening rural-urban disparities in life expectancy, U.S., 1969–2009. Am J Prev Med. 2014;46(2):e19–e29. doi: 10.1016/j.amepre.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 5.Singh GK, Siahpush M. Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969–2009. J Urban Health. 2014;91(2):272–292. doi: 10.1007/s11524-013-9847-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cosby AG, Neaves TT, Cossman RE, et al. Preliminary evidence for an emerging nonmetropolitan mortality penalty in the United States. Am J Public Health. 2008;98(8):1470–1472. doi: 10.2105/AJPH.2007.123778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cossman JS, James WL, Cosby AG, Cossman RE. Underlying causes of the emerging nonmetropolitan mortality penalty. Am J Public Health. 2010;100(8):1417–1419. doi: 10.2105/AJPH.2009.174185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Probst JC, Laditka SB, Moore CG, Harun N, Powell MP, Baxley EG. Rural-urban differences in depression prevalence: implications for family medicine. Fam Med. 2006;38(9):653–660. [PubMed] [Google Scholar]
- 9.Pagoto SL, Ma Y, Bodenlos JS, et al. Association of depressive symptoms and lifestyle behaviors among Latinos at risk of type 2 diabetes. J Am Diet Assoc. 2009;109(7):1246–1250. doi: 10.1016/j.jada.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jacka FN, Mykletun A, Berk M, Bjelland I, Tell GS. The association between habitual diet quality and the common mental disorders in community-dwelling adults: the Hordaland Health study. Psychosom Med. 2011;73(6):483–490. doi: 10.1097/PSY.0b013e318222831a. [DOI] [PubMed] [Google Scholar]
- 11.Jacka FN, Pasco JA, Mykletun A, et al. Association of Western and traditional diets with depression and anxiety in women. Am J Psychiatry. 2010;167(3):305–311. doi: 10.1176/appi.ajp.2009.09060881. [DOI] [PubMed] [Google Scholar]
- 12.Florez KR, Dubowitz T, Ghosh-Dastidar MB, Beckman R, Collins RL. Associations between depressive symptomatology, diet, and body mass index among participants in the supplemental nutrition assistance program. J Acad Nutr Diet. 2015;115(7):1102–1108. doi: 10.1016/j.jand.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beydoun MA, Kuczmarski MT, Mason MA, Ling SM, Evans MK, Zonderman AB. Role of depressive symptoms in explaining socioeconomic status disparities in dietary quality and central adiposity among US adults: a structural equation modeling approach. Am J Clin Nutr. 2009;90(4):1084–1095. doi: 10.3945/ajcn.2009.27782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lutfiyya MN, Chang LF, Lipsky MS. A cross-sectional study of US rural adults’ consumption of fruits and vegetables: do they consume at least five servings daily? BMC Public Health. 2012;12:280. doi: 10.1186/1471-2458-12-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu D, Huang J, Wang Y, Zhang D, Qu Y. Fruits and vegetables consumption and risk of stroke: a meta-analysis of prospective cohort studies. Stroke. 2014;45(6):1613–1619. doi: 10.1161/STROKEAHA.114.004836. [DOI] [PubMed] [Google Scholar]
- 16.He FJ, Nowson CA, Lucas M, MacGregor GA. Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: meta-analysis of cohort studies. J Hum Hypertens. 2007;21(9):717–728. doi: 10.1038/sj.jhh.1002212. [DOI] [PubMed] [Google Scholar]
- 17.Savoca MR, Arcury TA, Leng X, et al. The diet quality of rural older adults in the South as measured by healthy eating index-2005 varies by ethnicity. J Am Diet Assoc. 2009;109(12):2063–2067. doi: 10.1016/j.jada.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vitolins MZ, Tooze JA, Golden SL, et al. Older adults in the rural South are not meeting healthful eating guidelines. J Am Diet Assoc. 2007;107(2):265–272. doi: 10.1016/j.jada.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 19.Hagan KA, Chiuve SE, Stampfer MJ, Katz JN, Grodstein F. Greater adherence to the alternative Healthy Eating Index is associated with lower incidence of physical function impairment in the Nurses’ Health Study. J Nutr. 2016;146(7):1341–1347. doi: 10.3945/jn.115.227900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schwingshackl L, Hoffmann G. Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension score, and health outcomes: a systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2015;115(5):780–800. doi: 10.1016/j.jand.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 21.Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005–2008) J Rural Health. 2012;28(4):392–397. doi: 10.1111/j.1748-0361.2012.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Trivedi T, Liu J, Probst J, Merchant A, Jhones S, Martin AB. Obesity and obesity-related behaviors among rural and urban adults in the USA. Rural Remote Health. 2015;15(4):3267. [PubMed] [Google Scholar]
- 23.Johnston E, Johnson S, McLeod P, Johnston M. The relation of body mass index to depressive symptoms. Can J Public Health. 2004;95(3):179–183. doi: 10.1007/BF03403643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCrea RL, Berger YG, King MB. Body mass index and common mental disorders: exploring the shape of the association and its moderation by age, gender and education. Int J Obes (Lond) 2012;36(3):414–421. doi: 10.1038/ijo.2011.65. [DOI] [PubMed] [Google Scholar]
- 25.Noh JW, Kwon YD, Park J, Kim J. Body mass index and depressive symptoms in middle aged and older adults. BMC Public Health. 2015;15:310. doi: 10.1186/s12889-015-1663-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stunkard AJ, Faith MS, Allison KC. Depression and obesity. Biol Psychiatry. 2003;54(3):330–337. doi: 10.1016/s0006-3223(03)00608-5. [DOI] [PubMed] [Google Scholar]
- 27.Mudd-Martin G, Rayens MK, Lennie TA, et al. Fatalism moderates the relationship between family history of cardiovascular disease and engagement in health-promoting behaviors among at-risk rural Kentuckians. J Rural Health. 2015;31(2):206–216. doi: 10.1111/jrh.12094. [DOI] [PubMed] [Google Scholar]
- 28.United States Department of Agriculture, Economic Research Service. Rural-Urban Continuum Codes. http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx. Accessed July 11, 2016.
- 29.Viocare Technologies. VioScreen. http://www.viocare.com/vioscreen.html. Accessed June 22, 2016.
- 30.Kristal AR, Kolar AS, Fisher JL, et al. Evaluation of web-based, self-administered, graphical food frequency questionnaire. J Acad Nutr Diet. 2014;114(4):613–621. doi: 10.1016/j.jand.2013.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guenther PM, Reedy J, Krebs-Smith SM. Development of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108(11):1896–1901. doi: 10.1016/j.jada.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 32.Guenther PM, Reedy J, Krebs-Smith SM, Reeve BB. Evaluation of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108(11):1854–1864. doi: 10.1016/j.jada.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 33.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129(25 Suppl 2):S102–S138. doi: 10.1161/01.cir.0000437739.71477.ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 36.Hayes AF. The PROCESS macro for SPSS and SAS. http://processmacro.org/index.html. Accessed June 27, 2016.
- 37.Hiza HA, Casavale KO, Guenther PM, Davis CA. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J Acad Nutr Diet. 2013;113(2):297–306. doi: 10.1016/j.jand.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 38.Champagne CM, Casey PH, Connell CL, et al. Poverty and food intake in rural America: diet quality is lower in food insecure adults in the Mississippi Delta. J Am Diet Assoc. 2007;107(11):1886–1894. doi: 10.1016/j.jada.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 39.Vitolins MZ, Quandt SA, Bell RA, Arcury TA, Case LD. Quality of diets consumed by older rural adults. J Rural Health. 2002;18(1):49–56. doi: 10.1111/j.1748-0361.2002.tb00876.x. [DOI] [PubMed] [Google Scholar]
- 40.Quirk SE, Williams LJ, O’Neil A, et al. The association between diet quality, dietary patterns and depression in adults: a systematic review. BMC Psychiatry. 2013;13:175. doi: 10.1186/1471-244X-13-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rahe C, Unrath M, Berger K. Dietary patterns and the risk of depression in adults: a systematic review of observational studies. Eur J Nutr. 2014;53(4):997–1013. doi: 10.1007/s00394-014-0652-9. [DOI] [PubMed] [Google Scholar]
- 42.Rahe C, Baune BT, Unrath M, et al. Associations between depression subtypes, depression severity and diet quality: cross-sectional findings from the BiDirect Study. BMC Psychiatry. 2015;15:38. doi: 10.1186/s12888-015-0426-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Appelhans BM, Whited MC, Schneider KL, et al. Depression severity, diet quality, and physical activity in women with obesity and depression. J Acad Nutr Diet. 2012;112(5):693–698. doi: 10.1016/j.jand.2012.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bonnet F, Irving K, Terra JL, Nony P, Berthezene F, Moulin P. Depressive symptoms are associated with unhealthy lifestyles in hypertensive patients with the metabolic syndrome. J Hypertens. 2005;23(3):611–617. doi: 10.1097/01.hjh.0000160219.71350.d2. [DOI] [PubMed] [Google Scholar]
- 45.Bonnet F, Irving K, Terra JL, Nony P, Berthezene F, Moulin P. Anxiety and depression are associated with unhealthy lifestyle in patients at risk of cardiovascular disease. Atherosclerosis. 2005;178(2):339–344. doi: 10.1016/j.atherosclerosis.2004.08.035. [DOI] [PubMed] [Google Scholar]
- 46.Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2003;158(12):1139–1147. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- 47.Jacka FN, Cherbuin N, Anstey KJ, Butterworth P. Does reverse causality explain the relationship between diet and depression? J Affect Disord. 2015;175:248–250. doi: 10.1016/j.jad.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 48.Pirotta M, Densley K, Forsdike K, Carter M, Gunn J. St John’s wort use in Australian general practice patients with depressive symptoms: their characteristics and use of other health services. BMC Complement Altern Med. 2014;14:204. doi: 10.1186/1472-6882-14-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Anderson TJ, Saman DM, Lipsky MS, Lutfiyya MN. A cross-sectional study on health differences between rural and non-rural U.S. counties using the County Health Rankings. BMC Health Serv Res. 2015;15:441. doi: 10.1186/s12913-015-1053-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hsia RY, Shen YC. Percutaneous Coronary Intervention in the United States: Risk Factors for Untimely Access. Health Serv Res. 2016;51(2):592–609. doi: 10.1111/1475-6773.12335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hardin-Fanning F. Adherence to a Mediterranean diet in a rural Appalachian food desert. Rural Remote Health. 2013;13(2):2293. [PubMed] [Google Scholar]
- 52.Ervin RB. Healthy Eating Index-2005 total and component scores for adults aged 20 and over: National Health and Nutrition Examination Survey, 2003–2004. Natl Health Stat Report. 2011;(44):1–9. [PubMed] [Google Scholar]
- 53.Rehm CD, Monsivais P, Drewnowski A. The quality and monetary value of diets consumed by adults in the United States. Am J Clin Nutr. 2011;94(5):1333–1339. doi: 10.3945/ajcn.111.015560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dash SR, O’Neil A, Jacka FN. Diet and Common Mental Disorders: The Imperative to Translate Evidence into Action. Front Public Health. 2016;4:81. doi: 10.3389/fpubh.2016.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jacka FN, Sacks G, Berk M, Allender S. Food policies for physical and mental health. BMC Psychiatry. 2014;14:132. doi: 10.1186/1471-244X-14-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gortmaker SL, Swinburn BA, Levy D, et al. Changing the future of obesity: science, policy, and action. Lancet. 2011;378(9793):838–847. doi: 10.1016/S0140-6736(11)60815-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Maurer J, Taren DL, Teixeira PJ, et al. The psychosocial and behavioral characteristics related to energy misreporting. Nutr Rev. 2006;64(2 Pt 1):53–66. doi: 10.1111/j.1753-4887.2006.tb00188.x. [DOI] [PubMed] [Google Scholar]
- 58.Miller GA, Chapman JP. Misunderstanding analysis of covariance. J Abnorm Psychol. 2001;110(1):40–48. doi: 10.1037//0021-843x.110.1.40. [DOI] [PubMed] [Google Scholar]


