Abstract
Background
While pets are found in more than 50% of U.S. homes, the effect of pet allergen exposure on asthma morbidity in the United States population is not well documented.
Objective
To determine the effect of dog and cat allergen exposures on asthma morbidity in the U.S. population.
Methods
NHANES is a representative sample of civilian U.S. population. Data on asthma, dog and cat allergen levels in bedroom dust, as well as specific IgE to dog and cat were analyzed for all participants >= 6 years of age.
Results
Pets are common in U.S. with more that 50% of households having a dog or cat or both. The prevalence of allergic sensitization in the NHANES population was similar for dog and cat with both being approximately 12%. Among those who were sensitized, elevated exposure to pet allergens was associated with an increased prevalence of asthma and asthma attacks. Indeed, 44.2% of the asthma attacks were attributable to exposure to high levels of dog allergen in the bedroom among asthmatics sensitive to dog and 30.3% attributable to cat allergen exposure among the comparable cat sensitive-exposed group. Projecting these results to the U.S. population, indicates more than 1 million increased asthma attacks each year for the dog sensitive-exposed group and more than 500,000 increased asthma attacks for the cat sensitive-exposed population of asthmatics.
Conclusion
Elevated exposure to dog and cat allergens among those sensitized individuals with asthma is associated with excess asthma attacks. Reducing pet allergen exposures has the potential for a significant decrease in asthma morbidity.
Keywords: asthma, pets, hospitalizations, allergen exposure, cat, dog, allergen sensitization
Introduction
The influence of pets in the development of asthma, allergy, and exacerbation of existing asthma is complicated. Sensitization to dog and/or cat in early life is a strong predictor of the development of childhood asthma.1 The National Health and Nutrition Examination Survey (NHANES) III found that more cases of asthma could be attributed to sensitization to cat allergen than any other sensitization.2 On the contrary, other investigations have demonstrated a protective effect of pets in early life on developing sensitization3,4 and asthma.1
However, it is known that when sensitized individuals with asthma are exposed to allergens to which they are sensitized, their asthma can become more severe and/or difficult to manage.5 To date, the impact of dog and cat allergen exposures on asthma morbidity among sensitized individuals has not been investigated at the national level, although sensitization to dog (11.8%) and cat (12.1%) is common in the U.S. population,6 and pet ownership is even more common a 2012 American Veterinary Medical Association survey reported that 36.5% of U.S. households having a dog and 30.4% having a cat.7 The NHANES 2005–2006 is the first study of a nationally representative sample to collect dust from U.S. homes; analyze the dust for dog and cat allergens; draw blood to assess dog and cat sensitization; and evaluate asthma morbidity. The home dust allergen assay data did not become available until 2014 because of delays in the laboratory analysis phase of this component.8 These data offer a unique opportunity to determine the importance of dog and cat exposure on asthma morbidity in the U.S. population.
Methods
The NHANES 2005–2006 was a population-based survey conducted by the National Center for Health Statistics (NCHS) to determine the health and nutritional status of the civilian, non-institutionalized U.S. population. The NHANES 2005–2006 protocol was approved by the NCHS Institutional Review Board.9 Signed consent was obtained from all participants 18 years and older. For minors, a parent/guardian provided permission to participate and written assent was provided by children aged 7–17 years.
Trained technicians collected a single, combined sample of dust from the participant’s bedroom bed and floor using a standardized protocol.8 A detailed description of dust collection, storage, and processing is provided in the Supplement. Dust samples were assayed for allergen concentrations using the universal allergen standard (UAS) and MARIA® assay (Indoor Biotechnologies, Charlottesville, VA). UAS values can be easily converted to earlier ELISA measures in order to compare to previously published values (Table E1 in the Supplement).10 Endotoxin levels were assessed with Limulus amebocyte lysate assay.11
Participants ≥ 6 years were tested for allergen-specific IgE antibodies (sIgE) to dog and cat dander with the Pharmacia Diagnostics Immuno-CAP 1000 System (Kalamazoo, Michigan), now known as Thermo Scientific™ ImmunoCAP specific IgE. The upper and lower limits of detection (LLOD) were 1,000 kU/L and 0.35 kU/L, respectively. For samples less than the LLOD, NHANES provided a value equal to the LLOD divided by the square root of 2; for those above the upper limit 1,000 kU/L was provided by NHANES.
Outcome Definitions
Physician-diagnosed, current asthma was defined as a participant responding in the affirmative to the following questions: “Has a doctor or other health professional ever told you that you have asthma?” and “Do you still have asthma?”
Only participants with physician-diagnosed, current asthma were questioned about asthma attacks (“During the past 12 months, have you had an episode of asthma or an asthma attack?”) and about emergency care visits: (“During the past 12 months have you had to visit an emergency room or urgent care center because of asthma?”).
Sensitization for each allergen was defined as a specific-IgE concentration of ≥0.35 kU/L. Elevated pet allergen levels were defined by literature-based morbidity thresholds for cat and dog (8 µg/g and 10 µg/g, respectively) based on previous ELISA standards, which were converted to compare directly with the data generated by use of the UAS in the MARIA® assay, 3.19 µg/g and 2.11 µg/g, respectively.10
Statistical Analyses
Specific IgE and cat and dog allergen concentrations were log-transformed to establish normality. Differences in prevalence of sensitivity, exposure and pet ownership across population characteristics were tested with the chi-square statistic.
The primary association of interest was between sensitivity and exposure (dichotomized at the morbidity threshold for each allergen) and asthma. Unadjusted and adjusted log odds were estimated with logistic regression, and then converted to differences in probabilities by using the inverse-logit function, p=exp[ɑ]/(1+exp[ɑ])12. Differences were adjusted for age, gender, race/ethnicity, poverty index ratio (PIR), serum cotinine levels and endotoxin. Interaction effects were assessed using a 2-way interaction between sensitivity and exposure.
Statistical significance was established a priori at 0.05 for main effects and 0.10 for interactions. The sample weight variable (WTAL2YR) was created by NCHS and used in all analyses to account for the analytic subsample in order to obtain unbiased national estimates. The survey design variables representing the sampling strata (SDMVSTRA) and PSU (SDMVPSU) were used to calculate the SEs for the complex survey design. Analyses were performed with R version 3.2 and survey package (version 3.30)12 to adjust for the complex sampling design and confirmed with SAS (Version 9.1.3; SAS, Inc., Cary, NC) survey sampling procedures.
Results
Of the 5,845 participants in the home allergen sample aged 6 years or more, 5,238 (89.6%) had blood drawn to assess allergen-specific IgE levels and home dust samples collected to measure allergen levels. No significant differences were noted between the full sample and this analytic subsample.
Pet Ownership and Pet Allergen Exposures
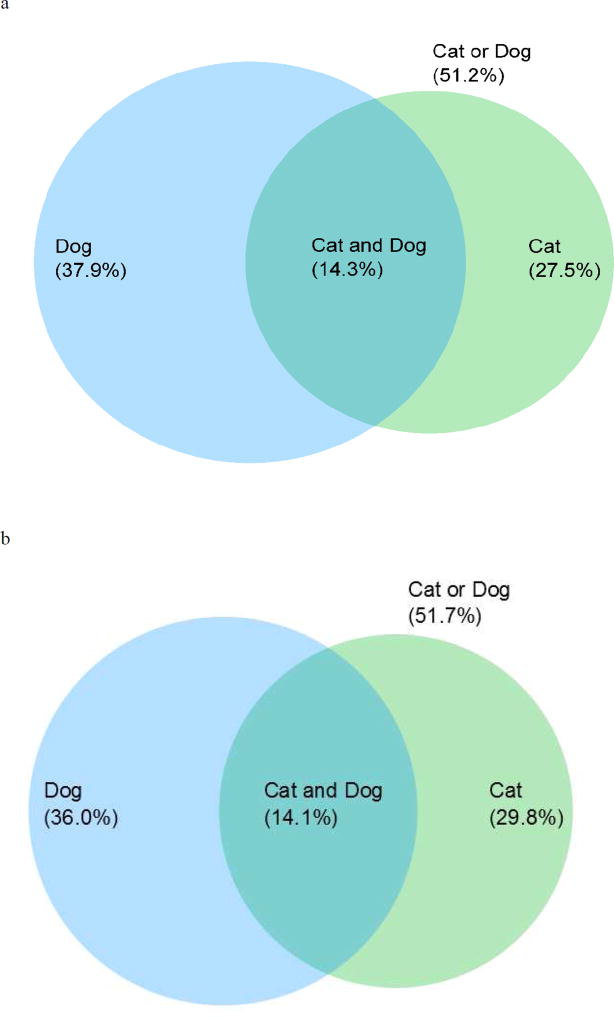
Current pet ownership was common, with 51.2% of the participants reporting either a dog (37.9%, SE=1.99) or cat (27.5%, SE=1.81) present in their home and 14.3% reporting both (Table 1 and Figure 1a). Among those with asthma, pet ownership was slightly higher with 42.2% of the households having a dog and 31.2% owning a cat. Pet ownership varied across socio-demographic groups, with both dog and cat ownership being significantly more common among those who were younger; non-Hispanic White; with higher education and income (Table 1).
Table 1.
Demographic Characteristics of Pet Ownership, Pet Sensitization and Pet Allergen Exposure
| Dog | Cat | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| Variables | Levels | Ownership | Exposure | Sensitivity | Ownership | Exposure | Sensitivity | |||||||
|
| ||||||||||||||
| n* | % (SE) | p-value | % (SE) | p-value | % (SE) | p-value | % (SE) | p-value | % (SE) | p-value | % (SE) | p-value | ||
| Overall | 5238 | 37.9 (1.99) | 36.0 (2.21) | 12.1 (0.64) | 27.5 (1.81) | 29.8 (1.76) | 12.4 (0.67) | |||||||
|
| ||||||||||||||
| Gender | Male | 2586 | 38.1 (2.20) | 0.81 | 35.7 (2.47) | 0.74 | 13.5 (0.81) | 0.005 | 26.5 (1.76) | 0.20 | 27.3 (1.65) | <0.001 | 13.4 (0.86) | 0.008 |
| Female | 2652 | 37.7 (2.06) | 36.2 (2.22) | 10.7 (0.81) | 28.5 (2.17) | 32.2 (2.14) | 11.4 (0.68) | |||||||
|
| ||||||||||||||
| Age | 6–18 | 2008 | 46.2 (3.66) | <0.001 | 44.9 (3.48) | <0.001 | 14.9 (1.02) | <0.001 | 30.0 (2.46) | <0.001 | 32.2 (2.38) | <0.001 | 13.2 (1.39) | 0.05 |
| 19–59 | 2288 | 38.6 (2.22) | 36.3 (2.38) | 12.7 (0.80) | 29.9 (2.14) | 31.4 (2.09) | 12.9 (0.71) | |||||||
| 60–85+ | 942 | 27.1 (1.73) | 25.8 (2.03) | 7.2 (0.96) | 16.9 (1.73) | 21.9 (1.82) | 9.8 (1.44) | |||||||
|
| ||||||||||||||
| Race/Ethnicity | Non-Hispanic White | 2018 | 43.6 (2.27) | <0.001 | 42.3 (2.60) | <0.001 | 11.2 (0.81) | <0.001 | 33.5 (2.04) | <0.001 | 36.4 (1.61) | <0.001 | 12.7 (0.87) | 0.01 |
| Non-Hispanic Black | 1442 | 13.6 (1.73) | 10.1 (1.25) | 17.4 (1.24) | 6.9 (0.78) | 7.4 (0.98) | 13.1 (1.62) | |||||||
| Mexican American | 1377 | 25.4 (2.13) | 22.2 (1.79) | 10.1 (1.14) | 7.8 (1.03) | 10.7 (1.20) | 9.2 (0.98) | |||||||
| Other | 401 | 37.0 (3.92) | 33.2 (4.27) | 13.9 (1.42) | 27.0 (3.94) | 26.4 (4.94) | 11.8 (1.54) | |||||||
|
| ||||||||||||||
| Education | <12th grade | 1528 | 28.8 (3.79) | <0.001 | 23.6 (3.29) | <0.001 | 8.6 (0.87) | 0.007 | 18.8 (2.78) | 0.01 | 19.4 (3.38) | 0.004 | 8.9 (1.12) | 0.04 |
| 12th grade | 1279 | 43.6 (3.60) | 39.2 (3.25) | 12.6 (1.04) | 26.7 (3.12) | 29.5 (2.19) | 13.1 (1.68) | |||||||
| >12th grade | 2248 | 38.4 (2.41) | 38.6 (2.55) | 13.0 (1.03) | 31.4 (2.63) | 34.0 (2.05) | 13.3 (0.98) | |||||||
|
| ||||||||||||||
| Poverty Index Ratio (PIR) | 1st [0 – 1.52] | 1999 | 27.7 (2.88) | <0.001 | 24.7 (2.90) | <0.001 | 11.5 (1.18) | 0.87 | 18.2 (2.52) | <0.001 | 21.1 (2.56) | <0.001 | 10.8 (1.03) | 0.20 |
| 2nd [1.53 – 4.52] | 2238 | 42.1 (2.64) | 39.8 (2.63) | 12.4 (1.03) | 28.0 (2.55) | 29.2 (1.89) | 12.6 (0.90) | |||||||
| 3rd [4.53 – 5.0] | 787 | 40.7 (3.39) | 41.2 (3.64) | 12.2 (1.57) | 36.4 (3.76) | 41.2 (3.06) | 13.5 (1.43) | |||||||
|
| ||||||||||||||
| Cotinine | 1st [0.01 – 0.02] | 1304 | 36.9 (2.93) | 0.26 | 36.6 (3.36) | 0.19 | 10.9 (1.34) | 0.46 | 25.4 (3.55) | 0.38 | 27.4 (2.80) | 0.24 | 11.5 (1.23) | 0.48 |
| 2nd [0.03 – 22.30] | 2915 | 36.6 (2.60) | 34.2 (2.66) | 12.6 (0.88) | 27.2 (2.40) | 29.7 (2.55) | 12.8 (0.96) | |||||||
| 3rd [22.31 – 1156[ | 988 | 41.6 (2.56) | 38.9 (2.28) | 12.2 (0.95) | 30.5 (1.89) | 32.6 (1.99) | 12.1 (0.75) | |||||||
|
| ||||||||||||||
| Endotoxin | 1st [0.017 – 7.97] | 1143 | 25.3 (2.61) | <0.001 | 19.4 (2.44) | <0.001 | 11.4 (1.50) | 0.52 | 23.9 (2.62) | 0.03 | 23.0 (1.86) | <0.001 | 12.3 (1.09) | 0.80 |
| 2nd [7.98 – 33.40] | 2550 | 39.3 (2.27) | 39.0 (2.46) | 11.8 (0.82) | 27.7 (2.40) | 30.9 (2.38) | 12.1 (0.97) | |||||||
| 3rd [33.41 – 4723] | 1545 | 47.6 (2.87) | 46.5 (3.43) | 13.3 (1.10) | 30.8 (2.67) | 34.4 (2.87) | 13.0 (1.08) | |||||||
Unweighted sample sizes calculated from Exposure/Sensitivity
Figure 1.
a. Ownership of Cat and Dog in the United States Population
b. Exposure to Cat and Dog Allergen in the United States Population
In U.S. homes levels of dog allergen exposure exceeding the clinical threshold associated with asthma morbidity were present in 36.0% (SE=2.21) of bedrooms (median = 0.451 µg/g), while the clinically relevant morbidity threshold for cat allergen was exceeded in 29.8% (SE=1.76) of bedrooms (median = 0.260 µg/g) (Table 1, Figure 1b, Table E2 in the Supplement). Allergen levels exceeding the clinically relevant thresholds were more common for pet owners than non-pet owners: dog 84.4% vs. 6.7%, p<0.001 cat 90.2% vs. 7.1%, p<0.001. Allergen exposure varied across socio-demographic groups similarly to pet ownership except that exposure to elevated levels of cat allergen was higher for females (32.2%) than males (27.3%, p<0.001) despite similar proportions of ownership: females 28.5%, males 26.5%, p=0.20). Higher concentrations of dust endotoxin were significantly associated with both dog and cat ownership and exposure (Table 1).
Allergen Sensitivity and Pet Ownership
The rate of allergen sensitization was very similar for dog 12.1% (SE=0.64) and cat 12.4% (SE=0.67) (Table 1). Pet allergen sensitization varied by socio-demographic factors, with lower rates of sensitization for dog and cat among females; those ≥60 years of age; and lower levels of education. Mexican Americans and non-Hispanic whites had the lowest rates of sensitization for dog, while Mexican Americans had the lowest rates of sensitization to cat.
Sensitization was slightly higher for participants reporting ownership of that particular pet, but this difference was not significant. For dog owners, 12.2% were sensitized to dog allergen versus 12.1% (p=0.90) of those not owning a dog. For cat owners, 13.9% were sensitized to cat allergen versus 11.9% (p=0.23) of individuals not owning a cat. A family history of asthma was not related to pet ownership (dog: yes = 36.8% vs. no=36.2%, p=0.83; cat: yes =25.8% vs. no=26.9%, p=0.62). Among individuals with a pet sensitivity, pet ownership of the pet to which the individual was sensitized, was higher among asthmatics than non-asthmatics (dog: 47% vs 35.3%, p<0.05; cat: 39.7% vs 28.3%, p=0.09). For cat, the levels of sIgEs increased with increasing levels of exposure (p=0.05) while a small but statistically insignificant increase was seen for dog (p=0.21) (Figure E1).
Impact of Allergen Sensitivity and Exposure to Pets on Asthma Morbidity
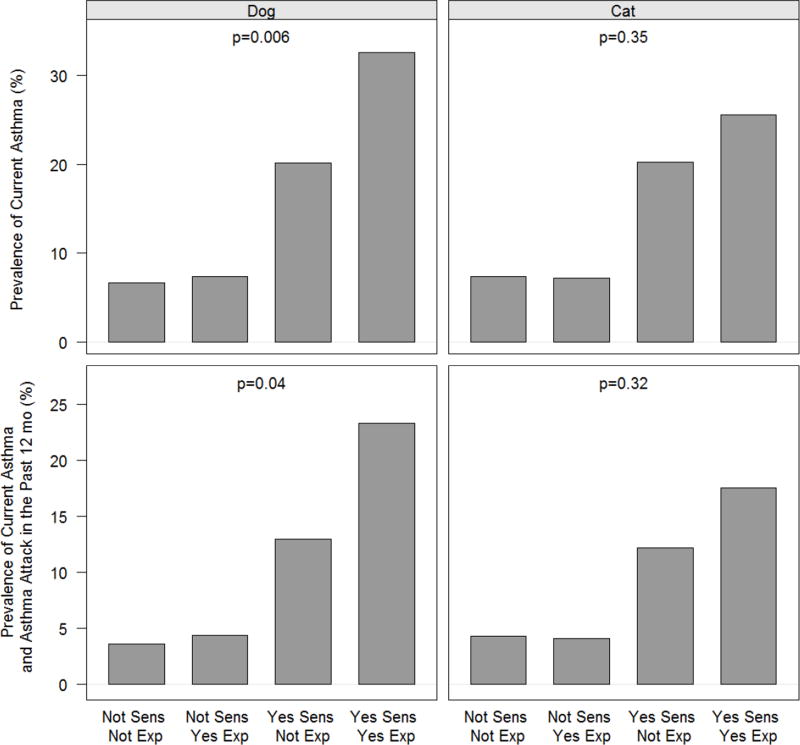
Current asthma and asthma attacks in the prior 12 months were examined to assess the impact of sensitization, exposure, and exposure conditional on sensitization using both adjusted and unadjusted models with similar results for both. Sensitization to either dog or cat increased both current asthma and asthma attacks in the past 12 months, while exposure to elevated allergen levels had little impact on either outcome (Table 2). However, when pet allergen exposure was evaluated conditional on sensitization, among those not sensitized exposure had little to no impact on asthma outcomes, but among the sensitized there were increases for the outcomes for cat and dog (Figure 2, Table E3 in the supplement). However, the combined effects of sensitivity and exposure was only statistically significant in each model for dog.
Table 2.
Exposure or Sensitivity Associations with Asthma and Asthma Attacks (n=5,238)
| Sensitivity | Exposure | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Exposure | Outcome* | Model | Not Sensitive (% SE) |
Sensitive (% SE) | Sensitivity effect (% 95% CI) |
p | Not Exposed (% SE) |
Exposed (% SE) | Exposure effect (% 95% CI) |
p |
| Dog | Current asthma | Unadjusted | 6.9 | 24.8 | 18.0 | <0.001 | 8.2 | 10.6 | 2.4 | 0.10 |
| (0.59) | (3.92) | (9.7,26.2) | (0.79) | (1.10) | (−0.5,5.3) | |||||
| Adjusted** | 6.2 | 23.6 | 17.3 | <0.001 | 7.9 | 10.2 | 2.4 | 0.19 | ||
| (0.67) | (3.89) | (9.3,25.4) | (0.91) | (1.46) | (−1.2,5.9) | |||||
| Asthma Attack in Past 12 months | Unadjusted | 3.8 | 16.7 | 12.9 | <0.001 | 4.6 | 6.8 | 2.3 | 0.04 | |
| (0.30) | (2.75) | (7.5,18.3) | (0.65) | (0.78) | ( 0.1,4.5) | |||||
| Adjusted | 3.0 | 14.0 | 11.0 | <0.001 | 4.0 | 5.6 | 1.6 | 0.22 | ||
| (0.41) | (2.30) | (6.6,15.4) | (0.58) | (1.17) | (−1.0,4.2) | |||||
|
| ||||||||||
| Cat | Current asthma | Unadjusted | 7.2 | 21.9 | 14.6 | <0.001 | 9.0 | 9.2 | 0.2 | 0.88 |
| (0.61) | (2.60) | (9.0,20.2) | (0.69) | (1.03) | (−2.2,2.6) | |||||
| Adjusted | 6.8 | 21.3 | 14.5 | <0.001 | 8.5 | 8.4 | −0.2 | 0.90 | ||
| (0.72) | (2.71) | (8.8,20.1) | (0.81) | (1.24) | (−2.8,2.5) | |||||
| Asthma Attack in Past 12 months | Unadjusted | 4.2 | 13.9 | 9.7 | <0.001 | 5.3 | 5.5 | 0.2 | 0.80 | |
| (0.37) | (1.79) | (6.4,13.0) | (0.52) | (0.76) | (−1.5,1.9) | |||||
| Adjusted | 3.5 | 11.8 | 8.3 | <0.001 | 4.5 | 4.2 | −0.4 | 0.64 | ||
| (0.48) | (1.45) | (5.7,11.0) | (0.53) | (0.89) | (−1.9,1.2) | |||||
Outcomes for those with physician diagnosed asthma and who still have asthma.
Adjusted for Age, Gender, Race/Ethnicity, PIR (Poverty Index Ratio), Cotinine and Endotoxin.
Figure 2.
Unadjusted Exposure and Sensitivity Associations with Asthma
The Impact of Pet Allergen Exposures on the U.S. Population with Asthma and Sensitivity to Pets
One of the strengths of a carefully stratified, population-based study with precise sampling procedures such as NHANES is that inferences can be made to the general population with respect to the effect on disease morbidity (Table 3). Applying the observed rates to the U.S. population, we estimate that approximately 33.1% of those above age 6 with asthma are also sensitive to dog allergen. The rate of attacks in this group was 23.3%. In contrast, the attack rate among those with asthma and sensitive to dog allergen but not exposed was 13.0%. This difference in attack rates allows us to estimate that 1,161,000 excess asthma attacks (44.2% of the total) occur each year as compared to a similar group not exposed to elevated dog allergen in the bedroom.
Table 3.
Population Projections for Asthma Attacks and Emergency Care Visits for those with Asthma and Pet-Sensitivity
| A- Asthma Attack in Past 12 months | |||||
|---|---|---|---|---|---|
| Dog Sensitive (n=28,833,000) |
Cat Sensitive (n=29,527,000) |
||||
| Exposed | No | Yes | No | Yes | |
| n= | 17,563,000 | 11,270,000 | 19,159,000 | 10,368,000 | |
| Asthma Attacks: | 2,283,000 | 2,626,000 | 2,337,000 | 1,814,000 | |
| (13.0%) | (23.3%) | (12.2%) | (17.5%) | ||
| Expected Asthma Attacks * | 1,465,000 | 1,265,000 | |||
| Excess Asthma Attacks with Exposure | 1,161,000 | 549,000 | |||
| % Attributed to Exposure | 44.2% | 30.3% | |||
| B- Asthma Emergency Care Visits in Past 12 months | |||||
|---|---|---|---|---|---|
| Dog Sensitive (n=28,833,000) |
Cat Sensitive (n=29,527,000) |
||||
| Exposed | No | Yes | No | Yes | |
| n= | 17,563,000 | 11,270,000 | 19,159,000 | 10,368,000 | |
| Asthma Emergency Care: | 685,000 | 789,000 | 728,000 | 746,000 | |
| (3.9%) | (7.0%) | (3.8%) | (7.2%) | ||
| Expected Asthma Emergency Care Visits * | 440,000 | 394,000 | |||
| Excess Asthma Emergency Care Visits | 349,000 | 352,000 | |||
| % Attributed to Exposure | 44.2% | 47.2% | |||
= calculated based on attack rate of unexposed
Looking at cat we estimate that approximately 30% of those above age 6 with asthma are also sensitive to cat allergen. The rate of attacks in asthmatics sensitized to cat and exposed to elevated levels of cat allergen in the bedroom was 17.5%. In contrast, the attack rate among those with asthma and sensitive to cat allergen but not exposed was just 12.2%. Thus there were 549,000 excess attacks (30.3% of the total) as compared to a similar group not exposed to elevated cat allergen in the bedroom.
Asthma exacerbations leading to an emergency care visit have a considerably greater economic impact and here we find a similar pattern. The rate of these visits within a 12-month period for those with asthma that are both sensitive and exposed to elevated dog allergen levels is 7.0%, compared to a 3.9% rate for those with asthma who are sensitive to dog allergen but not exposed. Among the dog sensitized and exposed group, of the total of 789,000 emergency care visits, 349,000 (44.2%) are associated with exposure to elevated levels of dog allergen in the bedroom. Among the cat sensitized and exposed group, 352,000 (47.2%) of the total of 746,000 emergency care visits were associated with exposure to elevated levels of cat allergen in the bedroom.
Discussion
Pet ownership, pet allergen exposure and sensitization to pets are common in the U.S. population and most common among population subgroups who typically are less likely to be at risk for adverse environmental exposures. Individuals with asthma who are sensitized and exposed to pet allergens have more asthma attacks and emergency care visits for asthma. We estimate more than 1,700,000 excess asthma attacks and nearly 700,000 excess emergency care visits for asthma each year are associated with exposure to elevated levels of pet allergen in the bedroom among asthmatics sensitive to pets. Medication use was not included in these analyses as the objective is to show the population impact of exposure and sensitization as it exists in the U.S. population. As use of appropriate medication would be expected to reduce the impact of exposure, limiting our analyses to just untreated asthmatics would overestimate the impact. It should be noted that pet allergen exposure in the absence of sensitization did not increase asthma attacks or unscheduled visits.
Home exposure to pet allergens may not reflect the total exposure burden, which could contribute to the inconsistent results with regard to cat. Several investigations have demonstrated that exposure to pet allergens, especially for cat, in schools and day care centers is prevalent and elevated exposure levels can be more common than those found in homes.13–15 The lower effect seen with cat allergen exposure in the bedroom most likely reflects the more frequent exposure to clinically relevant levels of cat allergen outside of the bedroom. This other exposure could easily moderate the importance of the bedroom exposure.
When examining the relationship between pets and health outcomes, there is always a concern about individuals with a disease-altering their pet-keeping habits as a result of their disease, thus leading to a reverse causality. Namely, those with the greatest sensitivity to cat or dog are the least likely to own pets making it appear that the lowest levels of exposure (as found in the homes of non-pet owners) leads to higher sensitivity. Surprisingly, pet ownership was more common for both cats and dogs among those with asthma than those without asthma. Moreover, among sensitized asthmatics, pet ownership of the pet to which they were sensitized was higher than among non-sensitized asthmatics. The relationship of pet ownership among those with sensitization and asthma appears to be complex. For example, the European Community Respiratory Health Survey found avoidance of cat ownership after the development of asthma or allergy but not so for dogs.16 In contrast, the NHANES 2005–2006 found no relationship between personal sensitization or family history of asthma and pet ownership.
These results provide some clarity to the somewhat inconsistent data of earlier studies of pet allergen sensitivity and asthma morbidity. In prior studies, dog allergen exposure has a more consistent effect on asthma morbidity than cat allergen. In a study of asthmatic children, elevated levels of dog allergen among sensitized individuals as compared with non-sensitized individuals were associated with Global Initiative for Asthma determined asthma severity, wheezing, and controller medication use in the prior 12 months, while among those sensitized to cat allergen exposure was associated only with asthma severity, as compared to non-sensitized.17 The combination of sensitization and exposure to the sensitizing pet allergen has been associated with decreased lung function in early life in an European birth cohort study.18 Another study in Northern Sweden reported increasing levels of IgE to cat or dog was associated with increased asthma severity and persistence.19 However, not all studies have found an effect of exposure to cat. The European Respiratory Health Survey observed no association for cat allergen measured in mattresses and asthma symptoms in the total or sensitized population.20,19,13–15
The relationship between exposure to allergen levels and current sensitization is less clear. High levels of cat allergen during infancy have been shown to be positively correlated with sensitization at 2 years but not 6 years, while cat ownership during the first 6 years of life was associated with sensitization at age 6 years in a German birth cohort.21 In the U.S., the Childhood Asthma Management Program observed that levels of dog and cat allergen in household dust were not related to sensitization rates.22 A study in Detroit of 9–12 year old children revealed a linear increase in dog allergen-specific IgE associated with home allergen levels, but not for cat.23 Other investigations have reported high levels of allergen exposure may even induce a tolerance-like state.4
The national scope of the NHANES sample and the standardized method of data collection are among the greatest strengths of this study. The systematic, complex sampling design of the NHANES surveys enables researchers to make projections to the entire U.S. population. This precision allows us to identify population-based relationships that may have important public health implications even in the absence of traditional statistical significance thresholds being met. For example, although the effect for cat sensitivity and exposure among asthmatics is weaker than those observed for dog, the projected increase of more than one-half million excess asthma attacks has important public health implications with regard to excess asthma morbidity and healthcare utilization. While the data collection of NHANES is quite extensive, it is only a single point in time reflecting current pet ownership, allergen exposure in just one room. Nonetheless, the relationship between pet allergen exposure and pet sensitivity among those with asthma appears to be quite clear and points to rather dramatic excess asthma morbidity and healthcare utilization in the U.S. population.
A recent practice parameter advises sensitized individuals to either not get a pet, remove pets from the environment, or take measures to reduce exposure to the allergen.24 These findings provide compelling evidence for that recommendation. The results from this NHANES investigation make clear that the combination of asthma, pet exposure, and pet sensitivity results in considerable excess asthma morbidity. With more than half of the U.S. population owning pets and 1 out of 10 children having asthma, efforts to reduce allergen exposure could have a major impact on asthma morbidity and health care utilization.
Supplementary Material
Highlights.
What is already known about this topic?
Both dog and cat ownership and sensitization are common in the United States. It is known that exposure to pets can increase asthma symptoms for those who are sensitized to the particular pet allergen.
What does this article add to our knowledge?
Exposure to elevated dog or cat allergen in the bedrooms of sensitized asthmatics increases the number of asthma attacks dramatically. Using data from a U.S. population-based study, this study quantifies that increase on a national level.
How does this study impact current management guidelines?
This study highlights the importance of implementing environmental allergen control in homes of asthmatics who are sensitized to, and have pets at home.
Acknowledgments
Funding: This research was supported in part by the Intramural Research Program of the NIH, National Institute of Environmental Health Sciences (Z01 ES025041) and National Institute of Allergy and Infectious Diseases under contract number N01-AI-25482 and grant number and UM2AI117870. PST is supported by NIH P30 ES005605.
Abbreviations
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Survey
- PIR
Poverty Index Ratio
- UAS
Universal Allergen Standard
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Stoltz DJ, Jackson DJ, Evans MD, et al. Specific patterns of allergic sensitization in early childhood and asthma & rhinitis risk. Clin Exp Allergy. 2013;43:233–41. doi: 10.1111/cea.12050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arbes SJ, Jr, Gergen PJ, Vaughn B, Zeldin DC. Asthma cases attributable to atopy: results from the Third National Health and Nutrition Examination Survey. J Allergy Clin Immunol. 2007;120:1139–45. doi: 10.1016/j.jaci.2007.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ownby DR, Johnson CC, Peterson EL. Exposure to dogs and cats in the first year of life and risk of allergic sensitization at 6 to 7 years of age. JAMA. 2002;288:963–72. doi: 10.1001/jama.288.8.963. [DOI] [PubMed] [Google Scholar]
- 4.Platts-Mills T, Vaughan J, Squillace S, Woodfolk J, Sporik R. Sensitisation, asthma, and a modified Th2 response in children exposed to cat allergen: a population-based cross-sectional study. Lancet. 2001;357:752–6. doi: 10.1016/S0140-6736(00)04168-4. [DOI] [PubMed] [Google Scholar]
- 5.Gruchalla RS, Pongracic J, Plaut M, et al. Inner City Asthma Study: relationships among sensitivity, allergen exposure, and asthma morbidity. J Allergy Clin Immunol. 2005;115:478–85. doi: 10.1016/j.jaci.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Salo PM, Arbes SJ, Jr, Jaramillo R, et al. Prevalence of allergic sensitization in the United States: results from the National Health and Nutrition Examination Survey (NHANES) 2005–2006. J Allergy Clin Immunol. 2014;134:350–9. doi: 10.1016/j.jaci.2013.12.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.U.S. Pet Ownership Statistics. [Accessed February 2, 2017]; at https://www.avma.org/KB/Resources/Statistics/Pages/Market-research-statistics-US-pet-ownership.aspx?PF=1.
- 8.National Health and Nutrition Examination Survey 2005–2006. Data Documentation, Codebok, and Frequencies: Allergens - Household Dust (ALDUST_D) [Accessed August 22, 2016];National Center for Healthe Statics. at http://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/ALDUST_D.htm.
- 9.NCHS Research Ethics Review Board (ERB) Appproval. [Accessed August 22, 2016];National Center for Health Statistics. at http://www.cdc.gov/nchs/nhanes/irba98.htm.
- 10.Filep S, Tsay A, Vailes L, et al. A multi-allergen standard for the calibration of immunoassays: CREATE principles applied to eight purified allergens. Allergy. 2012;67:235–41. doi: 10.1111/j.1398-9995.2011.02750.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thorne PS, Mendy A, Metwali N, et al. Endotoxin Exposure: Predictors and Prevalence of Associated Asthma Outcomes in the United States. Am J Respir Crit Care Med. 2015;192:1287–97. doi: 10.1164/rccm.201502-0251OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lumley Thomas. Complex surveys: a guide to analysis using R. Vol. 565. John Wiley & Sons; 2011. [Google Scholar]
- 13.Permaul P, Hoffman E, Fu C, et al. Allergens in urban schools and homes of children with asthma. Pediatr Allergy Immunol. 2012;23:543–9. doi: 10.1111/j.1399-3038.2012.01327.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salo PM, Sever ML, Zeldin DC. Indoor allergens in school and day care environments. J Allergy Clin Immunol. 2009;124:185–92. 92, e1–9. doi: 10.1016/j.jaci.2009.05.012. quiz 93–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tranter DC, Wobbema AT, Norlien K, Dorschner DF. Indoor allergens in Minnesota schools and child care centers. J Occup Environ Hyg. 2009;6:582–91. doi: 10.1080/15459620903103454. [DOI] [PubMed] [Google Scholar]
- 16.Svanes C, Zock JP, Anto J, et al. Do asthma and allergy influence subsequent pet keeping? An analysis of childhood and adulthood. J Allergy Clin Immunol. 2006;118:691–8. doi: 10.1016/j.jaci.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 17.Gent JF, Belanger K, Triche EW, Bracken MB, Beckett WS, Leaderer BP. Association of pediatric asthma severity with exposure to common household dust allergens. Environ Res. 2009;109:768–74. doi: 10.1016/j.envres.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lowe LA, Woodcock A, Murray CS, Morris J, Simpson A, Custovic A. Lung function at age 3 years: effect of pet ownership and exposure to indoor allergens. Arch Pediatr Adolesc Med. 2004;158:996–1001. doi: 10.1001/archpedi.158.10.996. [DOI] [PubMed] [Google Scholar]
- 19.Perzanowski MS, Ronmark E, James HR, et al. Relevance of specific IgE antibody titer to the prevalence, severity, and persistence of asthma among 19-year-olds in northern Sweden. J Allergy Clin Immunol. 2016 doi: 10.1016/j.jaci.2016.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen CM, Thiering E, Zock JP, et al. Is there a threshold concentration of cat allergen exposure on respiratory symptoms in adults? PLoS One. 2015;10:e0127457. doi: 10.1371/journal.pone.0127457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen CM, Rzehak P, Zutavern A, et al. Longitudinal study on cat allergen exposure and the development of allergy in young children. J Allergy Clin Immunol. 2007;119:1148–55. doi: 10.1016/j.jaci.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 22.Huss K, Adkinson NF, Jr, Eggleston PA, Dawson C, Van Natta ML, Hamilton RG. House dust mite and cockroach exposure are strong risk factors for positive allergy skin test responses in the Childhood Asthma Management Program. J Allergy Clin Immunol. 2001;107:48–54. doi: 10.1067/mai.2001.111146. [DOI] [PubMed] [Google Scholar]
- 23.Williams AH, Smith JT, Hudgens EE, et al. Allergens in household dust and serological indicators of atopy and sensitization in Detroit children with history-based evidence of asthma. J Asthma. 2011;48:674–84. doi: 10.3109/02770903.2011.599909. [DOI] [PubMed] [Google Scholar]
- 24.Portnoy JM, Kennedy K, Sublett JL, et al. Environmental assessment andexposure control: a practice parameter - furry animals. Ann Allergy Asthma Immunol. 2012;108:e1–e15. doi: 10.1016/j.anai.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.