Abstract
Objective
To evaluate, among adolescents 10–17 years with an incident hypertensive BP (≥95th percentile) at a primary care visit, whether TeenBP, a novel electronic health record (EHR) linked clinical decision support tool (CDS), improved recognition of elevated BP and return for follow-up BP evaluation.
Methods
We conducted a pragmatic cluster randomized trial in 20 primary care clinics in a large Midwestern medical group. Ten clinics received the TeenBP CDS, including an alert to remeasure a hypertensive BP at that visit, an alert that a hypertensive BP should be repeated in 1–3 weeks and patient-specific order sets. In the 10 usual care (UC) clinics, elevated BPs were displayed in red font in the EHR. Comparisons between CDS and UC used generalized linear mixed models.
Results
The study population included 607 CDS patients and 607 UC patients with an incident hypertensive BP. In adjusted analyses, at the index visit, CDS patients were more likely to have their hypertensive BP based on two or more BPs (47.1% versus 27.6%, p=0.007) and to have elevated BP (ICD-9 796.2) diagnosed (28.2% versus 4.2%, p<0.001). In a multivariate model adjusting for age, sex, SBP percentile, and visit type, rates for repeat BP measurement within 30 days were 14.3% at TeenBP CDS clinics versus 10.6% at UC clinics (p=0.07).
Conclusions
The TeenBP CDS intervention significantly increased repeat BP measurement at the index visit and recognition of a hypertensive BP. Rates for follow-up BP measurement at 30 days were low and did not differ between TeenBP and UC subjects.
Keywords: Decision support, hypertension, adolescents
Introduction
Hypertension affects nearly one third of adults 18 and older in the United States.1 While hypertension is less frequently diagnosed in adolescents, isolated hypertensive blood pressures (BP) are common. Most youth with a single hypertensive BP measured at a school-based screening or outpatient visit will have a normotensive measurement at their next visit.2–4 However, for up to 10% of adolescents, an incident hypertensive BP will be their first indication of new onset hypertension.5 Furthermore, there is increasing evidence of the tracking of adolescent hypertension into adulthood, representing a potentially reversible cause for cardiovascular disease.6–8
The Fourth Report on the Diagnosis, Evaluation and Treatment of High Blood Pressure in Children and Adolescents (Fourth Report), defines hypertension as having BP that is at or above the 95th percentile, based on age, sex and height adjusted norms, at three separate health care visits.9,10 For adolescents with a first BP in the stage 1 hypertension range (≥95th percentile and < 99th percentile + 5mm Hg), measurement at a follow-up visit, within one to two weeks, is recommended. Adolescents with an incident BP measurement in stage 2 hypertension range, (>99th percentile + 5 mm Hg), should have a subsequent BP measured within seven days.9,10
Prior data suggest BP is routinely measured in adolescents at primary care visits.11 However, isolated hypertensive BP measurements in adolescents are rarely clinically recognized12,13 and few patients return for follow-up within the recommended time periods.4 Barriers to recognition include that thresholds for hypertensive BPs are not intuitive,12 algorithms for next steps in management are complicated,9 and clinicians have competing priorities at health care visits.
TeenBP is a sophisticated electronic clinical decision support (CDS) tool, designed to improve recognition and early management of hypertension in youth. Aims of this study were to evaluate the impact of TeenBP on provider recognition of incident hypertensive BPs and rates of follow-up BP measurement in those age 10–17 years.
Methods
Setting
This two-year pragmatic cluster randomized trial took place during 2014–2015 in 20 dedicated primary care clinics within a large Midwestern medical group that provides over 30,000 visits annually to 10–17 year olds. Data for the present analyses are from the first intervention year. All clinics use a common electronic health record (EHR), (EpiCare, Verona, WI), and follow the same standardized procedures for height, weight and BP measurement. Heights were measured using stadiometers and weights were routinely recorded with standardized electronic scales. BP was routinely measured by registered nurses or medical assistants at preventive health visits and at a majority of acute or follow-up visits11 using an automated device (Omron, Omron Healthcare). Those measuring BP were trained to do so based on a detailed written protocol, consistent with American Heart Association standards, with patients rested for 3 to 5 minutes prior to measurement and with appropriate patient positioning, cuff size, and placement of the BP cuff. Repeat measurement of a hypertensive BP by the rooming nurse was routinely recommended as per the medical group protocol. Across all clinical sites, when a height and BP were recorded at the same visit, BP percentiles were calculated and displayed within the EHR. BPs ≥95th percentile were then displayed in the EHR in red with an exclamation mark.
This study was approved by the HealthPartners Institutional Review Board with a waiver of informed consent and it is registered on ClinicalTrials.gov (NCT01760239).
Description of the TeenBP CDS tool
TeenBP is a web-based, electronic health record (EHR) linked, CDS system developed for this project through an iterative process over a 12-month period starting in 2012. It was pilot tested by our team at a single clinical site within the same large medical group from 12/12/13 – 3/4/14. The process for CDS development, testing and piloting, accounting for existing national guidelines on BP management and preferences of clinical leaders within the medical group, while ensuring integration with clinical workflow and technical feasibility, has been previously described.14 The CDS development and piloting aimed to ensure that the best practice advisories and links to CDS were consistent with CDS best practices.15
The TeenBP CDS system is activated when a BP is entered into the vitals section of the EHR. TeenBP then transfers available EHR data from the index and prior visits including: height, weight, problem lists, discharge diagnoses, medications and laboratory data to a web-based server where complex decision support algorithms are applied to assign patients into clinically actionable categories based on their current and prior BPs, BMI, past medical history and recent laboratory testing. Patient medications and diagnoses that may lower or increase BP were also displayed in the CDS. A summary of the patient’s BP and other relevant data are then transmitted back to the EHR and displayed in real time. The analyses in the present study are restricted to patients with a first BP in a 2-year window that is ≥95th percentile, and without prior hypertension or elevated BP diagnoses.
The TeenBP system provides up to 3 EHR alerts or best practice advisories that appear as pop-up windows for the rooming nurse. The first alert would request a height measurement, if a BP was entered in the EHR and there was no height recorded within the prior 12 months. The second alert would notify the rooming staff that a repeat BP should be measured, if an initial SBP or DBP was ≥95th percentile. The third best practice advisory would ask the rooming nurse to notify the provider, if the average systolic BP (SBP) or diastolic BP (DBP) percentile was ≥95th percentile. If the rooming nurse did not update the height data or repeat a BP measurement when alerted, no additional decision support was provided.
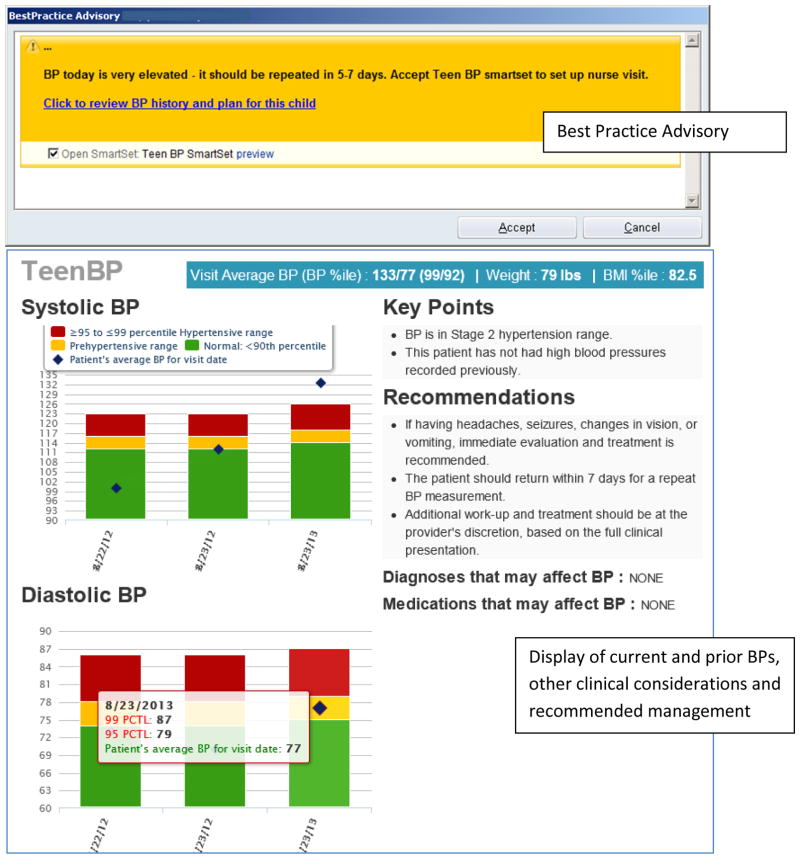
If the alerts had been followed and requested information had been recorded, TeenBP provided additional targeted decision support to medical providers, based on the BP percentile at that visit, prior BPs recorded in the EHR and prior diagnoses. For patients with the average of the initial and repeated SBP or DBP at a single visit ≥95th percentile but <99th percentile + 5mm Hg, no prior BPs ≥95th percentile recorded in the EHR, and no prior diagnoses of hypertension (ICD-9 401–405) or elevated blood pressure (ICD-9 796.2), a best practice advisory or EHR alert displayed the message, “BP today is elevated – it should be repeated in 1–3 weeks. Accept TeenBP SmartSet to set up nurse visit.” The provider could then accept the TeenBP SmartSet to add the following: a diagnosis of “elevated blood pressure reading, without diagnosis of hypertension (ICD-9 796.2), an order for a nurse visit to recheck the BP, and patient educational material regarding elevated BP and hypertension to be added to the patient discharge instructions. The best practice advisory also contained a hyperlink to a web-based display of the patient’s current and prior blood pressures, along with relevant medications and comorbidities. For patients whose first elevated SBP or DBP was in the stage 2 hypertensive range (BP≥99th percentile + 5mmHG), the approach was similar, except a follow-up visit was recommended in 5–7 days. (Figure 1)
Figure 1.
Example of TeenBP decision support
Randomization
Randomization took place four weeks before the start of the intervention. We first stratified the twenty participating clinic sites into three groups based on proportion of patients with public insurance. Within each group, we then sorted clinics into pairs by adolescent patient volume. Using a random number generator, one clinic within each pair was randomly selected to receive the TeenBP CDS while the other continued with usual care (UC) for BP management, resulting in 10 clinics assigned to the TeenBP CDS and 10 clinics to UC.
Training and Implementation
The study Principal Investigator (EOK) and project manager (HLE) conducted in-person trainings at each of the 10 TeenBP CDS intervention sites, within 4 weeks of randomization. Rooming staff, registered nurses, and providers were encouraged to attend the one hour training sessions over the lunch hour. Lunch was provided. TeenBP went live at the 10 intervention sites on 4/15/2014. On a monthly basis, we provided feedback to nurse managers regarding their clinic’s (a) rate of repeating elevated BP measures at the index visit, and (b) proportion of targeted visits at which medical providers opened the CDS visual display or SmartSet, when prompted.
Study population
For these analyses, the study population included youth 10–17 years of age with a first elevated BP (SBP or DBP) ≥95th percentile recorded at a Pediatric or Family Practice outpatient visit from 5/1/14 – 4/30/2015 at one of 20 participating clinical sites. If more than one BP was recorded at a single visit, the average of two or more readings was used to calculate SBP and DBP percentiles. Patients with prior hypertension or elevated BP diagnoses, or who were pregnant or postpartum were excluded. Patients with no height recorded in the EHR at the index visit or within the prior year were also excluded, because it was not possible to calculate BP percentiles for those patients.
Outcomes
The a priori specified primary outcome was return for follow-up BP measurement within 30 days of a first or index hypertensive level BP. Additional outcomes included: repeat measurement of a hypertensive BP at the index visit, provider recognition of a hypertensive BP, and patient return for BP measurement within 90 days of the index visit.
Covariates
Variables gathered from electronic health databases included patient demographics (age, sex, race/ethnicity, language, and insurance type), patient clinical characteristics (exact SBP and DBP percentiles and body mass index [BMI] at index visit), provider department, and visit-related factors (visit type, number of primary care visits in prior 6 months).
Analytic approach
This study was powered at 80% (2-sided alpha=0.05) to detect a difference in the proportion of patients having BP re-measured within 30 days for 25% of subjects in the TeenBP CDS arm compared to 12% in usual care. The sample size was based on an expected 1226 adolescents with incident elevated BPs recorded from 18 clinics, and an expected ICC=0.04 for BP repeat measurement.
Differences by study arm in patient and visit attributes were tested with Pearson’s chi-square test and independent sample t-tests. Generalized linear mixed models with a logit link and a random intercept for clinic were used to test the effect of the intervention on binary outcomes of BP repeat measurement at 30 and 90 days, repeat measurement of an elevated BP at the index visit, and provider recognition of an elevated BP. Each model included a binary indicator for study arm and covariates selected a-priori of age, sex, SBP percentile at the index visit, and index visit type (well child or acute/follow-up visit). Adjusted, model-predicted proportions and 95% confidence intervals are reported for each outcome. For the reporting of other predictors of BP repeat measurement at 30 days, age and SBP percentile are recoded into categories (age 10–13 vs. 14–17; SBP percentile >99% vs. <=99%) to enhance interpretability of odds ratios. In secondary analyses, we evaluated outcomes stratified by BMI and by visit type. All analyses were 2-sided and p values of less than 0.05 were considered statistically significant. Corrections for multiple comparisons were not conducted. All analyses were conducted with SAS version 9.4 (SAS Institute, Cary NC).
Results
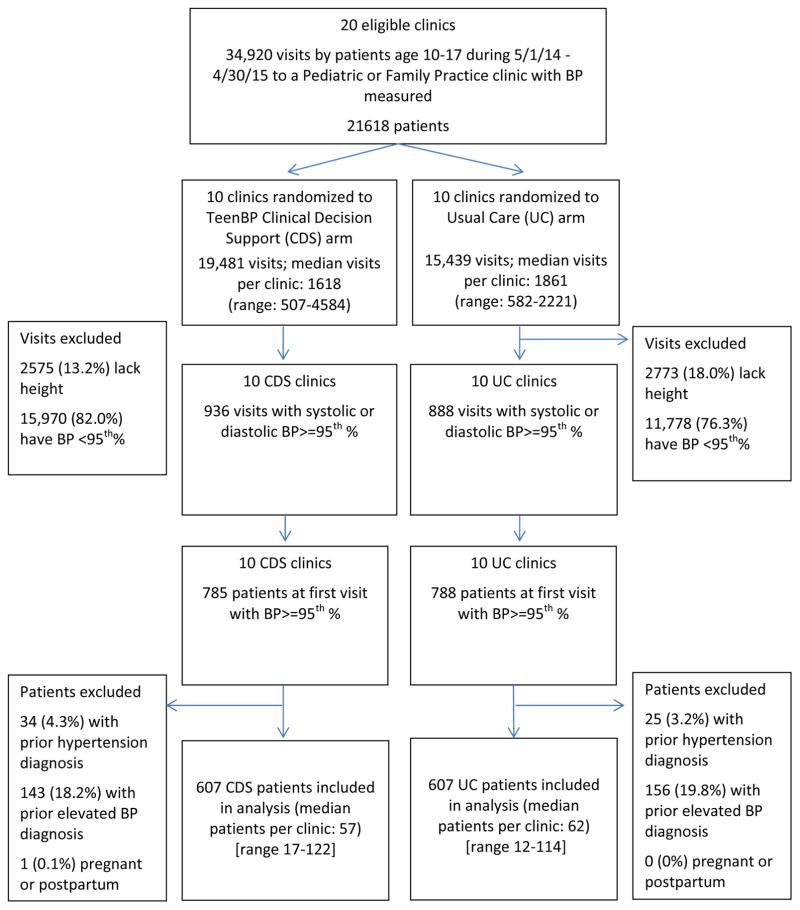
During the 12-month study period, from 4/30/14–4/29/15, there were 19,481 visits (from 11,947 patients) to the 10 TeenBP CDS clinics among 10–17 year olds. Of these, 785 patients had a first documented SBP or DBP ≥95th percentile (6.6%), with no hypertensive level BPs recorded in the EHR in the prior two years. At the 10 UC clinics, over this same time period, for the same age group, there were 15,439 visits (from 10,098 patients) and 788 patients with a first documented SBP or DBP ≥95th percentile (7.8%). After excluding those with a prior hypertension or elevated BP diagnosis (n=358) and female adolescents who were pregnant or postpartum (n=1), our final study population included 607 patients at the TeenBP CDS clinics and 607 patients at the UC clinics with an incident hypertensive BP. (Figure 2)
Figure 2.
CONSORT diagram of subjects enrolled from TeenBP clinical decision support and usual care clinics
The characteristics of the study population are in Table 1. The mean age was 13.6 years, 52% were female and over 90% were privately insured. Baseline demographic and clinical characteristics did not vary significantly between TeenBP CDS and UC subjects, but a significantly greater number of TeenBP CDS subjects were seen by family practice and had their hypertensive BP measured during an acute or follow-up visit.
Table 1.
Characteristics at the first visit with a hypertensive blood pressure (≥95th percentile)
| TeenBP Intervention (n=607) | Usual Care (n=607) | p | ||
|---|---|---|---|---|
|
| ||||
| Age, years | mean (s.d.) | 13.7 (2.2) | 13.5 (2.2) | 0.13 |
|
| ||||
| Female n (%) | 314 (51.7) | 322 (53.1) | 0.65 | |
|
| ||||
| Race | ||||
| White | 363 (59.8) | 338 (55.7) | 0.63 | |
| Black | 111 (18.3) | 120 (19.8) | ||
| Asian | 61 (10.1) | 67 (11.0) | ||
| Other | 17 (2.8) | 23 (3.8) | ||
| Unknown | 55 (9.1) | 59 (9.7) | ||
|
| ||||
| Hispanic ethnicity | n (%) | 41 (6.8) | 40 (6.6) | 0.91 |
|
| ||||
| Language | n (%) | |||
| English | 564 (92.9) | 558 (91.9) | 0.56 | |
| Spanish | 15 (2.5) | 13 (2.1) | ||
| Othera | 28 (4.6) | 36 (5.9) | ||
|
| ||||
| Insurance | n (%) | 0.48 | ||
| Private | 568 (93.6) | 557 (91.8) | ||
| Public | 33 (5.4) | 42 (6.9) | ||
| Self-pay | 6 (1.0) | 8 (1.3) | ||
|
| ||||
| BMI percentile | n (%) | 0.73 | ||
| <85th | 234 (43.8) | 241 (46.3) | ||
| 85-<95th | 120 (22.5) | 113 (21.7) | ||
| ≥95th | 180 (33.7) | 167 (32.1) | ||
|
| ||||
| BP percentile | ||||
| SBP≥99th percentile | 104 (17.1) | 80 (13.2) | 0.14 | |
| SBP≥95th and <99th percentile | 353 (58.2) | 378 (62.3) | ||
| DBP>=95th percentile only | 150 (24.7) | 149 (24.6) | ||
|
| ||||
| Primary care visits in 6 months prior to index visit | ||||
| 0 | 361 (59.5) | 371 (61.1) | 0.68 | |
| 1 | 148 (24.4) | 148 (24.4) | ||
| 2 | 61 (10.1) | 49 (8.1) | ||
| 3 | 22 (3.6) | 27 (4.5) | ||
| 4+ | 15 (2.5) | 12 (2.0) | ||
|
| ||||
| Index visit type | ||||
| Well child | 263 (43.3) | 323 (53.2) | <0.001 | |
| Acute or follow-up | 344 (56.7) | 284 (46.8) | ||
|
| ||||
| Index visit department | ||||
| Family practice | 237 (39.0) | 202 (33.3) | 0.04 | |
| Pediatrics | 370 (61.0) | 405 (66.7) | ||
Other languages: Amharic, Arabic, Cantonese, French, Hindi, Hmong, Karen, Mandarin, Nepali, Oromo, Russian, Somali, Vietnamese, ASL, Other.
Recognition of Elevated Blood Pressure
Rooming staff and treating providers at TeenBP clinics were more likely to recognize a hypertensive BP. Compared to UC, the TeenBP CDS patients were more likely to have their incident hypertensive BP based on the average of two or more BPs measured at the index visit (47.1% versus 27.6%, p=0.007). The TeenBP CDS patients also were more likely to have elevated BP (ICD–9 796.2) diagnosed at their index visit (28.2% versus 4.2%, p<0.001). (Table 2). Results stratified by BMI and by visit type are shown in Tables 3 and 4.
Table 2.
Blood pressure repeat measurement, elevated blood pressure diagnosis, and follow-up blood pressure measurements at TeenBP intervention and usual care sites
| TeenBP Intervention (n=607) | Usual Care (n=607) | p | |
|---|---|---|---|
| Two or more BP measurements at index visit | 47.1 (35.0 – 59.5) |
27.6 (21.8 – 34.2) |
0.007 |
| Elevated BP diagnosis made at index visita | 28.2 (20.6 – 37.1) |
4.2 (2.5 – 7.0) |
<0.001 |
| Blood pressure re-measured within 30 days of index visit | 14.3 (11.4 – 17.8) |
10.6 (8.3 – 13.5) |
0.07 |
| Blood pressure re-measured within 90 days of index visit | 26.0 (21.7 – 30.7) |
23.4 (18.3 – 29.5) |
0.46 |
Adjusted, model-based percentages include covariates of study arm, age, sex, SBP percentile at index visit, index visit type (well-child or acute/follow-up visit), and a random intercept for clinic. Percentage and 95% confidence interval reported.
Based on an encounter diagnosis or problem list addition of elevated blood pressure (ICD-9 796.2)
Table 3.
Blood pressure repeat measurement, elevated blood pressure diagnosis, and follow-up blood pressure measurements at TeenBP intervention and usual care sites, stratified by BMI*
| TeenBP Intervention (n=534) | Usual Care (n=521) | p | |
|---|---|---|---|
|
| |||
| Two or more BP measurements at index visit | |||
| BMI<95th percentile | 49.9 | 25.2 | 0.003 |
| BMI ≥95th percentile | 47.0 | 37.2 | 0.31 |
|
| |||
| Elevated BP diagnosis made at index visita | |||
| BMI<95th percentile | 29.6 | 2.2 | <0.001 |
| BMI ≥95th percentile | 31.1 | 9.7 | <0.001 |
|
| |||
| Blood pressure re-measured within 30 days of index visit | |||
| BMI<95th percentile | 13.5 | 9.2 | 0.07 |
| BMI ≥95th percentile | 14.7 | 10.8 | 0.28 |
|
| |||
| Blood pressure re-measured within 90 days of index visit | |||
| BMI<95th percentile | 26.7 | 20.5 | 0.15 |
| BMI ≥95th percentile | 24.1 | 25.7 | 0.78 |
n=708 with BMI<95th percentile, n=347 with BMI≥95th percentile; excluding n=159 with missing BMI data at index visit
Adjusted, model-based percentages include covariates of study arm, age, sex, SBP percentile at index visit, index visit type (well-child or acute/follow-up visit), BMI, BMI by study arm interaction, and a random intercept for clinic.
Based on an encounter diagnosis of elevated blood pressure or a listing of elevated blood pressure in the problem list.
Table 4.
Blood pressure repeat measurement, elevated blood pressure diagnosis, and follow-up blood pressure measurements at TeenBP intervention and usual care sites, stratified by visit type*
| TeenBP Intervention | Usual Care | p | |
|---|---|---|---|
| (n=607) | (n=607) | ||
|
| |||
| Two or more BP measurements at index visit | |||
| Acute or follow-up visit | 43.1 | 23.8 | 0.007 |
| Well child visit | 51.3 | 31.9 | 0.01 |
|
| |||
| Elevated BP diagnosis made at index visita | |||
| Acute or follow-up visit | 25.7 | 3.4 | <0.001 |
| Well child visit | 31.0 | 5.1 | <0.001 |
|
| |||
| Blood pressure re-measured within 30 days of index visit | |||
| Acute or follow-up visit | 17.6 | 15.1 | 0.43 |
| Well child visit | 11.8 | 6.8 | 0.05 |
|
| |||
| Blood pressure re-measured within 90 days of index visit | |||
| Acute or follow-up visit | 32.0 | 30.0 | 0.67 |
| Well child visit | 20.5 | 17.5 | 0.44 |
n=628 with acute or follow-up visit, n=586 with well child visit;
Adjusted, model-based percentages include covariates of study arm, age, sex, SBP percentile at index visit, index visit type (well-child or acute/follow-up visit), BMI, BMI by study arm interaction, and a random intercept for clinic.
Based on an encounter diagnosis of elevated blood pressure or a listing of elevated blood pressure in the problem list.
BP measurements at follow-up
The primary outcome was return for repeat BP measurement within 30 days of the index or first hypertensive BP. At TeenBP CDS clinics 97 (16.0%) patients returned for repeat BP measurement at 30 days as compared to 66 (10.9%) at UC clinics. In a multivariate model adjusting for age, sex, SBP percentile, and visit type, rates for repeat BP measurement within 30 days were 14.3% (95% CI: 11.4–17.8) at TeenBP CDS clinics versus 10.6% (95% CI: 8.3–13.5) at UC clinics (p=0.07). By 90 days following the index hypertensive BP, 173 (28.5%) TeenBP CDS patients returned for BP measurement versus 136 (22.4%) of UC patients. Adjusted rates for return for BP measurement at 90 days were 26.0% for TeenBP CDS patients and 23.4% for UC patients; these differences were not significant. (Table 2)
Of 607 intervention patients, the best practice advisory and link to the TeenBP CDS (Figure 1) displayed for 290 (48%) where 2 or more BPs were recorded at that visit. Of these, for 67 (23%) the provider opened the CDS, with rates varying from 7–54% across the 10 intervention clinics.
Exploratory analyses
In exploratory analyses, we describe the subset of 173 TeenBP CDS and 136 UC patients who had a repeat BP recorded within 90 days of their index hypertensive BP. Most repeat BPs (89%) were measured at acute or follow-up visits. As compared to UC patients, TeenBP CDS patients were more likely to have their repeat BP recorded at a nursing visit (12.7% versus 3.7%). Most BPs measured at follow-up were normotensive. Overall, 23.6% of first follow-up BPs within 90 days had either SBP, DBP or both ≥95th percentile and rates did not differ significantly between CDS and UC patients.
Across the full study cohort, including both TeenBP CDS and UC patients, in multivariate analyses, predictors of repeat BP measurement within 30 days were older age group (aOR=1.67, 95% CI: 1.16–2.43), SBP >99th percentile (aOR=1.98, 95% CI: 1.26–3.11) and having the index elevated BP at an acute or follow-up visit (aOR=2.01, 95% CI: 1.41–2.87).
Discussion
Standards published in the Fourth Report and more recently updated in the Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents are the generally accepted guidelines for BP measurement and follow-up of elevated BP in children and adolescents. However, few data are available to assess how CDS linked within the EHR could improve adherence with these guidelines. In this pragmatic cluster randomized trial of over 1200 adolescents with an incident hypertensive BP measured during a primary care visit, we were able to show that adherence with recommended guidelines for follow-up was low, and even when follow-up occurred within 90 days, 76.4% had normal BP. The TeenBP intervention CDS was able to increase nurse and provider recognition that a BP was ≥95th percentile, as shown by increased rates for repeat BP measurement at the index visit (47.1% versus 27.6%) and provider diagnoses (28.2% versus 4.2%) at intervention versus UC sites. However, the novel EHR-linked CDS was not able to significantly increase return visits for further BP measurement.
Current guidelines recommending remeasurement of an incident hypertensive BP within 1–2 weeks suggest urgency for diagnosing hypertension in adolescents. While hypertension is important to identify because of its association with long term cardiovascular morbidity,16,17 in our study, and studies with other similar populations, incident hypertensive BPs were normal in most subjects on repeat measurement.3,4 Using data from the Cardiovascular Risk in Young Finns Study, it has been demonstrated that the accuracy for prediction of hypertension in adulthood was improved with two or more BP measurements during childhood or adolescence.18 The low rates for patient return for BP measurement at 30 or even 90 days following the index hypertensive BP may represent low clinician awareness of the recommended timing for follow-up BP measurement; or clinicians may disagree with clinical recommendations to remeasure mildly elevated BP.19 The recent U.S. Preventive Service Task Force conclusion that there is currently insufficient evidence to support routine hypertension screening in children and adolescents supports the apparent clinician feelings about remeasurement.20 Despite overall low follow-up rates, it was reassuring that most patients had normal BP at follow-up and subjects with a higher SBP, who would be more likely to have sustained hypertension and require further evaluation, had a higher rate of return for repeat BP measurement.
The TeenBP intervention led to increased provider awareness that a BP was elevated, a necessary first step towards increasing patient and family adherence to follow-up recommendations. This increased recognition is consistent with prior studies on EHR linked alerts for pediatric hypertension.21 An electronic alert such as that in TeenBP, delivered at the beginning of an office visit, can assist providers with visit planning and management of competing priorities13 that might interfere with addressing BP. However, even at CDS intervention sites, less than half of hypertensive BPs were recognized by providers. This may be due to a number of factors including: 1) at sick visits, isolated hypertensive BP readings may be attributed to pain or fever; 2) at preventive health visits, hypertensive BP readings may be attributed to patient anxiety regarding vaccines to be administered; 3) at all eligible visits, our classification of BP percentiles, consistent with guidelines,10 was based on the average of all BPs recorded at the visit. In contrast, clinicians may have based diagnoses and management on the second or last BP measurement recorded at the visit, both of which would tend to lower than the initial measurement.
Despite the increased recognition of a hypertensive BP at intervention sites, TeenBP did not significantly increase return for follow-up BP measurements. The low follow-up rates, along with low rates of hypertensive BP among patients who do return, suggest that perhaps clinical guidelines regarding elevated BP follow-up and optimal timing for this follow-up should be reconsidered. Recommended follow-up intervals after an elevated BP measure are based primarily on expert opinion9,10, rather than a well-developed evidence base. An alternative option is that follow-up after a first elevated BP should be targeted to youth at highest risk for sustained hypertension, such as those with a strong family history of hypertension or with an index BP >99th percentile +5mm Hg.
Some limitations to this study should be noted. First, our findings represent results from a real-world, pragmatic trial. As such, BP was measured with automated devices in busy clinical practices, as opposed to use of manual sphygmomanometers. Nevertheless, BPs were measured consistently across TeenBP and UC sites and, thus, the use of automated devices should not have had an impact on differences reported between groups. Second, by design, in order to minimize alert fatigue and reinforce the importance of remeasuring a hypertensive BP before clinical evaluation, TeenBP decision support only displayed if two or more BP measurements were recorded in the EHR at the index visit. This may have diluted the observed impact of the intervention, because our analyses were “intention-to-treat” and about half of those at intervention clinics with an initial elevated BP did not have a second BP measurement at that visit, and thus did not have the TeenBP decision support deployed. Third, the intervention sites received monthly feedback regarding their rate that an initial elevated BP was repeated. This feedback may have increased re-measurement rates beyond that attributable to the CDS alone. Finally, the TeenBP intervention was conducted at a single integrated care system and findings should be confirmed in other delivery sites and patient populations.
In summary, among patients age 10–17 years with a first hypertensive BP, the TeenBP CDS intervention significantly increased repeated BP measurement at the index visit and significantly increased provider recognition of elevated BP, relative to UC clinics. However, despite this positive effect, rates for follow-up BP measurement at 30 and 90 days were low and did not differ between the TeenBP intervention clinics and those following usual care protocols.
What’s new.
This project demonstrates how an electronic clinical decision support tool, used at the point of care, can increase clinical recognition of incident hypertensive blood pressures in adolescents. Despite increased recognition, blood pressure follow-up was low at intervention and usual care sites.
Acknowledgments
Funding Source: All phases of this study were supported the National Institute of Health (R01 HL115082 [to EOK]). The sponsor was not involved in the study design, data collection, analysis or interpretation of data, writing of the manuscript or the decision to submit for publication.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to disclose.
Clinical Trial Registration: NCT01760239
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS data brief. 2013;(133):1–8. [PubMed] [Google Scholar]
- 2.McNiece KL, Poffenbarger TS, Turner JL, Franco KD, Sorof JM, Portman RJ. Prevalence of hypertension and pre-hypertension among adolescents. The Journal of pediatrics. 2007;150(6):640–644. 644 e641. doi: 10.1016/j.jpeds.2007.01.052. [DOI] [PubMed] [Google Scholar]
- 3.Sinaiko AR, Gomez-Marin O, Prineas RJ. Prevalence of "significant" hypertension in junior high school-aged children: the Children and Adolescent Blood Pressure Program. The Journal of pediatrics. 1989;114(4 Pt 1):664–669. doi: 10.1016/s0022-3476(89)80718-8. [DOI] [PubMed] [Google Scholar]
- 4.Daley MF, Sinaiko AR, Reifler LM, et al. Patterns of care and persistence after incident elevated blood pressure. Pediatrics. 2013;132(2):e349–355. doi: 10.1542/peds.2012-2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lo JC, Sinaiko A, Chandra M, et al. Prehypertension and hypertension in community-based pediatric practice. Pediatrics. 2013;131(2):e415–424. doi: 10.1542/peds.2012-1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Juhola J, Magnussen CG, Viikari JS, et al. Tracking of serum lipid levels, blood pressure, and body mass index from childhood to adulthood: the Cardiovascular Risk in Young Finns Study. The Journal of pediatrics. 2011;159(4):584–590. doi: 10.1016/j.jpeds.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 7.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117(25):3171–3180. doi: 10.1161/CIRCULATIONAHA.107.730366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Toschke AM, Kohl L, Mansmann U, von Kries R. Meta-analysis of blood pressure tracking from childhood to adulthood and implications for the design of intervention trials. Acta Paediatr. 2010;99(1):24–29. doi: 10.1111/j.1651-2227.2009.01544.x. [DOI] [PubMed] [Google Scholar]
- 9.Beck A, Crain AL, Solberg LI, et al. Severity of depression and magnitude of productivity loss. Annals of family medicine. 2011;9(4):305–311. doi: 10.1370/afm.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl 4th Report):555–576. [PubMed] [Google Scholar]
- 11.Parker ED, Sinaiko AR, Daley MF, et al. Factors Associated With Adherence to Blood Pressure Measurement Recommendations at Pediatric Primary Care Visits, Minnesota and Colorado, 2007–2010. Preventing chronic disease. 2015;12:E118. doi: 10.5888/pcd12.140562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brady TM, Solomon BS, Neu AM, Siberry GK, Parekh RS. Patient-, provider-, and clinic-level predictors of unrecognized elevated blood pressure in children. Pediatrics. 2010;125(6):e1286–1293. doi: 10.1542/peds.2009-0555. [DOI] [PubMed] [Google Scholar]
- 13.Beacher DR, Chang SZ, Rosen JS, et al. Recognition of elevated blood pressure in an outpatient pediatric tertiary care setting. The Journal of pediatrics. 2015;166(5):1233–1239. e1231. doi: 10.1016/j.jpeds.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 14.Kharbanda EO, Nordin JD, Sinaiko AR, et al. TeenBP: Development and Piloting of an EHR-Linked Clinical Decision Support System to Improve Recognition of Hypertension in Adolescents. EGEMS (Wash DC) 2015;3(2):1142. doi: 10.13063/2327-9214.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.JO, JT, DL, et al. Improving Outcomes with Clinical Decision Support: An Implementer's Guide. 2. Chicago, IL: HIMSS; 2012. [Google Scholar]
- 16.Rademacher ER, Jacobs DR, Jr, Moran A, Steinberger J, Prineas RJ, Sinaiko A. Relation of blood pressure and body mass index during childhood to cardiovascular risk factor levels in young adults. Journal of hypertension. 2009;27(9):1766–1774. doi: 10.1097/HJH.0b013e32832e8cfa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Erlingsdottir A, Indridason OS, Thorvaldsson O, Edvardsson VO. Blood pressure in children and target-organ damage later in life. Pediatr Nephrol. 2010;25(2):323–328. doi: 10.1007/s00467-009-1350-3. [DOI] [PubMed] [Google Scholar]
- 18.Oikonen M, Nuotio J, Magnussen CG, et al. Repeated Blood Pressure Measurements in Childhood in Prediction of Hypertension in Adulthood. Hypertension. 2016;67(1):41–47. doi: 10.1161/HYPERTENSIONAHA.115.06395. [DOI] [PubMed] [Google Scholar]
- 19.Cabana MD, Rand CS, Powe NR, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA : the journal of the American Medical Association. 1999;282(15):1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 20.Moyer VA. Screening for primary hypertension in children and adolescents: U.S. Preventive Services Task Force recommendation statement. Pediatrics. 2013;132(5):907–914. doi: 10.1542/peds.2013-2864. [DOI] [PubMed] [Google Scholar]
- 21.Brady TM, Neu AM, Miller ER, 3rd, Appel LJ, Siberry GK, Solomon BS. Real-time electronic medical record alerts increase high blood pressure recognition in children. Clin Pediatr (Phila) 2015;54(7):667–675. doi: 10.1177/0009922814559379. [DOI] [PMC free article] [PubMed] [Google Scholar]