Abstract
Delayed ejaculation (DE) is a poorly defined and uncommon form of male sexual dysfunction, characterized by a marked delay in ejaculation or an inability to achieve ejaculation. It is often quite concerning to patients and their partners, and sometimes frustrates couples' attempts to conceive. This article aims to review the pathophysiology of DE and anejaculation (AE), to explore our current understanding of the diagnosis, and to present the treatment options for this condition. Electronic databases were searched from 1966 to October 2017, including PubMed (MEDLINE) and Embase. We combined “delayed ejaculation,” “retarded ejaculation,” “inhibited ejaculation,” or “anejaculation” as Medical Subject Headings (MeSH) terms or keywords with “epidemiology,” “etiology,” “pathophysiology,” “clinical assessment,” “diagnosis,” or “treatment.” Relevant sexual medicine textbooks were searched as well. The literature suggests that the pathophysiology of DE/AE is multifactorial, including both organic and psychosocial factors. Despite the many publications on this condition, the exact pathogenesis is not yet known. There is currently no single gold standard for diagnosing DE/AE, as operationalized criteria do not exist. The history is the key to the diagnosis. Treatment should be cause-specific. There are many approaches to treatment planning, including various psychological interventions, pharmacotherapy, and specific treatments for infertile men. An approved form of drug therapy does not exist. A number of approaches can be employed for infertile men, including the collection of nocturnal emissions, prostatic massage, prostatic urethra catheterization, penile vibratory stimulation, probe electroejaculation, sperm retrieval by aspiration from either the vas deferens or the epididymis, and testicular sperm extraction.
Keywords: Anejaculation, Delayed ejaculation, Diagnosis, Physiopathology, Therapy
INTRODUCTION
The term delayed ejaculation (DE) (also called retarded ejaculation, inhibited ejaculation (IE), inadequate ejaculation, idiopathic anejaculation (AE), primary impotentia ejaculationis, or psychogenic AE) has been used to describe “a marked delay in or inability to achieve ejaculation” [1,2]. The term IE includes DE and AE. Segraves [3] criticized these terms as pejorative and is responsible for our current adoption of the term “delayed ejaculation.” The “difficulty” experienced in ejaculating may range from varying delays in latency to AE. Despite the confusion in terminology, men diagnosed with DE experience difficulties in ejaculation and orgasm. Sometimes both may occur during self-masturbation or manual, oral, vaginal, or anal stimulation by the partner. In the Diagnostic and Statistical Manual of Mental Disorders (DSM), fifth edition, the definition of DE requires 1 of 2 symptoms: either a marked delay in or a marked infrequency or absence of ejaculation on 75% to 100% of occasions for at least 6 months of partnered sexual activity without the individual desiring delay, and causing significant distress to the individual [4].
In that document, the terminology DE is meant to describe any and all of the ejaculatory disorders that result in a delay or absence of ejaculation. Ejaculatory latency is defined as the time it takes for a man to achieve ejaculation. For research purposes, this is often defined as the intravaginal ejaculation latency time (IELT), which is the time taken by a man to ejaculate during vaginal penetration. The Third International Consultation on Sexual Medicine defined DE as an IELT threshold beyond 20 to 25 minutes of sexual activity, as well as negative personal consequences such as bother or distress [5]. The 20- to 25-minute IELT criterion was chosen primarily because it represents a threshold of more than 2 standard deviations above the mean found in population-based studies of IELT. However. Perelman [6,7] criticized this time frame for ignoring 2 important findings: a) most men seeking help for DE pursue treatment because of its impact on coitus, and b) most men's IELT range is approximately 4 to 10 minutes [8,9,10]. Any bilateral deviation from the ~4- to 10-minute IELT range of the majority of men should meet the qualification for the temporal diagnostic criterion. Accordingly, Perelman [7] suggested the following definition for coital DE: a) inability/incapacity to choose to ejaculate intravaginally in less than ~10 minutes in all, or nearly all, coital encounters; b) not having the ability/capacity to choose to ejaculate sooner, but desiring the ability to do so; and c) experiencing negative personal consequences, such as distress, bother, frustration, and/or the avoidance of sexual intimacy. There seems to be a general agreement that low rates of DE are reported in the literature, and it appears to be the least common form of male sexual dysfunction. The prevalence rate of DE among the general population ranges from 1% of sexually active men (lifelong DE) to 5% (acquired DE) [11,12,13,14,15,16,17].
Some previous studies were carried out according to the DSM-III [16] and International Classification of Diseases, 10th edition [17] diagnostic criteria. The lack of an internationally accepted universal definition, combined with the absence of consensus about normative data for defining the duration of “normal” ejaculatory latency and the lack of a distinction between various types of delayed ejaculatory disorders (e.g., delayed vs. absent) among epidemiologic studies, limits our knowledge regarding the true prevalence of DE. Nonetheless, DE appears to be positively related to age [18,19,20], and its prevalence differs among races [17]. While some women enjoy the prolonged IELT, others may experience pain, question their own attractiveness, or suspect the partner's infidelity [21]. Although clinical advances have been made in the diagnosis and treatment of erectile dysfunction, there is a consensus that DE/AE is still a poorly understood disorder, with inconsistent practice patterns seen among practicing physicians [22]. This article aims to review the pathophysiology of DE/AE, to explore our current understanding of the diagnosis, and to present the treatment options for this condition.
ETIOLOGY AND PATHOPHYSIOLOGY
Ejaculation involves emission, bladder neck closure, and expulsion (ejaculation proper). In emission, seminal fluid is delivered to the posterior urethra. Sympathetic innervation (T10~L2) controls the emission, as well as contraction of the bladder neck to prevent retrograde ejaculation. During expulsion, the bulbocavernosus muscle, synchronized with the pelvic floor muscles, contracts to expel semen in an antegrade fashion through the anterior urethra. Somatic innervations (S2~S4) mediate this process. Generally, this reflex is controlled by both sympathetic and somatic neural inputs, as well as sensory inputs. Many neurotransmitters such as serotonin, dopamine, and norepinephrine play roles in ejaculatory physiology. Orgasm is a purely cerebral experience that usually, but not always, coincides with ejaculation. For many years, different views have existed regarding the etiology of DE/AE (Table 1). On one hand, it was argued that DE may be caused by psychosexual, psychosocial, or relationship problems. On the other hand, it has been argued that DE is caused by genetic, neurobiological, endocrine, anatomic, and infectious factors, or may be drug-induced. Many of these etiologic factors are not supported by good evidence-based data, but rather are based on case reports and case series. These etiological factors—organic and psychogenic etiologies—are neither independent nor mutually exclusive and may well interact with each other, and their pathological effects may vary between individuals [1,2,13].
Table 1. Etiological factors that may be involved in the pathophysiology of delayed ejaculation and anejaculation.
| I. Psychosexual and psychosocial factors | II. Organic and biological factors |
|---|---|
| a. Fears: | Aging |
| - Fear of pregnancy and fertility issues | |
| - Fear of castration and death | |
| - Fear of annihilation associated with loss of semen | |
| - Fear of loss of control | |
| - Fear of exposure and subsequent shame concerning the problem | |
| - Fears of abandonment/rejection | |
| - Fears of intimacy and loss of autonomy | |
| - Fears of hurting/defiling the partner | |
| - Fear of retaliation by the female or by other males | |
| - Success phobia | |
| b. Sexual orientation conflicts | Genetic factors (see Table 2) |
| c. Hostility and resentment | Neurobiological factors |
| d. Obsessive-compulsive personality traits | Congenital anatomical factors: |
| • Müllerian duct cyst | |
| • Wolffian duct abnormalities | |
| • Prune belly syndrome | |
| • Posterior urethral valves | |
| • Complete male epispadias | |
| • Bladder exstrophy | |
| • Sacral Tarlov cyst | |
| • Imperforate anus | |
| • Seminal megavesicle | |
| e. Performance anxiety | Neurogenic causes: |
| • Diabetic autonomic neuropathy | |
| • Multiple sclerosis | |
| • Spinal cord injury | |
| • Radical prostatectomy | |
| • Pelvic radiation therapy | |
| • Proctocolectomy | |
| • Bilateral sympathectomy | |
| • Abdominal aortic aneurysmectomy | |
| • Para-aortic lymphadenectomy. | |
| • Pelvic fracture-urethral distraction defect injury | |
| • Adult circumcision | |
| f. Lack of self-assertion | Infection/inflammation: |
| - Urethritis | |
| - Genitourinary tuberculosis | |
| - Schistosomiasis | |
| - Prostatitis | |
| - Orchitis | |
| - Orchialgia in testis cancer survivors | |
| g. An unwillingness to give of oneself in love | Endocrine: |
| - Hypogonadism | |
| - Hypothyroidism | |
| - Hyperprolactinemia | |
| h. Strong religious convictions, leading to guilt | Medications (Table 3) |
| i. Autosexual orientation: | |
| - Positive reinforcement associated with self-masturbation | |
| j. Unusual masturbation techniques: | |
| - High-frequency masturbation | |
| - Idiosyncratic and vigorous masturbation style | |
| - Disparity between the reality of sex with a partner and preferred sexual fantasy during masturbation | |
| k. Relationship factors: | |
| - Disparity between fantasy and partner | |
| - Partner sexual dysfunction | |
| l. Diminished sexual desire | |
| m. Insufficient sexual arousal and female sexual dysfunction | |
| n. Depression and other psychiatric diseases |
1. Psychogenic factors
Multiple proposed psychogenic factors may contribute to the pathogenesis of DE (Table 1). Althof [23] summarized these proposed psychogenic factors into 4 theories based on empirical support:
1) Insufficient sexual stimulation (mental and physical). This theory was proposed by Masters and Johnson [24] and Bancroft [25]. This theory perceives DE as being due to insufficient penile or mental stimulation, often associated with aging or diminished penile sensation. The main predictions of this theory were supported by findings from multiple studies [26,27,28]. Rowland et al [26] reported that men with DE had no apparent somatic etiology and experienced less sexual arousal than normal men. Teloken et al [27] performed an analysis of data from 206 patients who presented with secondary delayed orgasm/anorgasmia and noted abnormal penile sensation in 7%. Additionally, Xia et al [28] noted that patients with primary DE appeared to have penile shaft, rather than glans, hyposensitivity and hypoexcitability. Furthermore, Nelson et al [29] confirmed that penile vibratory stimulation (PVS) could adequately treat 72% of patients with secondary DE and orgasm, indicating that PVS may initiate the normal ejaculatory reflex.;
2) Unusual masturbation patterns and fantasy life. This theory stated that some men with DE tend to prefer unusual methods of masturbation over heterosexual intercourse with their partner. Perelman and Rowland [14] and Perelman [30] identified 3 factors that disproportionately characterized patients with DE: a) high-frequency masturbation (age-dependent mean of greater than 3 times per week), b) idiosyncratic masturbatory style (masturbation technique not easily duplicated by the partner's hand, mouth, or vagina), and c) disparity between the reality of sex with a partner and their preferred masturbatory fantasy.;
3) The concept of the third psychological theory was posited by Apfelbaum [31,32]. It conceptualizes DE as a subtle and disguised sexual desire disorder masquerading as DE. According to this concept, these patients mainly prefer solo masturbation, rather than partnered sex.;
And 4) the fourth theory considers DE as an outgrowth of a psychic conflict, making it psychodynamic in origin. The following conflicts have been reported: a) different types of fear (see Table 1); b) hostility toward one's partner; c) unwillingness to give oneself; and d) guilt from a strict religious upbringing [23].
2. Organic factors
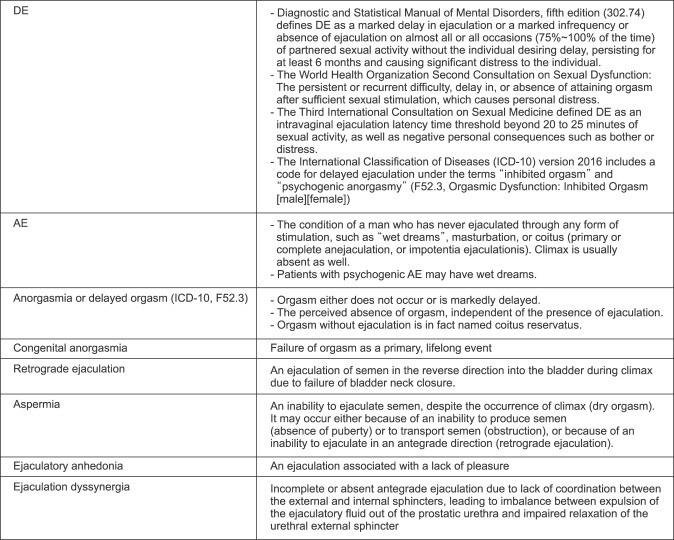
Any congenital abnormality, medical disease, surgical procedure, or drug that interferes with either central control of ejaculation or the peripheral control that includes sympathetic nerve supply to the vas deferens, bladder neck, prostate or seminal vesicles, as well as the somatic efferent nerve supply to the pelvic floor, can result in DE/AE and anorgasmia [5]. Many reports on DE/AE have been published, but several terminological discrepancies have caused controversy (Fig. 1). Several studies have reported that that DE/AE may be caused by several factors, including aging-related, congenital, genetic, neurogenic, infection/inflammation, endocrine, and pharmacologic causes (Table 1, 2, 3).
Fig. 1. Terminology and definitions of delayed ejaculation (DE)/anejaculation (AE) and the related terms.
Table 2. Summary of genetic polymorphisms that may have potential roles in DE/AE, especially SSRI-induced DE.
| Gene (Reference No) | Polymorphism or alleles | Diagnosis | Drug(s) | Measurement and type of sexual dysfunction | Main result |
|---|---|---|---|---|---|
| CYP 2D6 [51] | CYP2D6*1 | Depressive disorders | Paroxetine | - ASEX | DE was reported by poor metabolizers. |
| CYP2D6*3 | - Different types | ||||
| CYP2D6*4 | - Men (n=9)/women | ||||
| CYP2D6*5 | |||||
| CYP2D6*6 | |||||
| CYP 2D6 [53] | CYP2D6*1 | Depressive disorders, anxiety disorder | Paroxetine | - ASEX | Negative results in men |
| CYP2D6*3 | - Different types | ||||
| CYP2D6*4 | - Men (n=20)/women | ||||
| CYP2D6*5 | |||||
| CYP2D6*6 | |||||
| - 5HT2A receptor [52] | - 5HT2A | Depressive disorders | SSRIs | - Different types | - 5HT2A |
| - 1438 G/A (rs6311) | - Men (n=20)/women | - 1438 GG genotype was a significant predictor of lower arousal scores. | |||
| - GNB3 gene [52] | GNB3 825 C/T (rs5443) | Depressive disorders | SSRIs | - Different types | No significant relationship |
| - Men (N=20) /women | |||||
| SLC6A4 [55] | 5HTTLPR | Men and women with depression | Escitalopram or nortriptyline | Antidepressant side-effects, SFQ | HTTLPR was not associated with sexual dysfunction. |
| 68 candidate genes [54] | 68 candidate genes related to dopamine, serotonin, adrenergic receptors, glutamate, and neurotrophins as well as other signaling pathways and second-messenger genes | Caucasian men and women with major depressive disorder | Citalopram | PRISE | GRIA1 was associated with difficulty achieving orgasm. |
| HTR2A [56] | HTR2A -1438A>G (rs6311) | Han Chinese men with major depressive disorder | SSRI or venlafaxine (SNRI) | ASEX | HTR2A -1438 A/A genotype was associated with sexual dysfunction. |
| Many genes [59] | Genome-wide study examining ~186,000 SNPs | Japanese men and women with major depression | Paroxetine, fluvoxamine, milnacipran (SNRI) | - Clinician's assessment | GRIA3, GRIA1, GRIN3A, and GRIK2 were not associated with sexual dysfunction, including DE |
| - Different types | - SNPs in MDGA2 were associated with sexual dysfunction. | ||||
| - Men (n=106)/women | |||||
| ABCB1 [57] | rs1045642 | Depressive and anxiety disorders | Citalopram, paroxetine, venlafaxine, fluvoxamine, and sertrailine | - The ASEC-12 | No genetic association with sexual dysfunction |
| rs2032582 | - Different types | ||||
| rs1128503 | - Men (n=133)/women | ||||
| rs2235015 | |||||
| rs2235040 | |||||
| rs2032583 | |||||
| Many genes [58] | Genome-wide study examining ~34 SNPs | Major depressive disorder | Bupropion, buspirone, sertraline, venlafaxine, citalopram | - PRISE | 10 SNPs in SACM1L mediated the effects of bupropion on sexual side-effects. |
| - Different types | |||||
| - 1,439 enrolled (one-third were men.) | |||||
| Many genes [60] | Genome-wide study examining 421,789 SNPs | Major depressive disorder | Citalopram | - PRISE | All tested genes were not associated with citalopram-induced sexual dysfunction. |
| - Different types | |||||
| - 1,762 enrolled (number of men was not mentioned.) | |||||
| SLC6A4 [61] | 5HTTLPR | Idiopathic anejaculation | - | - Clinician's assessment and IIEF-5 | S and STin2.10 alleles were common in three patients with anejaculation. |
| - Anejaculation | |||||
| - 3 men | |||||
| Serotonin receptor subtypes 1A, 1B, and 2C genes [47] | rs6295 | Population-based sample of 1,399 male twins | - | - Self-reported IELT | rs11568817 in the gene encoding the 5-HT1B receptor showed an association with IELT indicating that individuals homozygous for the G allele had shorter IELTs, conferring protection against DE. |
| rs11568817 | |||||
| rs130058 | |||||
| rs13212041 | |||||
| rs6318 | |||||
| rs3813929 | |||||
| Oxytocin and vasopressin receptor genes [48] | 19 SNPs | Population-based sample of 1,517 men | - | - IELT, number of thrusts, anteportal ejaculation, and feeling of control. | A significant association was found with the rs75775 SNP in the oxytocin receptor gene, indicating that the heterozygote had an elevated risk of shorter IELTs, conferring protection against DE. |
DE: delayed ejaculation, AE: anejaculation, SSRIs: selective serotonin re-uptake inhibitors, CYP: cytochrome P450, ASEX: Arizona Sexual Experiences Scale, 5HT: serotonin, 5-HT2A: subtype of the 5-HT2 receptor, GNB3: guanine nucleotide-binding protein G subunit beta-3, SLC6: solute carrier family 6, 5-HTTLPR: serotonin-transporter-linked polymorphic region, SFQ: Social Functioning Questionnaire, PRISE: Patient-Rated Inventory of Side Effects, GRIA: glutamate receptor, ABCB1: gene encoding P-glycoprotein, ASEC-12: Antidepressant Side Effect Checklist, SNP: single-nucleotide polymorphism, SACM1L: SAC1 like phosphatidylinositide phosphatase, IIEF: International Index of Erectile Function, IELT: intravaginal ejaculation latency time.
Table 3. Medications that may delay ejaculation.
| Drug | Possible mechanism | |
|---|---|---|
| 1 | SSRIs | - Activation of a particular serotonin receptor subtype: 5HT2 receptors |
| Citalopram | - Anticholinergic actions | |
| Escitalopram | - Blockade of α-1 noradrenergic receptors | |
| Fluvoxamine | - Antihistaminergic actions | |
| Fluoxetine | - Antidopaminergic actions | |
| Paroxetine | - Elevated prolactin | |
| Sertraline | - Inhibitory effects on nitric oxide synthase | |
| 2 | Other antidepressants | - Activation of a particular serotonin receptor subtype: 5HT2 receptors |
| Amitriptyline | - Anticholinergic actions | |
| Amoxapine | - Blockade of α-1 noradrenergic receptors | |
| Clomipramine | - Antihistaminergic actions | |
| Desipramine | - Antidopaminergic actions | |
| Desmethylimipramine | - Elevated prolactin | |
| Duloxetine | - Inhibitory action on nitric oxide synthase | |
| Imipramine | ||
| Mirtazapine | ||
| Nortriptyline | ||
| Protriptyline | ||
| Trazodone | ||
| Venlafaxine | ||
| 3 | Monoamine oxidase inhibitors | - Activation of serotonergic neurotransmission |
| Isocarboxazid | - Blockade of α-1 noradrenergic receptors | |
| Pargyline | - Decreased dopamine activity | |
| Phenelzine | ||
| Tranylcypromine | ||
| 4 | Anxiolytics | - Increased central serotonergic activity |
| Alprazolam | - Stimulate muscle relaxation | |
| Chlordiazepoxide | - Sedative effect | |
| 5 | Neuroleptics | - Inhibits dopamine activity |
| Mesoridazine | - Increases the level of prolactin | |
| - Blocks peripheral cholinergic and alpha-adrenergic receptors | ||
| 6 | Diuretics | - Direct effects on vascular smooth muscle cells |
| Thiazide | - Reduces the response to catecholamines | |
| 7 | Anti-inflammatory drug | - Blocks the enzyme cyclooxygenase, leading to inhibition of smooth muscle contraction in the vas deferens and seminal vesicles |
| Naproxen | ||
| 8 | α1-blockers | - Inhibition of α1-adrenergic receptor subtypes |
| Alfuzosin | - Inhibition of smooth muscle contraction in the vas deferens and seminal vesicles. | |
| Doxazosin | ||
| Silodosin | ||
| Tamsulosin | ||
| Terazosin | ||
| 9 | GABA transaminase inhibitors | - Inhibition of GABA transaminase, leading to increased brain concentrations of GABA (inhibitory) |
| Aminocaproic acid | ||
| 10 | Antihypertensives | - Reduction of central sympathetic outflow |
| Bethanidine | - α-1 and β-adrenergic blocking properties | |
| Guanadrel | - Produce sedation or depression | |
| Guanethidine | - Interfere with corporal smooth muscle constriction | |
| Labetalol | - Increased levels of prolactin | |
| Methyldopa | ||
| Prazosin | ||
| Phenoxybenzamine | ||
| Reserpine | ||
| 11. | Antipsychotics | - α-blocking properties and possibly also calcium channel blocking |
| Chlorpromazine | - Postsynaptic dopamine antagonism, leading to inhibition of motivation and increased prolactin | |
| Haloperidol | - Agonistic serotonergic effects | |
| Perphenazine | - Histamine receptor antagonism | |
| Thioridazine | - Blockage of acetylcholine receptors | |
| Butaperazine | ||
| Chlorprothixene | ||
| 12. | Opiates | - Blockade of presynaptic opioid receptors involved in the ejaculatory circuit. |
| Methadone | - Inhibit LH and T. | |
| Tramadol | - Inhibit thyroid-stimulating hormone. | |
| 13. | Antiepileptics | - Inhibition of calcium currents appears to lead to reduced neurotransmitter release and attenuation of postsynaptic excitability |
| Carbamazepine | - Increases the level of sex hormone-binding globulin, leading to reduction of free or bioavailable testosterone | |
| Gabapentin | ||
| Pregabalin | ||
| 14. | Muscle relaxants | - Inhibitory effect on GABAB receptors at the lumbosacral spinal cord level |
| Baclofen | - Inhibition of motor efferent nerves | |
| 15. | 5-α reductase inhibitors | - Deleterious effect on the biosynthesis and function of neurosteroids in the central nervous system, blocking neurogenesis |
| Dutasteride | - Accumulation of cholesterol in neurons, leading to neurodegeneration | |
| Finasteride | ||
| 16. | Ganglionic blocker | - Blocks nicotinic receptors at sympathetic ganglia. |
| Hexamethonium | ||
| 17. | Alcohol | - Sedative effects |
| - Increases in prolactin | ||
| - Increases estrogen | ||
| - Decreases in 5-α-reductase | ||
| - Localized gonadal tissue damage | ||
GABA: gamma-aminobutyric acid, LH: luteinizing hormone, T: testosterone.
1) Aging
An age-dependent increase in the prevalence of DE was reported in various studies [33,34,35]. This finding may be related to decreased penile sensitivity with age, which has been attributed to possible ultrastructural or degenerative age-related changes in the penile receptors [36,37,38], leading to progressive axonal sensory loss [39,40]. Other factors include age-related comorbidities, such as depression, diabetes, or late-onset hypogonadism [19], or medical, surgical, or radiation therapy for a number of age-related diseases that can affect ejaculatory function [41,42]. Additionally, some researchers have hypothesized that DE is caused, at least in part, by slower bulbocavernous reflexes and reduced spinal stimulation associated with aging [43,44]. Despite these age-related changes, Paduch et al [15] failed to show a significant correlation between DE and age (odds ratio=0.67; 95% confidence interval, 0.39~1.16; p=0.149) in a prospective observational study of 988 subjects.
3. Genetic factors
DE is marked by etiological complexity (it is multifactorial and many cases are idiopathic), and a range of severity from DE to AE [1,5,45]. In addition, ejaculatory latency is greatly variable [8,10]. These findings have led to the hypothesis that genetic factors can affect a person's predisposition to DE/AE. Unfortunately, a Finnish twin study showed that genetics influenced premature ejaculation (PE), but not DE [46]. In contrast, Jern et al [47] documented that the single-nucleotide polymorphism (SNP) rs11568817 in the gene encoding the 5-HT1B receptor showed an association with IELT, indicating that individuals homozygous for the G allele had a shorter IELT, conferring protection against DE. In another study, Jern et al [48] noted that a SNP for the oxytocin receptor gene OXTR (rs75775) was associated with differences in self-reported IELT and perceived ejaculatory control suggesting that heterozygotes had an elevated risk of a shorter IELT, conferring protection against DE (Table 2). These results suggest that this topic may warrant further investigation.
Patients who receive serotonergic antidepressants frequently report sexual dysfunction. A very high elevated risk (7-fold) for DE/AE was observed in selective serotonin reuptake inhibitor (SSRI) users [49]. The significant heterogeneity in the occurrence and the presentation of SSRI-related sexual dysfunction may suggest underlying genetic factors [50]. Several studies have applied genomic techniques to identify candidate genes and potential genetic risk factors for SSRI-induced DE/AE, utilizing either the candidate gene approach (genotyping of a limited number of genes) [51,52,53,54,55,56,57,58] or the genome-wide association approach (genotyping of hundreds of thousands of polymorphisms) [59,60,61]. Table 2 summarizes the results of these studies. No group of polymorphisms has been consistently demonstrated to explain a relevant proportion of the variance in SSRI-induced DE/AE. These findings require replication before firm conclusions can be drawn.
4. Neurobiological factors
Waldinger et al [62] and Waldinger and Schweitzer [63] introduced a dynamic neurobiological theory of PE and DE. According to this “ejaculation distribution theory,” lifelong DE, as well as PE, is considered to be part of a normal biological variability in IELT. It is postulated that any random sample of men is likely to include a minority of men with (nearly) always early ejaculation, and a second minority who (nearly) always suffer from DE, while the majority have a “normal” or “average” IELT. The finding of significant variability in IELT values among the general population—from 0.55 to 44.1 minutes—supports this theory [8,10]. Men with a genetically determined higher ejaculatory threshold set point could sustain more prolonged and intense sexual stimulation and could exert more control over ejaculation [64]. Accordingly, life-long (primary) DE with a very high set point, like lifelong PE, is considered to be primarily a neurobiological variant. Presumably, affected individuals suffer from a susceptibility that interacts with a variety of psychosocial, environmental, cultural, and medical risk factors to result in DE [6]
5. Other organic causes
The list of organic causes possibly leading to DE/AE is extensive and is outlined in Table 1, 2, 3. A full discussion of each factor is beyond the scope of this review. New etiologies continue to be added to the list of causes. “Difficulty” in ejaculating has been reported in patients with congenital abnormalities that may compromise the functions of the vas deferens, ejaculatory duct, prostate, seminal vesicle, and urethra [65,66,67,68].
The neurological mechanisms that lead to DE/AE are damage to the sympathetic ganglia and/or injury of post-ganglionic sympathetic nerve fibers to the organs of emission, mainly as a result of a neuro-logic disease, trauma, or pelvic surgery (Table 1). Additionally, DE/AE is common in patients with pelvic cancer treated with radiation therapy. DE was reported by 40% of 109 prostate cancer patients who received a radiation dose of 78 Gy (Gray, 1 Gy=100 rad), while AE was reported by 11% of patients [69]. The prevalence of ejaculatory dysfunction appears to increase as time elapses after radiation therapy. In a previous study, the proportion of patients experiencing AE 1, 3, and 5 years after radiation therapy was 16%, 69%, and 89%, respectively [70]. In these circumstances, DE/AE may be associated with decreased sensitivity in the penis [69]. However, the influence of these neurological factors on ejaculation is due to more than just neurological reasons, as the accessory sexual glands and pathway for semen are removed or injured during radical pelvic surgery. Moreover, sexual dysfunction is a multidimensional construct of numerous bio-psychosocial factors that can be influenced by surgery in a variety of ways, including impacts to a patient's cosmetic appearance, psychological state, preoperative radiation, stoma formation in rectal cancer, surgical complications, and increased age.
While DE/AE occurs in up to 17.9% of multiple sclerosis patients [71], the majority of patients with spinal cord injury (SCI) (52%) cannot ejaculate during sexual intercourse [72]. Even though diabetes mellitus is considered to be a known cause of DE/AE, the true incidence of these conditions in individuals with diabetes is unclear. In a population-based study [73] inability to reach orgasm with masturbation was slightly more prevalent (21.1%) in diabetic subjects than in those without diabetes (14.9%). The most common causes of AE are retroperitoneal lymph node dissection and SCI, which jointly account for almost 90% of cases [74].
Erectile dysfunction, PE, and painful ejaculation are the leading sexual symptoms of urogenital infections. However, there is no definitive evidence of the actual frequency of DE/AE in patients with urogenital infections or of the true pathophysiological role of these inflammatory disorders in ejaculatory delay [75]. Urogenital infections can produce scarring and obstruction anywhere in the male reproductive tract. Disorders affecting levels of testosterone (T), prolactin, and thyroid hormone have also been associated with DE/AE. T appears to play a facilitatory role in the control of the ejaculatory reflex [76], but estimated ejaculation times during vaginal intercourse and/or masturbation were not associated with serum T levels in a recent study [77]. Once again, there is weak evidence of an association between hyperprolactinemia and DE [78]. In contrast, hypothyroidism was strongly associated with longer IELT (DE), while shorter IELT (PE) was linked to hyperthyroidism [35,79].
Complaints of DE/AE in patients taking medications are not uncommon. Different medications may interfere with either central or peripheral control of ejaculation, potentially affecting the IELT (Table 3). Pharmacological agents that have been associated with DE/AE include tricyclic antidepressants, SSRIs, monoamine oxidase inhibitors, neuroleptics, diuretics, narcotics, alpha 1-blockers, antiepileptics, 5-alpha reductase inhibitors, alcohol, and others [41,80]. The literature suggests that DE/AE is the most commonly reported sexual dysfunction associated with antidepressant use; other frequently reported problems include delayed and/or absent orgasm, reduced and/or absent sexual desire, and erectile dysfunction.
DIAGNOSIS
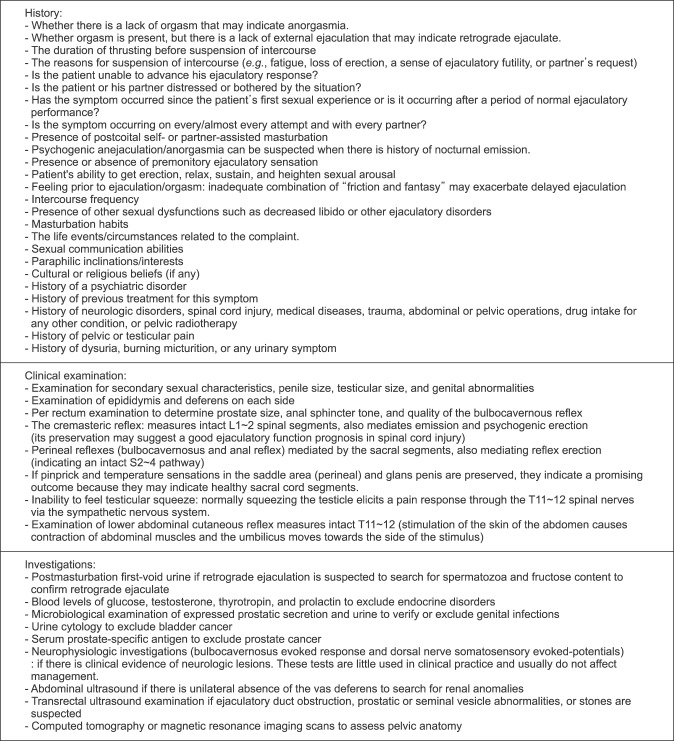
Unfortunately, there is currently no single gold standard for diagnosing DE/AE, as operationalized criteria do not exist [3,7,22]. Because many organic and psychological factors may be involved in the pathogenesis of DE/AE, a careful clinical history and appropriate physical examination should focus on all related symptoms and signs. A list of an assessment steps that might be helpful in the evaluation of the patient is presented in Fig. 2. The history is the key to the diagnosis of DE/AE. Evaluation begins by exclusion of retrograde ejaculation, absence of puberty, genital tract obstruction, anorgasmia, and other sexual dysfunctions that may be misdiagnosed as DE/AE, such as erectile dysfunction, a subtly decreased libido, ejaculatory pain, the partner's sexual dysfunction, sexual orientation conflicts, or paraphilic inclinations/interests. It is important in the history to ascertain whether the complaint concerns DE/AE, the sensation of orgasm, or both. Ejaculation occurs in the genitals, whereas orgasm is a central sensory event with significant subjective variation. Ejaculation and orgasm usually occur together, but not always. The sensation of orgasm in the absence of antegrade ejaculation suggests retrograde ejaculation, absence of puberty, or genital tract obstruction. The second step is to confirm the presence of DE/AE by asking about the duration of thrusting before suspension of intercourse, the ability to advance the ejaculatory response, and the level of distress or bother caused by this situation. The evaluation may involve determining whether DE is lifelong or acquired and global or situational. In the generalized form (lifelong or acquired), the history may reveal whether the patient is experiencing substantial delay or absence of ejaculation/orgasm in all circumstances. In a considerable number of cases of DE/AE, the patient is typically unable to ejaculate in the presence of a partner (especially during coitus) but is able to orgasm and ejaculate during solo masturbation. If a man is only able to ejaculate through masturbation, it is important to assess whether he has an idiosyncratic masturbatory style [7,21]. Men with DE/AE have demonstrated high levels of relationship distress, sexual dissatisfaction, anxiety about their sexual performance, and lower frequencies of coital activity than sexually functional men [21,28,81]. The third step is to uncover the predisposing issues and the potential risk factors that are believed to participate in the pathogenesis of DE/AE. A focused clinical examination, questionnaires (such as Male Sexual Health Questionnaire, International Index of Erectile Function, and others), laboratory tests, and radiologic imaging may help diagnose these potential risk factors (Table 1, 2, Fig. 2).
Fig. 2. Relevant aspects of history-taking, physical examination, and investigations.
Physicians need to carefully balance the risk of missing serious causes with the wise use of often scarce and costly investigative resources, especially in developing countries. Sometimes the diagnosis of the risk factor(s) unfolds over time and across several episodes of care. In addition, the etiologic diagnostic process can also extend across multiple specialties and in different locations.
TREATMENT
Defining firm recommendations to approach the treatment of DE/AE is difficult for a condition that is less common and heterogeneous, for which the literature is confined to case reports, case series, and small studies. There are many approaches to treatment planning. A rigid treatment plan is not suitable for all patients. Factors that affect the choice of treatment strategies may include:
1) Clinical judgment regarding the etiology of DE/AE and making sound decisions. This implies the active involvement of other specialties in the management of the condition.;
2) The physician's experience, such as training in communication skills and the management of sexual problems. These factors have been shown to affect professional behavior [82].;
3) The medical, anatomical, pharmacologic, and surgical risks associated with DE/AE. In these cases, treatment should be cause-specific. Neurogenic AE is usually irreversible, and thus the patient might be counseled to seek alternative methods to improve patient and partner satisfaction. A positive cremasteric reflex in patients with SCI suggests intact emission, and patients should be encouraged to attempt ejaculation or to explore possible retrograde ejaculation [83]. In a recent randomized controlled trial [84], a 2% replacement T solution was not associated with significant improvement in DE/AE in androgen-deficient men, suggesting that androgen deficiency is not the sole contributor to ejaculatory dysfunction. In contrast, a pharmaceutical company-sponsored multicenter randomized, double-blind controlled trial [85] showed improvement of ejaculatory function in hypogonadal men receiving a 2% T solution. Unfortunately, in the latter study, ejaculatory dysfunction was not one of the inclusion criteria. Autonomic and somatic nerve preservation is indispensable to minimize postoperative sexual sequelae regardless of the surgical approach (posterior, lateral, anterior, or perineal dissection). When the hypogastric and homolateral pelvic plexuses are preserved unilaterally, ejaculation is preserved in 25% to 47% of cases, but when the pelvic plexus is preserved partially but the hypogastric nerve is not, ejaculation is maintained in 0% of patients. In contrast, when the pelvic autonomic nerves are completely preserved, ejaculation is preserved in 55% to 83% of patients [86,87].;
4) The presence of co-occurring mental disorders, sexual orientation conflicts, unusual masturbation techniques, strong religious convictions, hostility, fears, relationship factors, or paraphilic inclinations/interests must be assessed because these factors may narrow the scope of possible treatment strategies and help the physician identify whether psychiatric care is needed.;
5) Consultation with a gynecologist may have a significant impact on cases associated with the partner's sexual dysfunction or other gynecological disorders, as DE/AE may be triggered by the fear of hurting the partner or a decrease in the perceived attractiveness of the partner, if she has had a mastectomy, hysterectomy, or other types of disfigurement.;
6) If fertility is an issue, it can be managed relatively efficiently in cases of AE with collection of nocturnal emissions, PVS, rectal probe electroejaculation (EEJ), and/or microsurgical sperm aspiration [88,89]. Men of reproductive age should be informed of the risk of infertility due to AE following radical pelvic surgery and the need for sperm harvesting and assisted reproductive techniques.;
7) Patient preferences are an important consideration in the treatment of DE/AE. For example, a patient's preference preference regarding the partner's participation is more critical to successful outcomes than the partner's attendance at all office visits [90].;
And 8) success depends on the patient's willingness and capacity to follow various interventions [6].
1. Psychological interventions
Paying special attention to psychogenic factors may additionally reinforce the therapeutic success of some patients. Many psychotherapeutic treatments have been described for the management of DE/AE, addressing known or suspected psychogenic causes [6,23,30,31,32,45]. These include but not limited to: a) cognitive behavioral therapy and sex education; b) masturbatory retraining and adjustment of sexual fantasies; c) psychotherapy targeting the areas of conflict and sensate focus exercises; d) altering one's orientation from oneself to one's partner; e) sexual anxiety reduction by teaching the individual mindfulness and breathing techniques, progressive relaxation, and increasing sensory tolerance; f) couples' sex therapy and the use of interactional techniques; and g) the sexual tipping point model, which emphasizes the utility of a biopsychosocial-cultural perspective combined with special attention to the patient's narrative. Treatment is patient-centered and holistic, and integrates a variety of therapies as needed [for more details see ref. 6]. Generally, these psychological maneuvers appear to be effective in case reports and case series but none have been properly evaluated in large-scale studies.
2. Pharmacotherapy
Attempts have been made to treat DE/AE using off-label medications based on pharmacological and physiologic considerations [91,92,93]. However, an approved drug does not exist. These medications facilitate ejaculation by different mechanisms of action (Table 4), have limited success, and may lead to significant side effects.
Table 4. Pharmacotherapy for delayed ejaculation and anejaculation.
| Drug | Proposed mechanism | Dose | Timing | Common side effect |
|---|---|---|---|---|
| Testosterone | Correct hypogonadism | 2% testosterone solution | Applied once a day, at the same time each morning. | Pain, redness, swelling, gum or mouth irritation, breast pain, cough |
| Cabergoline | - Dopamine agonist on D2 receptors | 0.5 mg twice/wk | At bedtime | Nausea, drowsiness, cardiac valve regurgitation and heart failure |
| - Activates 5-HT2B receptors | ||||
| Bupropion | Dopamine and norepinephrine reuptake inhibitor | 150~300 mg/d | In the morning | Palpitations, urinary frequency, blurred vision, chest pain, agitation, psychosis |
| Amantadine | Facilitates presynaptic dopamine release and inhibits dopamine reuptake post-synaptically | - As needed 100~400 mg | - For 2 days before sex | Nausea, dizziness, depression, anorexia, hallucinations, compulsivity, hypotension, abnormal dreams, headache, constipation/diarrhea, arrhythmias |
| - 75~100 mg daily | - 2~3 times per day | |||
| Cyproheptadine | Antiserotonergic properties | 2~16 mg | - 1~2 hours before sex | Sedation, impaired concentration, nausea, dizziness, urinary retention, photosensitivity, rash, abdominal pain, fatigue |
| - Daily at bedtime | ||||
| Midodrine | α1-adrenergic receptor agonist | 7.5~30.0 mg | - As needed 30~120 minutes before sex | Dysuria, paresthesia, rigors, pruritus, piloerection, rash |
| - Daily 3 times per day | ||||
| Imipramine | α1-adrenergic receptor agonist | 25~75 mg | Daily at bedtime | Dry mouth, constipation, abdominal pain, blurred vision |
| Ephedrine | α1-adrenergic receptor agonist | 15~60 mg | 1 hour before sex | Nausea, headache, dizziness, insomnia, hypertension, hypervigilance, anxiety |
| Pseudoephedrine | α1-adrenergic receptor agonist | 60~120 mg | 2~3 hours before sex | Insomnia, anxiety, nausea, insomnia, tremor, urinary retention |
| Yohimbine | α2-adrenergic antagonist | 20~50 mg | - 1 hour before sex | Urinary retention, hyperglycemia, tachycardia, hypertension, irritability, dartos contraction, pleasurable tingling, tremor, nausea, dizziness |
| 5-HT1A agonist | - 3 times per day | |||
| Buspirone | 5HT1A agonist effect. | 20~60 mg | Twice daily | Dizziness, nausea, headache, fatigue, blurred vision, numbness, weakness, abdominal pain, insomnia |
| α2-adrenergic antagonist effect | ||||
| Oxytocin | Actions on peripheral oxytocin or vasopressin receptors | 16~24 IU intranasally | - During sex or sublingually before sex | Nausea, vomiting, hypertension, afibrinogenemia |
| Bethanechol | Muscarinic receptor agonist, adrenergic effects | - 10~20 mg | - As needed 1~2 hours before sex | Abdominal pain, nausea, diarrhea, headache, urinary urgency |
| - 30~100 mg | - Twice daily | |||
| Lisdexamfetamine dimesylate | Releases dopamine and norepinephrine from the presynaptic nerve terminals, blocks catecholamine re-uptake by competitive inhibition | 60 mg | 2 hours prior to masturbation or sex | Raynaud's phenomenon (reduced blood flow to the hands and feet), and tachycardia, abdominal pain, blurred vision erectile dysfunction |
| Roboxetine | Norepinephrine reuptake inhibitor | 4~8 mg | Daily | Insomnia, dizziness, dry mouth, constipation, nausea, and excessive sweating |
Given the variety of drugs available for managing DE/AE, the question of which to choose can be a complicated issue in clinical practice. The choice of drug should be guided by etiologic factors, illness characteristics (DE or AE), the patient's preferences, the clinical evidence, and the physician's comfort with different drugs. It is known that the response is relatively poor in neurogenic DE/AE. Of interest is the recent single-case report of the successful oral administration of 60 mg of lisdexamfetamine dimesylate (a prodrug that is converted by the liver to the active dextroamphetamine. which is a noncatecholamine, sympathomimetic amine) 2 hours prior to masturbation in a patient with neurogenic AE [92]. In contrast, a recent double-blind randomized placebo-controlled small study [94] showed that midodrine was similar to placebo in inducing antegrade ejaculation in patients with SCI. For patients who suffer from antidepressant-related DE/AE, shifting to another antidepressant such as bupropion or adding cabergoline if they have hyperprolactinemia may be the most prudent option. For patients with idiopathic DE, symptomatic management with a drug or a combination of drugs aimed at more than 1 therapeutic target may be an option of choice. Hence, the selection of a drug should be tailored to the needs of individual patients and the specific circumstances of each case. Generally, drug treatment does not always produce normal ejaculation, but it may enable partial antegrade ejaculation or retrograde ejaculation.
3. Treatment of infertility issues
Here again, a number of approaches can be employed. The simplest approach is to collect nocturnal emissions in a spermicide-free condom for assisted reproduction [88]. Some patients may report sporadic events of nocturnal emission or ejaculation induced by severe emotional excitement unrelated to sexual activity. A second, simple approach to obtain spermatozoa from psychogenic AE is through vigorous prostatic massage [95] or prostatic urethra catheterization [96]. The presence of spermatozoa in the prostatic urethra may be due to ejaculation dyssynergia (Fig. 1). Assisted ejaculation in the form of PVS is the next choice for sperm retrieval in idiopathic AE and is the first choice in neurogenic AE because it is noninvasive and inexpensive [97]. It requires an intact lumbosacral cord segment. Spinal cord lesions above T10 suggest a better response. In patients in whom PVS fails, EEJ may be successful [89]. The adverse effects profile of these procedures may include skin irritation, high blood pressure, rectal mucosa burning, and autonomic dysreflexia, which can be pretreated with 10 to 40 mg of sublingual nifedipine approximately 15 minutes prior to PVS, which can blunt the increase in blood pressure in men with a history of SCI. In the vast majority of these men, motile spermatozoa can be obtained through assisted ejaculation. When such procedures fail, sperm retrieval through either percutaneous vasal sperm aspiration or minimally invasive epididymal sperm aspiration may be an option [98]. Ejaculate samples retrieved from men with SCI typically are characterized by a normal sperm concentration, but abnormally low sperm motility and viability. Despite the impaired sperm parameters, the pregnancy outcomes of assisted reproduction using sperm from men with SCI are similar to those using sperm from non-SCI men. In cases with azoospermia, testicular sperm extraction for intracytoplasmic sperm injection is a feasible option [99]. Approaches for sperm recovery should be considered and employed in a step-wise fashion, starting with the most cost-effective and least invasive options [98]. The patient should realize that with any approach for sperm recovery there is some risk of hematoma, infection, or pain, all of which are likely to resolve with time.
CONCLUSIONS
The literature suggests that the pathophysiology of DE/AE is multifactorial, including both organic and psychosocial factors that are neither independent nor mutually exclusive. Despite the many publications on this condition, the exact pathogenesis is not yet known. There is currently no single gold standard for diagnosing DE/AE, as operationalized criteria do not exist. The history is the key to the diagnosis. Treatment should be cause-specific. There are many approaches to treatment planning, including various psychological interventions, pharmacotherapy, and specific treatments for infertile men. No approved drug therapy exists. A rigid treatment plan is not suitable for all patients. A number of approaches can be employed for infertile men, including collection of nocturnal emissions, vigorous prostatic massage, prostatic urethra catheterization, PVS, rectal probe EEJ, sperm retrieval from either the vas deferens or the epididymis, or testicular sperm extraction.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
Author Contribution: Research conception & design: Abdel-Hamid IA, Ali OI. Performing the experiments: not applicable. Data acquisition: all authors. Data analysis and interpretation: not applicable. Statistical analysis: not applicable. Drafting of the manuscript: Abdel-Hamid IA, Ali OI. Critical revision of the manuscript: all authors. Receiving grant: none. Approval of final manuscript: all authors.
References
- 1.Munjack DJ, Kanno PH. Retarded ejaculation: a review. Arch Sex Behav. 1979;8:139–150. doi: 10.1007/BF01541234. [DOI] [PubMed] [Google Scholar]
- 2.Shull GR, Sprenkle DH. Retarded ejaculation reconceptualization and implications for treatment. J Sex Marital Ther. 1980;6:234–246. doi: 10.1080/00926238008406089. [DOI] [PubMed] [Google Scholar]
- 3.Segraves RT. Considerations for a better definition of male orgasmic disorder in DSM V. J Sex Med. 2010;7:690–695. doi: 10.1111/j.1743-6109.2009.01683.x. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 5.Rowland D, McMahon CG, Abdo C, Chen J, Jannini E, Waldinger MD, et al. Disorders of orgasm and ejaculation in men. J Sex Med. 2010;7:1668–1686. doi: 10.1111/j.1743-6109.2010.01782.x. [DOI] [PubMed] [Google Scholar]
- 6.Perelman MA. Psychosexual therapy for delayed ejaculation based on the sexual tipping point model. Transl Androl Urol. 2016;5:563–575. doi: 10.21037/tau.2016.07.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perelman MA. Reexamining the definitions of PE and DE. J Sex Marital Ther. 2017;43:633–644. doi: 10.1080/0092623X.2016.1230161. [DOI] [PubMed] [Google Scholar]
- 8.Waldinger MD, Quinn P, Dilleen M, Mundayat R, Schweitzer DH, Boolell M. A multinational population survey of intravaginal ejaculation latency time. J Sex Med. 2005;2:492–497. doi: 10.1111/j.1743-6109.2005.00070.x. [DOI] [PubMed] [Google Scholar]
- 9.Patrick DL, Althof SE, Pryor JL, Rosen R, Rowland DL, Ho KF, et al. Premature ejaculation: an observational study of men and their partners. J Sex Med. 2005;2:358–367. doi: 10.1111/j.1743-6109.2005.20353.x. [DOI] [PubMed] [Google Scholar]
- 10.Waldinger MD, McIntosh J, Schweitzer DH. A five-nation survey to assess the distribution of the intravaginal ejaculatory latency time among the general male population. J Sex Med. 2009;6:2888–2895. doi: 10.1111/j.1743-6109.2009.01392.x. [DOI] [PubMed] [Google Scholar]
- 11.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281:537–544. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 12.Fugl-Meyer AR, Sjögren Fugl-Meyer K. Sexual disabilities, problems, and satisfaction in 18–74 year old Swedes. Scand J Sexol. 1999;3:79–105. [Google Scholar]
- 13.Simons JS, Carey MP. Prevalence of sexual dysfunctions: results from a decade of research. Arch Sex Behav. 2001;30:177–219. doi: 10.1023/a:1002729318254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perelman MA, Rowland DL. Retarded ejaculation. World J Urol. 2006;24:645–652. doi: 10.1007/s00345-006-0127-6. [DOI] [PubMed] [Google Scholar]
- 15.Paduch DA, Polzer P, Morgentaler A, Althof S, Donatucci C, Ni X, et al. Clinical and demographic correlates of ejaculatory dysfunctions other than premature ejaculation: a prospective, observational study. J Sex Med. 2015;12:2276–2286. doi: 10.1111/jsm.13027. [DOI] [PubMed] [Google Scholar]
- 16.Nathan SG. The epidemiology of the DSM-III psychosexual dysfunctions. J Sex Marital Ther. 1986;12:267–281. doi: 10.1080/00926238608415413. [DOI] [PubMed] [Google Scholar]
- 17.Nazareth I, Boynton P, King M. Problems with sexual function in people attending London general practitioners: cross sectional study. BMJ. 2003;327:423. doi: 10.1136/bmj.327.7412.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blanker MH, Bosch JL, Groeneveld FP, Bohnen AM, Prins A, Thomas S, et al. Erectile and ejaculatory dysfunction in a community-based sample of men 50 to 78 years old: prevalence, concern, and relation to sexual activity. Urology. 2001;57:763–768. doi: 10.1016/s0090-4295(00)01091-8. [DOI] [PubMed] [Google Scholar]
- 19.Corona G, Lee DM, Forti G, O'Connor DB, Maggi M, O'Neill TW, et al. Age-related changes in general and sexual health in middle-aged and older men: results from the European male ageing study (EMAS) J Sex Med. 2010;7:1362–1380. doi: 10.1111/j.1743-6109.2009.01601.x. [DOI] [PubMed] [Google Scholar]
- 20.Rosen RC, Heiman JR, Long JS, Fisher WA, Sand MS. Men with sexual problems and their partners: findings from the international survey of relationships. Arch Sex Behav. 2016;45:159–173. doi: 10.1007/s10508-015-0568-3. [DOI] [PubMed] [Google Scholar]
- 21.Perelman MA. Patient highlights. Delayed ejaculation. J Sex Med. 2013;10:1189–1190. doi: 10.1111/jsm.12141. [DOI] [PubMed] [Google Scholar]
- 22.Butcher MJ, Welliver RC, Jr, Sadowski D, Botchway A, Köhler TS. How is delayed ejaculation defined and treated in North America? Andrology. 2015;3:626–631. doi: 10.1111/andr.12041. [DOI] [PubMed] [Google Scholar]
- 23.Althof SE. Psychological interventions for delayed ejaculation/orgasm. Int J Impot Res. 2012;24:131–136. doi: 10.1038/ijir.2012.2. [DOI] [PubMed] [Google Scholar]
- 24.Masters WH, Johnson VE. Human sexual inadequacy. Boston: Little, Brown; 1970. [Google Scholar]
- 25.Bancroft J. Human sexuality and its problem. London: Churchill Livingstone; 2008. [Google Scholar]
- 26.Rowland DL, Keeney C, Slob AK. Sexual response in men with inhibited or retarded ejaculation. Int J Impot Res. 2004;16:270–274. doi: 10.1038/sj.ijir.3901156. [DOI] [PubMed] [Google Scholar]
- 27.Teloken P, Nelson C, Mulhall J. Secondary delayed orgasm: patterns, correlates and predictors. J Urol. 2012;187:e562 [Google Scholar]
- 28.Xia JD, Han YF, Pan F, Zhou LH, Chen Y, Dai YT. Clinical characteristics and penile afferent neuronal function in patients with primary delayed ejaculation. Andrology. 2013;1:787–792. doi: 10.1111/j.2047-2927.2013.00119.x. [DOI] [PubMed] [Google Scholar]
- 29.Nelson CJ, Ahmed A, Valenzuela R, Parker M, Mulhall JP. Assessment of penile vibratory stimulation as a management strategy in men with secondary retarded orgasm. Urology. 2007;69:552–555. doi: 10.1016/j.urology.2006.02.048. discussion 555-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perelman MA. Idiosyncratic masturbation patterns: a key unexplored variable in the treatment of retarded ejaculation by the practicing urologist. J Urol. 2005;173:340. [Google Scholar]
- 31.Apfelbaum B. Retarded ejaculation: a much-misunderstood syndrome. In: Lieblum SR, Rosen RC, editors. Principles and practice of sex therapy. 2nd ed. New York: Guilford Press; 1989. pp. 168–202. [Google Scholar]
- 32.Apfelbaum B. Retarded ejaculation: a much-misunderstood syndrome. In: Leiblum SR, Rosen RC, editors. Principles and practice of sex therapy. 3rd ed. New York: Guilford Press; 2000. pp. 205–241. [Google Scholar]
- 33.Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts male aging study. J Urol. 1994;151:54–61. doi: 10.1016/s0022-5347(17)34871-1. [DOI] [PubMed] [Google Scholar]
- 34.O'Leary MP, Rhodes T, Girman CJ, Jacobson DJ, Roberts RO, Lieber MM, et al. Distribution of the brief male sexual inventory in community men. Int J Impot Res. 2003;15:185–191. doi: 10.1038/sj.ijir.3900996. [DOI] [PubMed] [Google Scholar]
- 35.Corona G, Jannini EA, Lotti F, Boddi V, De Vita G, Forti G, et al. Premature and delayed ejaculation: two ends of a single continuum influenced by hormonal milieu. Int J Androl. 2011;34:41–48. doi: 10.1111/j.1365-2605.2010.01059.x. [DOI] [PubMed] [Google Scholar]
- 36.Edwards AE, Husted JR. Penile sensitivity, age, and sexual behavior. J Clin Psychol. 1976;32:697–700. doi: 10.1002/1097-4679(197607)32:3<697::aid-jclp2270320345>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 37.Halata Z, Munger BL. The neuroanatomical basis for the protopathic sensibility of the human glans penis. Brain Res. 1986;371:205–230. doi: 10.1016/0006-8993(86)90357-4. [DOI] [PubMed] [Google Scholar]
- 38.Tammaro A, Parisella FR, Cavallotti C, Persechino S, Cavallotti C. Ultrastructural age-related changes in the sensory corpuscles of the human genital skin. J Biol Regul Homeost Agents. 2013;27:241–245. [PubMed] [Google Scholar]
- 39.Rowland DL, Greenleaf W, Mas M, Myers L, Davidson JM. Penile and finger sensory thresholds in young, aging, and diabetic males. Arch Sex Behav. 1989;18:1–12. doi: 10.1007/BF01579287. [DOI] [PubMed] [Google Scholar]
- 40.Rowland DL. Penile sensitivity in men: a composite of recent findings. Urology. 1998;52:1101–1105. doi: 10.1016/s0090-4295(98)00413-0. [DOI] [PubMed] [Google Scholar]
- 41.Montejo AL, Montejo L, Navarro-Cremades F. Sexual side-effects of antidepressant and antipsychotic drugs. Curr Opin Psychiatry. 2015;28:418–423. doi: 10.1097/YCO.0000000000000198. [DOI] [PubMed] [Google Scholar]
- 42.Hendren SK, O'Connor BI, Liu M, Asano T, Cohen Z, Swallow CJ, et al. Prevalence of male and female sexual dysfunction is high following surgery for rectal cancer. Ann Surg. 2005;242:212–223. doi: 10.1097/01.sla.0000171299.43954.ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brindley GS, Gillan P. Men and women who do not have orgasms. Br J Psychiatry. 1982;140:351–356. doi: 10.1192/bjp.140.4.351. [DOI] [PubMed] [Google Scholar]
- 44.Richardson D, Nalabanda A, Goldmeier D. Retarded ejaculation: a review. Int J STD AIDS. 2006;17:143–150. doi: 10.1258/095646206775809141. [DOI] [PubMed] [Google Scholar]
- 45.Foley S. The complex etiology of delayed ejaculation: assessment and treatment implications. J Fam Psychother. 2009;20:261–282. [Google Scholar]
- 46.Jern P, Santtila P, Witting K, Alanko K, Harlaar N, Johansson A, et al. Premature and delayed ejaculation: genetic and environmental effects in a population-based sample of Finnish twins. J Sex Med. 2007;4:1739–1749. doi: 10.1111/j.1743-6109.2007.00599.x. [DOI] [PubMed] [Google Scholar]
- 47.Jern P, Westberg L, Johansson A, Gunst A, Eriksson E, Sandnabba K, et al. A study of possible associations between single nucleotide polymorphisms in the serotonin receptor 1A, 1B, and 2C genes and self-reported ejaculation latency time. J Sex Med. 2012;9:866–872. doi: 10.1111/j.1743-6109.2011.02618.x. [DOI] [PubMed] [Google Scholar]
- 48.Jern P, Westberg L, Johansson A, Jonsson L, Corander J, Sandnabba NK, et al. Are single nucleotide polymorphisms in the oxytocin and vasopressin 1A/1B receptor genes likely candidates for variation in ejaculatory function? BJU Int. 2012;110:E1173–E1180. doi: 10.1111/j.1464-410X.2012.11419.x. [DOI] [PubMed] [Google Scholar]
- 49.Corona G, Ricca V, Bandini E, Mannucci E, Lotti F, Boddi V, et al. Selective serotonin reuptake inhibitor-induced sexual dysfunction. J Sex Med. 2009;6:1259–1269. doi: 10.1111/j.1743-6109.2009.01248.x. [DOI] [PubMed] [Google Scholar]
- 50.Stevenson JM, Bishop JR. Genetic determinants of selective serotonin reuptake inhibitor related sexual dysfunction. Pharmacogenomics. 2014;15:1791–1806. doi: 10.2217/pgs.14.114. [DOI] [PubMed] [Google Scholar]
- 51.Zourková A, Hadasová E. Relationship between CYP 2D6 metabolic status and sexual dysfunction in paroxetine treatment. J Sex Marital Ther. 2002;28:451–461. doi: 10.1080/00926230290001565. [DOI] [PubMed] [Google Scholar]
- 52.Bishop JR, Moline J, Ellingrod VL, Schultz SK, Clayton AH. Serotonin 2A -1438 G/A and G-protein Beta3 subunit C825T polymorphisms in patients with depression and SSRI-associated sexual side-effects. Neuropsychopharmacology. 2006;31:2281–2288. doi: 10.1038/sj.npp.1301090. [DOI] [PubMed] [Google Scholar]
- 53.Zourková A, Cesková E, Hadasová E, Ravcuková B. Links among paroxetine-induced sexual dysfunctions, gender, and CYP2D6 activity. J Sex Marital Ther. 2007;33:343–355. doi: 10.1080/00926230701385589. [DOI] [PubMed] [Google Scholar]
- 54.Perlis RH, Laje G, Smoller JW, Fava M, Rush AJ, McMahon FJ. Genetic and clinical predictors of sexual dysfunction in citalopram-treated depressed patients. Neuropsychopharmacology. 2009;34:1819–1828. doi: 10.1038/npp.2009.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Strohmaier J, Wüst S, Uher R, Henigsberg N, Mors O, Hauser J, et al. Sexual dysfunction during treatment with serotonergic and noradrenergic antidepressants: clinical description and the role of the 5-HTTLPR. World J Biol Psychiatry. 2011;12:528–538. doi: 10.3109/15622975.2011.559270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liang CS, Ho PS, Chiang KT, Su HC. 5-HT2A receptor -1438 G/A polymorphism and serotonergic antidepressant-induced sexual dysfunction in male patients with major depressive disorder: a prospective exploratory study. J Sex Med. 2012;9:2009–2016. doi: 10.1111/j.1743-6109.2012.02769.x. [DOI] [PubMed] [Google Scholar]
- 57.de Klerk OL, Nolte IM, Bet PM, Bosker FJ, Snieder H, den Boer JA, et al. ABCB1 gene variants influence tolerance to selective serotonin reuptake inhibitors in a large sample of Dutch cases with major depressive disorder. Pharmacogenomics J. 2013;13:349–353. doi: 10.1038/tpj.2012.16. [DOI] [PubMed] [Google Scholar]
- 58.Clark SL, Adkins DE, Aberg K, Hettema JM, McClay JL, Souza RP, et al. Pharmacogenomic study of side-effects for antidepressant treatment options in STAR*D. Psychol Med. 2012;42:1151–1162. doi: 10.1017/S003329171100239X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kurose K, Hiratsuka K, Ishiwata K, Nishikawa J, Nonen S, Azuma J, et al. Genome-wide association study of SSRI/SNRI-induced sexual dysfunction in a Japanese cohort with major depression. Psychiatry Res. 2012;198:424–429. doi: 10.1016/j.psychres.2012.01.023. [DOI] [PubMed] [Google Scholar]
- 60.Adkins DE, Clark SL, Åberg K, Hettema JM, Bukszár J, McClay JL, et al. Genome-wide pharmacogenomic study of citalopram-induced side effects in STAR*D. Transl Psychiatry. 2012;2:e129. doi: 10.1038/tp.2012.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Huang YY, Zhang XS, Gao JJ, Gao P, Liang CZ. Association between serotonin transporter 5-HTTLPR and STin2 VNTR polymorphisms and anejaculation: a preliminary report. Asian J Androl. 2017;19:719–720. doi: 10.4103/1008-682X.182821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Waldinger MD, Berendsen HH, Blok BF, Olivier B, Holstege G. Premature ejaculation and serotonergic antidepressants-induced delayed ejaculation: the involvement of the serotonergic system. Behav Brain Res. 1998;92:111–118. doi: 10.1016/s0166-4328(97)00183-6. [DOI] [PubMed] [Google Scholar]
- 63.Waldinger MD, Schweitzer DH. Retarded ejaculation in men: an overview of psychological and neurobiological insights. World J Urol. 2005;23:76–81. doi: 10.1007/s00345-004-0487-8. [DOI] [PubMed] [Google Scholar]
- 64.McMahon CG. Premature ejaculation. Indian J Urol. 2007;23:97–108. doi: 10.4103/0970-1591.32056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Moretti M, Facchini F, Grande M, Larosa M, Leone M, Ziglioli F, et al. Ejaculatory system cysts: a case report. Urologia. 2014;81(Suppl 23):S32–S37. doi: 10.5301/RU.2014.11999. [DOI] [PubMed] [Google Scholar]
- 66.Taskinen S, Heikkilä J, Santtila P, Rintala R. Posterior urethral valves and adult sexual function. BJU Int. 2012;110:E392–E396. doi: 10.1111/j.1464-410X.2012.11091.x. [DOI] [PubMed] [Google Scholar]
- 67.Reddy SS, Inouye BM, Anele UA, Abdelwahab M, Le B, Gearhart JP, et al. Sexual health outcomes in adults with complete male epispadias. J Urol. 2015;194:1091–1095. doi: 10.1016/j.juro.2015.04.082. [DOI] [PubMed] [Google Scholar]
- 68.Park W, Zwink N, Rösch WH, Schmiedeke E, Stein R, Schmidt D, et al. Sexual function in adult patients with classic bladder exstrophy: a multicenter study. J Pediatr Urol. 2015;11:125.e1–125.e6. doi: 10.1016/j.jpurol.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 69.Frey A, Pedersen C, Lindberg H, Bisbjerg R, Sønksen J, Fode M. Prevalence and predicting factors for commonly neglected sexual side effects to external-beam radiation therapy for prostate cancer. J Sex Med. 2017;14:558–565. doi: 10.1016/j.jsxm.2017.01.015. [DOI] [PubMed] [Google Scholar]
- 70.Sullivan JF, Stember DS, Deveci S, Akin-Olugbade Y, Mulhall JP. Ejaculation profiles of men following radiation therapy for prostate cancer. J Sex Med. 2013;10:1410–1416. doi: 10.1111/jsm.12101. [DOI] [PubMed] [Google Scholar]
- 71.Lew-Starowicz M, Rola R. Sexual dysfunctions and sexual quality of life in men with multiple sclerosis. J Sex Med. 2014;11:1294–1301. doi: 10.1111/jsm.12474. [DOI] [PubMed] [Google Scholar]
- 72.Anderson KD, Borisoff JF, Johnson RD, Stiens SA, Elliott SL. Long-term effects of spinal cord injury on sexual function in men: implications for neuroplasticity. Spinal Cord. 2007;45:338–348. doi: 10.1038/sj.sc.3101978. [DOI] [PubMed] [Google Scholar]
- 73.Lindau ST, Tang H, Gomero A, Vable A, Huang ES, Drum ML, et al. Sexuality among middle-aged and older adults with diagnosed and undiagnosed diabetes: a national, population-based study. Diabetes Care. 2010;33:2202–2210. doi: 10.2337/dc10-0524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ohl DA, Quallich SA, Sønksen J, Brackett NL, Lynne CM. Anejaculation and retrograde ejaculation. Urol Clin North Am. 2008;35:211–220. doi: 10.1016/j.ucl.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 75.Chen J. The pathophysiology of delayed ejaculation. Transl Androl Urol. 2016;5:549–562. doi: 10.21037/tau.2016.05.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Corona G, Jannini EA, Mannucci E, Fisher AD, Lotti F, Petrone L, et al. Different testosterone levels are associated with ejaculatory dysfunction. J Sex Med. 2008;5:1991–1998. doi: 10.1111/j.1743-6109.2008.00803.x. [DOI] [PubMed] [Google Scholar]
- 77.Morgentaler A, Polzer P, Althof S, Bolyakov A, Donatucci C, Ni X, et al. Delayed ejaculation and associated complaints: relationship to ejaculation times and serum testosterone levels. J Sex Med. 2017;14:1116–1124. doi: 10.1016/j.jsxm.2017.06.013. [DOI] [PubMed] [Google Scholar]
- 78.Nair S, Milsom S. Anejaculation as the presenting feature of pituitary microadenoma. Fertil Steril. 2008;90:2012.e21–2012.e23. doi: 10.1016/j.fertnstert.2007.12.064. [DOI] [PubMed] [Google Scholar]
- 79.Carani C, Isidori AM, Granata A, Carosa E, Maggi M, Lenzi A, et al. Multicenter study on the prevalence of sexual symptoms in male hypo- and hyperthyroid patients. J Clin Endocrinol Metab. 2005;90:6472–6479. doi: 10.1210/jc.2005-1135. [DOI] [PubMed] [Google Scholar]
- 80.La Torre A, Giupponi G, Duffy D, Conca A, Cai T, Scardigli A. Sexual dysfunction related to drugs: a critical review. part V: α-blocker and 5-ARI drugs. Pharmacopsychiatry. 2016;49:3–13. doi: 10.1055/s-0035-1565100. [DOI] [PubMed] [Google Scholar]
- 81.Abdel-Hamid IA, Saleh el-S. Primary lifelong delayed ejaculation: characteristics and response to bupropion. J Sex Med. 2011;8:1772–1779. doi: 10.1111/j.1743-6109.2010.02131.x. [DOI] [PubMed] [Google Scholar]
- 82.Tsimtsiou Z, Hatzimouratidis K, Nakopoulou E, Kyrana E, Salpigidis G, Hatzichristou D. Predictors of physicians' involvement in addressing sexual health issues. J Sex Med. 2006;3:583–588. doi: 10.1111/j.1743-6109.2006.00271.x. [DOI] [PubMed] [Google Scholar]
- 83.Courtois F, Charvier K, Leriche A, Vézina JG, Côté I, Raymond D, et al. Perceived physiological and orgasmic sensations at ejaculation in spinal cord injured men. J Sex Med. 2008;5:2419–2430. doi: 10.1111/j.1743-6109.2008.00857.x. [DOI] [PubMed] [Google Scholar]
- 84.Paduch DA, Polzer PK, Ni X, Basaria S. Testosterone replacement in androgen-deficient men with ejaculatory dysfunction: a randomized controlled trial. J Clin Endocrinol Metab. 2015;100:2956–2962. doi: 10.1210/jc.2014-4434. [DOI] [PubMed] [Google Scholar]
- 85.Maggi M, Heiselman D, Knorr J, Iyengar S, Paduch DA, Donatucci CF. Impact of testosterone solution 2% on ejaculatory dysfunction in hypogonadal men. J Sex Med. 2016;13:1220–1226. doi: 10.1016/j.jsxm.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 86.Masui H, Ike H, Yamaguchi S, Oki S, Shimada H. Male sexual function after autonomic nerve-preserving operation for rectal cancer. Dis Colon Rectum. 1996;39:1140–1145. doi: 10.1007/BF02081416. [DOI] [PubMed] [Google Scholar]
- 87.Pettus JA, Carver BS, Masterson T, Stasi J, Sheinfeld J. Preservation of ejaculation in patients undergoing nerve-sparing postchemotherapy retroperitoneal lymph node dissection for metastatic testicular cancer. Urology. 2009;73:328–331. doi: 10.1016/j.urology.2008.08.501. discussion 331-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Meng X, Fan L, Liu J, Wang T, Yang J, Wang J, et al. Fresh semen quality in ejaculates produced by nocturnal emission in men with idiopathic anejaculation. Fertil Steril. 2013;100:1248–1252. doi: 10.1016/j.fertnstert.2013.07.1979. [DOI] [PubMed] [Google Scholar]
- 89.Soeterik TF, Veenboer PW, Lock TM. Electroejaculation in psychogenic anejaculation. Fertil Steril. 2014;101:1604–1608. doi: 10.1016/j.fertnstert.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 90.Perelman MA. Sex coaching for physicians: combination treatment for patient and partner. Int J Impot Res. 2003;15(Suppl 5):S67–S74. doi: 10.1038/sj.ijir.3901075. [DOI] [PubMed] [Google Scholar]
- 91.Abdel-Hamid IA, Elsaied MA, Mostafa T. The drug treatment of delayed ejaculation. Transl Androl Urol. 2016;5:576–591. doi: 10.21037/tau.2016.05.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lyons MD, Lentz AC, Coward RM. Lisdexamfetamine dimesylate (Vyvanse) for the treatment of neurogenic anejaculation. Am J Mens Health. 2017;11:618–619. doi: 10.1177/1557988316658640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pryor JP. Erectile and ejaculatory problems in infertility. In: Hargreave TB, editor. Male infertility. London: Springer; 1997. pp. 319–336. [Google Scholar]
- 94.Leduc BE, Fournier C, Jacquemin G, Lepage Y, Vinet B, Hétu PO, et al. Midodrine in patients with spinal cord injury and anejaculation: a double-blind randomized placebo-controlled pilot study. J Spinal Cord Med. 2015;38:57–62. doi: 10.1179/2045772314Y.0000000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fahmy I, Kamal A, Metwali M, Rhodes C, Mansour R, Serour G, et al. Vigorous prostatic massage: a simple method to retrieve spermatozoa for intracytoplasmic sperm injection in psychogenic anejaculation: case report. Hum Reprod. 1999;14:2050–2053. doi: 10.1093/humrep/14.8.2050. [DOI] [PubMed] [Google Scholar]
- 96.Soler JM, Previnaire JG, Mieusset R. Evidence of a new pattern of ejaculation in men with spinal cord injury: ejaculation dyssynergia and implications for fertility. Spinal Cord. 2016;54:1210–1214. doi: 10.1038/sc.2016.78. [DOI] [PubMed] [Google Scholar]
- 97.Castle SM, Jenkins LC, Ibrahim E, Aballa TC, Lynne CM, Brackett NL. Safety and efficacy of a new device for inducing ejaculation in men with spinal cord injuries. Spinal Cord. 2014;52(Suppl 2):S27–S29. doi: 10.1038/sc.2014.110. [DOI] [PubMed] [Google Scholar]
- 98.Fode M, Ohl DA, Sønksen J. A step-wise approach to sperm retrieval in men with neurogenic anejaculation. Nat Rev Urol. 2015;12:607–616. doi: 10.1038/nrurol.2015.241. [DOI] [PubMed] [Google Scholar]
- 99.Raviv G, Madgar I, Elizur S, Zeilig G, Levron J. Testicular sperm retrieval and intra cytoplasmic sperm injection provide favorable outcome in spinal cord injury patients, failing conservative reproductive treatment. Spinal Cord. 2013;51:642–644. doi: 10.1038/sc.2013.44. [DOI] [PubMed] [Google Scholar]