ABSTRACT
Background: Globally, stillbirth remains a significant public health issue, particularly in developing countries such as Bangladesh.
Objective: This study aimed to investigate the potential predictors of stillbirths in Bangladesh over a ten-year period.
Methods: The Bangladesh Demographic and Health Surveys data for the years 2004, 2007, 2011 and 2014 (n = 29,094) were used for the study to investigate the predictors of stillbirths. Stillbirth was examined against a set of community, socio-economic and child characteristics, using a multivariable logistic regression model that adjusted for cluster and sampling variability.
Results: The pooled rate of stillbirth in Bangladesh was 28 in 1000 births (95% CI: 22, 34). Stillbirth rates were higher in rural compared to urban areas in Bangladesh. Mothers who had a secondary or higher level of education (OR = 0.59, 95%CI: 0.43–0.82, P = 0.002) and those with primary education (OR = 0.66, 95%CI: 0.55–0.80, P < 0.001) were less likely to experience stillbirths compared to mothers with no education. Mothers with more than two children were significantly less likely to have stillbirths compared to mothers with one child. Those from poor households reported increased odds of stillbirth compared to those from rich households.
Conclusion: Our analysis indicated that no maternal education, primiparity and poor household were predictors of stillbirths in Bangladesh. A collaborative effort is needed to reduce stillbirth rates among these high-risk groups in Bangladesh, with the socio-economic and health-related Sustainable Development Goals providing a critical vehicle for the co-ordination of this work.
KEYWORDS: Bangladesh, infants, mortality, predictors, stillbirths, under-five
Background
The Global Burden of Disease, Injuries and Risk Factors Study 2015 (GBD 2015) reported that the rate of stillbirth has fallen worldwide by 47% since 1990, and more quickly from the year 2000 [1]. Despite this decline, recent studies have reported that global estimates of stillbirth ranged from 2.1 million [1] to 2.6 million [2] in 2015, and approximately 98% of those fetal deaths occurred in developing countries [1,2]. Variation in global estimates of the stillbirth rate may be due to access to data sources and modelling strategy, as both studies used the standard definition for stillbirth (fetal death after 28 weeks’ gestation).
The United Nations reported that Bangladesh made a significant improvement in reducing under-5 mortality rate during the Millennium Development Goals (MDG) era (between 1990 and 2015) [3]. Despite this achievement, Bangladesh remains a major contributor to stillbirth rates in South Asia [2] with a reported stillbirth rate of 20 per 1000 live births in 2015 [1]. Stillbirths have an enormous impact on mothers, families, health care professionals and the community [4]. Previous studies have quantified the direct [5,6] and indirect [4] financial costs for parents after an experience of stillbirth, however, the psychological and social costs associated with stillbirth have been described as unquantifiable [7].
Based on the health burden associated with stillbirth, there is a renewed focus at the global level on ending preventable stillbirths by 2030 (Sustainable Development Goal, SDG-3.2) [8,9]. Similarly, the Lancet Series on ending preventable stillbirths highlighted the need for policy formulation and ongoing research, particularly improved data collection to support the implementation of evidence-based initiatives [8]. In the context of this global goal, country-specific evidence would be helpful in informing targeted interventions and policy decision-making to reduce stillbirth in Bangladesh.
In Bangladesh, information on risk factors for stillbirths is limited at the national level. Previous studies conducted in rural areas [10,11] and the inner city of Dhaka [12] found that a lack of maternal education, older maternal age (≥35 years), history of alcohol intake and drug abuse were associated with higher rates of stillbirth. The generalisability of these findings to the broader Bangladesh population may be limited, given differences in socio-economic status and geographical regions. The burden of stillbirths can vary within a country, with economically disadvantaged communities having higher rates compared to their economically well-off counterparts [13].
Using a reliable and population-based maternal and child health data source (Bangladesh Demographic and Health Survey, BDHS), we provide nationally representative information on the rate and predictors of stillbirth. Our study aimed to investigate the predictors of stillbirth in Bangladesh, using the BDHS datasets for the period (2004–2014).
Methods
Data sources
Datasets for the years 2004, 2007, 2011 and 2014 from the BDHS were pooled and used for the study. We pooled data across time to increase sample size and statistical power, consistent with previous studies [14–16]. The BDHS data were collected by the National Institute of Population Research and Training (NIPORT), with technical support from Measure DHS through the Inner City Fund (ICF) International. A weighted total sample of 29,094 pregnancies over 28 weeks’ gestation for women aged 15–49 years were included in the final analysis (2004: n = 6,395; 2007: n = 5,409; 2011: n = 9,021; and 2014: n = 8,269). The data were weighted to ensure the representativeness of the survey results at the national level.
In the 2011 and 2014 BDHS, a new administrative region called ‘Rangpur’ was created, and when Rangpur was removed from the overall data sets, a total weighted sample of 27,540 pregnancies over 28 weeks’ gestation for women aged 15–49 years was obtained (2004: n = 6,395; 2007: n = 5,409; 2011: n = 8,315; and 2014: n = 7,421). Data with Rangpur (general Bangladesh population) and without Rangpur were reported in this present study to ensure robustness of the analyses. The average response rate for the four surveys was 98%. A detailed description of the survey methodology, sampling procedure and questionnaires used for data collection is provided elsewhere [17].
Outcome variable
The study outcome was stillbirth, defined as death of a fetus of more than or equal to 28 weeks’ gestation, consistent with previous studies [1,2,12]. The outcome was recorded as a binary variable in the datasets, coded as ‘1’ for stillbirth and ‘0’ for no stillbirth.
Study factors
The study factors included community, socio-demographic and child factors. These were selected based on previously published studies and availability of data [10–12]. The community factors were place of residence (urban or rural) and geographical region, covering divisions in Bangladesh, namely: Barisal, Chittagong, Dhaka, Khulna, Rajshahi, Sylhet and Rangpur. Socio-demographic factors included number of children ever born, age of mother at the time of the interview, mother’s working status, mother’s marital status, mother’s body mass index (BMI), parents’ level of education, mother’s age at index childbirth, desire for pregnancy, mother’s access to the media (television, radio or newspaper). Child factors comprised gender of the child, previous multiple births, previous death of a sibling and combined birth rank and interval. Based on previous studies [18,19], we combined birth order and interval in the analysis because of the impact of birth order that may be mediated by the birth interval. Household wealth index was constructed by NIPORT and ICF International [17], using the principal components analysis by assigning weights to three household characteristics; namely: type of floor and wall; access to electricity; and six household assets; namely, possession of a radio, television, bicycle, motorcycle, car and fridge. The household wealth index was ranked across the four surveys, where household wealth index was divided into three categories. The bottom 40% of households were arbitrarily classified as poor households, the next 40% as the middle households and the top 20% as rich households [20]. Type of cooking fuels available to household members at the time of survey will be referred to as ‘household air pollution from solid fuel’. Household air pollution from solid fuel were categorised as solid fuels (coal/lignite, charcoal, wood, straw/shrubs/grass, agricultural crop, animal dung) and non-solid fuels (electricity, liquefied petroleum gas (LPG), natural gas, biogas, kerosene).
Statistical analysis
Frequency tabulations were first conducted to describe the distributions of data by years of the survey, followed by calculation of the rate of stillbirths, unadjusted odds ratios (OR) and their 95% confidence interval (CI) of all potential predictors.
A three-stage model was performed for the multivariable logistic regression analyses by following a conceptual model that was employed by Chowdhury et al. [21]. In the first modelling stage, community and socio-economic determinants were examined, and only significant variables associated with the study outcome at 5% significance level were retained in model 1. In the second stage, the significant variables in model 1 were added to child demographic factors. In the final stage, media factors and environmental factor were added to significant variables in model 2 to determine factors associated with stillbirth. All analyses were performed in Stata statistical software version 14 (Stata Corp., College Station, TX, USA) that adjusted for sampling weights, intra-cluster variability and sampling design to provide population-based estimates.
Ethics
The study used existing survey datasets that are available online by application, with all identifier information removed. The surveys were approved by the Ethics Committee of the ICF International, USA and the National Research Ethics Committee of Bangladesh Medical Research Council (BMRC), Bangladesh. We obtained approval from Measure DHS to download and use the data for the study.
Results
Characteristics of the study population
The majority of mothers were from the Dhaka administrative region (32.2%), with the smallest group from the Barisal region (5.8%). Half of the mothers belonged to the youngest age group (15–24 years, 50.1%), with 8.8% aged 35–49 years. Mothers with no schooling and those with only primary education were almost equally represented (43.7% and 45.5%, respectively). Approximately 18 out of every 100 households were categorised as wealthy, and 42 out of every 100 households were categorised as poor households. Female and male children were almost equally distributed (Table 1).
Table 1.
Characteristics of the study population in Bangladesh, 2004–2014 (n = 29,094).
| With Rangpur (a) (n = 29,094) |
Without Rangpur (n = 27,540) |
|||||
|---|---|---|---|---|---|---|
| VARIABLE | n | n* | %* | n | n* | %* |
| COMMUNITY LEVEL FACTORS | ||||||
| Year of survey | ||||||
| 2004 | 6287 | 6395 | 22.0 | 6287 | 6395 | 23.2 |
| 2007 | 5473 | 5409 | 18.6 | 5473 | 5409 | 19.6 |
| 2011 | 8986 | 9021 | 31.0 | 7527 | 8316 | 30.2 |
| 2014 | 8069 | 8269 | 28.4 | 6714 | 7420 | 26.9 |
| Cluster type | ||||||
| Urban | 8965 | 6423 | 22.1 | 8242 | 6212 | 22.6 |
| Rural | 19,850 | 22,670 | 77.9 | 17,759 | 21,328 | 77.4 |
| Region | ||||||
| Barisal | 3313 | 1685 | 5.8 | 3313 | 1685 | 6.1 |
| Chittagong | 5876 | 6472 | 22.2 | 5876 | 6472 | 23.5 |
| Dhaka | 5406 | 9354 | 32.2 | 5406 | 9354 | 34.0 |
| Khulna | 3296 | 2605 | 9.0 | 3296 | 2605 | 9.5 |
| Rajshahi | 4124 | 4609 | 15.8 | 4124 | 4608 | 16.7 |
| Sylhet | 3986 | 2815 | 9.7 | 3986 | 2815 | 10.2 |
| Rangpur | 2814 | 1554 | 5.3 | |||
| SOCIOECONOMIC DETERMINANTS | ||||||
| Mother’s Age (years) (n = 29,087) | ||||||
| 15–24 | 14,271 | 14,576 | 50.1 | 13,102 | 13,920 | 50.6 |
| 25–34 | 11,890 | 11,953 | 41.1 | 10,571 | 11,239 | 40.8 |
| 35–49 | 2634 | 2558 | 8.8 | 2308 | 2375 | 8.6 |
| Mother working status (n = 29,090) | ||||||
| Not working | 23,132 | 23,095 | 79.4 | 20,648 | 21,719 | 78.9 |
| Working | 5679 | 5995 | 20.6 | 5351 | 5818 | 21.1 |
| Mother BMI (kg/m2) (n = 28,939) | ||||||
| ≤18 | 6329 | 6360 | 21.9 | 5597 | 5967 | 21.7 |
| 19–25 | 18,595 | 19,064 | 65.5 | 16,905 | 18,090 | 65.7 |
| 25+ | 3724 | 3515 | 12.1 | 3350 | 3337 | 12.1 |
| Maternal marital status | ||||||
| Currently married | 28,282 | 28,572 | 98.2 | 25,519 | 27,041 | 98.2 |
| Formerly married | 533 | 522 | 1.8 | 482 | 499 | 1.8 |
| Maternal highest level of education (n = 29,079) | ||||||
| No schooling | 12,235 | 12,712 | 43.7 | 10,930 | 11,969 | 43.5 |
| Primary | 12,775 | 12,939 | 44.5 | 11,524 | 12,246 | 44.5 |
| Secondary or more | 3785 | 3428 | 11.8 | 3527 | 3309 | 12.0 |
| Paternal highest level of education (n = 29,077) | ||||||
| No schooling | 13,898 | 14,440 | 49.6 | 12,413 | 13,588 | 49.3 |
| Primary | 9608 | 9697 | 33.3 | 8690 | 9178 | 33.3 |
| Secondary or more | 5291 | 4940 | 17.0 | 4880 | 4756 | 17.3 |
| Household Wealth Index | ||||||
| Rich | 5763 | 5118 | 17.6 | 5123 | 4860 | 17.7 |
| Middle | 11,526 | 11,684 | 40.2 | 10,568 | 11,178 | 40.6 |
| Poor | 11,526 | 12,291 | 42.3 | 10,310 | 11,502 | 41.8 |
| CHILD DETERMINANTS | ||||||
| Sex (n = 28,685) | ||||||
| Female | 13,861 | 14,019 | 48.2 | 12,547 | 13,285 | 48.2 |
| Male | 14,538 | 14,666 | 50.4 | 13,137 | 13,899 | 50.5 |
| Birth rank and birth interval | ||||||
| 2nd/3rd birth rank, more than 2 years interval | 10,675 | 10,935 | 37.6 | 9776 | 10,455 | 38.0 |
| 1st birth rank | 9948 | 9996 | 34.4 | 9164 | 9556 | 34.7 |
| 2nd/3rd birth rank, less than or equal to 2 years interval | 1924 | 1907 | 6.6 | 1677 | 1777 | 6.5 |
| 4th birth rank, more than 2 years interval | 5178 | 5200 | 17.9 | 4453 | 4787 | 17.4 |
| 4th birth rank, less than or equal to 2 years interval | 1090 | 1056 | 3.6 | 931 | 965 | 3.5 |
| Previous Death of Sibling | ||||||
| No | 28,067 | 28,352 | 97.5 | 25,318 | 26,832 | 97.4 |
| Yes | 748 | 742 | 2.6 | 683 | 708 | 2.6 |
| Number of children born (n = 29,011) | ||||||
| 1 | 7990 | 7999 | 27.5 | 7401 | 7675 | 27.9 |
| 2 | 8732 | 8868 | 30.5 | 8012 | 8485 | 30.8 |
| 3 | 5278 | 5412 | 18.6 | 4727 | 5110 | 18.6 |
| 4+ | 6733 | 6732 | 23.1 | 5795 | 6196 | 22.5 |
| Number of children under-five years | ||||||
| 1–2 | 17,873 | 18,113 | 62.3 | 16,467 | 17,365 | 63.1 |
| 3 or more | 10,942 | 10,981 | 37.7 | 9534 | 10,175 | 37.0 |
| MEDIA FACTORS | ||||||
| Watches television every week (n = 29,011) | ||||||
| Yes | 16,123 | 16,080 | 55.3 | 14,775 | 15,421 | 56.0 |
| No | 12,688 | 13,011 | 44.7 | 11,224 | 12,116 | 44.0 |
| Listens to radio every week (n = 29,088) | ||||||
| Yes | 5158 | 5385 | 18.5 | 5019 | 5305 | 19.3 |
| No | 23,650 | 23,703 | 81.5 | 20,975 | 22,229 | 80.7 |
| Reads newspaper (n = 29,075) | ||||||
| Yes | 4501 | 4115 | 14.1 | 4054 | 3902 | 14.2 |
| No | 24,291 | 24,960 | 85.8 | 21,930 | 23,621 | 85.8 |
| ENVIRONMENTAL FACTOR | ||||||
| Type of cooking fuel (n = 26,325) | ||||||
| Solid fuel | 2995 | 2943 | 10.1 | 2644 | 2846 | 10.3 |
| Non-solid fuel | 23,140 | 23,382 | 80.4 | 20,871 | 22,018 | 80.0 |
&Weighted for the sampling probability; n& weighted ‘n’
*percentage did not add up to 100% because of missing values.
(a) Overall Bangladesh population
Rates and predictors of stillbirths
As shown in Figure 1(a) (with Rangpur), the rate of stillbirth was 37 [95% confidence interval (CI): 32, 42] per 1000 births in 2004; 30 (95% CI: 25, 35) per 1000 births in 2007, 26 (95% CI: 23, 29) per 1000 births in 2011 and 21 (95% CI: 18, 25) per 1000 births in 2014. From 2004 to 2014, the overall rate of stillbirth was 28 (95% CI: 22, 34) per 1000 births. These results indicated that stillbirth decreased significantly in 2011 and 2014 compared to 2004, but in 2007 compared to 2011 and 2014, there was no significant decrease in stillbirth rate. In comparison to the population with Rangpur (Figure 1(a)), there was no significant differences in the rate of stillbirth in the population without Rangpur (Figure 1(b)).
Figure 1.
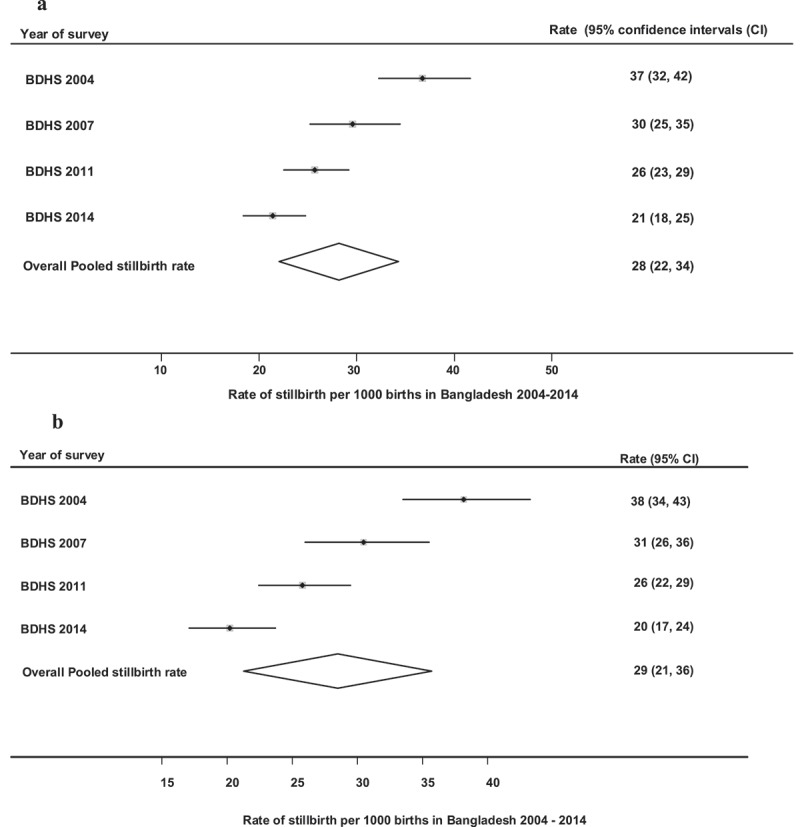
(a) Rate of stillbirth per 1000 births in Bangladesh (with Rangpur), 2004–2014. (b)Rate of stillbirth per 1000 births in Bangladesh (without Rangpur) 2004–2014.
The analysis showed that the rate of stillbirth was higher among rural mothers, older women, mothers with no schooling and mothers from poor households in Bangladesh (with Rangpur) [Table 2]. The stillbirth rate was significantly higher among households who reported non-solid fuel use and mothers who reported fourth birth order of child with more than 2 years’ birth interval.
Table 2.
Rate and univariate analysis of stillbirth by study factors in Bangladesh, 2004–2014.
| With Rangpur (a) |
Without Rangpur |
|||||||
|---|---|---|---|---|---|---|---|---|
| Rate 95%[CI] | Unadjusted odds ratio |
Rate 95%[CI] | Unadjusted odds ratio |
|||||
| VARIABLE | OR | (95% CI) | OR | (95% CI) | ||||
| COMMUNITY LEVEL FACTORS | ||||||||
| Cluster type | ||||||||
| Urban | 23 [19, 48] | 1.00 | 22 [18, 26] | 1.00 | ||||
| Rural | 30 [28, 43] | 1.36 | 1.13 | 1.65 | 30 [27, 32] | 1.39 | 1.14 | 1.69 |
| Region | ||||||||
| Barisal | 28 [19, 36] | 1.00 | 28 [19, 36] | 1.00 | ||||
| Chittagong | 26 [22, 30] | 0.93 | 0.65 | 1.34 | 26 [22, 30] | 0.93 | 0.65 | 1.35 |
| Dhaka | 27 [24, 30] | 1.01 | 0.71 | 1.44 | 27 [24, 30] | 1.02 | 0.71 | 1.45 |
| Khulna | 24 [18, 30] | 0.87 | 0.57 | 1.32 | 24 [18, 30] | 0.87 | 0.57 | 1.33 |
| Rajshahi | 33 [28, 39] | 1.26 | 0.87 | 1.82 | 33 [28, 39] | 1.26 | 0.87 | 1.83 |
| Sylhet | 33 [26, 39] | 1.26 | 0.85 | 1.88 | 33 [26, 39] | 1.27 | 0.85 | 1.90 |
| Rangpur | 36 [26, 46] | 1.37 | 0.88 | 2.14 | ||||
| SOCIOECONOMIC DETERMINANTS | ||||||||
| Mother’s Age (years)* | ||||||||
| 15–24 | 28 [26, 31] | 1.00 | 28 [25, 31] | 1.00 | ||||
| 25–34 | 28 [25, 31] | 0.99 | 0.85 | 1.15 | 28 [25, 31] | 0.99 | 0.85 | 1.16 |
| 35–49 | 31 [24, 38] | 1.09 | 0.85 | 1.40 | 31 [24, 38] | 1.11 | 0.86 | 1.44 |
| Mother working status | ||||||||
| Not working | 35 [31, 39] | 1.00 | 28 [26, 30] | 1.00 | ||||
| Working | 33 [26, 40] | 0.97 | 0.76 | 1.25 | 29 [25, 34] | 1.05 | 0.88 | 1.25 |
| Mother BMI (kg/m2)* | ||||||||
| ≤18 | 30 [25, 34] | 1.00 | 30 [25, 34] | 1.00 | ||||
| 19–25 | 29 [26, 31] | 0.97 | 0.82 | 1.15 | 28 [26, 31] | 0.95 | 0.80 | 1.14 |
| 25+ | 24 [19, 29] | 0.81 | 0.62 | 1.06 | 23 [18, 28] | 0.78 | 0.59 | 1.03 |
| Maternal marital status | ||||||||
| Currently married | 28 [26, 30] | 1.00 | 27 [25, 29] | 1.00 | ||||
| Formerly married | 63 [41, 85] | 2.28 | 1.56 | 3.32 | 59 [37, 81] | 2.18 | 1.46 | 3.23 |
| Maternal highest level of education* | ||||||||
| No schooling | 34 [31, 38] | 1.00 | 34 [30, 37] | 1.00 | ||||
| Primary | 25 [22, 28] | 0.72 | 0.62 | 0.84 | 25 [22, 28] | 0.73 | 0.62 | 0.85 |
| Secondary or more | 20 [15, 25] | 0.57 | 0.44 | 0.75 | 20 [15, 25] | 0.59 | 0.45 | 0.77 |
| Paternal highest level of education* | ||||||||
| No schooling | 33 [30, 36] | 1.00 | 32 [29, 35] | 1.00 | ||||
| Primary | 28 [24, 31] | 0.84 | 0.72 | 0.99 | 27 [24, 31] | 0.85 | 0.72 | 0.99 |
| Secondary or more | 17 [13, 21] | 0.51 | 0.40 | 0.65 | 17 [13, 20] | 0.51 | 0.40 | 0.65 |
| Household Wealth Index | ||||||||
| Rich | 18 [14, 21] | 1.00 | 17[14, 21] | 1.00 | ||||
| Middle | 30 [26, 33] | 1.71 | 1.35 | 2.17 | 29 [26, 33] | 1.74 | 1.35 | 2.23 |
| Poor | 32 [29, 35] | 1.85 | 1.46 | 2.35 | 31 [28, 35] | 1.87 | 1.46 | 2.40 |
| CHILD DEMOGRAPHICS | ||||||||
| Gender* | ||||||||
| Female | 14 [12, 16] | 1.00 | 15 [13, 17] | 1.00 | ||||
| Male | 13 [12, 16] | 0.97 | 0.79 | 1.19 | 14 [12, 17] | 0.97 | 0.80 | 1.19 |
| Birth rank and birth interval | ||||||||
| 2nd/3rd birth rank, more than 2 years interval | 11 [9,13] | 1.00 | 11 [9,13] | 1.00 | ||||
| 1st birth rank | 16 [14, 19] | 1.47 | 1.16 | 1.87 | 16 [14, 19] | 1.48 | 1.16 | 1.88 |
| 2nd/3rd birth rank, less than or equal to 2 years interval | 16 [10, 22] | 1.49 | 0.99 | 2.23 | 17 [11, 23] | 1.53 | 1.02 | 2.29 |
| 4th birth rank, more than 2 years interval | 102 [93, 111] | 9.91 | 8.05 | 12.20 | 98 [89, 107] | 9.12 | 7.38 | 11.25 |
| 4th birth rank, less than or equal to 2 years interval | 19 [10, 27] | 1.79 | 1.09 | 2.92 | 20 [11, 29] | 1.87 | 1.15 | 3.06 |
| Previous Death of Sibling | ||||||||
| No | 28 [26, 30] | 1.00 | 28 [26, 30] | 1.00 | ||||
| Yes | 37 [23, 51] | 1.31 | 0.88 | 1.96 | 38 [23, 52] | 1.36 | 0.90 | 2.04 |
| Number of children born* | ||||||||
| 1 | 35 [31, 39] | 1.00 | 34 [34, 38] | 1.00 | ||||
| 2 | 21 [18, 24] | 0.57 | 0.47 | 0.69 | 21 [17, 24] | 0.58 | 0.48 | 0.71 |
| 3 | 20 [17, 24] | 0.58 | 0.46 | 0.73 | 20 [16, 24] | 0.58 | 0.46 | 0.74 |
| 4+ | 25 [21, 29] | 0.70 | 0.57 | 0.85 | 25 [21, 29] | 0.73 | 0.59 | 0.89 |
| Number of children under-five years | ||||||||
| 1–2 | 33 [31, 36] | 1.00 | 32 [30, 35] | 1.00 | ||||
| 3+ | 20 [18, 23] | 0.61 | 0.52 | 0.71 | 21 [18, 23] | 0.63 | 0.53 | 0.74 |
| MEDIA FACTORS | ||||||||
| Watches TV every week* | ||||||||
| Yes | 25 [22, 27] | 1.00 | 24 [22, 27] | 1.00 | ||||
| No | 33 [30, 36] | 1.36 | 1.18 | 1.58 | 33 [30, 36] | 1.38 | 1.19 | 1.60 |
| Listens to radio every week* | ||||||||
| Yes | 31 [26, 36] | 1.00 | 31 [26, 36] | 1.00 | ||||
| No | 28 [26, 30] | 0.90 | 0.76 | 1.08 | 27 [25, 30] | 0.88 | 0.74 | 1.06 |
| Read newspaper* | ||||||||
| Yes | 19 [14, 23] | 1.00 | 18 [14, 22] | 1.00 | ||||
| No | 30 [28, 32] | 1.61 | 1.27 | 2.05 | 30 [27, 32] | 1.63 | 1.27 | 2.10 |
| ENVIRONMENTAL FACTOR | ||||||||
| Type of cooking fuel* | ||||||||
| Solid fuel | 18 [13, 23] | 1.00 | 28 [16, 39] | 1.00 | ||||
| Non-solid fuel | 31 [28, 33] | 1.56 | 1.18 | 2.04 | 37 [33, 41] | 1.34 | 0.82 | 2.18 |
*Rates did not add up because of missing values.
Note: 95% confidence intervals (CI) that include 1.00 indicate a non-significant result.
(a) Overall Bangladesh population
Multivariable analyses were performed with and without Rangpur division and showed that there was no substantial statistical difference between inclusion or removal of Rangpur division from the data sets. In this study, we provide interpretation of findings for all regions of Bangladesh (analyses with Rangpur division). In the multivariable analyses, the odds of stillbirth were significantly lower in educated mothers compared to those who had no schooling (Table 3). The risk of stillbirth was significantly higher among mothers from poorer households compared to those from rich households. Mothers with four or more children were significantly less likely to have a stillbirth compared to those who had one child. Mothers who did not read newspapers every week were significantly more likely to experience a stillbirth compared to those who read newspapers every week.
Table 3.
Predictors of stillbirth: adjusted odds ratio (AOR) in Bangladesh, 2004–2014.
| With Rangpur (a) |
Without Rangpur |
|||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | AOR | (95%CI) | P value | AOR | (95%CI) | P value | ||
| Year of survey | ||||||||
| 2004 | 1.00 | 1.00 | ||||||
| 2007 | 0.81 | 0.66 | 1.00 | 0.045 | 0.75 | 0.61 | 0.93 | 0.010 |
| 2011 | 0.54 | 0.44 | 0.66 | <0.001 | 0.52 | 0.42 | 0.65 | <0.001 |
| 2014 | 0.47 | 0.38 | 0.59 | <0.001 | 0.41 | 0.32 | 0.52 | <0.001 |
| Maternal highest level of education | ||||||||
| No schooling | 1.00 | 1.00 | ||||||
| Primary | 0.66 | 0.55 | 0.80 | <0.001 | 0.67 | 0.55 | 0.81 | <0.001 |
| Secondary or more | 0.59 | 0.43 | 0.82 | 0.002 | 0.63 | 0.44 | 0.89 | 0.008 |
| Household Wealth Index | ||||||||
| Rich | 1.00 | 1.00 | ||||||
| Middle | 1.30 | 1.01 | 1.66 | 0.040 | 1.51 | 1.14 | 2.01 | 0.004 |
| Poor | 1.47 | 1.13 | 1.90 | 0.004 | 1.62 | 1.21 | 2.16 | 0.001 |
| Number of children born | ||||||||
| 1 | 1.00 | 1.00 | ||||||
| 2 | 0.56 | 0.46 | 0.69 | <0.001 | 0.57 | 0.46 | 0.70 | <0.001 |
| 3 | 0.49 | 0.39 | 0.63 | <0.001 | 0.49 | 0.38 | 0.63 | <0.001 |
| 4+ | 0.53 | 0.43 | 0.66 | <0.001 | 0.51 | 0.40 | 0.65 | <0.001 |
| Number of children under-five years | ||||||||
| 1–2 | 1.00 | 1.00 | ||||||
| 3 or more | 0.74 | 0.63 | 0.88 | 0.001 | 0.76 | 0.63 | 0.91 | 0.003 |
| Read newspaper | ||||||||
| Yes | 1.00 | 1.00 | ||||||
| No | 1.34 | 1.02 | 1.76 | 0.037 | 1.38 | 1.03 | 1.86 | 0.033 |
Independent variables adjusted for community and socio-economic, child, media and environmental factor.
(a) Overall Bangladesh population
Discussion
The study found that the rates of stillbirth were lower in 2014 compared to 2004. Stillbirth rates were higher in rural areas compared to urban areas in Bangladesh, and low maternal education, poor household, and having one child (primiparity) were significant predictors of stillbirth in Bangladesh. A further stratified analysis (with or without Rangpur division) showed no substantial statistical differences in the results.
The finding that stillbirth declined during the decade 2004–2014 is consistent with previous studies which reported lower rates of stillbirth in Bangladesh between 2009 and 2015 [11,12] and from 1990 to 2015 [1]. The reduction in the rates of stillbirth in Bangladesh has been attributed to a range of maternal and newborn interventions and socioeconomic policies. These include overall economic growth; improved education and social empowerment of women; increased health sector financing and investment; the scale-up of family planning services; and increased access to skilled birth attendants and expansion of the private health sector [22]. The marked improvement in child survival may also be due to the broader influence of programmatic commitments to the MDG’s between 1990 and 2015. Notably, the United Nations reported that Bangladesh was among the few countries worldwide to meet MDG-4 and MDG-5 (reduction of under-5 and maternal mortalities) [3]. While under-5 and maternal mortality rates are not direct measures of stillbirth rate, improvement in appropriate antenatal care, skilled births assistance and newborn care have been described as the core solutions to ending preventable stillbirth [22,23].
Although our study observed no association between maternal age and stillbirth, previous studies from developing countries such as Sudan [24] and Nigeria [25] and developed countries such as Australia [26] and the USA [27] have reported a higher risk of stillbirths in women aged over 35 years. The higher rate of stillbirths among older women may be due to increased risk of congenital anomalies associated with advanced maternal age. In contrast, hospital-based studies conducted in India [28] and Nigeria [29] reported an increased risk of stillbirths in mothers aged less than 20 years. This finding may reflect a lack of education, limited autonomy to make household decisions and poor health-seeking behaviours among teenage women, as reported in Nigeria [30] and India [31]. Nevertheless, a population-based study from Taiwan reported an increased risk of stillbirths in both older (>40 years) and younger mothers (<20 years) [32].
Consistent with previous studies conducted in developing countries, from rural Bangladesh to Uganda [10,11,33,34], this study showed that stillbirth rates were higher among mothers with no formal education compared to educated mothers. A study conducted in Norway indicated that stillbirth rates were higher in Norwegian women with fewer years of education, but not among Pakistani immigrant women in Norway [24]. In addition, our study found that mothers from poor households were more likely to experience stillbirths compared to those from rich households. A link between poverty and higher rates of stillbirth has been documented in developing countries [35,36], and a combination of no formal education associated with low-income family income may act as a major obstacle to timely and appropriate decision to seek early medical care in pregnant women. Our study provides supportive evidence that a lack of maternal education is associated with an increased risk of stillbirth in Bangladesh. This finding will assist public health campaigners advocating for targeted socio-educational initiatives to increase female education in Bangladesh.
In Bangladesh, the proportion of women who give birth at home with assistance from a traditional birth attendant (TBA) remains high [17], highlighting the poor uptake of appropriate perinatal health services such as antenatal care (ANC) and birth assistance from skilled health professionals. Antenatal care is an essential public health intervention and is recommended for all pregnant women worldwide by the WHO, based on evidence underpinning its importance in improving maternal and child health outcomes. However, in rural Bangladesh in particular, a range of factors have been linked with the persistent use of home birthing with TBA’s [37] including; traditional beliefs, poverty, religious fallacy, poor road networks, limited knowledge on the importance of healthcare services and a shortage of skilled health workers. Bangladesh would likely see further substantial improvements in child survival by implementing interventions that increase access to, and use of perinatal services, particularly among mothers in rural settings and other high-risk groups.
This study revealed that the risk of stillbirth was lower in mothers who had more than two children compared to those with one child, consistent with findings from previous studies, which indicated that stillbirth rates were higher among primiparous women [26,38]. In this setting this could be partly attributed to the young age of first-time mothers which is also a known risk for stillbirth, and lower use of health services and knowledge of the importance of timely and routine ANC.
The study findings have policy implications for public health experts, policy decision-makers, health administrators and developmental partners in Bangladesh. The Lancet Series [2,4,8] suggest a roadmap for ending preventable stillbirths. These include stronger independent accountability within countries, the establishment of stillbirth prevention strategic plans, empowerment of women and families, ensuring skilled birth attendance in health facilities, reduction in stigma associated with stillbirths and improvement in bereavement care. Achievement of SDG-3.2 (end preventable deaths of newborns and children under-five years of age by 2030) appears feasible in Bangladesh given the country’s MDGs achievement, however, targeted financial investment and strong political commitment are required. Furthermore, achievement of SDG-3.2 in Bangladesh would require collaborative efforts among various government and non-government agencies at both national and sub-national levels, as well as drawing experiences and capacities from the implementation of the MDGs agenda.
Strengths and limitations
The following limitations should be considered when interpreting the study findings. First, the study used cross-sectional data, and a temporal association between exposure variables and the outcome cannot be determined. Second, the diagnosis of stillbirth was based on self-report, and this is a likely source of recall bias as respondents may incorrectly recall the gestational age they experienced a stillbirth. Third, data on other potential predictors of stillbirths (such as antepartum and intrapartum events, congenital anomalies or maternal drug use) as reported elsewhere [39] were not available. This latter information would have provided an additional contextual understanding of determinants of stillbirths in Bangladesh. Fourth, the study used pooled cross-sectional data, where population characteristics may differ over time. However, we adjusted for period and intra-cluster variability [40]. Additional information on the broader limitations of the DHS data utilisation has been described elsewhere [41].
Despite these limitations, the study has several specific strengths. First, selection bias is unlikely to affect the study findings, given the nationally representative sample and the high response rates that averaged 98%. Second, the BDHS used standardised questionnaires for data collection that provides population-based information on maternal and child health over time, allowing comparability across populations and time. Third, the data were collected by high-quality interviewers, which reduces the potential effect of interviewer bias. Fourth, this study provides country-wide evidence on predictors of stillbirths to health experts who can advocate for interventions to improve child survival and health at the national level in Bangladesh.
Conclusion
Our analysis showed that rates of stillbirth were lower in 2014 compared to 2004 in Bangladesh, and risk factors for stillbirth were low maternal education, primiparity and poor household. These findings highlight the need for collaborative efforts to end poverty, ensure healthy lives for all, promote inclusive and equitable education, and empower women to improve child survival in Bangladesh. Drawing lessons from the implementation of MDGs would help accelerate progress towards achievement of ending preventable stillbirths in Bangladesh by 2030.
Biography
TA and KEA were involved in the conception and designed for this study; TA performed the analysis and contributed to the manuscript draft. FAO interpreted results, drafted the original manuscript and critically revised the final manuscript. KEA, GJS, ANP, MAH, HM, MJD and CRG provided data analysis and interpretation advice, and revised drafts of the manuscript. All authors read and approved the final manuscript.
Responsible Editor Stig Wall, Umeå University, Sweden
Funding Statement
None.
Acknowledgments
The authors are grateful to Measure DHS for providing the datasets for the analysis.
Disclosure statement
No potential conflict of interest was reported by the authors.
Ethics and consent
The study used existing survey datasets that are available online by application, with all identifier information removed. The surveys were approved by the Ethics Committee of the ICF International, USA and the National Research Ethics Committee of Bangladesh Medical Research Council (BMRC), Bangladesh. We obtained approval from Measure DHS to download and use the data for the study.
Paper context
Globally, stillbirth is a significant public health issue, particularly in developing countries such as Bangladesh. We examined nationally representative data to identify potential predictors of stillbirths in Bangladesh over a ten-year period. Our study found that stillbirth rates were higher in rural areas, and no maternal education, poor household and primiparity were predictors of stillbirths in Bangladesh. There is need for more collaborative action to end preventable deaths and improve child survival in Bangladesh.
References
- [1]. Wang H, Bhutta ZA, Coates MM, et al. Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2]. Lawn JE, Blencowe H, Waiswa P, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet. 2016;387:587–603. [DOI] [PubMed] [Google Scholar]
- [3]. United Nations The millennium development goals report 2015. New York: United Nations; 2015. [Google Scholar]
- [4]. Heazell AE, Siassakos D, Blencowe H, et al. Stillbirths: economic and psychosocial consequences. Lancet. 2016;387:604–616. [DOI] [PubMed] [Google Scholar]
- [5]. Mistry H, Heazell AE, Vincent O, et al. A structured review and exploration of the healthcare costs associated with stillbirth and a subsequent pregnancy in England and Wales. BMC Pregnancy Childbirth. 2013;13:236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Gold KJ, Sen A, Xu X.. Hospital costs associated with stillbirth delivery. Matern Child Health J. 2013;17:1835–1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. Tarricone R. Cost-of-illness analysis: what room in health economics? Health Policy (New York). 2006;77:51–63. [DOI] [PubMed] [Google Scholar]
- [8]. Frøen JF, Friberg IK, Lawn JE, et al. Stillbirths: progress and unfinished business. Lancet. 2016;387:574–586. [DOI] [PubMed] [Google Scholar]
- [9]. United Nations Sustainable development - knowledge platform: united nations; 2017. [cited 2017 May 16]. Available from: https://sustainabledevelopment.un.org/sdg3. [Google Scholar]
- [10]. Cherry N, Shaikh K, McDonald C, et al. Stillbirth in rural Bangladesh: arsenic exposure and other etiological factors: a report from Gonoshasthaya Kendra. Bull World Health Organ. 2008;86:172–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11]. Owais A, Faruque ASG, Das SK, et al. Maternal and antenatal risk factors for stillbirths and neonatal mortality in rural Bangladesh: a case-control study. PLoS One. 2013;8:e80164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12]. Nahar S, Rahman A, Nasreen HE. Factors influencing stillbirth in Bangladesh: a case–control study. Paediatr Perinat Epidemiol. 2013;27:158–164. [DOI] [PubMed] [Google Scholar]
- [13]. Say L, Donner A, Gülmezoglu AM, et al. The prevalence of stillbirths: a systematic review. Reprod Health. 2006;3:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14]. Ogbo FA, Page A, Idoko J, et al. Diarrhoea and suboptimal feeding practices in Nigeria: evidence from the national household surveys. Paediatr Perinat Epidemiol. 2016;30:346–355. [DOI] [PubMed] [Google Scholar]
- [15]. Ok E, Ke A, Mj D, et al. Risk factors for postneonatal, infant, child and under-5 mortality in Nigeria: a pooled cross-sectional analysis. BMJ Open. 2015;5:e006779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16]. Ogbo FA, Agho K, Ogeleka P, et al. Infant feeding practices and diarrhoea in sub-Saharan African countries with high diarrhoea mortality. PLoS One. 2017;12:e0171792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17]. National Institute of Population and Training Mitra and Associates D [Bangladesh], ICF International Bangladesh demographic and health survey 2013. In: National Institute of Population and Training, editor. Maryland, USA: National Institute of Population and Training and ICF International; 2014. [Google Scholar]
- [18]. Titaley CR, Dibley MJ, Agho K, et al. Determinants of neonatal mortality in Indonesia. BMC Public Health. 2008;8:232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19]. Kembo J, Van Ginneken JK. Determinants of infant and child mortality in Zimbabwe: results of multivariate hazard analysis. Demogr Res. 2009;21:367–384. [Google Scholar]
- [20]. Abir T, Agho KE, Page AN, et al. Risk factors for under-5 mortality: evidence from Bangladesh demographic and health survey, 2004–2011. BMJ Open. 2015;5:e006722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21]. Chowdhury AH, Islam SS, Abdul Karim D. Covariates of neonatal and post-neonatal mortality in Bangladesh. Global J Human-Social Sci Res. 2013;13:7–14. [Google Scholar]
- [22]. Ministry of Health and Family Welfare, World Health Organisation, World Bank, Alliance for Health Policy and Systems Research Success factors for women’s and children’s health. Bangladesh: Ministry of Health and Family Welfare; 2015. [Google Scholar]
- [23]. Horton R, Samarasekera U. Stillbirths: ending an epidemic of grief. Lancet. 2016;387:515–516. [DOI] [PubMed] [Google Scholar]
- [24]. Ali AAA, Adam I. Anaemia and stillbirth in Kassala hospital, eastern Sudan. J Trop Pediatr. 2011;57:62–64. [DOI] [PubMed] [Google Scholar]
- [25]. Ukaegbe U, Nwogu-Ikojo E, Ezegwui H, et al. Stillbirths at a tertiary medical centre in Enugu, Nigeria. Trop J Med Res. 2011;15:1–4. [Google Scholar]
- [26]. Gordon A, Raynes-Greenow C, McGeechan K, et al. Risk factors for antepartum stillbirth and the influence of maternal age in New South Wales Australia: a population based study. BMC Pregnancy Childbirth. 2013;13:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27]. Reddy UM, Ko C-W, Willinger M. Maternal age and the risk of stillbirth throughout pregnancy in the USA. Am J Obstet Gynecol. 2006;195:764–770. [DOI] [PubMed] [Google Scholar]
- [28]. Mukhopadhyay P, Chaudhuri R, Paul B. Hospital-based perinatal outcomes and complications in teenage pregnancy in India. J Health, Popul Nutr. 2010;28:494–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29]. Olusanya BO, Solanke OA. Predictors of term stillbirths in an inner-city maternity hospital in Lagos, Nigeria. Acta Obstet Gynecol Scand. 2009;88:1243–1251. [DOI] [PubMed] [Google Scholar]
- [30]. Onadeko M, Avokey F, Lawoyin T. Observations of stillbirths, birthweight and maternal haemoglobin in teenage pregnancy in Ibadan, Nigeria. Afr J Med Med Sci. 1996;25:81–86. [PubMed] [Google Scholar]
- [31]. Mukhopadhyay P, Chaudhuri R, Paul B. Hospital-based perinatal outcomes and complications in teenage pregnancy in India. J Health Popul Nutr. 2010;28:494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32]. Hu I-J, Chen P-C, Jeng S-F, et al. A nationwide survey of risk factors for stillbirth in Taiwan, 2001–2004. Pediatrics Neonatal. 2012;53:105–111. [DOI] [PubMed] [Google Scholar]
- [33]. Nankabirwa V, Tumwine JK, Tylleskär T, et al. Perinatal mortality in eastern Uganda: a community based prospective cohort study. PLoS One. 2011;6:e19674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34]. Assaf S, Khawaja M, DeJong J, et al. Consanguinity and reproductive wastage in the Palestinian Territories. Paediatr Perinat Epidemiol. 2009;23:107–115. [DOI] [PubMed] [Google Scholar]
- [35]. Lee AC, Mullany LC, Tielsch JM, et al. Community-based stillbirth rates and risk factors in rural Sarlahi, Nepal. Int J Gynecol Obstetrics. 2011;113:199–204. [DOI] [PubMed] [Google Scholar]
- [36]. Cripe SM, Phung TTT, Nguyen TPL, et al. Risk factors associated with stillbirth in Thai Nguyen Province, Vietnam. J Trop Pediatr. 2007;53:366–367. [DOI] [PubMed] [Google Scholar]
- [37]. Sarker BK, Rahman M, Rahman T, et al. Reasons for preference of home delivery with traditional birth attendants (TBAs) in Rural Bangladesh: a qualitative exploration. PLoS One. 2016;11:e0146161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38]. Flenady V, Koopmans L, Middleton P, et al. Major risk factors for stillbirth in high-income countries: a systematic review and meta-analysis. Lancet. 2011;377:1331–1340. [DOI] [PubMed] [Google Scholar]
- [39]. McClure EM, Pasha O, Goudar SS, et al. Epidemiology of stillbirth in low‐middle income countries: a global network study. Acta Obstet Gynecol Scand. 2011;90:1379–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40]. Park I, Lee H. Design effects for the weighted mean and total estimators under complex survey sampling. Qual Contr App Stat. 2006;51:381. [Google Scholar]
- [41]. Corsi DJ, Neuman M, Finlay JE, et al. Demographic and health surveys: a profile. Int J Epidemiol. 2012;41:1602–1613. [DOI] [PubMed] [Google Scholar]


