Abstract
Human papilloma virus (HPV) is a common virus that can cause genital warts and certain cancers. The HPV vaccine is effective in preventing many HPV-associated diseases, however, vaccination rates suggest many remain unprotected. This study examined successful strategies used by physicians to improve HPV vaccination rates.
Providers with above average vaccination rates were identified. A representative from each provider participated in an interview to identify strategies used to boost HPV vaccination.
Key strategies in ensuring vaccine completion were reminders, education, standing orders, and scheduling future vaccine appointments at time of first dose. Other successful strategies included coupling the HPV vaccine with adolescent vaccines, administering during well-visits, and recommending the vaccine as protection against cancer and genital warts.
Findings suggest successful and widely used methods among high performing providers in Louisiana, the majority of which should be easily reproducible with minimal resources to improve HPV vaccination rates.
INTRODUCTION
Human papillomavirus (HPV) is a common virus that has been shown to cause genital warts, as well as anogenital and oropharyngeal cancers.1 In fact, HPV is estimated to cause close to 27,000 cancers each year in the U.S.1 and an average of 1,429 cancers annually in Louisiana.2,3 Most cervical cancers are caused by HPV, but so are a majority of the cancers of the vagina, vulva, penis, anus, and throat.
The first HPV vaccine was approved by the Food and Drug Administration over a decade ago, and the various iterations of the vaccine have been shown to be effective in preventing cervical cancer and other HPV-associated cancers and genital warts. Vaccines are available for males and females ages 9–26, however, the federal Advisory Committee on Immunization Practices (ACIP) has recommended routine vaccination for male and female adolescents ages 11–12.4
Under the Affordable Care Act, most health plans must cover a defined set of preventive services with no cost-sharing by the patient, including HPV vaccination for children from age 11–21. The included health plans are Medicaid, the plans in the insurance marketplace, most small and large group plans, and most employer self-insured plans. While some plans existing before 2010 were grandfathered in and not required to provide the preventive services with no cost-sharing, the percentage of plans falling into this category is decreasing, and, over time, most plans will lose this status.5
Despite evidence that the vaccine is effective in reducing infection and its coverage by most insurances, rates remain below the Health People 2020 recommendation of 80%,6,7 suggesting that many in the U.S. remain unprotected. The 2015 National Immunization Survey (NIS) results for completing all three shots in the HPV series for females was 39.3% and for males was 30.5% in Louisiana,7 both of which are significantly lower than the Healthy People 2020 target of 80% vaccination coverage. In October 2016, the Centers for Disease Control and Prevention changed its recommendations to a two shot series for adolescents under 15.8 While this should ease some of the barriers associated with series completion, with only 60.3% of females and 49.5% of males initiating the series in Louisiana in 2015, there is still a great deal of room for improvement.9
Previous research examined various methods used to increase vaccine uptake.10–14 These strategies range from educating both the providers and parents/adolescents to system changes, such as implementing standing orders or a reminder recall system. The study by Cassidy et al. supports the benefit of provider recommendation; 78.3% of parents mentioned that a recommendation from the providers aided in their decision to vaccinate. This study, as well as others, illustrate the benefit of patient reminders.10–14 Other studies have found that shot records helped to improve vaccination rates.11,14
In examining vaccination providers in Louisiana, it was obvious that some providers were having better HPV vaccination outcomes compared to other providers in the state (unpublished data). So what strategies are pediatricians and other healthcare providers in Louisiana using to increase the HPV vaccination rate and how can these strategies be used in any practice? The intent of this study was to discover uncommon but successful strategies providers can implement in their practices at little to no cost to increase initiation and completion of the vaccine series.
METHODS
This study sought to identify uncommon but successful behaviors that lead to better outcomes in HPV vaccination. The purpose was to identify best practices used by top performers. This qualitative study was conducted by the Louisiana Cancer Prevention and Control Program (LCP) with assistance from the Louisiana Department of Health Office of Public Health Immunization Office. The Immunization Office identified providers with above average HPV vaccination rates based on total volume of vaccine administered compared to all providers in Louisiana. The volume of vaccine administered was determined by utilization of the immunization information system, Louisiana Immunization Network for Kids Statewide (LINKS), for inventory management. Three high-volume providers were identified in each of the nine public health regions in the state. Additional inclusion criteria were: 1) the key informant had to be 18 years or older, 2) be a healthcare provider or clinic director/administrator, and 3) providers must participate in Louisiana’s childhood immunization program and be English speaking. As a result, 28 providers were identified as having above average vaccine uptake. Of the 28 providers, 25 were pediatric clinics. The three remaining clinics offered services across age ranges. This study was approved by the Institutional Review Board.
The selected providers were contacted via letter from the Louisiana Immunization Office to explain the study and were asked if they agreed to be contacted by LCP. Contact information was then given to LCP to conduct key informant interviews.
Structured interviews were conducted with a representative from each of the twelve providers who participated in the study. The interviews were conducted using an interview guide developed by LCP to explore strategies providers used to increase HPV vaccine uptake. The interview guide included questions to elicit information on provider demographics and strategies used to increase HPV vaccination. General topics assessed were provider policies and procedures, provider-parent interaction, and provider strategies to increase HPV vaccination. Interviews were conducted over the phone and recorded with participant permission.
Statistical Analysis
Interviews were recorded for transcription and analyzed using NVivo11 qualitative analysis software. Interviews were linked with providers’ demographic data in NVivo. Each interview was independently coded. This was an iterative process. After completion of the independent coding, the authors came together to reviews the codes and identify common themes (Table 1). Differences were resolved through consensus.
Table 1.
Common themes
| Themes | Child Codes |
|---|---|
| Appointment | Patient given appointment for vaccination during current visit |
| Education |
|
| Insurance | Insurance is seen as a barrier or facilitator to receiving vaccines |
| Adolescent Vaccines | HPV vaccine is offered as an adolescent vaccine or along with other adolescent vaccines (Meningitis or Tdap)
|
| Prevent Cancer | Reason for getting HPV vaccine is cancer prevention |
| Protect | HPV vaccine is seen as protection against cancer or genital warts |
| Recommendation |
|
| Relationship | Building a relationship with patient aids in HPV vaccination |
| Reminders |
|
| Sexual Activity | HPV vaccine is associated with sexual activity |
| Shot Records | Clinic checks shot records to determine what vaccines patient is eligible for during visit |
| Standing Orders | Clinic has standing orders for vaccines, may or may not include HPV |
| Well Visit | HPV vaccine is talked about, offered or given during well visit |
RESULTS
Twelve of the 28 providers agreed to participate in the study. The 16 providers that did not participate either did not return calls to schedule an interview, chose not to participate, or a representative was not able to answer interview questions. The participants came from seven of the nine public health regions of the state and seven of the 64 parishes in the state. The sample consisted of providers whose patient populations were entirely or partially children, ages 0–18. Six providers had a patient population of 100% children. The remaining providers had patient populations of at least 85% children. The majority (79%) of the patient populations of the participating providers had family incomes below 200% of the federal poverty level.
Themes identified through the analysis are shown in Table 1. The interviews showed that high-performing providers used a variety of strategies to get parents and youth/adolescents to initiate and complete the three-dose HPV vaccine series: education, standing orders, reminders, and scheduling vaccine appointments during current appointment. Other successful strategies included coupling the HPV vaccine with adolescent vaccines, administering during well visits, recommending the vaccine, and indicating that the HPV vaccine protects against cancer (Figure 1).
Figure 1.
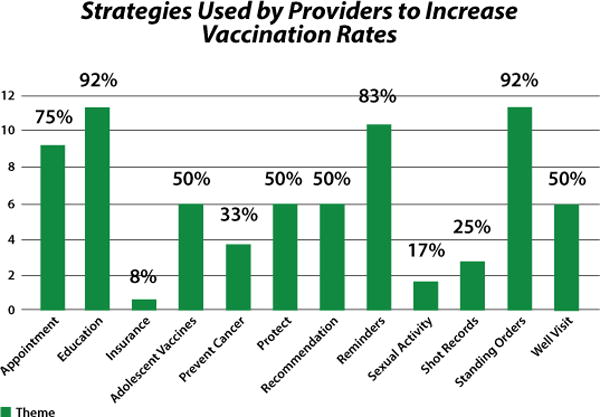
Strategies used by providers to increase vaccination rates
These researchers discovered that examining shot records helped providers stay abreast of patients that were eligible for the vaccine. As a result, patients and parents were able to receive education about the vaccine or the vaccine itself at well child visits or other doctor appointments.
The most frequently used strategies (Figure 1) were education (n=11) and standing orders (n=11), followed by reminders (n=10) and scheduling appointments for doses two and three during the current visit (n=8). Other strategies that were used moderately often include: offering the HPV vaccine with the other adolescent vaccines (n=6), indicating that the vaccine can protect against cancer (n=6), recommending the vaccine to patients (n=6), and offering the vaccine during well visits (n=6). The least frequent strategy reported by providers was informing parents that their insurance may cover the cost of the vaccine, thereby removing cost as a barrier (n=1) and only two providers indicated discussing the association of HPV infection with sexual activity.
Specific provider comments regarding strategies to increase HPV vaccination rates are detailed in Table 2.
Table 2.
What Louisiana Healthcare Providers are Saying
| Theme | Quote |
|---|---|
| Education | “We start educating parents then on what HPV is. I always give them the statistics on the amount of our the population estimated to already have HPV and not even be aware of it because it is typically asymptomatic so the parents are just very receptive…” (Interview 7) |
| Standing Orders | “We do have standing orders and yes it includes HPV vaccinations and all the vaccinations that we give.” (Interview 1) |
| Reminders |
“…we have a pamphlet about how they can sign up for text messaging… we give a reminder call about all of our appointments the day before so we try to remind them to come in and then we send out patient reminders to go through the LINKS system.” (Interview 12) “…we have what is called Televox and what it does is call the home and gives them friendly reminders of their appointment and we usually do it two or three days ahead of the appointment time… Then we have Televox give them an appointment for the next time and we have Televox to remind them of the appointment. So the Televox will call them and let them know that they have an appointment on whatever day it is and there it is located.” (Interview 6) |
| Appointments | “We would also schedule the next visit at the current visit and that really helps with completion…” (Interview 3) |
| Protects Against Cancer | “I let them know that it protects them against the cervical, oral, and anal cancers and that it takes all three (shots)…” (Interview 1) |
| Group with Other Vaccines | “…we just grouped into the 11 year old vaccine with tetanus and meningitis vaccine.” (Interview 3) |
| Include in Well Visit as Well as Any Other Visit | “We try to make sure that they are up to date on their wellness visits and when they do come in for their wellness visits their shot records are reviewed as well as when they come in for other office visits.” (Interview 10) |
| Make the Recommendation | “We start offering it when they come in for their 11 year old visits and most of them pretty much say that they will get it but each visit they come in and we see that they don’t have the Gardasil, then we offer it to them again and ask them if they have any questions and have the doctors back us up to try to get them vaccinated…” (Interivew 12) |
| Make the Recommendation | “We go over their shot records pretty much every visit. Whether they come in sick or well or whatever, we try to keep up with them. We have thousands of kids linked here so it’s very difficult. We try to make sure that they are up to date on their wellness visits and when they do come in for their wellness visits, their shot records are reviewed as well as when they come in for other office visits. If we see that they are past due for shots, even if they are sick and can’t give them, we tell then to schedule an appointment in 7–10 days for a recheck and possibly to get their shots.” (Interview 10) |
DISCUSSION
Studies have shown that a physician recommendation may be the most important factor in HPV vaccination adherence,15,16 and according to Reiter, et al., vaccine initiation is higher among parents who receive such recommendations.17 At least one study has found that pediatricians and family physicians are reluctant to recommend the vaccine because of the perceived necessity to discuss sexual activity in children.18 However, one systematic review found that only 6–12% of parents indicated a concern that the vaccine would promote sexual activity across the studies reviewed.16 Another study, a systematic review of European studies, found that parents of children who had received prior vaccines had higher rates of acceptance of the HPV vaccine in all 23 studies reviewed.19 Along with these studies, our findings support the idea that physicians may be more successful by including the vaccine in their general recommendations for vaccines and limiting such discussion only to those families who ask. In fact, the CDC suggests recommending the HPV vaccine in the same way that other child and adolescent vaccines are offered, that is without lengthy discussions on transmission.20
Many physicians miss the opportunity to recommend and administer the vaccine at crucial 11 or 12-year wellness visits.21 This study discovered several approaches to reducing these missed opportunities. This includes having standing orders for HPV vaccination and making that recommendation at every visit, well or sick. Other successful providers simply included the vaccine in the list of recommendations for the 11 or 12-year well visit. Combining both approaches should significantly decrease missed opportunities.
The findings of this study included the use of reminder calls and text messages and scheduling appointments for subsequent doses at the time of the first dose to increase adherence to series completion. While moving to a two-dose series should facilitate completion, further investigation is warranted on systems changes including alternative hours and sites for vaccination to overcome the barriers to completing the series.
While insurance coverage was not mentioned frequently by those interviewed, informing parents about their coverage could reduce hesitancy related to financial burdens. According to the 2015 Louisiana Health Insurance Survey, 59.6% of children in Louisiana are covered by Medicaid, which covers vaccination at no cost to parents.22 Of children in Louisiana, in 2016 less than 4% had no health insurance and less than 7.5% and dropping were covered by grandfathered plans and could be expected to have out of pocket expenses for vaccination.23 This leave approximately 90% of children in Louisiana fully covered for HPV vaccination.
There are some limitations to this study. The sample size is small and involves clinics with a large population of patients under 200% FPL and covered by Medicaid. Therefore, the same strategies may not be applicable to providers with patients who are above the federal poverty level, are largely covered by private insurance, have significantly smaller or larger patient populations or are located in rural or suburban area.
The practices are summarized in Figure 2. The next steps in this process will be to design ways to allow other providers to practice these behaviors and monitor the effectiveness of such practices. To that end, the Louisiana Immunization Work Group has been formed with the mission of improving immunization rates through coordinated activities and sharing of information. The partnership includes the Louisiana Department of Health Immunization Program, medical society chapters including the Louisiana Chapter of the American Academy of Pediatrics, cancer programs such as the American Cancer Society and the Louisiana Cancer Prevention and Control Programs, immunization partners, health systems, and insurance partners.
Figure 2.
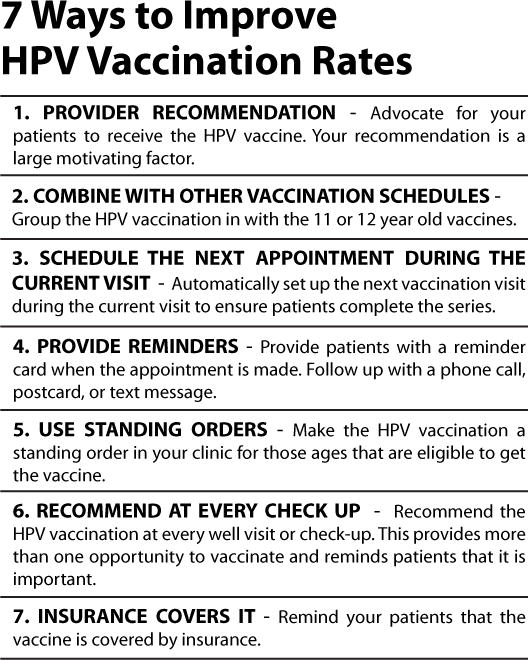
Seven Way to Improve HPV Vaccination Rates
CONCLUSION
This study uncovered successful and widely used methods among high performing providers in Louisiana. The majority of these strategies require simple system changes within the practice that should be easily reproducible to improve HPV vaccination rates. Further, these practices require minimal resources and most if not all can easily be implemented in any practice. Collaborative efforts are underway in Louisiana to disseminate these and other practices.
Acknowledgments
Supported in part by 1 U54 GM104940 from the National Institute of General Medical Sciences of the National Institutes of Health which funds the Louisiana Clinical and Translational Science Center. Supported in part by the Grant or Cooperative Agreement Number, 5 U58 DP003915, funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health, the Centers for Disease Control and Prevention or the Department of Health and Human Services.
Contributor Information
Donna Lisa Williams, Associated with the Louisiana State University Health Sciences Center, School of Public Health.
Courtney Suzanne Wheeler, Associated with the Centers for Disease Control and Prevention.
Michelle Lawrence, Associated with the Louisiana State University Health Sciences Center, School of Public Health.
Stacy Stevens Hall, Associated with the Louisiana Department of Health, Office of Public Health Immunization Program.
Michael Hagensee, Associated with the Louisiana State University Health Sciences Center, School of Medicine.
References
- 1.HPV and Cancer. Atlanta (GA): Centers for Disease Control and Prevention; 2016. http://www.cdc.gov/cancer/hpv/statistics/cases.htm. Accessed March 15, 2016. [Google Scholar]
- 2.Maniscalco L, Lefante C, Hsieh M, Andrews P, Pareti L, Mumphrey B, Ferguson DB, Schmidt B, Li X, Peterson L, O’Flarity M, Lynch MA, Wu XC, editors. Cancer in Louisiana, 2009–2013. New Orleans: Louisiana Tumor Registry; 2015. Cancer in Louisiana; Vol. 31. [Google Scholar]
- 3.Saraiya M, Unger ER, Thompson TD, Lynch CF, Hernandez BY, Lyu CW, Steinau M, Watson M, Wilkinson EJ, Hopenhayn C, Copeland G, Cozen W, Peters ES, Huang Y, Saber MS, Altekruse S, Goodman MT, HPV Typing of Cancers Workgroup US assessment of HPV types in cancers: implications for current and 9-valent HPV vaccines. Journal of the National Cancer Institute. 2015;107:djv086. doi: 10.1093/jnci/djv086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control Prevention. FDA licensure of bivalent human papillomavirus vaccine (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP) MMWR Morb Mortal Wkly Rep. 2010;59(20):626–9. [PubMed] [Google Scholar]
- 5.Preventive Services Covered by Private Health Plans under the Affordable Care Act. The Henry J. Kaiser Family Foundation; 2015. http://kff.org/health-reform/fact-sheet/preventive-services-covered-by-private-health-plans. Accessed February 9, 2017. [Google Scholar]
- 6.Markowitz LE, Liu G, Hariri S, Steinau M, Dunne EF, Unger ER. Prevalence of HPV After Introduction of the Vaccination Program in the United States. Pediatrics. 2016;137(3):1–9. doi: 10.1542/peds.2015-1968. [DOI] [PubMed] [Google Scholar]
- 7.Healthy People 2020 Topics & Objectives. Immunization and Infectious Diseases. Objective IID-11.4. Increase the vaccination coverage level of 3 doses of human papillomavirus (HPV) vaccine for females by age 13 to 15 years. Objective IID-11.5. Increase the vaccination coverage level of 3 doses of human papillomavirus (HPV) vaccine for males by age 13 to 15 years. Washington (DC): Healthy People 2020; 2014. http://www.healthypeople.gov. Accessed March 15, 2016. [Google Scholar]
- 8.#Preteen Vax News. Centers for Disease Control and Prevention. 2016 Oct; Special Edition. [Google Scholar]
- 9.2015 NIS-Teen Vaccination Coverage Table Data. Atlanta (GA): Centers for Disease Control and Prevention; 2015. http://www.cdc.gov/vaccines/imz-managers/coverage/nis/teen/tables/14/tab01_iap_2014.pdf. Accessed September 21, 2016. [Google Scholar]
- 10.Cassidy B, Braxter B, Charron-Prochownik D, Schlenk EA. A quality improvement initiative to increase HPV vaccine rates using an educational and reminder strategy with parents of preteen girls. J Pediatr Health Care. 2014;28(2):155–64. doi: 10.1016/j.pedhc.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 11.Rand CM, Brill H, Albertin C, Humiston SG, Schaffer S, Shone LP, et al. Effectiveness of centralized text message reminders on human papillomavirus immunization coverage for publicly insured adolescents. J Adolesc Health. 2015;56(5 Suppl):S17–20. doi: 10.1016/j.jadohealth.2014.10.273. [DOI] [PubMed] [Google Scholar]
- 12.Niccolai LM, Hansen CE. Practice- and Community-Based Interventions to Increase Human Papillomavirus Vaccine Coverage: A Systematic Review. JAMA Pediatr. 2015;169(7):686–92. doi: 10.1001/jamapediatrics.2015.0310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fiks AG, Grundmeier RW, Mayne S, Song L, Feemster K, Karavite D, et al. Effectiveness of decision support for families, clinicians, or both on HPV vaccine receipt. Pediatrics. 2013;131(6):1114–24. doi: 10.1542/peds.2012-3122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moss JL, Reiter PL, Dayton A, Brewer NT. Increasing adolescent immunization by webinar: a brief provider intervention at federally qualified health centers. Vaccine. 2012;30(33):4960–3. doi: 10.1016/j.vaccine.2012.05.042. [DOI] [PubMed] [Google Scholar]
- 15.Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination amont US adolescents: a systematic review of the literature. JAMA Pediatrics. 2014;168(1):76–82. doi: 10.1001/jamapediatrics.2013.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brewer N, Fazekas K. Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Preventive Medicine. 2007;45:107–111. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 17.Reiter PL, Brewer NT, Gottlieb SL, McRee AL, Smith JS. Parents’ health beliefs and HPV vaccination of their adolescent daughters. Soc Sci Med. 2009;69(3):475–80. doi: 10.1016/j.socscimed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 18.Daley MF, Crane LA, Markowitz LE, Black SR, Beaty BL, Barrow J, et al. Human papillomavirus vaccination practices: a survey of US physicians 18 months after licensure. Pediatrics. 2010;126(3):425–33. doi: 10.1542/peds.2009-3500. [DOI] [PubMed] [Google Scholar]
- 19.Fernández de Cassadevante V, Cuesta J, Cantarero-Arévalo Dterminants in the uptake of the human papillomavirus vaccine: a systematic review based on European studies. Fontiers in Oncology. 2015;5:141. doi: 10.3389/fonc.2015.00141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tips and Timesavers for talking with parents about HPV vaccine. Atlanta (GA): Centers for Disease Control and Prevention; 2016. http://www.cdc.gov/hpv/hcp/answering-questions.html. Accessed June 22, 2016. [Google Scholar]
- 21.Whiteman H. Many doctors discouraging HPV vaccination, study finds. Medical News Today. 2015 Oct 22; [Google Scholar]
- 22.Barnes S, Terrell D, Virgets S, Henderson M. Louisiana Health Insurance Survey. Louisiana Department of Health and Hospitals 2015 [Google Scholar]
- 23.Claxton G, Rae M, Long M, Damico A, Sawyer B, Foster G, Whitmore H, Schapiro L. Employer Health Benefits 2016 Annual Survey. The Henry J Kaiser Family Foundation and the Health Research & Educational Trust. 2016 Sep 14; [Google Scholar]


