Abstract
Purpose
To report longitudinal changes over time after surgery in the topography of the optic disc, thickness of the circum papillary retinal nerve fiber layer (c-RNFL), and thickness of the macular ganglion cell complex (m-GCC) in a case of juvenile open angle glaucoma.
Observations
Case report based on one patient. After significant edema of the optic disc for 2 months, the cup depth and cup volume measured by Heidelberg retina tomograph images showed reversal, which lasted for 3 years. The c-RNFL thickness and m-GCC thickness measured by spectral domain optical coherence tomography first increased for a week and then continued to decrease until 6 months after operation. These two parameters reached a plateau after 3 years. The mean deviation of global visual field indices of the Humphrey visual field revealed a very mild reduction for this 3 year period.
Conclusions and importance
In juvenile onset glaucoma, changes in c-RNFL thickness and m-GCC thickness after operation were not consistent with changes in optic disc cupping. Changes in the thicknesses of the c-RNFL or m-GCC, rather than changes in the optic disc changes, may be good surrogate measures to confirm the effectiveness of glaucoma surgery.
Keywords: Reversal of cupping, Optical coherence tomography, Scanning laser tomography, Juvenile glaucoma
1. Introduction
Reversal of cupping in young patients is a widely recognized phenomenon. However, there has not been any documentation in the literature of cases using both OCT and HRT. Here, we present a case report demonstrating reversal of cupping documented by both spectral domain optical coherence tomography (SD-OCT) and Heidelberg retina tomography (HRT) as well as disc photos for a 3-year longitudinal course.
2. Case report
A 16-year-old Japanese boy without any relevant medical history was referred to Toho University Ohashi Medical Center in January 2011, complaining of decreased visual field in the left eye (OS). Written informed consent was obtained for publishing personal identifying information.
Onset was first noted 8 months prior with a remarkably increased intraocular pressure (IOP) OS. Despite receiving maximum tolerable doses of relevant medications, including oral acetazolamide, patient's IOP OS was not reduced. At first presentation, the IOP by Goldmann applanation tonometry was 19 mmHg in the right eye (OD) and 35 mmHg OS. The best-correct visual acuity was 30/30 in both eyes. The corneal diameter was 13.8 mm in OS and 12.8 mm in OD, and the thickness was 518 μm in both eyes. The pupil OS was found to be mydriatic and showed a weakened light reflux. Gonioscopy revealed grade IV angles bilaterally. Fundus examination revealed significant optic disc cupping OS and was within normal limits OD. The patient then underwent trabeculotomy with an adjunctive use of mitomycin C.
The patient's eyes were scanned using an SD-OCT (Optovue, CA, USA) for c-RNFL and m-GCC thicknesses and an HRT III (Heidelberg Engineering, Heidelberg, Germany) for disc morphological changes and fundus photos. All imaging modalities were performed 16 times for 3 years. The Humphrey visual field was also examined 8 times for 3 years.
The IOP OS decreased to 3–4 mmHg at 3 weeks after the operation. During this period, we did not observe any macular folds, choroidal effusions or corneal findings consistent with hypotony. Two months postoperation, the IOP OS stabilized to the mid-teens (14–17 mmHg) with medication; this stabilized IOP OS was sustained for 3 years with medication.
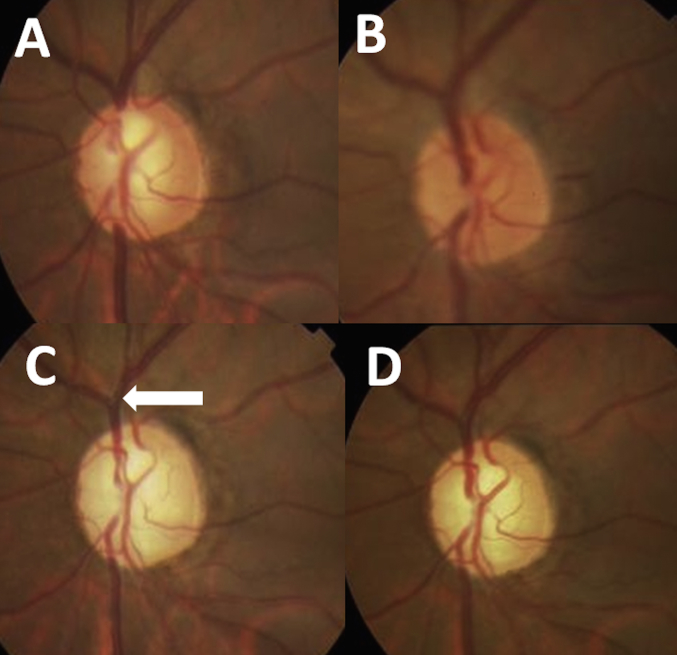
The optic disc OS showed severe cupping before operation (Fig. 1A), and significant edema (Fig. 1B) was observed just after the operation, lasting for 2 months. Thereafter, the rim width at 12 o'clock became thicker and the bent of vessels inside the cupping around 12 o'clock became milder than those before operation. (Fig. 1C), and these phenomena lasted for 3 years (Fig. 1D). After the optic disc edema disappeared, fundus images revealed that the distance from the optic disc edge to the vascular bifurcation was increased (Fig. 1C, arrow).
Fig. 1.
A–D, Optic disc photographs at the pre-operative visit (A) and 7 days (B), 6 months (C), and 36 months (D) after operation. The white arrow in C shows the increased distance from the optic disc edge to the vascular bifurcation.
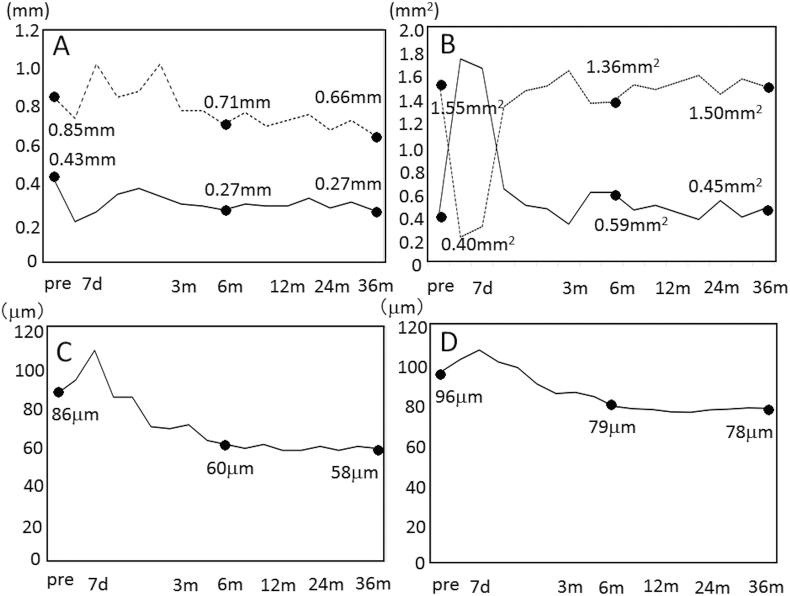
Reversal of the mean and maximum cup depth was sustained for 3 years after the operation (Fig. 2A). However, reversal of the cup area and rim area was sustained for only 3 months (Fig. 2B).
Fig. 2.
A, Mean cup depth (continuous line) and maximum cup depth (dotted line). B, Rim area (continuous line) and cup area (dotted line). C, circum papillary retinal nerve fiber layer thickness. D, macular ganglion cell complex thickness. The numbers in each graph show the values at the pre-operative visit and 6 months, and 36 months after the operation.
The thicknesses of the circum papillary retinal nerve fiber layer (c-RNFL) and macular ganglion cell complex (m-GCC) changed synchronously for 3 years (Fig. 2C and D), first increasing for 1 week after operation and then decreasing for up to 6 months after operation, reaching a value that was worse than the pre-operative value (Fig. 2C and D).
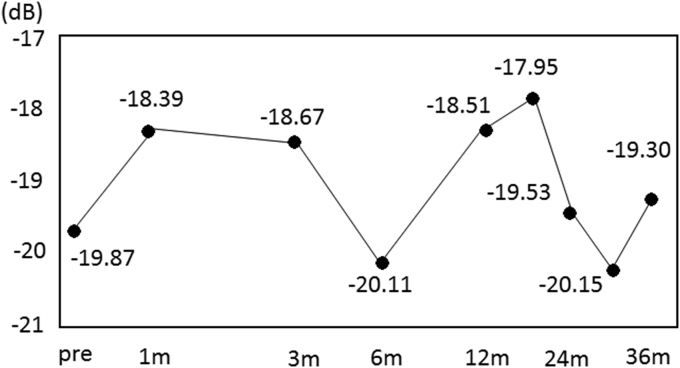
The MD slope revealed only a very mild reduction (−0.22 dB per year) for 3 years (Fig 3).
Fig. 3.
Change in the mean deviation of the Humphrey visual field.
3. Discussion
Here, we report a case of reversal of cupping documented over a 3-year longitudinal course. This case exhibited changes in c-RNFL thickness and m-GCC thickness after operation, which were not consistent with changes in optic disc cupping, in a case of juvenile glaucoma.
Reversal of cupping reportedly occurs more frequently in patients undergoing surgery than in patients receiving medical treatment [1], [2], [3], [4]. Most patients showing a 40% reduction in the IOP after glaucoma surgery reportedly show improved optic nerve morphology, as measured by the HRT [3]. The amount of improvement has been correlated highly with the percent reduction in the IOP [3]. But while reversal of cupping is associated with a lower IOP, it is not associated with improved visual function [5]. Chang and Grajewski reported a case in which a postoperative reduction in cupping and a subsequent increase in neuroretinal rim area are associated with a paradoxical thinning of the RNFL using SD-OCT [6]. In our case, the cup and rim areas were reversed for only a relatively short time and then worsened to the pre-operative level after 3 years. Only the cup depth exhibited a postoperative reduction after 3 years. On the other hand, the c-RNFL and m-GCC continued to decrease for 6 months under controlled IOP after the operation, indicating that visual field defects may be worsened after operation until the decrease in nerve fibers is halted. Therefore, changes in the thicknesses of the c-RNFL or m-GCC, rather than changes in the optic disc changes, may be good surrogate measures to confirm the effectiveness of glaucoma surgery.
As another interesting finding in our case, the retina and retinal vessels may shift with increases and decreases in the IOP because the vascular bifurcation clearly moved away from the disc edge in association with the reduction in the IOP.
4. Conclusion
In this case of juvenile open angle glaucoma, changes in c-RNFL and m-GCC thicknesses after operation were not consistent with changes in optic disc cupping.
References
- 1.Quigley H.A. The pathogenesis of reversible cupping in congenital glaucoma. Am. J. Ophthalmol. 1977;84:358–370. doi: 10.1016/0002-9394(77)90680-8. [DOI] [PubMed] [Google Scholar]
- 2.Quigley H.A. Childhood glaucoma: results with trabeculotomy and study of reversible cupping. Ophthalmology. 1982;89:219–226. doi: 10.1016/s0161-6420(82)34803-4. [DOI] [PubMed] [Google Scholar]
- 3.Lesk M.R., Spaeth G.L., Azuara-Blanco A., Araujo S.V., Katz L.J., Terebuh A.K., Wilson R.P., Moster M.R., Schmidt C.M. Reversal of optic disc cupping after glaucoma surgery analyzed with a scanning laser tomograph. Ophthalmology. 1999;106:1013–1018. doi: 10.1016/S0161-6420(99)00526-6. [DOI] [PubMed] [Google Scholar]
- 4.Yuen D., Buys Y.M. Disc photography and Heidelberg retinal tomography documentation of reversal of cupping following trabeculotomy. Graefes Arch. Clin. Exp. Ophthalmol. 2010;248:1671–1673. doi: 10.1007/s00417-010-1422-x. [DOI] [PubMed] [Google Scholar]
- 5.Parrish R.K., 2nd, Feuer W.J., Schiffman J.C., Lichter P.R., Musch D.C., CIGTS Optic Disc Study Group Five-year follow-up optic disc findings of the collaborative initial glaucoma treatment study. Am. J. Ophthalmol. 2009;147:717–724. doi: 10.1016/j.ajo.2008.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang T.C., Grajewski A.L. Paradoxical thinning of the retinal nerve fiber layer after reversal of cupping: a case report of primary infantile glaucoma. Indian J. Ophthalmol. 2013 Apr 3 doi: 10.4103/0301-4738.97092. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]