Abstract
Purpose
To describe a case of fungal endophthalmitis secondary to Curvularia after cataract surgery.
Observations
This case showed delayed and recalcitrant fungal endophthalmitis secondary to Curvularia despite treatment with pars plana vitrectomy, intravitreal antifungal therapy, and systemic antifungals.
Conclusions and importance
Curvularia-associated endophthalmitis should be considered in the differential diagnosis of delayed post-cataract endophthalmitis, especially in tropical or subtropical geographical areas. Awareness and early identification, timely removal of the nidi of sequestration, and prolonged antifungal treatments are important for the eradication of Curvularia-associated endophthalmitis.
Keywords: Endophthalmitis, Curvularia, Fungus
1. Introduction
Curvularia is a dematiaceous filamentous fungus, which is ubiquitous in soil and plants, especially in warm climates [1], [2]. Endophthalmitis associated with Curvularia is a rare event. We describe a case of delayed and recalcitrant fungal endophthalmitis secondary to Curvularia infection.
2. Case report
A 78-year old female presented with a one-week history of painless red eye with decreased best corrected visual acuity (BCVA) in the right eye (OD). There were no known inciting factors; however, she had uncomplicated cataract surgery in the affected eye three years prior. Her past medical history was significant for hypertension, hyperlipidemia, and rheumatoid arthritis (RA), and her family history was otherwise non-contributory.
On examination, BCVA was 20/50 OD with an intraocular pressure (IOP) of 23 mmHg. On the anterior segment examination, there were 1+ cells and flare in the anterior chamber without keratic precipitate or hypopyon. The posterior chamber intraocular lens was centered and clear with no deposits or posterior capsule opacity (PCO). On dilated fundus examination, there was no vitritis or cystoid macular edema. Slit lamp and fundus exam OS was normal. She was treated with topical difluprednate four times per day OD.
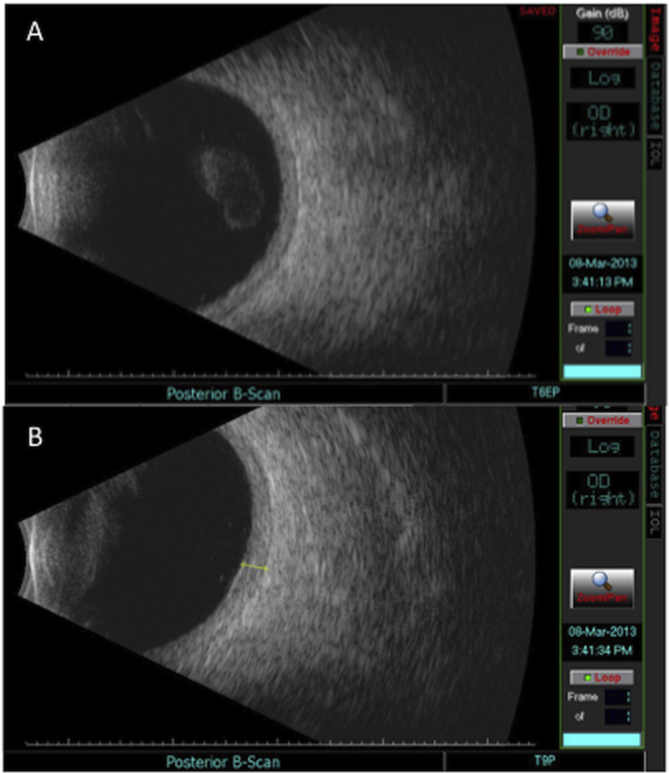
One month later, BCVA declined to 20/400 with increased anterior uveitis. Fibrin deposits on the posterior capsule were noted, as well as 2+ vitritis (Fig. 1A). B-scan ultrasound showed vitreous opacities with diffuse thickening of the retina and choroidal layers posteriorly (Fig. 2). The patient was initially treated with oral prednisone 60 mg daily for two weeks for suspected RA-associated scleritis by an outside provider, and endophthalmitis was not initially considered given the time delay since cataract surgery.
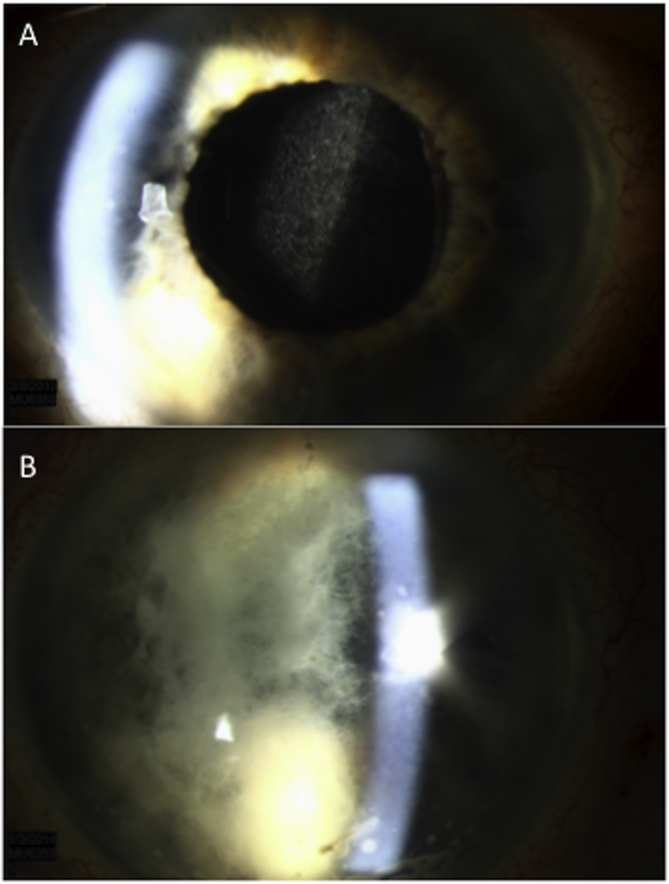
Fig. 1.
Slit-lamp photographs of the affected right eye. 1A - initial visit with significant posterior capsular opacification, fibrin deposits on the posterior capsule. 1B - 6-week follow-up with extensive fibrin throughout the anterior chamber.
Fig. 2.
B-scan ultrasound at one month follow-up after the initial presentation. 2A - scattered vitreous opacities consistent with dense vitritis. 2B - diffuse thickening of retina and the choroidal layers posteriorly (measuring approximately 2.2 mm).
The patient had counting fingers vision without any pain just two weeks later. There was 4+ cell and flare in the anterior chamber, but without a hypopyon. There were new focal white clumps of the posterior capsule. A 23-gauge pars plana vitrectomy was performed for presumed chronic endophthalmitis and the vitreous specimen was sent to microbiology for culture. During the procedure, intravitreal amphotericin (5 μg/0.1 cc), vancomycin (1 mg/0.1 cc), and ceftazidime (2.25 mg/0.1 cc) were administered. The patient was also started on oral voriconazole 200 mg twice per day. Vitreous cultures identified fungal Curvularia species.
Four weeks after surgery, the vision improved to 20/250. Repeat intravitreal amphotericin (5 μg/0.1 cc) was performed due to persistent inflammation. Oral voriconazole was continued and topical prednisolone acetate 1% drops four times daily was initiated. Two months later, the BCVA improved to 20/150. A moderate epiretinal membrane OD developed which was treated with vitrectomy and membrane peeling.
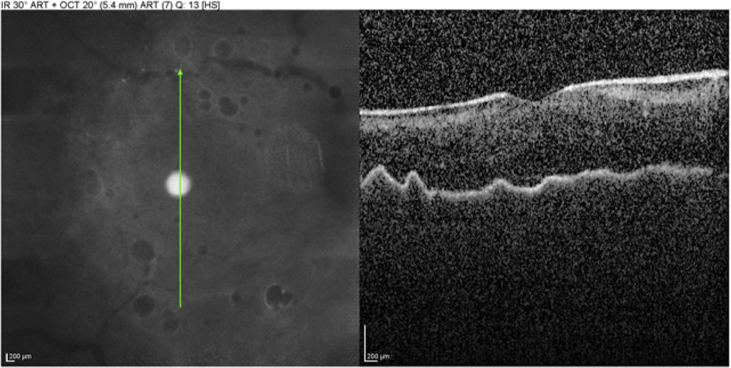
At one month follow-up, the BCVA worsened to 20/250 with a low IOP of 5 mmHg OD. A 360-degree iris neovascularization was seen. A laser posterior capsulotomy was performed for the dense PCO OD. The PCO contained small foci of hypo-pigmented deposits. She developed a hypotony maculopathy one month later with BCVA of 20/1250 (Fig. 3). A posterior subtenons injection of triamcinolone acetonide (40 mg) was done to increase the IOP. Six weeks later, the BCVA was worse with a light perception vision and an IOP of 4 mmHg. The AC showed extensive and dense fibrin (Fig. 1B). She had a persistent vitritis with extensive thickening and elevation of the retina/choroid layer (Fig. 4). Vitreous tap and repeat intravitreal Amphotericin (5 μg) was administered.
Fig. 3.
Optical coherence tomography at two months following membrane peeling surgery, complicated by hypotony with choroidal folds in the macula.
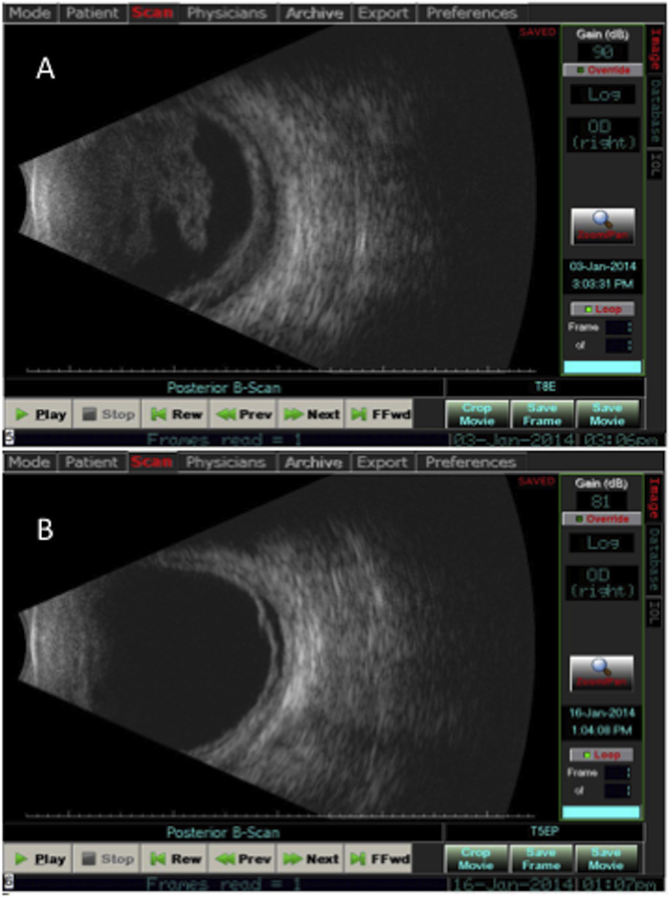
Fig. 4.
B-scan ultrasound at 6-week follow-up after posterior subtenon injection of triamcinolone acetonide (A) and after the third intravitreal injection of Amphotericin B (B). A. Vitreous opacities with extensive thickening of the retina/choroid. B. Diminished vitreous opacities with extensive thickening of the retina/choroid layer (2.1 mm in greatest thickness), and a shallow elevation of retina at 4 o’clock just posterior to equator).
On the subsequent one week follow-up, the vitreous appeared clear and the choroidal elevation resolved; however, the 360-degree extensive thickening of the retina/choroid layer persisted and a shallow exudative retinal detachment developed (Fig. 4). Intravitreal Amphotericin (5 μg/0.1 cc) was repeated. As retinal detachment was threatening the macula, pars plana vitrectomy with vitreous biopsy, scleral buckling, intraocular lens removal, intravitreal voriconazole (100 μg/0.1 cc) and oil insertion was done. The vitreous biopsy was once again positive for Curvularia species.
One-week post-operatively, her BCVA improved to hand motion with an IOP of 15 mmHg. The infectious disease service was consulted and she was admitted to hospital for intravenous voriconazole 100 mg daily for five days. She was placed on long-term oral voriconazole 300 mg twice per day and has been stable with hand motion vision since then. A written consent was obtained from the patient for publication of personal information (including medical record details).
3. Discussion
Endophthalmitis is a devastating diagnosis and bacteria are the main causes [3]. Only a small portion of cases is thought to be associated with fungal infections [4]. Curvularia, which lives in the soil and on plants, is found in tropical climates, and is spread by airborne spores [5]. To date, there are only eleven reported cases of endophthalmitis secondary to Curvularia. [6], [7], [8], [9], [10] Among those cases, eight patients had a preceding history of cataract surgery [6], [8], [9], [10], while four had a previous history of trauma [7], [9], [10]. Our case is unique due to its delayed and recalcitrant course.
Among all the cases with a preceding history of cataract surgery, the interval between surgery and initial symptom was between 1 and 5 months [6], [8], [9], [10]. In our case, the interval from surgery to initial symptom was three years, an unusually delayed-onset postoperative endophthalmitis associated with Curvularia.
In the literature, only two patients retained vision of 20/30 after aggressive antifungal treatment for Curvularia-associated endophthalmitis [8], [9]. Our patient most recently had hand motion vision, despite aggressive anti-fungal therapy both locally and systemically, as well as multiple surgeries. Hence, endophthalmitis due to Curvularia should be considered in the differential diagnosis of endophthalmitis post cataract surgery, especially in tropical or subtropical areas.
In cases of endophthalmitis caused by Curvularia, the correct diagnosis can be challenging for those who have a preceding cataract surgery. This may be related to its delayed-onset, or lack of knowledge about the typical clinical presentations of this condition due to its rarity. However, in the previous cases of Curvularia-associated endophthalmitis, PCO or posterior capsular plaque was described in 4 out of 8 patients who had an inciting event of cataract surgery [8], [10]. In our case, the PCO was also seen and may be an important sign to identify, or at least suspect, a diagnosis of endophthalmitis related to Curvularia.
In this case, the use of steroids (topical, oral, and periocular) without the concurrent anti-fungal coverage might have led to the activation or worsening of the underlying endophthalmitis secondary to Curvularia. Our case shows recalcitrant Curvularia endophthalmitis despite treatment with pars plana vitrectomy, intravitreal antifungal therapy, and systemic antifungals. It was likely that the intraocular lens and lens capsule were the nidi of the Curvularia infection, which should have been removed earlier on.
Oral administration of voriconazole can achieve an intravitreal concentration of 0.81 μg/ml, which is higher than 90% of minimum inhibitory concentration for Curvularia [11]. Hence, systemic voriconazole is a good option for Curvularia endophthalmitis. Oral administration of voriconazole 200 mg every 12 hours should be started when fungal etiology first suspected [12].
4. Conclusions
We describe a case of delayed and recalcitrant fungal endophthalmitis secondary to Curvularia despite treatment with pars plana vitrectomy, intravitreal antifungal therapy, and systemic antifungals. Curvularia-associated endophthalmitis should be considered in the differential diagnosis of delayed post-cataract endophthalmitis, especially in tropical or subtropical geographical areas. Awareness and early identification, timely removal of the nidi of sequestration, and prolonged antifungal treatments are important for the eradication of Curvularia-associated endophthalmitis.
Statement
The authors didn’t receive any grant support or research funding for this study. The manuscript has not been presented at any meeting.
Acknowledgements
A. Funding & Support: None. B. Financial & Proprietary Disclosure. Almeida: Allergan (Honoraria), Alcon (Honoraria), Genentech (Honoraria), Novartis (Honoraria). C. Statement about Conformity with Author Information: Full adherence to the Declaration of Helsinki and all Federal and State laws.
References
- 1.Rao K.V. Fungi from diversified habitats. Indian J. Bot. 1986;9:164–167. [Google Scholar]
- 2.Flournoy D.J., Mullins J.B., McNeal R.J. Isolation of fungi from rose bush thorns. J. Okla State Med. Assoc. 2000;93:271–274. [PubMed] [Google Scholar]
- 3.Benz M.S., Scott I.U., Flynn H.W., Jr., Unonius N., Miller D. Endophthalmitis isolates and antibiotic sensitivities: a 6-year review of culture-proven cases. Am. J. Ophthalmol. 2004;137:38–42. doi: 10.1016/s0002-9394(03)00896-1. [DOI] [PubMed] [Google Scholar]
- 4.Marangon F.B., Miller D., Giaconi J.A., Alfonso E.C. In vitro investigation of voriconazole susceptibility for keratitis and endophthalmitis fungal pathogens. Am. J. Ophthalmol. 2004;137:820–825. doi: 10.1016/j.ajo.2003.11.078. [DOI] [PubMed] [Google Scholar]
- 5.Wilhelmus K.R., Jones D.B. Curvularia keratitis. Trans. Am. Ophthalmol. Soc. 2001;99:111–132. [PMC free article] [PubMed] [Google Scholar]
- 6.Kaushik S., Ram J., Chakrabarty A., Dogra M.R., Brar G.S., Gupta A. Curvularia lunata endophthalmitis with secondary keratitis. Am. J. Ophthalmol. 2001;131:140–142. doi: 10.1016/s0002-9394(00)00648-6. [DOI] [PubMed] [Google Scholar]
- 7.Pathengay A., Miller D.M., Flynn H.W., Jr., Dubovy S.R. Curvularia endophthalmitis following open globe injuries. Arch. Ophthalmol. 2012;130:652–654. doi: 10.1001/archophthalmol.2011.1701. [DOI] [PubMed] [Google Scholar]
- 8.Pathengay A., Shah G.Y., Das T., Sharma S. Curvularia lunata endophthalmitis presenting with a posterior capsular plaque. Indian J. Ophthalmol. 2006;54:65–66. doi: 10.4103/0301-4738.21625. [DOI] [PubMed] [Google Scholar]
- 9.Berbel R.F., Casella A.M., de Freitas D., Höfling-Lima A.L. Curvularia lunata endophthalmitis. J. Ocul. Pharmacol. Ther. 2011;27:535–537. doi: 10.1089/jop.2011.0002. [DOI] [PubMed] [Google Scholar]
- 10.Rachitskaya A.V., Reddy A.K., Miller D., Davis J., Flynn H.W., Jr., Smiddy W., Lara W., Lin S., Dubovy S., Albini T.A. Prolonged Curvularia endophthalmitis due to organism sequestration. JAMA Ophthalmol. 2014:1123–1126. doi: 10.1001/jamaophthalmol.2014.1069. [DOI] [PubMed] [Google Scholar]
- 11.Hariprasad S.M., Mieler W.F., Lin T.K., Sponsel W.E., Graybill J.R. Voriconazole in the treatment of fungal eye infections: a review of current literature. Br. J. Ophthalmol. 2008;92:871–878. doi: 10.1136/bjo.2007.136515. [DOI] [PubMed] [Google Scholar]
- 12.Chhablani J. Fungal endophthalmitis. Expert Rev. Anti Infect. Ther. 2011;9:1191–1201. doi: 10.1586/eri.11.139. [DOI] [PubMed] [Google Scholar]