Abstract
Purpose
To report the detailed macular morphology documented by spectral-domain optical coherence tomography (SD-OCT) in a patient with retinitis pigmentosa (RP) and diabetic retinopathy (DR).
Observations
A 54-year-old man with a hemoglobin A1c level of 11.4% was referred for decreased visual acuity (VA) bilaterally (right eye, 20/100; left eye, 20/40). Funduscopy showed typical retinal findings of RP bilaterally. The macular area of both fundi showed retinal dot-and-blot hemorrhages, hard exudates. Time-domain OCT revealed macular edema in the right eye. The patient was diagnosed with RP accompanied by DR bilaterally. Five years after the first visit, the BCVAs remained 20/100 in the right eye and 20/40 in the left eye. SD-OCT showed that the retinas were thinner temporal to the maculas. The external limiting membrane line (ELM) and the ellipsoid zone of the photoreceptors line (EZ) was not visible in the foveal region in the right eye and temporal to the macula in both eyes. The image revealed the characteristic intraretinal and intrachoroidal hyrerreflective foci, the number of which increased corresponding to the extent of the disappearance of the ELM and EZ line with thinning of the outer nuclear layer (ONL). In addition, the image also showed a great number of the hyperreflective foci in the ONL and the choriocapillaris in the foveal region in the right eye compared with the left eye.
Conclusions
In the current case, the SD-OCT findings suggested that the characteristic hyrerreflective foci clinically observed in the fundi of a patient with RP accompanied by DR are present in the retinal layers and the choroid. In addition, the foci in the retinal and choroidal layers in the foveal region may increase as vision declines corresponding to the disappearance of the ELM and EZ line.
Keywords: Retinitis pigmentosa, Diabetic retinopathy, Spectral-domain optical coherence tomography, Retinal hyrerreflective foci, Choroidal hyrerreflective foci
1. Introduction
Retinitis pigmentosa (RP) and diabetic retinopathy (DR) are common diseases. However, very few cases have been reported in which DR was present in an eye with RP [1]. Arden reported that none of 55 patients with diabetes had DR with RP in a survey of patients with long-term diabetes mellitus and RP [2]. Therefore, the pathologies of both complicated eyes remain incompletely understood.
The recently developed high-resolution spectral-domain optical coherence tomography (SD-OCT) devices visualize more detailed anatomic macular morphologies and allow detailed in vivo visualization of the retinal and choroidal structures that approaches the histologic level. We present the case of a patient with RP accompanied by DR documented by SD-OCT (Spectralis HRA-OCT, Heidelberg Engineering, Heidelberg, Germany).
2. Case report
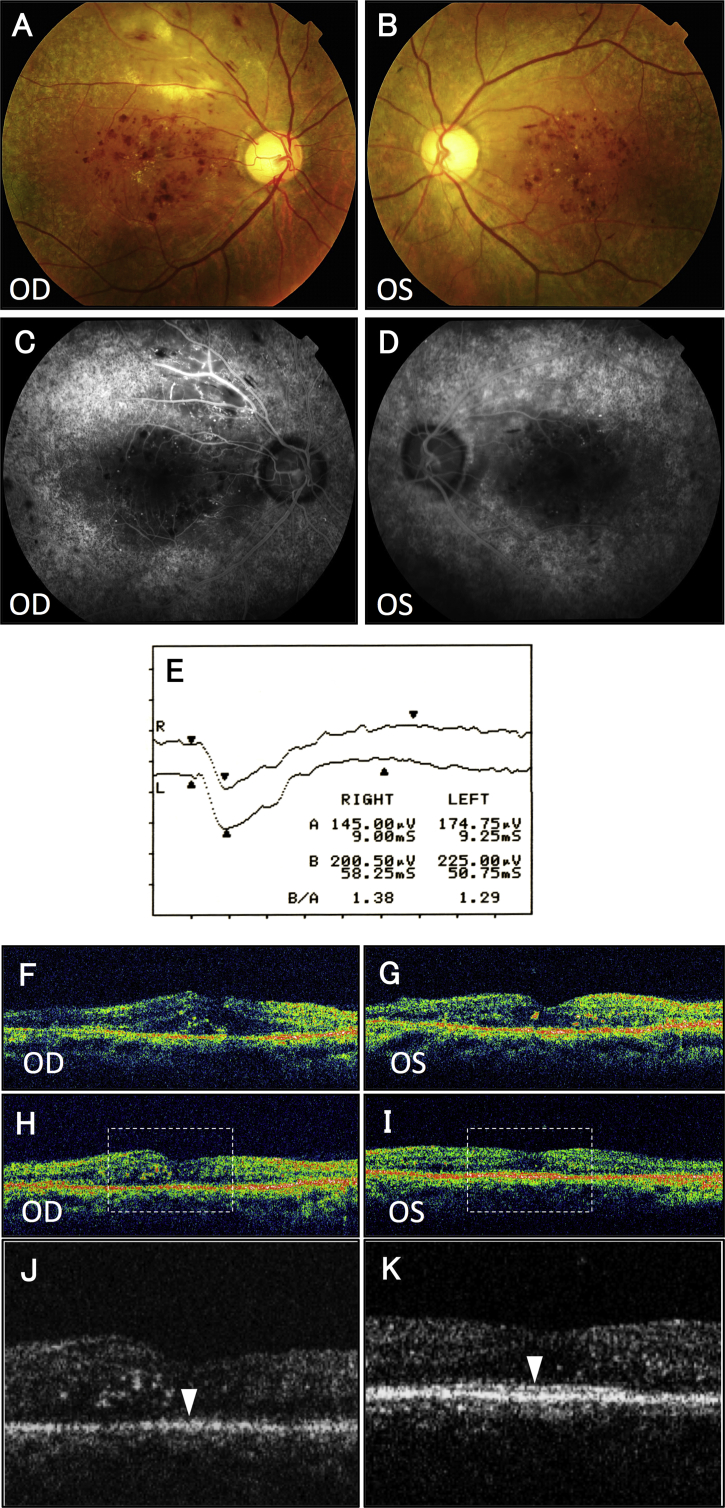
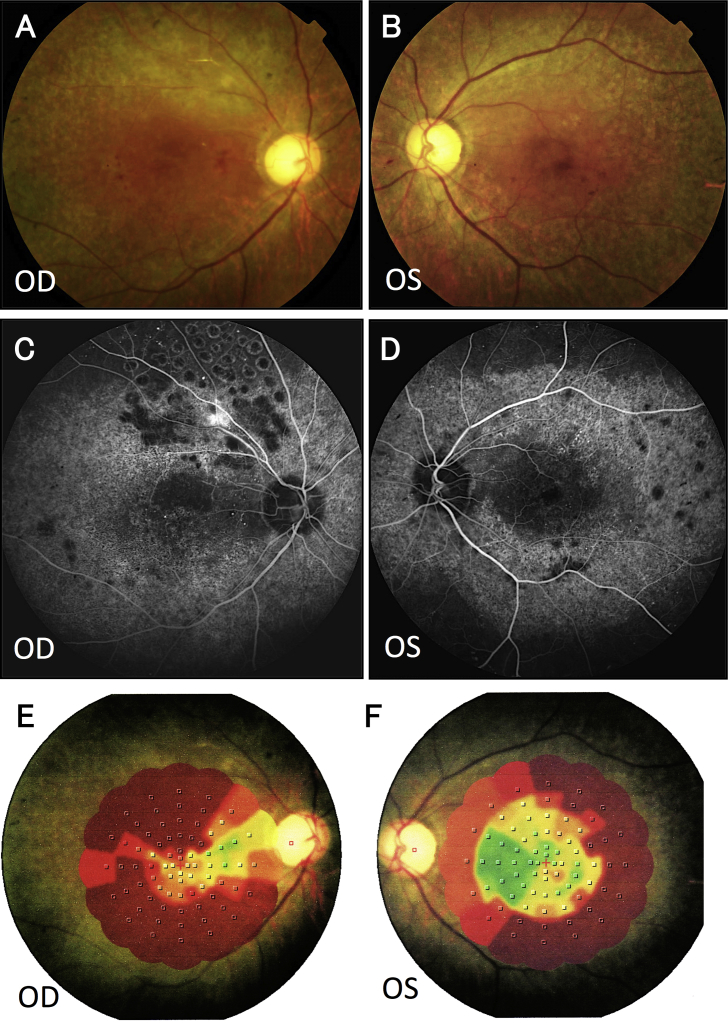
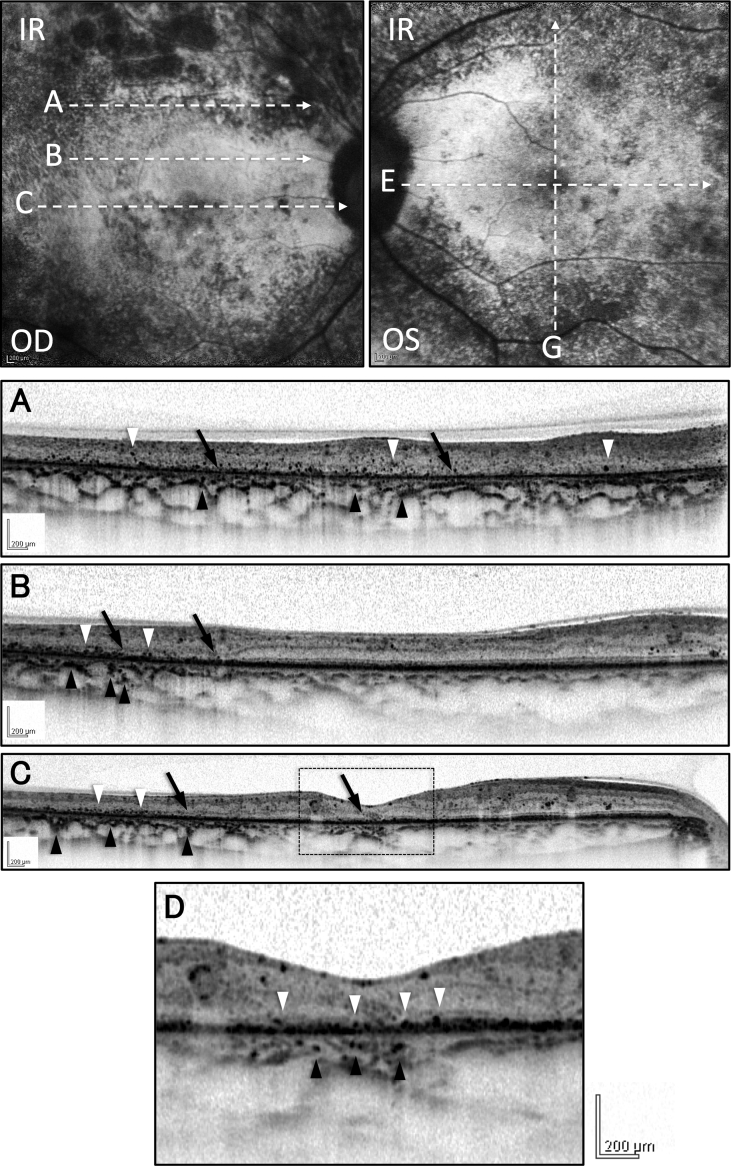
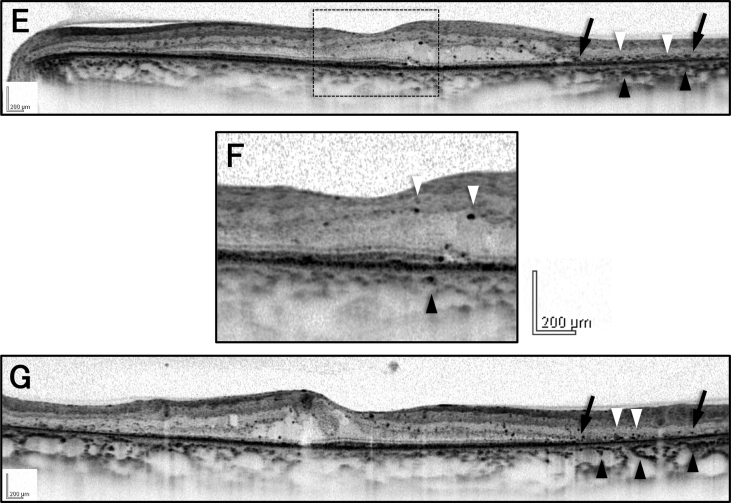
A 54-year-old man had a fasting blood sugar and hemoglobin A1c levels of 332 mg/dl and 11.4%, respectively. He presented with blurred vision bilaterally and was referred to our Retina Service for a detailed examination and tertiary care of the DR. His best-corrected visual acuities (BCVAs) were 20/100 in the right eye and 20/40 in the left eye. Funduscopic examination showed typical retinal findings of RP, i.e., retinal pigment epithelium (RPE) degeneration, bone spicule-like pigmentation, and attenuated retinal vessels in the mid-peripheral area bilaterally. The macular area of both eyes showed retinal dot-and-blot hemorrhages, hard exudates (Fig. 1A, 1B). Moreover, the patient appeared to have a great deal of hard exudates superior to the macula of the right eye (Fig. 1A). Fluorescein angiography showed hyperfluorescence in the mid-peripheral area that corresponded to the RPE degeneration, small hyperfluorescent spots from microaneurysms surrounding the fovea in both eyes (Fig. 1C, 1D). The angiogram of the right eye shows a large area of non-perfusion and clinical retinal ischemia with marked leakage of dye along the superotemporal retinal artery, which is not very typical of an isolated diabetic retinopathy (Fig. 1C). The electroretinography recording was subnormal bilaterally (Fig. 1E). The patient was diagnosed with RP accompanied by DR in both eyes. Time-domain OCT (TD-OCT: Stratus OCT; Carl Zeiss Meditec, Dublin, California, USA) revealed macular edema and serous foveal detachment in the right eye (Fig. 1F). The foveal contour and outer foveal layer in the left eye was well preserved (Fig. 1G). Central foveal thicknesses were 401 μm in the right eye and 245 μm left eyes. A diagnosis was made of diabetic macular edema (ME) in his right eye with retinitis pigmentosa assigned on the basis of these clinical symptoms and ocular signs. Posterior sub-Tenon injection of triamcinolone acetonide (40 mg) was performed for macular edema in the right eye. Photocoagulation was applied in the area of non-perfusion and clinical retinal ischemia superior to the macula. 3 month later, TD-OCT revealed the regression of ME and the foveal thickness was decreased to 316μm in the right eye (Fig. 1H) and the ellipsoid zone of the photoreceptors (EZ) line remained absent in the foveal lesion in the right eye (Fig. 1J). The EZ line could be seen in the foveal region in the left eye (Fig. 1K). Best-corrected visual acuity did not improve in the right eye. Five years after the first visit, HbA1c had improved to 6.4%. Therefore, the macular hemorrhage was decreased (Fig. 2A, 2B). The BCVAs remained 20/100 in the right eye and 20/40 in the left eye. Fluorescein angiography showed hyperfluorescence in the mid-peripheral area that corresponded to the RPE degeneration, small hyperfluorescent spots from microaneurysms surrounding the fovea in both eyes (Fig. 2C, 2D). The angiogram of the right eye also shows concentric constriction of hyperfluorescence corresponding to the RPE degeneration and retinal photocoagulation scars with diminished leakage of dye along the superotemporal retinal artery (Fig. 2C). Microperimetry visual field examination (Micro Perimeter 1, Nidek, Gamagori, Japan) showed concentric constriction of the field bilaterally and a paracentral scotoma in the right eye (Fig. 2E, 2F). SD-OCT revealed that the central foveal thicknesses were 158 μm in the right eye and 244 μm left eyes. SD-OCT also showed that the retina was thinner temporal to the macula in both eyes (Fig. 3. A, B, C, E, G). The external limiting membrane line (ELM) and the EZ line could not be seen in the foveal region in the right eye and temporal to the macula in the left eye (Fig. 3C, 3E). The image also revealed the characteristic intraretinal and intrachoroidal hyrerreflective foci. The number of retinal and choroidal hyrerreflective foci increased corresponding to the extent of the disappearance of the ELM and EZ line with thinning of the outer nuclear layer (ONL) (Fig. 3. A, B, C, E, G). In addition, the image also showed a great number of the hyperreflective foci in the ONL and the choriocapillaris in the foveal region in the right eye compared with the left eye (Fig. 3D, 3F).
Fig. 1.
Funduscopic examination shows typical retinal findings of retinitis pigmentosa, such as retinal pigment epithelium (RPE) degeneration, bone spicule-like pigmentation, and attenuated retinal vessels in the mid-peripheral area in both eyes. The macular areas of both fundus have retinal dot-and-blot hemorrhages, hard exudates (A, B). Moreover, the right eye appears to have a great deal of hard exudates superior to the macula (A). Fluorescein angiography shows hyperfluorescence in the mid-peripheral area that corresponding to the RPE degeneration, small hyperfluorescent spots from microaneurysms surrounding the fovea in both eyes (C, D). The angiogram of the right eye shows a large area of non-perfusion and clinical retinal ischemia with marked leakage of dye along the superotemporal retinal artery (C). The electroretinography recording is subnormal bilaterally (E). Time-domain OCT (TD-OCT: Stratus OCT; Carl Zeiss Meditec, Dublin, California, USA) shows macular edema and serous foveal detachment in the right eye (F). The foveal contour and outer foveal layer in the left eye is well preserved (G). Central foveal thicknesses are 401 μm in the right eye and 245 μm left eyes (F, G). TD-OCT reveals the regression of ME and the foveal thickness is decreased to 316μm in the right eye (H). Magnified images of the area outline by the dashed line in the TD-OCT image (H, I). The ellipsoid zone of the photoreceptors (EZ) remains absent in the foveal lesion in the right eye (J). The EZ line can be seen in the foveal region in the left eye (K). OD, right eye; OS, left eye.
Fig. 2.
Funduscopic examination shows that the macular hemorrhage was decreased in both eyes (A, B). Fluorescein angiography shows hyperfluorescence in the mid-peripheral area that corresponding to the RPE degeneration, small hyperfluorescent spots from microaneurysms surrounding the fovea in both eyes (C, D). The angiogram of the right eye also shows concentric constriction of hyperfluorescence corresponding to the RPE degeneration and retinal photocoagulation scars with diminished leakage of dye along the superotemporal retinal artery (C). Microperimetry visual field examination shows concentric constriction of the field bilaterally and a paracentral scotoma in the right eye (E, F). OD, right eye; OS, left eye.
Fig. 3.
Spectral-domain optical coherence tomography (SD-OCT) images are extracted from the areas of the dashed arrows on the infrared fundus images. The SD-OCT images show that the retina appears thinner temporal to the macula in both eyes. SD-OCT reveals that the central foveal thicknesses were 158 μm in the right eye and 244 μm left eyes (A, B, C, E, G). The external limiting membrane line (ELM) and the ellipsoid zone of the photoreceptors (EZ) line are not be seen in the foveal region in the right eye (C) and temporal to the macula in both eyes (C, E) (arrows). The images also show the characteristic intraretinal hyperreflective foci (white arrowheads) and intrachoroidal hyperreflective foci (black arrowheads) in both eyes (A–G). The number of retinal and choroidal hyrerreflective foci increased corresponding to the extent of the disappearance of the ELM and EZ line with thinning of the outer nuclear layer (ONL) (A–G). A magnified image of the area outline by the dashed line in the SD-OCT image (C, E) shows that a great number of the hyperreflective foci in the ONL (white arrowheads) and the choriocapillaris (black arrowheads) in the foveal region in the right eye compared with the left eye (D, F). IR, infrared fundus image; OD, right eye; OS, left eye.
The patient provided written consent for publication of personal information including medical record details and photographs.
3. Discussion
Very few cases have been reported in which DR was present in an eye with RP [1], [2]. Fluorescein angiography and SD-OCT provided important findings in the current patient with RP accompanied by DR. First, the angiogram of the right eye shows a large area of non-perfusion and clinical retinal ischemia with marked leakage of dye along the superotemporal retinal artery, which is not very typical of an isolated diabetic retinopathy. These findings may presents a combination of non-perfusion of diabetic retinopathy with leakage of dye along retinal artery together with the retinal degeneration of clinical retinitis pigmentosa.
Second, the SD-OCT findings of the hyrerreflective foci were present not only in the retinal layers of eyes with RP accompanied by DR but were prevalent in the choroidal layers. Bolz et al. used SD-OCT and reported distinct retinal hyrerreflective foci associated with diabetic macular edema scattered throughout all retinal layers. Those investigators suggested that the hyrerreflective foci might have been macrophages, migrating RPE cells, or extravasated lipoproteins resulting from retinal inflammation or the breakdown of retinal vessel barriers. Therefore, these hyrerreflective foci may represent subclinical initial steps in the development of intraretinal hard exudates [3]. Recently, hyrerreflective foci were observed in retinas with other pathologies, such as those with RP [4]. Kuroda et al. reported that intraretinal hyrerreflective foci in the ONLs were seen more often in the advanced stage of RP [4]. Histopathological analysis of the retina in eyes with RP has shown that the outer segments of the rod photoreceptors are shortened and that this initial change in the degenerating retina is followed by gradual loss of whole cells as the disease progresses [5]. Subsequently, RPE cells migrate into the retina and accumulate around the walls of the retinal blood vessels [6]. Therefore, Kuroda et al. hypothesized that thinning of the ONL seems to result from photoreceptor cell death and these hyrerreflective foci in the thinning ONL may have resulted from photoreceptor cell death and subsequent RPE cell migration into the ONL and degeneration [4]. Although the mechanism of development of retinal and choroidal hyperreflective foci remains unclear in the current case, we hypothesized that the foci in the outer retina may reflect the photoreceptor cell death and a downward migration from the inner retina with accompanying retinal hyrerreflective foci attributed to DR with thinning of the ONL of a degeneration process of RP and the presence of hyperreflective foci in choroidal layers, as well as in retinal layers, might suggest migration of the photoreceptor cell death and RPE cellular toward both the outer retina and choroid, possibly following a degeneration process of RP over time.
Third, the number of the choroidal hyrerreflective foci increased corresponding to the extent of the disappearance of ELM and EZ line with thinning of the ONL in the current case. In addition, the SD-OCT image also showed a great number of the hyperreflective foci in the ONL and the choriocapillaris in the foveal region in the right eye compared with the left eye. More recently, Piri et al. reported the hyrerreflective foci observed in the fundus of the patients in Stargardt disease are present not only in the retinal layers but also in the choroid by SD-OCT imaging, and their prominence in the Bruch's membrane/RPE complex, choriocapillaris, and Sattler layer was correlated with disease severity in terms of retinal atrophy, decreased vision, and disease duration [7]. Therefore, the authors hypothesized that this findings may suggest migration of the lipofuscin deposits from the outer retina toward both the inner retina and choroid, following a degradation process [7]. Although the reason is unclear why the number of choroidal hyrerreflective foci increased corresponding to the extent of the disappearance of the ELM and EZ line with thinning of the ONL in the current case, we believe that the lesions may reflect the photoreceptor cell death and a subsequent RPE cellular migration into both the outer retina and choroid, possibly following a degeneration process of RP over time. Furthermore, as apparent in Fig. 2D of the right eye, the hyperreflective foci in the retinal and choroidal layers in the foveal region may increase as vision declines corresponding to the disappearance of the ELM and EZ line.
4. Conclusions
Unfortunately, we can't show the SD-OCT images obtained from patients at the initial visit because we didn't have SD-OCT machines when a patient is first seen. The lack of serial SD-OCTs made it impossible to monitor possible changes in the hyrerreflective foci over time, including changes in the number and position of the foci in the retina and choroid in the current case; however, the current SD-OCT findings suggested that the characteristic hyrerreflective foci clinically observed in the fundi of a patient with RP accompanied by DR are present not only in the outer retinal layers but also in the choroid. The current case showed that the hyperreflective foci may be correlated with the degree of retinal degeneration involved with disease progression.
Conflict of interest
The authors report no financial support or financial conflict of interest.
Ethical approval
The current study followed the tenets of the Declaration of Helsinki, and the Institutional Review Board of Asahikawa Medical University approved the prospective study design.
References
- 1.Hotta K., Hotta J. Cystoid macular edema related to diabetic retinopathy with retinitis pigmentosa. Jpn. J. Ophthalmol. 2006;50:390–393. doi: 10.1007/s10384-005-0332-7. [DOI] [PubMed] [Google Scholar]
- 2.Arden G.B. The absence of diabetic retinopathy in patients with retinitis pigmentosa: implications for pathophysiology and possible treatment. Br. J. Ophthalmol. 2001;85:366–370. doi: 10.1136/bjo.85.3.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bolz M., Schmidt-Erfurth U., Deak G. Optical coherence tomographic hyperreflective foci: a morphologic sign of lipid extravasation in diabetic macular edema. Ophthalmology. 2009;116:914–920. doi: 10.1016/j.ophtha.2008.12.039. [DOI] [PubMed] [Google Scholar]
- 4.Kuroda M., Hirami Y., Hata M. Intraretinal hyperreflective foci on spectral-domain optical coherence tomographic images of patients with retinitis pigmentosa. Clin. Ophthalmol. 2014;8:435–440. doi: 10.2147/OPTH.S58164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Milam A.H., Li Z.Y., Cideciyan A.V., Jacobson S.G. Clinicopathologic effects of the Q64ter rhodopsin mutation in retinitis pigmentosa. Invest. Ophthalmol. Vis. Sci. 1996;37:753–765. [PubMed] [Google Scholar]
- 6.Li Z.Y., Possin D.E., Milam A.H. Histopathology of bone spicule pigmentation in retinitis pigmentosa. Ophthalmology. 1995;102:805–816. doi: 10.1016/s0161-6420(95)30953-0. [DOI] [PubMed] [Google Scholar]
- 7.Piri N., Nesmith B.L., Schaal S. Choroidal hyperreflective foci in Stargardt disease shown by spectral-domain optical coherence tomography imaging: correlation with disease severity. JAMA Ophthalmol. 2015;133:398–405. doi: 10.1001/jamaophthalmol.2014.5604. [DOI] [PubMed] [Google Scholar]