Abstract
Patient: Female, 21
Final Diagnosis: Valsalva retinopathy
Symptoms: Sudden visual loss due to twin-pregnancy
Medication: None
Clinical Procedure: Conservative treatment of valsalva retinopathy with good and careful prognosis
Specialty: Ophthalmology
Objective:
Uncommon and rare case
Background:
Valsalva retinopathy is a rare but sight-threatening condition with sudden visual loss. Twin-pregnancy is known as a confirmed risk factor for Valsalva retinopathy.
Case Report:
A 21-year-old twin-pregnant Chinese woman with 31 weeks of gestation complained of a sudden decrease of visual acuity in her right eye for five hours. Based on the patient’s medical history, clinical findings, laboratory testing and optical coherence tomography (OCT) imaging studies, Valsalva retinopathy was confirmed. Initially, we managed the patient with Nd: YAG (neodymium-doped yttrium aluminum garnet) laser to puncture the posterior portion of the vitreous. As the laser failed to puncture the posterior hyaloid face due to dense premacular hemorrhages, we switched to conservative treatment. We reviewed the case with the patient 12 weeks after an uneventful vaginal delivery. Her right visual acuity had spontaneously increased to 6/6 with no active medical intervention.
Conclusions:
Valsalva retinopathy can be caused by twin-pregnancy. Patients with Valsalva retinopathy can be managed conservatively with careful prognosis following failed laser treatment. Ophthalmologists and obstetrician should coordinate properly and pay more attention to Valsalva retinopathic patients with twin-pregnancy.
MeSH Keywords: Hemorrhagic Disorders; Pregnancy, Twin; Valsalva Maneuver
Background
Valsalva retinopathy is a rare condition that presents itself with sudden visual decrease due to pre-retinal hemorrhaging [1,2]. It often occurs in Valsalva maneuvers such as vomiting, constipation, coughing, or even vigorous sexual activity [3–5].
Pregnancy is also known as a confirmed risk factor of Valsalva retinopathy [6]; and it can induce several immunological, hormonal, and hematologic changes that increase the possibilities of hemorrhage [7]. Valsalva retinopathy usually occurs during vomiting and physical labor activities. In the past, Valsalva retinopathy during twin-pregnancy was rarely noted or reported. Here, we report a case of Valsalva retinopathy with a twin-pregnant female. This case was unusual as it underwent Valsalva retinopathy without vomiting and/or severe coughing. After a failed Nd: YAG (neodymium-doped yttrium aluminum garnet) laser procedure the patient was managed with conservative treatment and good prognosis.
Case Report
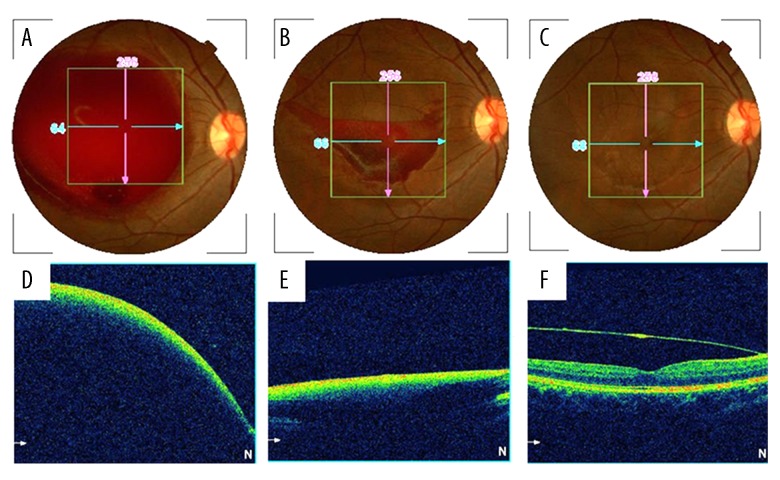
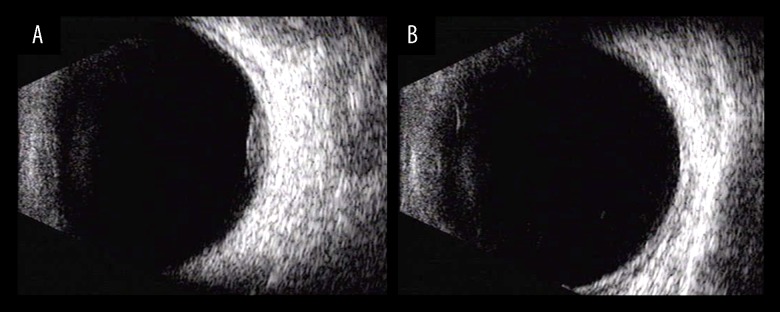
A 21-year-old twin-pregnant Chinese woman with 31 weeks of gestation experienced a sudden visual loss in her right eye for five hours prior to the initial outpatient clinic visit. Her symptoms displayed no vomiting or severe coughing. She was diagnosed with a twin-pregnancy as two fetuses were identified in her uterus by ultrasound scan. The patient’s previous medical history was not remarkable. She had no history of vascular disease or blood dyscrasia. Her best uncorrected visual acuity was 20/20 in the left eye and hand motion in 50 cm in the right eye. Direct and indirect pupillary response, anterior segment examination, and ocular motility were normal. An enlarged (8–10 disc diameter) pre-retinal hemorrhage was found in the macula (Figure 1A, 1D) by retinal examination. Optical coherence tomography (OCT) revealed a dome-shaped hypo-reflective area. The hemorrhage location was subhyaloid. Ocular ultrasound showed pre-retinal eminence in her right eye (Figure 2A, 2B). Complete blood count, blood pressure, coagulation profiles, and fasting blood glucose were all within normal ranges. The diagnosis of Valsalva retinopathy was confirmed on the basis of clinical findings, history, fundus examination, and OCT imaging. We gave the patient three options to consider: observation alone, Nd: YAG laser membranotomy, or vitrectomy. Considering the potential risks, benefits, and costs of surgery and laser, at this stage the patient chose a conservative approach for two weeks. During the first two weeks, conservative management including half sitting position, and avoidance of strenuous activities were recommended. Medication was not given to the patient. After a two week observation period, her right visual acuity did not improve. Two weeks later, the patient asked for Nd: YAG laser to puncture the posterior portion of the vitreous. YAG laser membranotomy was performed (VISULAS YAG III, Carl Zeiss, Germany) under contact laser lenses (Volk Fundus laser lens, OH, USA). Nd: YAG was applied in single shots to the hyaloid face beginning at 1.7 mJ to 3.8 mJ. However, the laser failed to puncture the posterior hyaloid face as a result of dense premacular hemorrhages. The hyaloid membrane was not perforated when the energy power was increased to 3.8 mJ. We then prescribed conservative treatment. A normal vaginal delivery was recommended by her obstetrician upon maturity of pregnancy. We reviewed the case with the patient 12 weeks after an uneventful vaginal delivery and found that half of the hemorrhage was absorbed (Figure 1B, 1E). As a result, her right eye visual acuity had spontaneously increased to 6/6 with no active medical intervention. The case showed complete resolution of the subhyaloid hemorrhage. At nine month follow-up, the patient’s uncorrected visual acuity kept at 6/6 with complete absorption of the subhyaloid hemorrhage. A split premacular membrane was found in the macular region (Figure 1C, 1F).
Figure 1.
Retina fundus photographs (A–C) and optical coherence tomography (D–F) of the right eye. An enlarged (8–10 disc diameters) preretinal hemorrhage located in the macula (A, D) at 31 weeks of gestation. Half of the hemorrhage was absorbed (B, E) 12 weeks after giving birth naturally. Complete reabsorption of the subhyaloid hemorrhage and a split premacular membrane were found in the macular region (C, F) nine month later.
Figure 2.
Ocular ultrasound showed preretinal eminence (A) which subsequently disappeared after five months (B).
Discussion
Valsalva retinopathy typically presents as a sudden visual loss which is caused by a premacular hemorrhage following a Valsalva maneuver [1,6]. It was first reported in 1973 by Duane [7]. Patients often have a history of strenuous physical activity that enhanced the intra-thoracic or intra-abdominal pressure [8]. Pregnancy is also known as a risk factor of Valsalva retinopathy [9,10]. Elevation in intravenous pressure and intra-abdominal pressure could further cause rupture of superficial retinal capillaries [7,10]. In the present study, we reported a rare case of Valsalva retinopathy with twin-pregnancy. This case was unusual as the Valsalva retinopathy due to twin-pregnancy occurred without vomiting and severe coughing. After observation and a failed Nd: YAG laser procedure, the patient was managed with conservative treatment and had good final prognosis.
The reason for Valsalva retinopathy in twin-pregnancy is that the enlarged uterus elevates intra-abdominal pressure and compresses the veins. These changes lead to increased intravenous pressure. As a result, potential Valsalva retinopathy can occur [9,11]. Spontaneous rupture of perifoveal capillaries causes sudden visual loss. Predilection to the macula is explained by the absence of firm attachments of the inner limiting membrane (ILM) to the retina at the posterior pole peripheral from the macular fovea [9,11,12]. Hemorrhage in Valsalva retinopathy may be subhyaloid, beneath ILM or at the interface between them [10]. Rarely, it can be seen between ILM and the nerve fiber layer, which is self-limited because of the anatomical structure [1,10].
Different therapeutic approaches have been reported regarding Valsalva retinopathy during pregnancy [13–15]. Therapeutic treatments including conservative management, Nd: YAG membranotomy, and vitrectomy have been used. The choice depends on the location and size of the hemorrhage. With a hemorrhage size less than one disc diameter, it tends to spontaneously absorption in a short time; a conservative treatment, therefore, is generally rational. El-Defrawy et al. reported a conservative approach for retinal hemorrhage in pregnant women [14]. In patients with a large hemorrhage, spontaneous resorption of the hemorrhage may take a longer time, sometimes months. This may produce permanent visual injuries due to macular pigmentary changes, formation of epimacular membrane, and macular hole, or toxic damage to the retina due to long lasting contact with hemoglobin or iron [11,16,17]. Under such circumstances, Nd: YAG laser is recommended to drain the entrapped blood through a focal opening into the vitreous cavity where it is absorbed more rapidly and thus relieve the tension of the ILM sooner. Nd: YAG is also an effective treatment in non-dense and non-coagulated preretinal hemorrhages. One thing to be noted is that drainage with laser treatment is not possible for coagulated premacular hemorrhage. Another point to be noted is that closer proximity to the retinal surface presents an additional risk when using laser treatment. Occasionally, complications may occur. This may include macular hole, retinal detachment, epiretinal membrane formation, and persistent unsealed ILM [1,16]. Under such circumstances, vitrectomy is more effective and safer than other treatments for dense premacular hemorrhages. Surgery is not absolutely free of risks. Some complications, such as retinal breaks and cataracts, may occur accidentally.
The particularity of this case was that the patient underwent observation, a failed Nd: YAG laser procedure and conservative treatment. During the first two weeks, conservative management was recommended. After two weeks of observation period, her right visual acuity did not improve. Two weeks later, the patient asked for Nd: YAG laser to puncture the posterior portion of the vitreous. However, the laser failed to puncture the posterior hyaloid face as a result of dense premacular hemorrhages. Then conservative treatment was chosen again. The treating procedure of this case may infer that Valsalva retinopathy during pregnancy should be managed conservatively rather than by Nd: YAG laser treatment. Moreover, the current literature lacks useful data to address the safety to YAG laser or surgical interventions to the fetus and the ideal timing for any proposed intervention.
There are still a lot of controversies on the ideal timing for any proposed intervention for such cases. There is also no general consensus on the optimum obstetric and anesthetic management of such pregnant cases. The patient in this study had vaginal delivery as recommendation by her obstetrician. There are yet debates as to whether spontaneous vaginal delivery is liable to exacerbate the hemorrhage [18]. Potential interventions may include elective caesarean section under epidural/general anesthesia to prevent progression by limiting venous pressure. Ultimately, patients should be counseled and advised about the risks of methods of delivery and their wishes should be carefully considered when making a final decision to prevent disease progression and recurrence. There is no evidence that caesarean section is necessary. A spontaneous vaginal delivery may not increase the risk of recurrent hemorrhage. Another factor that should be kept in mind is that general anesthesia may induce a rebleeding due to vasodilation owing to hypoxia and hypercarpea [7,19]. Extubation also leads to significant elevated venous pressure followed by coughing [19]. Epidural anesthesia has also been shown to associate with preretinal hemorrhaging. This is attributed to an increased cerebrospinal fluid pressure within the epidural space. It can increase retinal venous pressure and cause subsequent hemorrhage [7,19].
The case of Valsalva hemorrhage in this report did not present with vomiting. It was somewhat different from several previous reports [3–5]. The Valsalva hemorrhage in this case most likely occurred as a result of the twin-pregnancy. Twin-pregnancy with larger uterus can lead to elevation in intravenous pressure and intra-abdominal pressure, which can cause spontaneous rupture of superficial retinal capillaries [7,10]. Therefore, twin-pregnancy is a confirmed and important risk factor for Valsalva retinopathy.
The prognosis for patients with Valsalva retinopathy is generally promising. The condition requires equitable close observations [8]. Vision acuity usually returns to normal state over a time, varying from weeks to months [1,7,8,10]. Some of these patients may experience poor visual outcomes due to pigmentary impairments in the macula [18].
This unusual case of Valsalva retinopathy has prompted us to further study twin-pregnant women; with cooperation of gynecologists, we will pay close attention to observe the fundus, as to whether possible conservative treatment is needed.
Conclusions
In summary, we report a case of Valsalva retinopathy during twin-pregnancy. Patients with Valsalva retinopathy can be managed conservatively following failed laser treatment. Ophthalmologists and obstetrician should coordinate properly and pay more attention to Valsalva retinopathic patients with twin-pregnancy.
Abbreviations:
- Nd: YAG
neodymium-doped yttrium aluminum garnet;
- OCT
optical coherence tomography;
- ILM
inner limiting membrane
Footnotes
Conflict of interest
None.
References:
- 1.García Fernández M, Navarro JC, Castaño CG. Long-term evolution of Valsalva retinopathy: A case series. J Med Case Rep. 2012;6:346. doi: 10.1186/1752-1947-6-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jayaprakasam A, Matthew R, Toma M, Soni M. Valsalva retinopathy in pregnancy: SD-OCT features during and after Nd: YAG laser hyaloidotomy. Ophthalmic Surg Lasers Imaging. 2011;17:42. doi: 10.3928/15428877-20110210-06. Online: e26–28. [DOI] [PubMed] [Google Scholar]
- 3.Hassan M, Tajunisah I. Valsalva haemorrhagic retinopathy after push-ups. Lancet. 2011;377:504. doi: 10.1016/S0140-6736(10)60677-0. [DOI] [PubMed] [Google Scholar]
- 4.Choudhry N, Rao RC. Images in clinical medicine. Valsalva retinopathy. N Engl J Med. 2014;370(8):e13. doi: 10.1056/NEJMicm1304102. [DOI] [PubMed] [Google Scholar]
- 5.Michaels L, Tint NL, Alexander P. Postcoital visual loss due to valsalva retinopathy. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2014-207130. bcr2014207130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sabella P, Bottoni F, Staurenghi G. Spectral-domain OCT evaluation of Nd: YAG laser treatment for Valsalva retinopathy. Graefes Arch Clin Exp Ophthalmol. 2010;248:599–601. doi: 10.1007/s00417-009-1252-x. [DOI] [PubMed] [Google Scholar]
- 7.Duane TD. Valsalva hemorrhagic retinopathy. Trans Am Ophthalmol Soc. 1972;70:298–313. [PMC free article] [PubMed] [Google Scholar]
- 8.Park SW, Seo MS. Subhyaloidhemorrhage treated with SF6 gas injection. Ophthalmic Surg Lasers Imaging. 2004;35:335–37. [PubMed] [Google Scholar]
- 9.Dağlioğlu MC, Coşkun M, Ilhan N, et al. Posterior hyaloidotomy by Nd: YAG laser application in patient with postpartum depression caused by Valsalva retinopathy. Case Rep Ophthalmol. 2013;4:64–68. doi: 10.1159/000350773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goel N, Kumar V, Seth A, et al. Spectral-domain optical coherence tomography following Nd: YAG laser membranotomy in Valsalva retinopathy. Ophthalmic Surg Lasers Imaging. 2011;42(3):222–28. doi: 10.3928/15428877-20110224-01. [DOI] [PubMed] [Google Scholar]
- 11.De Maeyer K, Van Ginderdeuren R, Postelmans L, et al. Sub-inner limiting membrane haemorrhage: Causes and treatment with vitrectomy. Br J Ophthalmol. 2007;91(7):869–72. doi: 10.1136/bjo.2006.109132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meyer CH, Mennel S, Rodrigues EB, Schmidt JC. Persistent premacular cavity after membranotomy in Valsalva retinopathy evident by optical coherence tomography. Retina. 2006;26(1):116–18. doi: 10.1097/00006982-200601000-00024. [DOI] [PubMed] [Google Scholar]
- 13.Al-Mujaini AS, Montana CC. Valsalva retinopathy in pregnancy: A case report. J Med Case Rep. 2008;2:101. doi: 10.1186/1752-1947-2-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El-Defrawy H, Sallam A, McKechnie CJ, Zambarakji H. Valsalva retinopathy in pregnancy. Should we treat? JRSM Short Rep. 2011;2:45. doi: 10.1258/shorts.2011.011035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ladjimi A, Zaouali S, Messaoud R, et al. Valsalva retinopathy induced by labour. Eur J Ophthalmol. 2002;12:336–38. doi: 10.1177/112067210201200417. [DOI] [PubMed] [Google Scholar]
- 16.Xie ZG, Yu SQ, Chen X, et al. Macular hole secondary to Valsalva retinopathy after doing push-up exercise. BMC Ophthalmol. 2014;14:98. doi: 10.1186/1471-2415-14-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ramsay RC, Knobloch WH, Cantrill HL. Timing of vitrectomy for active proliferative diabetic retinopathy. Ophthalmology. 1986;93(3):283–89. doi: 10.1016/s0161-6420(86)33742-4. [DOI] [PubMed] [Google Scholar]
- 18.Wickremasinghe SS, Tranos PG, Davey C. Valsalva haemorrhagic retinopathy in pregnant woman: Implications for delivery. Acta Ophthalmol Scand. 2003;81(4):420–22. doi: 10.1034/j.1600-0420.2003.00102.x. [DOI] [PubMed] [Google Scholar]
- 19.Chidley KE, Law R, Vanner G. Caesarean section following a recent retinal hemorrhage. Anaesthesia. 1998;53(5):477–85. doi: 10.1046/j.1365-2044.1998.00394.x. [DOI] [PubMed] [Google Scholar]