Abstract
Background:
Aboriginal people in Canada have an unduly high burden of end-stage kidney disease (ESKD) and many live in rural settings. Peritoneal dialysis (PD) is a home-based dialysis modality that may provide a valuable alternative to in-center hemodialysis which is relatively underutilized by the Aboriginal population.
Objective:
We aim to assess the barriers to PD utilization in Aboriginal patients with ESKD.
Design:
This article is a prospective observational cohort study.
Setting:
The setting involves 3 predialysis clinics in Winnipeg, Kingston, and Moose Factory.
Patients:
The patients were 99 individuals (67 non-Aboriginal and 32 Aboriginal) who were at least 18 years of age with an estimated glomerular filtration rate of less than 30 mL/min/1.73m2, and were enrolled in one of the 3 study sites from April 2011 to October 2013.
Measurements:
Patient demographics and comorbidities were documented. Barriers to PD, PD as modality choice, and Aboriginal status were assessed via patient survey upon study enrollment. PD use as the initial dialysis modality was assessed via monthly patient follow-up for 1 year after enrollment in the study.
Methods:
The patient survey was created based on literature review of known barriers to PD, repaired based on direct patient feedback, and tested for reliability via the test-retest method. Differences in PD choice, barriers to PD, and PD use between Aboriginal and non-Aboriginal patients were determined by chi-square test and logistic regression.
Results:
All patients enrolled in the study completed the survey. Mean age was 65.5 versus 54.6 years for non-Aboriginals and Aboriginals, respectively. Barriers to PD significantly associated with Aboriginal status were lack of money (odds ratio [OR]: 21.3; 95% confidence interval [CI]: 5.3-86.4; P < .0001) and anxiety (OR: 2.8; 95% CI: 1.1-7.1; P = .03). There was no difference in PD choice between non-Aboriginals and Aboriginals (66.7% vs 68.8%, respectively; P = .83). One of 67 non-Aboriginals (1.5%) and 5 of 32 Aboriginals (15.6%) died prior to initiating dialysis (P = .013). No significant difference was observed between non-Aboriginals (33%) and Aboriginals (28%) in use of PD (P = .81).
Limitations:
Small sample size was a limitation of this study.
Conclusions:
Aboriginal people in Canada have a disproportionately large burden of ESKD, and PD could provide an alternative to in-center hemodialysis for those living in rural areas. Our study identified anxiety and lack of money as barriers to PD significantly associated with Aboriginal status. When choosing dialysis modality, shared decision making between physicians and patient is of key importance to weigh all potential benefits and risks and emphasize the Aboriginal patient’s values and preferences. These results can be used to guide future research and to help devise interventions targeting barriers to PD in Aboriginals.
Keywords: Aboriginal, peritoneal dialysis, barrier, disparity
Abrégé
Contexte:
Au Canada, un nombre important de personnes autochtones habitent en région rurale, et cette population présente un taux exagérément élevé d’insuffisance rénale terminale (IRT) par rapport à la population générale. La dialyse péritonéale (DP) est une modalité de dialyse que le patient reçoit à domicile et qui pourrait s’avérer une solution de remplacement intéressante à l’hémodialyse en centre, laquelle est relativement sous-utilisée par les patients autochtones.
Objectif de l’étude:
Nous voulions recenser les facteurs qui restreignent l’utilisation de la DP chez les patients autochtones souffrant d’IRT.
Type d’étude:
Il s’agit d’une étude de cohorte observationnelle et prospective.
Cadre de l’étude:
Trois cliniques de prédialyse situées à Winnipeg, à Kingston et à Moose Factory ont pris part à l’étude.
Patients:
La cohorte était constituée de 99 patients adultes (67 allochtones et 32 autochtones) dont le débit de filtration glomérulaire estimé (DFGe) était de moins de 30 ml/min/1,73 m2. Les participants à l’étude ont été recrutés parmi les patients des trois centres de prédialyse mentionnés ci-haut entre avril 2011 et octobre 2013.
Mesures:
On a d’abord noté les données démographiques et les comorbidités des patients. Ensuite, un sondage réalisé auprès des patients au moment du recrutement a permis d’établir leur statut autochtone ou allochtone, de déterminer les facteurs qui constituaient un frein à leur utilisation de la DP, de même que des données sur l’usage de la DP comme modalité de dialyse. Le choix de la DP comme modalité initiale a été déterminé par un suivi mensuel sur une période d’un an post-recrutement.
Méthodologie:
Les obstacles à l’utilisation de la DP comme modalité de dialyse figurant dans le sondage étaient basés sur une revue de la littérature recensant ces facteurs. Le sondage a ensuite été modifié en fonction de la rétroaction offerte par les patients, et sa fiabilité a été évaluée par la méthode du test-retest. Les divergences observées entre le choix ou non de la DP comme modalité de dialyse, les facteurs freinant son utilisation et les variations relevées en regard de l’origine ethnique des patients (autochtones ou allochtones) ont été établies par le test du chi carré et par régression logistique.
Résultats:
Tous les patients inclus dans l’étude ont répondu au sondage. L’âge moyen des patients allochtones était de 65,5 ans alors qu’il était de 54,6 ans pour les patients autochtones. Les entraves à l’utilisation de la DP associées de façon significative avec le statut d’autochtone étaient le manque d’argent (RC=21,3; IC 95% 5,3-86,4; p<0,0001) et l’anxiété (RC=2,8; IC 95 1,1-7,1; p=0,03). Aucune différence n’a été observée entre allochtones et autochtones (66,7 % contre 68,8 % respectivement; p=0,83) en ce qui concerne le choix de la DP comme modalité de dialyse. Un patient allochtone (1,5 %) et 5 patients autochtones (15,6 %) sont décédés au cours de la période couverte par l’étude. Enfin, aucune variation significative n’a été observée entre les patients autochtones et allochtones (28 % et 33 % respectivement; p=0,81) en regard de l’utilisation de la DP comme modalité de dialyse.
Limites de l’étude:
La taille restreinte de l’échantillon limite la portée de cette étude.
Conclusion:
Au Canada, l’insuffisance rénale terminale affecte les patients autochtones de façon disproportionnelle. Pour ceux d’entre eux qui habitent en région rurale, la dialyse péritonéale, qui se pratique à domicile, pourrait s’avérer une solution de remplacement intéressante à l’hémodialyse conventionnelle qui elle, se pratique en centre hospitalier. Notre étude a révélé que l’anxiété et le manque d’argent constituaient des facteurs restreignant l’utilisation de la DP chez la population autochtone. Dans le choix d’une modalité de dialyse, la prise de décision conjointe du patient avec les médecins revêt une importance majeure : d’abord pour bien mesurer les bienfaits et les risques potentiels, mais également pour tenir compte des valeurs et des préférences du patient autochtone. Ces résultats pourront servir à orienter les recherches futures et à concevoir des interventions ciblant les facteurs qui freinent l’utilisation de la DP chez les patients autochtones atteints d’IRT.
What was known before
Aboriginals in Canada have a high burden of end-stage kidney disease and low utilization of peritoneal dialysis compared with non-Aboriginals.
What this adds
Based on a self-reported patient survey, Aboriginals perceive lack of money and anxiety as significant barriers to the use of peritoneal dialysis. In our patients, as in other cohorts, risk of death before dialysis was higher in Aboriginal patients.
Introduction
Over 1.4 million people, 4.3% of Canada’s total population, self-identify as Aboriginal, encompassing First Nations, Inuit, and Metis.1 Aboriginal people in Canada have an unduly high burden of kidney disease, with a 4 times higher incidence rate of end-stage kidney disease (ESKD) than non-Aboriginal people.2 While diabetes is the leading cause of ESKD in Aboriginal patients,3 a combination of medical and societal factors such as hypertension, vascular disease, glomerulonephritis,4 poverty, poor access to health care, and delayed referral to a nephrologist5 may all contribute to this growing burden of ESKD. Aboriginals also have a significantly lower rate of renal transplantation than white patients in Canada.6 Consequently, there has been an 8-fold increase in the number of Aboriginal dialysis patients between 1980 and 2000.7
Peritoneal dialysis (PD) is dialysis therapy that can be done at home. In prospective studies, approximately 64% to 75% of ESKD patients are medically eligible for PD.8,9 In general, PD patients appear to have a lower mortality rate compared with hemodialysis (HD) patients in the first few years of treatment,10 lower cost, and an overall similar quality of life.8,11 The early survival benefits of PD may be due to preservation of residual renal function.12 As a home-based therapy, PD provides a valuable alternative for patients living in remote areas. In-center HD is typically available only at larger centers that may require long travel distance 3 times per week for patients to receive HD. Despite this, the proportion of incident patients on PD in Canada remained approximately 20% in 2015.13
Approximately half of Canada’s Aboriginal population lives outside urban centers, divided between reserves and nonreserve rural areas.1 Initiating in-center HD usually requires relocation to a larger and more urban center. For people living in the James Bay Coastal Region of Ontario, Moose Factory Island is the only site with an HD unit. Due to the remote geography and lack of year-round road access from communities up the coast from Moose Factory, patients in other communities cannot travel for weekly dialysis and must relocate if this is the selected modality. A qualitative study of Aboriginal patients who have relocated from their community to access HD describes a loss of community, cultural and spiritual isolation as well as alienation from children and friends.14 To avoid relocation, it is plausible that Aboriginal patients with ESKD living in rural areas would choose PD as their chronic modality. However, in an observational study of incident Canadian dialysis patients,15 Aboriginals were less likely to initiate PD therapy compared with whites even though a significantly larger proportion lived in rural locations. Aboriginal patients were also more likely to switch from peritoneal to HD.
Prior studies have examined and devised targeted interventions to overcome barriers to PD. Medical, cognitive, psychological, and social barriers to PD, rather than absolute contraindications, often contribute to physician and patient preference to initiate HD. For example, age, comorbid conditions, and living alone are positively associated with patient preference of HD.16 Thus, elderly patients over the age of 70 are less likely to choose PD, even after completing predialysis education.9 Measures to overcome these barriers, such as increasing home care assistance, have resulted in a significant increase in PD uptake in the elderly population in Toronto, Canada.16
A series of studies also found an increased utilization of self-care dialysis when a knowledge barrier for a specific population was identified and an appropriate intervention was applied. An assessment of barriers to self-care dialysis was conducted in an in-center HD unit in Canada.17 Barriers were divided into 3 groups: knowledge, attitudes, and skills. Sixty percent of respondents reported that they lacked knowledge in the various dialysis modalities. Frequent attitude barriers were (a) the belief that patients should not be dialyzed without direct supervision (53%) and (b) fear of social isolation (54%).The most frequent skills barrier was lack of space at home, reported by 42% of respondents. Following this survey, patients with chronic kidney disease (CKD) were enrolled in a randomized controlled trial and assigned to usual care, or a 2-phase educational intervention that targeted these frequently identified barriers. Patients assigned to the education arm were significantly more likely to choose self-care dialysis.18 However, no prior studies have examined the unique barriers to PD in Aboriginals with ESKD.
The purpose of the study is to assess the medical, cultural, cognitive, and psychological barriers to PD utilization in Aboriginal patients. Results will be used to devise and implement a targeted intervention to increase PD use in this population.
Methods
Study Sites
Patients were enrolled at 3 different predialysis clinics located in Winnipeg, Kingston, and Moose Factory (Kingston satellite). All patients in the predialysis clinic receive care and dialysis modality education as per the local standard of care, by a multidisciplinary team comprised of a nephrologist, social worker, and nurse trained in dialysis modality education.
Patient Recruitment and Follow-up
Patients included in this study were required to be at least 18 years of age and enrolled at one of the 3 study sites with an estimated glomerular filtration rate of less than 30 mL/min/1.73 m.2 Patients at these clinics represent a heterogeneous population inclusive of Aboriginal and non-Aboriginal patients from reserves, nonreserve rural areas, and urban centers. Patients who self-identified as First Nations, Inuit, or Metis were considered Aboriginal, and all others were considered non-Aboriginal. Patients were excluded from this study if they had an absolute contraindication for PD, including a history of abdominal scarring, abdominal hernia, morbid obesity, inflammatory bowel disease, diverticulitis, ileostomy, colostomy, ascites, abdominal vascular aneurysms, large polycystic kidneys, or residence in a nursing home that does not permit PD.
Consecutive eligible patients were approached for study recruitment and enrolled after providing informed consent. Patient survey (see below) was administered by research staff immediately upon study enrollment. When required, translator services were provided to prevent selection bias for English-only speaking patients. Adherence to the Canadian Institutes for Health Research guidelines for health research involving Aboriginal people was maintained from recruitment of patients to the conclusion of this study. Patient recruitment occurred over a 3-year period, with 1-year follow-up after enrollment.
Outcome Definitions
PD eligibility was defined as capability to conduct self-care PD as determined by the predialysis multidisciplinary team that assessed clinical factors which precluded patients from PD. These factors included but were not limited to impaired manual dexterity, poor vision or hearing, inadequate reading or writing ability, or inadequate space to perform PD.
PD choice was defined as patient choice of PD, as assessed by survey on patient enrollment into the study, prior to initiation of any dialysis modality.
PD use was the primary study outcome, and defined as the first dialysis at home after completion of training.
Data Collection
Upon enrollment, patients completed a written survey (see below for details of survey design) identifying their choice of dialysis modality, Aboriginal status, and barriers to PD. Baseline demographics, comorbidities, and PD eligibility were recorded using medical chart review. Patients were followed on a monthly basis for 1 year after enrollment to assess for initiation of dialysis, modality of dialysis utilized, mortality, and transitions between PD and HD.
Survey Design and Validation
The patient survey used in this study was created based on literature review of known barriers to PD, repaired based on direct patient feedback, and tested for reliability via the test-retest method.19 First, a literature review was conducted to assess previously validated surveys regarding barriers to PD. A preliminary survey was created based on the literature and given to a pilot group of randomly selected Aboriginal and non-Aboriginal patients in the predialysis clinic. Sixteen patients (12 non-Aboriginal and 4 Aboriginal) were initially administered the survey, and then retested a month later. The preliminary survey was comprised of a series of binary questions and additionally had a section for open-ended questions to screen for additional barriers to PD. Additional and thematically recurrent barriers to PD described by patients in the initial survey were integrated into the subsequent survey. The final survey consisted of 4 barrier domains and 20 barriers. The kappa statistic was calculated for each question using the test-retest method. Agreement was greater than 81% for all questions indicating excellent reliability. The survey was administered to patients by research staff immediately upon patient enrollment.
Sample Size Calculation
Sample size calculation was conducted by extrapolation of data from a prior retrospective study that examined PD use in patients both Aboriginal and non-Aboriginal patients at Kingston General Hospital.20 This study provided estimates on the proportion of Aboriginal and non-Aboriginal patients who initiate PD, which is consistent with the primary outcome of our study. To detect a 58% standardized difference in this proportion (45% Aboriginal and 18% non-Aboriginal patients) with 90% and a significance level of 0.05, a sample size of 124 patients was deemed necessary. This sample size calculation with continuity correction is based in the normal approximation to the binomial distribution and equal numbers of Aboriginal and non-Aboriginal patients.
Statistical Analysis
Baseline demographic characteristics were compared between Aboriginal and non-Aboriginal patients using a t test for continuous variables and chi-square test for categorical variables versus Fisher exact test as appropriate. The proportion of PD choice, eligibility, and use was compared between groups using the chi-square test and logistic regression. For self-identified barriers to PD, Aboriginal and non-Aboriginal responses were compared using the chi-square test and logistic regression analyses. In exploratory analysis, barriers associated with non-PD use were compared in Aboriginal and non-Aboriginal patients, and frequency of barriers associated with Aboriginals living remotely from dialysis center (>500 km) were compared with other Aboriginals. For all analyses, differences were considered significant a priori if the 2-sided P value is less than .05. STATA version 12 was used for all analyses.
Results
Baseline Demographics and Comorbidities
Patients were enrolled from 2011 to 2013, with follow-up completed in October 2014. A total of 99 participants were enrolled in this study consisting of 67 non-Aboriginal and 32 Aboriginal patients (20 from Kingston, 3 from Moose Factory and 76 from Winnipeg locations). All patients who enrolled in the study completed the survey. Statistically significant differences in demographic characteristics included mean age of participants (65.5 vs 54.6 years for non-Aboriginal and Aboriginal patients, respectively; P < .0001), and median distance from the study center (11 km vs 477 km for non-Aboriginal and Aboriginal patients, respectively; P value < .0001). Causes of ESKD, as documented in patient charts, were found to be significantly different between groups. Diabetes caused ESKD in 37.3% versus 84% in non-Aboriginal versus Aboriginal, respectively (P < .0001). Hypertension caused ESKD in 14.9% versus 0% in non-Aboriginal versus Aboriginal patients (P = .021). Patients in both groups had similar mean estimated glomerular filtration rates, body mass index (BMI), and total body weight at the time of enrollment (Table 1).
Table 1.
Baseline Demographics.
| Non-Aboriginal (n = 67) | Aboriginal (n = 32) | P value | |
|---|---|---|---|
| Mean age, y (SD) | 65.5 (11.4) | 54.6 (12.9) | <.0001 |
| % male | 61.2 | 40.6 | .06 |
| Mean weight, kg (SD) | 84.0 (23.4) | 85.4 (18.9) | .77 |
| Mean BMI, kg/m2 (SD) | 29.6 (6.8) | 31.0 (6.5) | .37 |
| Mean eGFR, mL/min/1.73 m2 (SD) | 10.9 (4.3) | 10.3 (3.0) | .47 |
| Study center, number enrolled | |||
| Kingston | 19 | 4 | — |
| Winnipeg | 48 | 28 | — |
| Median distance from study center, km (IQR) | 11 (4.7-91.1) | 476.6 (38.4-569.1) | <.0001 |
| Cause of ESKD, n (%) | |||
| Diabetes | 25 (37.3) | 27 (84.4) | <.0001 |
| Hypertension | 10 (14.9) | 0 | .021 |
| Glomerulonephritis | 14 (20.9) | 4 (12.5) | .311 |
| Other | 18 (26.9) | 1 (3.1) | .005 |
Note. BMI = body mass index; eGFR = estimated glomerular filtration rate; IQR = interquartile range; ESKD = end-stage kidney disease.
Barriers to PD
Among 20 different potential barriers across 4 domains assessed in this study, barriers to PD found to be significantly associated with Aboriginal status included lack of money (odds ratio [OR]: 21.3; 95% confidence interval [CI]: 5.3-86.4; P < .0001) and anxiety (OR: 2.8; 95% CI: 1.1-7.1; P = .03). Lack of motivation, lack of social support, lack of family support, and the belief that dialysis should be done in-hospital trended to deter non-Aboriginals from PD, although none achieved statistical significance (Table 2).
Table 2.
Barriers Survey Completed by Patient.
| Non-Aboriginal, n/N (%) | Aboriginal, n/N (%) | OR (95% CI) | P value | |
|---|---|---|---|---|
| Knowledge barriers | ||||
| Lack of awareness | 0 | 0 | NA | NA |
| Lack of explanation of options | 1/67 (1.50) | 1/32 (3.12) | 2.12 (0.13-35.12) | .60 |
| Lack of understanding | 11/66 (16.7) | 6/32 (18.8) | 1.15 (0.38-3.4) | .80 |
| Medical barriers | ||||
| Lack of strength | 10/67 (14.9) | 5/32 (15.6) | 1.05 (0.33-3.39) | .93 |
| Lack of mobility | 6/67 (9.0) | 2/32 (6.3) | 0.67 (0.13-3.6) | .64 |
| Poor health status | 4/67 (6.0) | 4/32 (12.5) | 2.25 (0.52-9.6) | .27 |
| Poor vision | 4/67 (6.0) | 5/32 (15.6) | 2.92 (0.73-11.71) | .12 |
| Poor hearing | 2/67 (3.0) | 1/32 (3.1) | 1.05 (0.09-12.01) | .97 |
| Poor memory | 3/67 (4.5) | 2/32 (6.3) | 1.42 (0.23-8.96) | .71 |
| Psychological barriers | ||||
| Anxious | 14/62 (22.6) | 14/31 (45.2) | 2.82 (1.12-7.11) | .03 |
| Afraid | 14/66 (21.2) | 9/32 (28.1) | 1.45 (0.55-3.84) | .45 |
| Dialysis should be done in-hospital | 10/62 (16.1) | 4/28 (14.3) | 0.87 (0.25-3.04) | .82 |
| Isolation | 14/64 (21.9) | 9/31 (29.03 | 1.46 (0.55-3.88) | .45 |
| Lack of Motivation | 29/65 (44.6) | 10/31 (32.3) | 0.59 (0.24-1.45) | .25 |
| Cultural and social barriers | ||||
| Language | 2/67 (3.0) | 4/32 (12.5) | 4.64 (0.80-26.83) | .08 |
| Lack of space | 15/65 (23.1) | 9/32 (28.1) | 1.30 (0.50-3.42) | .59 |
| Lack of time | 6/66 (9.1) | 3/31 (9.7) | 1.07 (0.25-4.60) | .93 |
| Lack of social support | 15/66 (22.7) | 5/32 (15.6) | 0.63 (0.21-1.92) | .41 |
| Family declines | 16/58 (27.6) | 5/23 (21.7) | 0.73 (0.23-2.29) | .59 |
| Lack of moneya | 3/47 (6.4) | 16/27 (59.3) | 21.33 (5.23-86.42) | <.0001 |
Note. OR = odds ratio; CI = confidence interval.
Assessed only in Winnipeg patients.
In exploratory analysis, barriers associated with non-PD use were compared in Aboriginal and non-Aboriginal patients, and none were found to be significant. When comparing remote dwelling with other Aboriginals, there was no significant difference in the frequency of barriers to PD except for “lack of motivation” which was significantly higher in nonremote dwelling Aboriginals (50% vs 0; P = .004; Supplementary Table 1).
Patient Outcomes
Assessment by a multidisciplinary team yielded no statistically significant difference in PD eligibility between non-Aboriginal versus Aboriginal patients (93.9% vs 87.5%, respectively; P = .27). In addition, no differences were demonstrated in PD choice between non-Aboriginal and Aboriginals, as identified by the patient survey (66.7% vs 68.8%, respectively; P = .83). One of 67 non-Aboriginal patients (1.5%) and 5 of 32 Aboriginal patients (15.6%) died prior to initiating dialysis (P = .013). In addition, 9 non-Aboriginal and 3 Aboriginal patients remained in CKD at the conclusion of this study and did not initiate dialysis, while 2 non-Aboriginals and 1 Aboriginal underwent a preemptive kidney transplant (Table 3). Three non-Aboriginals and no Aboriginals were lost to follow-up prior to initiating dialysis.
Table 3.
Study Outcomes.
| Non-Aboriginal (n = 67) | Aboriginal (n = 32) | P value | |
|---|---|---|---|
| PD eligibilitya (%) | 62 (93.9) | 28 (87.5) | .27 |
| PD choiceb | 44 (66.7) | 22 (68.8) | .83 |
| Died prior to starting dialysis (%) | 1 (1.5) | 5 (15.6) | .013 |
| Remained CKD | 9 (13.4) | 3 (9.4) | .75 |
| Preemptive transplant | 2 (3.0) | 1 (3.1) | 1.00 |
| Initiated dialysis (%) | 52 (77.6) | 23 (71.9) | .71 |
| PD use for first dialysis (primary outcome) | 21 (31.3) | 9 (28.1) | .81 |
| HD use for first dialysis | 31 (46.3) | 14 (43.8) | .89 |
| Crash start HD in-hospitalc | 9 (17.3) | 5 (21.7) | .76 |
Note. PD = peritoneal dialysis; CKD = chronic kidney disease; HD = hemodialysis.
Assessed by multidisciplinary team.
Assessed by patient.
In the subgroup of patients who started HD.
Among the non-Aboriginal patients who initiated dialysis (52 of 67 patients), only 40% (n = 21) initiated PD and the remaining 31 patients initiated HD. Among the Aboriginal patients who initiated dialysis (23 of 32 patients), only 39% (n = 9) initiated PD and the remaining 14 initiated HD. There was no statistically significant difference between the proportion of Aboriginal versus non-Aboriginal patients who initiated PD or HD. The proportion of dialysis patients who initiated PD, versus the proportion of enrolled patients who chose PD, was low in both Aboriginals (39% vs 68.8%) and non-Aboriginals (40% vs 66.7%). A similar proportion of patients also required a “crash start” to initiate HD in hospital in the non-Aboriginal and Aboriginal group (Table 3).
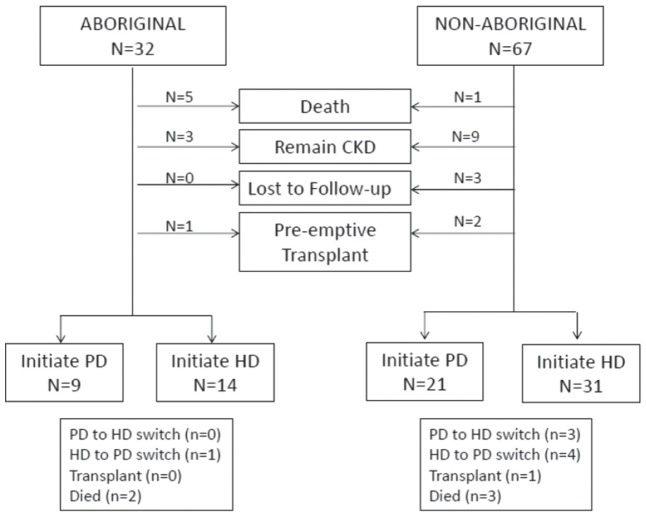
Very few patients had a switch in modality after initiation of dialysis, precluding meaningful comparison or analysis. In non-Aboriginal patients, 4 patients who initiated HD subsequently switched to PD, and 3 of 21 patients who initiated PD had technique failure and switched to HD. In Aboriginal patients, no patients had PD technique failure, and 1 patient switched from HD to PD. A total of 4 non-Aboriginal and 7 Aboriginal patients had died during the study period by the end of follow-up. A total of 3 non-Aboriginal and 1 Aboriginal patients were transplanted by the end of follow-up period (Figure 1).
Figure 1.
Study flow.
Note. CKD = chronic kidney disease; PD = peritoneal dialysis; HD = hemodialysis.
Discussion
This prospective cohort study followed Aboriginal and non-Aboriginal patients from 3 predialysis clinics with the objective of assessing PD use and associated barriers. We hypothesized that Aboriginals would have lower use of PD compared with non-Aboriginals. Barriers to PD were assessed by a patient survey administered prior to initiation of dialysis. Our results demonstrated no significant difference in PD use between non-Aboriginals and Aboriginals (31% vs 28%; P = .81). Aboriginal patients were significantly more likely to die prior to initiation of dialysis compared with non-Aboriginals (15.6% vs 1.5%; P = .013). Lack of money (OR: 21.33; 95% CI: 5.23-86.42; P < .0001) and anxiety (OR: 2.82; 95% CI: 1.12-7.11; P = .03) were identified as significant barriers to PD use in Aboriginal patients. Several other barriers trended to deter non-Aboriginal patients from PD, including lack of motivation, lack of social support, lack of family support, and the belief that dialysis should be done in-hospital, although none achieved statistical significance.
While our study did not demonstrate a significant difference in PD use, prior studies have demonstrated disparities in the use of PD in Aboriginals compared with non-Aboriginals. Tonelli et al reviewed 3823 incident dialysis patients from Alberta, Manitoba, or Saskatchewan using data from the Canadian Organ Replacement Registry. They report that after adjustment for age and comorbid features, Aboriginals were less likely to initiate PD than white patients (OR: 0.51; 95% CI: 0.40-0.65). This disparity in Aboriginal health care use extends to renal transplantation6 and also general health care utilization.21 Our sample size and duration of follow-up were too limited to determine survival after dialysis initiation. However, other studies assessing associations of dialysis modality and mortality in Canadian Aboriginals have had conflicting results. Sood et al report a study of the incident Canadian dialysis population using administrative data where Aboriginals on PD had higher mortality than Caucasians on PD (hazards ratio: 1.36; 95% CI: 1.13-1.62),22 as well as higher PD technique failure rates. These findings may be related to marginal PD candidates who are Aboriginal choosing PD to remain in their communities, thus resulting in an association with mortality and technique failure. However, Tonelli et al report no significant difference in mortality between Aboriginal and non-Aboriginal incident PD patients (HR: 1.00; 95% CI: 0.71-1.40).15 While these retrospective observational studies all attempted to adjust extensively for relevant covariates, residual confounding is still a potential limitation to interpretation. As approximately half of Aboriginal people live outside urban areas, both on and off reserve, PD may offer a valuable modality choice which avoids the need to move to an urban area to access an in-center HD unit. Given the uncertainty in the literature regarding potential adverse outcomes, initiation of PD in Aboriginal patients requires careful and individualized shared decision making to weigh all potential benefits and risks and emphasize the Aboriginal patient’s values and preferences.
We report a higher risk of death prior to initiation of dialysis in Aboriginal compared with non-Aboriginal patients. This finding is in line with the existing literature on the high risk of mortality in Aboriginal patients with CKD,2 perhaps related to reduced access to care5 or remote dwelling.23 However, a complex interplay of cultural, socioeconomic, medical, and psychological factors all contribute to the disproportionate mortality observed in Aboriginal patients and requires further study.
In this study, we report that barriers to PD significantly associated with Aboriginal status included anxiety and lack of money. These findings have not been previously published, but are not surprising given the existing literature on Aboriginal mental health and socioeconomic status. Carrière et al examined 2006 Canadian national census data, linked to the Discharge Abstract Database to describe patterns of hospitalization by Aboriginal identity.24 Compared with non-Aboriginals, First Nations living on reserve had a 3.6 times higher rate of hospitalization for mental and behavioral disorders. Firestone et al conducted a survey of 554 First Nations adults living in Hamilton, Ontario, to assess the prevalence of mental health disorders, and found 39% of respondents met criteria for anxiety and/or depression.25 Income disparity has also been well-documented in Canada’s Aboriginal population, contributing to our finding of lack of money as a significant barrier to PD in Aboriginal patients. In a report from the Canadian Center for Policy Alternatives, Wilson and Macdonald examined data from the 1996, 2001, and 2006 Canadian census to measure the income gap between Aboriginals and non-Aboriginals.26 In 2006, the median income for Aboriginal peoples was $18 962, 30% lower than the $27 097 median income in non-Aboriginals, with income gaps persist regardless of urban or rural residence. In this study, we also report that several factors trended as a barrier to deter non-Aboriginal patients from PD, including lack of motivation, lack of social support, lack of family support, and the belief that dialysis should be done in-hospital. It is of interest to note the trend that social factors in general do not seem to present a substantial barrier to PD for Aboriginal patients in this study, a finding which requires further study. It is interesting that participants reported lack of money as a barrier despite having quite comprehensive coverage for overall health care specifically for ESKD. This highlights a possible fundamental misconception that there would be associated costs with PD. This may reflect the educational program on dialysis modality selection and highlights a potential area for improvement. Even when accounting for deaths prior to initiating dialysis, preemptive transplantation, and modality switches after dialysis initiation, the proportion of patients in the study who chose PD still remained substantially higher than those who used PD. While our observational study did not collect additional patient or provider data to discern barriers to switching from HD to PD after dialysis initiation, this is an important topic for further study.
Several limitations could affect interpretation of the results of this study. First, despite extending the original planned 2-year enrollment period by a year, we were unable to enroll enough Aboriginal patients to meet our original sample size requirements. Thus, while our findings are underpowered to detect differences in the primary outcome of PD use, our findings related to barriers to PD in Aboriginals provide novel information which can be used for future research. Second, inherent to survey-based studies are biases that are difficult to correct. Not all survey questions were completed by all patients, leading to some missing data. Disenfranchised populations such as Aboriginal patients may be less inclined to participate in research, and Aboriginal patients who agreed to enroll in the study may be more motivated and thus more likely to initiate PD. Also, despite the demonstrated high reliability of the survey tool, participant-dependent response bias is difficult to control and can never be fully eliminated.
Third, “lack of money” was identified as a potential barrier by patients and study personnel at the Winnipeg site, and subsequently added to the survey. Thus, data on this variable are available only for Winnipeg patients (n = 76) and not those recruited from Kingston or Moose Factory (n = 23). Despite this lack of barrier data for some patients in the study, “lack of money” had a significant association with Aboriginal status. Finally, our observational study cannot fully address the complex cultural barriers to PD in the Aboriginal population, which would be best assessed using qualitative methodology.
In conclusion, Aboriginal people in Canada have an unduly high burden of kidney disease, with disproportionately high rates of ESKD and lower rates of transplantation compared with non-Aboriginals. Half of Canada’s Aboriginal population lives in rural locations, and PD provides a valuable alternative to in-center HD for these remote dwelling patients. Our study identified anxiety and lack of money as barriers to PD significantly associated with Aboriginal status. These results can be used for future research to devise targeted interventions to overcome these barriers, including standardized predialysis education sessions. Given the complex interplay of cultural, socioeconomic, medical, and psychological factors when choosing dialysis modality, shared decision making between physicians and patients to weigh all potential benefits and risks and emphasize the Aboriginal patient’s values and preferences is of key importance.
Footnotes
Ethics Approval and Consent to Participate: This research project was approved by the Queen’s University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board, and the University of Manitoba Bannatyne Campus Health Research Ethics Board.
Consent for Publication: We have the authors consent for publication.
Availability of Data and Materials: Data is available upon request.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was funded by an unrestricted research grant from Baxter Pharma.
Supplemental Material:Supplementary material is available for this article online.
References
- 1. Statistics Canada. Census of the people: Aboriginal people. https://www12.statcan.gc.ca/nhs-enm/2011/as-sa/99-011-x/99-011-x2011001-eng.cfm. Accessed March 3, 2017.
- 2. Gao S, Manns BJ, Culleton BF, et al. Prevalence of chronic kidney disease and survival among Aboriginal people. J Am Soc Nephrol. 2007;18(11):2953-2959. [DOI] [PubMed] [Google Scholar]
- 3. Canadian Institute for Health Information. End-Stage Renal Disease Among Aboriginal Peoples in Canada: Treatment and Outcomes. Ottawa, ON: Canadian Institute for Health Information; 2013. [Google Scholar]
- 4. Dyck RF, Tan L. Non-diabetic end-stage renal disease among Saskatchewan Aboriginal people. Clin Invest Med. 1998;21(1):33-38. [PubMed] [Google Scholar]
- 5. Gao S, Manns BJ, Culleton BF, et al. Access to health care among status Aboriginal people with chronic kidney disease. CMAJ. 2008;179(10):1007-1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tonelli M, Hemmelgarn B, Manns B, et al. Death and renal transplantation among Aboriginal people undergoing dialysis. CMAJ. 2004;171(6):577-582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hemmelgarn BR. CSCI Joe Doupe Lecture: end stage renal disease among Aboriginal people. Clin Invest Med. 2006;29(6):383-387. [PubMed] [Google Scholar]
- 8. Korevaar JC, Feith GW, Dekker FW, et al. Effect of starting with hemodialysis compared with peritoneal dialysis in patients new on dialysis treatment: a randomized controlled trial. Kidney Int. 2003;64(6):2222-2228. [DOI] [PubMed] [Google Scholar]
- 9. Jager KJ, Korevaar JC, Dekker FW, et al. The effect of contraindications and patient preference on dialysis modality selection in ESRD patients in the Netherlands. Am J Kidney Dis. 2004;43(5):891-899. [DOI] [PubMed] [Google Scholar]
- 10. Fenton SS, Schaubel DE, Desmeules M, et al. Hemodialysis versus peritoneal dialysis: a comparison of adjusted mortality rates. Am J Kidney Dis. 1997;30(3):334-342. [DOI] [PubMed] [Google Scholar]
- 11. Wasserfallen JB, Halabi G, Saudan P, et al. Quality of life on chronic dialysis: comparison between haemodialysis and peritoneal dialysis. Nephrol Dial Transplant. 2004;19(6):1594-1599. [DOI] [PubMed] [Google Scholar]
- 12. Bargman JM, Thorpe KE, Churchill DN; CANUSA Peritoneal Dialysis Study Group. Relative contribution of residual renal function and peritoneal clearance to adequacy of dialysis: a reanalysis of the CANUSA study. J Am Soc Nephrol. 2001;12(10):2158-2162. [DOI] [PubMed] [Google Scholar]
- 13. Canadian Institute for Health Information. Renal replacement therapy for end stage kidney disease. https://www.cihi.ca/sites/default/files/document/kidney_eskd_section_v0.1_en_2017.xlsx. Published February 2017. Accessed April 3, 2017.
- 14. Salvlaggio G, Kelly L, Minore B. Perspectives on health: experiences of First Nations dialysis patients relocated from remote communities for treatment. Can J Rural Med. 2003;8(1):19-24. [Google Scholar]
- 15. Tonelli M, Hemmelgarn B, Manns B, et al. Use and outcomes of peritoneal dialysis among Aboriginal people in Canada. J Am Soc Nephrol. 2005;16(2):482-488. [DOI] [PubMed] [Google Scholar]
- 16. Oliver MJ, Quinn RR, Richardson EP, Kiss AJ, Lamping DL, Manns BJ. Home care assistance and the utilization of peritoneal dialysis. Kidney Int. 2007;71(7):673-678. [DOI] [PubMed] [Google Scholar]
- 17. McLaughlin K, Manns B, Mortis G, Hons R, Taub K. Why patients with ESRD do not select self-care dialysis as a treatment option. Am J Kidney Dis. 2003;41(2):380-385. [DOI] [PubMed] [Google Scholar]
- 18. Manns BJ, Taub K, VanderStraeten C, et al. The impact of education on chronic kidney disease patients’ plans to initiate dialysis with self-care dialysis: a randomized trial. Kidney Int. 2005;68(4):1777-1783. [DOI] [PubMed] [Google Scholar]
- 19. Lavrakas PJ. (2008) Encyclopedia of Survey Research Methods; Sage Publications. [Google Scholar]
- 20. Iliescu EA, Yeates KE, McComb J, Morton AR. Modality choice among Aboriginal incident dialysis patients—influence of geographic location. Perit Dial Int. 2006;26(4):507-508. [PubMed] [Google Scholar]
- 21. Chung H, Ye M, Hanson C, et al. Disparities in healthcare utilisation rates for Aboriginal and non-Aboriginal Albertan residents, 1997-2006: a population database study. PLoS ONE. 2012;7(11):e48355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sood MM, Hemmelgarn B, Rigatto C, et al. Association of modality with mortality among Canadian Aboriginals. Clin J Am Soc Nephrol. 2012;7(12):1988-1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rucker D, Hemmelgarn BR, Lin M, et al. Quality of care and mortality are worse in chronic kidney disease patients living in remote areas. Kidney Int. 2011;79(2):210-217. [DOI] [PubMed] [Google Scholar]
- 24. Carrière G, Bougie E, Kohen D, Rotermann M, Sanmartin C. Acute care hospitalization by Aboriginal identity, Canada, 2006 through 2008. Health Rep. 2016;27(8):3-11. [PubMed] [Google Scholar]
- 25. Firestone M, Smylie J, Maracle S, McKnight C, Spiller M, O’Campo P. Mental health and substance use in an urban First Nations population in Hamilton, Ontario. Can J Public Health. 2015;106(6):e375-e381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wilson D, Macdonald D. The Income Gap Between Aboriginal Peoples and the Rest of Canada. Ottawa, Ontario: Canadian Centre for Policy Alternatives; 2010. [Google Scholar]