Abstract
Background:
Acute ruptures of the ulnar collateral ligament (UCL) of the thumb are common injuries in sports. Surgical repair has yielded excellent results and high return-to-sport (RTS) rates in elite athletes.
Purpose:
To determine (1) the RTS rate in Major League Baseball (MLB) players following thumb UCL repair, (2) postoperative career length and games played per season, (3) pre- and postoperative performance, (4) postoperative performance compared with matched control players, and (5) whether dominant and nondominant hand injuries respond differently.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
MLB players who underwent thumb UCL surgery from August 3, 1987, to September 6, 2016, were identified. Demographic and performance data were collected for each player, and matched controls were identified. RTS in the MLB was defined as playing in at least 1 MLB game after surgery. Comparisons were made by use of paired-samples Student t tests.
Results:
Twenty-one players were identified, with a mean ± SD age of 31.7 ± 3.9 years and mean experience in the MLB of 8.6 ± 3.3 years at time of surgery. Twenty-one players (100%) achieved RTS in the MLB at a mean 120.0 ± 75.9 days. No significant decrease was found in games per season or career length for any position following surgery. Infielders had a significantly lower rate of postoperative wins above replacement (WAR) compared with preoperatively (P = .006), but no significant differences in postoperative performance score were found compared with controls after the index date. No significant difference was found for performance between players undergoing surgery on their dominant hand and those who had surgery on their nondominant (glove) hand compared with controls.
Conclusion:
In this study, 100% of MLB players achieved RTS after thumb UCL repair, with in-season players returning at a mean of 8 weeks. Players who underwent thumb UCL repair played in a similar number of games per season and had similar career lengths in the MLB as controls. Infielders had a significantly lower postoperative WAR compared with preoperatively, but no significant postoperative performance score differences were noted when infielders were compared with post–index date matched controls. No significant performance differences were noted with regard to surgery on dominant and nondominant hands.
Keywords: thumb UCL, MLB, baseball, surgery, return to sport
Acute ruptures of the ulnar collateral ligament (UCL) of the thumb are common injuries in sports.17 The incidence is likely to rise secondary to an increase in athletic participation, with complete ruptures of the thumb UCL occurring at a high frequency in elite athletes.16,18,23 Recent injuries to high-profile Major League Baseball (MLB) players have generated an increased interest in performance and return to sport (RTS) following surgical repair of these injuries.2
The mechanism of injury typically involves hyperabduction or hyperextension of the thumb metacarpophalangeal (MCP) joint while the player is sliding into a base.3,9,14,20 Treatment can be influenced by hand dominance (throwing vs nonthrowing hand).5 Patients with incomplete injuries (sprains) with a stable thumb MCP joint have historically been treated nonoperatively with cast or spica splint immobilization in their nonthrowing, or glove, hand.5,14 However, complete tears of the thumb UCL treated nonoperatively may result in pain, instability, decreased pinch strength, and eventually symptomatic osteoarthritis.5,21 Surgical repair of complete tears and those with a Stener lesion has yielded excellent results in more than 90% of patients, with RTS rates ranging from 96% to 100% in elite-level athletes.6–8,21,23 However, no study has determined outcomes following thumb UCL repair in MLB players.
The purpose of this study was to determine (1) RTS rate in MLB players following thumb UCL repair, (2) postoperative career length and games played per season, (3) pre- and postoperative performance, (4) postoperative performance compared with matched control players, and (5) whether dominant and nondominant hand injuries respond differently. We hypothesized that MLB players who underwent thumb UCL repair would have (1) a greater than 90% RTS rate, (2) no significant difference in postoperative career length and games per season compared with matched controls, (3) no significant difference in postoperative performance compared with preoperative performance, (4) no significant postoperative performance difference when compared with matched controls, and (5) no significant difference between players undergoing surgery on their dominant hand and those who had surgery on their nondominant (glove) hand compared with controls.
Methods
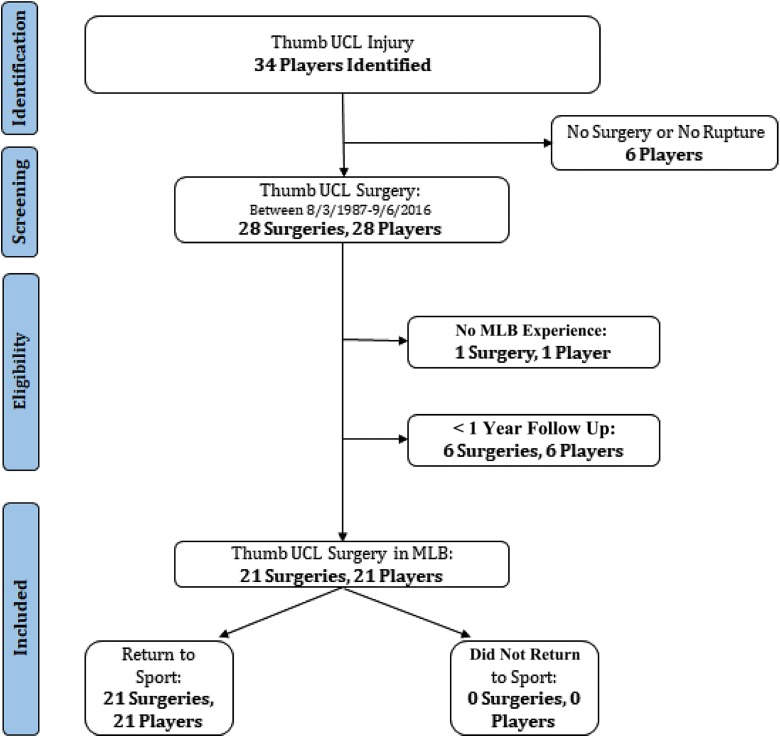
Players in MLB who sustained a thumb UCL tear and underwent repair were evaluated (Figure 1). These players were identified through MLB team websites, publicly available internet-based injury reports, player profiles and biographies, and press releases. The search was manually conducted by 2 orthopaedic surgery residents, with confirmation of the findings by the senior author (P.C.M.). Searches were performed for all MLB teams and players. This method has been used in several other investigations of professional athletes in the National Football League (NFL), National Hockey League (NHL), National Basketball Association (NBA), and Major League Soccer (MLS).10–13,22
Figure 1.
Flowchart illustrating application of exclusion criteria. MLB, Major League Baseball; UCL, ulnar collateral ligament.
All players identified were included in this study as it related to RTS rate. A player was deemed to achieve RTS if he played in any MLB game after surgery, regardless of whether it was during the same season. Inclusion criteria were any athletes on an active roster in the MLB prior to thumb UCL tear. Players were included if they were found to have thumb UCL repair surgery as reported by at least 2 separate sources. Athletes who were injured and underwent procedures before completing their first MLB regular season were excluded. Players who sustained a thumb UCL tear and underwent repair in the 2016 season were excluded from analysis because they had less than a 1-year opportunity to achieve RTS and to obtain postoperative statistics. Players undergoing nonsurgical treatment for a thumb UCL tear were excluded.
Demographic variables, including the player’s age, hand dominance (throwing hand), batting preference (right/left/switch), position, prior professional experience, and date of surgery, were recorded. Players were categorized by their positions, including catcher, infielder (including first baseman, second baseman, shortstop, and third baseman), outfielder (including left fielder, centerfielder, and right fielder), and pitcher. However, no pitchers who underwent surgery for this injury were identified. Performance statistics were collected from http://baseball-reference.com for each player identified before and after thumb UCL repair. Statistics were collected for regular-season MLB games only; spring training, minor league, and playoff games were excluded. Statistics used in this study included games, plate appearances, batting average, on-base percentage, slugging percentage, on-base percentage plus slugging percentage, wins above replacement (WAR), and ultimate zone rating (UZR). WAR is a sabermetric statistic (http://sabr.org/sabermetrics/statistics) used to assess a player’s overall value, and it takes into account fielding, hitting, and base running. A WAR of 2.0 means that over the course of the season, the player contributed to 2 wins more than a “replacement player” (an average player in the MLB). UZR is a statistic that quantifies the number of runs a player saves or gives up as determined by fielding. It is stratified into Gold Glove (+15.0), great (+10.0), above average (+5.0), average (0.0), below average (–5.0), poor (–10.0), and awful (–15.0). Preoperative UZR was calculated from the season of injury and the prior season. Postoperative UZR was calculated from the injury season and the first season postoperatively.
A control group was selected so we could compare data. Controls were matched to study cases based on position, age, years of experience, body mass index (BMI), and performance data prior to the surgery date. Each control was given an index date that matched the case player’s surgery date to compare postoperative or postindex performance. For example, if a player had surgery 3 years into his career, the control’s index date was 3 years into his career.
Player statistics for cases before and after surgery and for controls before and after the index date were collected and aggregated. Each statistical category was divided by seasons played to account for discrepancies in the number of total seasons played. The 1994 and 1995 MLB strike was taken into account because the definition of a full season in those years was an average of 113 and 144 games, respectively. The number of games played for athletes during that time frame was adjusted to reflect a full 162-game season.
All players were included in analyses of RTS, games per season, and career length. A Kaplan-Meier survivorship curve with “retirement” as the endpoint was constructed postoperatively for cases and post–index date for controls. Comparisons between case and control groups and preoperative and postoperative time points were made by use of 2-tailed paired-samples Student t tests; P values less than .05 were considered significant.
Results
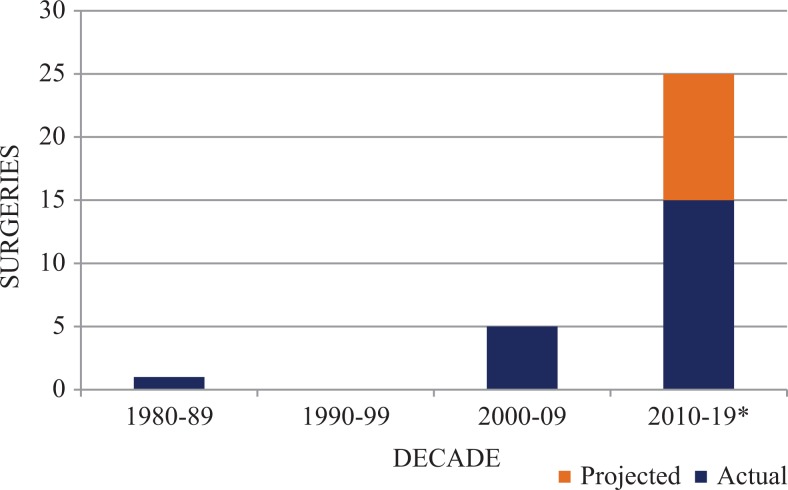
Overall, 21 thumb UCL repairs in 21 players from 1987 to 2015 were analyzed (Table 1). Fifteen repairs (71.4%) had occurred since 2010 (Figure 2). The mean ± SD player age was 31.7 ± 3.9 years and the mean experience in the MLB was 8.6 ± 3.3 years at time of surgery. Surgery occurred less than 1 week following injury in 15 players (71.4%), it occurred less than 1 month following injury in 1 player (4.8%), and the remaining 5 players (23.8%) waited until the off-season to undergo surgery. The infield positions (n = 11) represented the largest proportion of players who underwent thumb UCL repair (52.3%) (Table 1). Eight players (38.1%) underwent thumb UCL repair in their dominant hand (throwing hand). No significant performance difference was found between players undergoing surgery on their dominant hand and those who had surgery on their nondominant (glove) hand compared with controls (P > .05).
TABLE 1.
Time to Return to Sport (RTS) by Position
| Position | n | RTS, % | Days to RTS, mean ± SD |
|---|---|---|---|
| Catcher | 5 | 100.0 | 198.2 ± 42.1 |
| Infielder | 11 | 100.0 | 86.2 ± 60.7 |
| Outfielder | 5 | 100.0 | 116.2 ± 83.9 |
| Overall | 21 | 100.0 | 120.0 ± 75.9 |
Figure 2.
Number of thumb ulnar collateral ligament surgeries in Major League Baseball by decade. *Projected.
All 21 players (100%) achieved RTS in MLB at an average of 120.0 ± 75.9 days. Two players (9.5%) returned to sport in less than 6 weeks. An additional 6 players (28.6%) returned between 6 and 12 weeks, and the remaining 13 players (61.9%) returned after 12 weeks. Of the players who underwent surgery in-season, 11 (73.3%) returned within the same season as their injury and returned at an average of 56.2 ± 15.0 days. Five players (3 infielders and 2 catchers) underwent surgery after a prolonged period (average of 167.8 days) of playing with a thumb UCL injury. Two of these players injured their dominant hand.
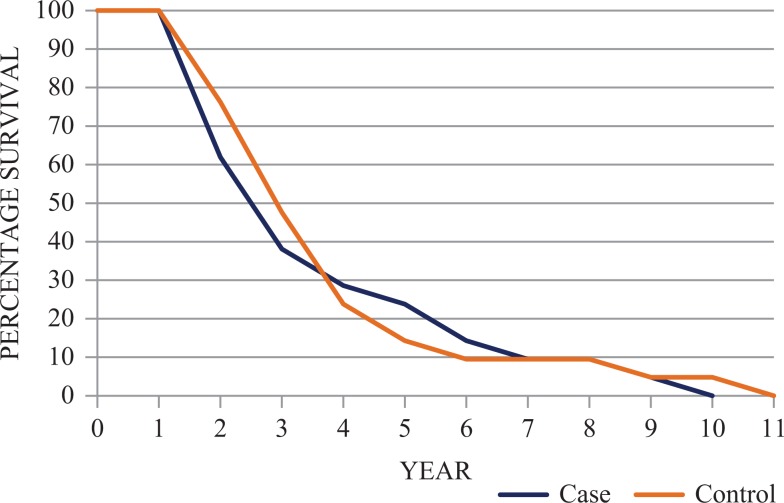
The overall 1-year MLB career survival rate of players undergoing thumb UCL repair was 100% (Figure 3). Players in the control group were not in the MLB significantly longer than players who underwent thumb UCL repair (3.3 ± 2.2 vs 3.1 ± 2.4 years, respectively; P > .05) (Tables 2 and 3). Players in the control group played in a similar number of games per season after the index date versus players who underwent thumb UCL repair (100.7 ± 30.0 vs 115.5 ± 28.5 games per season, respectively; P > .05).
Figure 3.
Kaplan-Meier survival analysis for cases and controls. Zero (0) signifies year of surgery for cases and index year for controls.
TABLE 2.
Presurgery and Preindex Statistics for Cases and Controls by Positiona
| Catcher | Infielder | Outfielder | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Statistic | Cases | Controls | P | Cases | Controls | P | Cases | Controls | P |
| Age | 32.8 ± 5.6 | 33.2 ± 4.5 | .771 | 31.7 ± 2.2 | 31.4 ± 2.2 | .281 | 30.6 ± 5.3 | 30.9 ± 4.7 | .678 |
| Exp | 9.4 ± 3.8 | 9.3 ± 5.0 | .964 | 8.4 ± 2.8 | 8.0 ± 1.9 | .388 | 8.0 ± 4.2 | 7.9 ± 3.3 | .894 |
| BMI | 28.0 ± 2.3 | 29.5 ± 3.1 | .337 | 26.5 ± 2.0 | 27.3 ± 1.9 | .279 | 28.0 ± 2.0 | 27.5 ± 1.5 | .730 |
| G/s | 104.9 ± 28.1 | 92.7 ± 25.6 | .238 | 118.1 ± 19.4 | 116.6 ± 24.0 | .846 | 129.1 ± 7.1 | 128.5 ± 20.9 | .943 |
| PA/s | 391.6 ± 135.3 | 338.6 ± 133.0 | .257 | 465.9 ± 123.9 | 466.4 ± 144.0 | .992 | 551.4 ± 32.4 | 534.3 ± 82.3 | .582 |
| BA | 0.277 ± 0.029 | 0.281 ± 0.027 | .311 | 0.281 ± 0.021 | 0.276 ± 0.017 | .221 | 0.275 ± 0.015 | 0.276 ± 0.020 | .695 |
| OBP | 0.337 ± 0.036 | 0.340 ± 0.032 | .952 | 0.351 ± 0.027 | 0.342 ± 0.023 | .132 | 0.342 ± 0.015 | 0.362 ± 0.026 | .063 |
| SLG | 0.409 ± 0.028 | 0.438 ± 0.077 | .718 | 0.441 ± 0.061 | 0.428 ± 0.046 | .723 | 0.475 ± 0.037 | 0.475 ± 0.054 | .790 |
| OPS | 0.746 ± 0.059 | 0.778 ± 0.100 | .705 | 0.791 ± 0.082 | 0.769 ± 0.059 | .452 | 0.816 ± 0.040 | 0.837 ± 0.079 | .478 |
aValues are presented as mean ± SD. P values determined by 2-tailed paired Student t test. BA, batting average; BMI, body mass index; Exp, seasons in Major League Baseball; G/s, games per season; OBP, on-base percentage; OPS; on-base percentage plus slugging percentage; PA/s, plate appearances per season; SLG, slugging percentage.
TABLE 3.
Postsurgery and Postindex Statistics for Cases and Controls by Positiona
| Catcher | Infielder | Outfielder | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Statistic | Cases | Controls | P | Cases | Controls | P | Cases | Controls | P |
| Seasons | 3.6 ± 3.4 | 5.3 ± 3.8 | .052 | 3.3 ± 2.3 | 2.6 ± 0.9 | .289 | 2.2 ± 1.6 | 2.9 ± 1.3 | .506 |
| G/s | 99.3 ± 43.9 | 93.8 ± 23.7 | .808 | 116.7 ± 18.4 | 98.1 ± 45.9 | .156 | 129.0 ± 26.8 | 113.4 ± 27.6 | .166 |
| PA/s | 372.4 ± 208.7 | 334.2 ± 104.1 | .945 | 441.1 ± 128.9 | 360.5 ± 219.0 | .050 | 502.9 ± 127.9 | 452.8 ± 163.5 | .185 |
| BA | 0.267 ± 0.066 | 0.270 ± 0.023 | .418 | 0.267 ± 0.028 | 0.271 ± 0.053 | .169 | 0.255 ± 0.021 | 0.260 ± 0.032 | .686 |
| OBP | 0.336 ± 0.056 | 0.349 ± 0.044 | .181 | 0.335 ± 0.025 | 0.340 ± 0.052 | .283 | 0.344 ± 0.046 | 0.351 ± 0.041 | .265 |
| SLG | 0.344 ± 0.066 | 0.414 ± 0.071 | .390 | 0.390 ± 0.064 | 0.425 ± 0.108 | .988 | 0.430 ± 0.066 | 0.451 ± 0.076 | .318 |
| OPS | 0.680 ± 0.119 | 0.763 ± 0.105 | .214 | 0.725 ± 0.086 | 0.765 ± 0.158 | .770 | 0.774 ± 0.110 | 0.803 ± 0.117 | .239 |
aValues are presented as mean ± SD. P values determined by 2-tailed paired Student t test. BA, batting average; G/s, games per season; OBP, on-base percentage; OPS, on-base percentage plus slugging percentage; PA/s, plate appearances per season; SLG, slugging percentage.
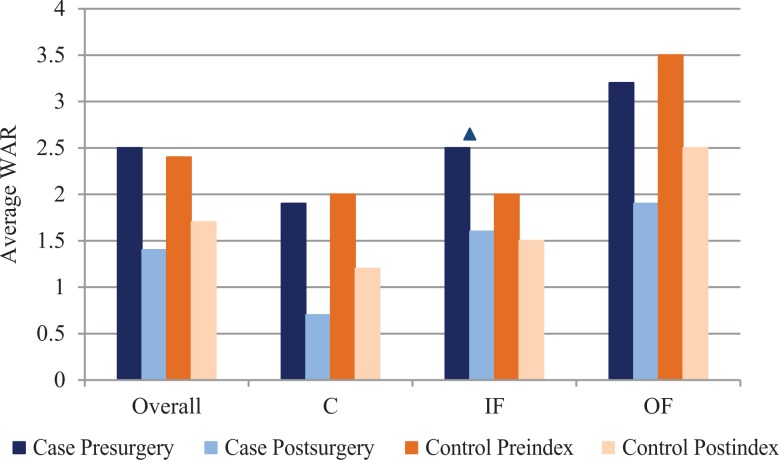
No significant (P > .05) differences were found in demographic, performance, and games per season data between cases and matched controls presurgery and preindex (Table 2) and in postoperative performance scores compared with preoperative scores (Table 3). We found no statistically significant (P > .05) decrease in games per season for any position after surgery (Table 3). No positions had a significant difference (P > .05) in postoperative performance when compared with preoperative, and we found no significant performance difference postoperatively when compared with matched controls (Table 3). Infielders had a significantly lower WAR following surgery compared with preoperatively (P = .0056), but no significant difference was noted between cases and controls (Figure 4).
Figure 4.
Average wins above replacement (WAR) by position before and after surgery compared with controls before and after the index date. ▴Statistically significant difference between pre- and postsurgery average WAR. C, catcher; IF, infielder; OF, outfielder.
We found no significant difference in UZR for infielders preoperatively and postoperatively (4.2 ± 6.1 vs 3.7 ± 7.2, respectively; P = .730). As well, we found no significant postoperative UZR difference between cases and controls (–0.3 ± 6.5; P = .201) for infielders. No significant postoperative UZR differences were noted for infielders based on hand dominance (n = 5) (preoperative, 5.2 ± 5.4; postoperative, 4.1 ± 8.4; P = .648).
Discussion
The study hypotheses were confirmed, with a 100% RTS rate and similar postoperative career length and games per season postoperatively following repair of thumb UCL tears in MLB players. No positions had a significant difference in postoperative performance compared with preoperative performance, and no significant postoperative performance difference was found in players compared with matched controls. Additionally, we found no significant difference between players undergoing surgery on their dominant hand and those who had surgery on their nondominant (glove) hand compared with controls. Infielders had a significantly lower WAR following surgery compared with preoperatively, but we found no significant difference between cases and controls.
No prior study has evaluated performance and RTS following thumb UCL repair in MLB players. However, analyses of collegiate and professional football players have revealed RTS rates ranging from 96% to 100% after surgery.6,10–13,23,24 The RTS rate from these prior studies is similar to the results of the present study in MLB players (100% RTS). Werner et al24 demonstrated an average RTS time of 49 days in collegiate football position players. This is shorter than the time found in the present study of MLB players, where those who underwent surgery in-season had an average RTS of 56.2 days. Of the 13 players who achieved RTS after 12 weeks, 61.5% were out of season when they were expected to return. Therefore, the RTS time is likely higher than it would have been had the players not been in the off-season.
The faster RTS in football players compared with MLB players is also likely due to the ability of football players to return to play while still wearing a thumb spica cast. Throwing, catching, and batting in baseball necessitate manual dexterity and fine motor movement of the hands, requirements that limit a player’s ability to return with a playing splint or cast. This limitation could affect players’ throwing or glove hand because thumb gripping power has been suggested to influence infielders’ glove hand on any ball fielded away from their body. With respect to return to batting, it has also been suggested that because the dominant hand (usually the top hand on the bat) often comes off the bat on follow-through, return to swinging a bat may be slower in the nondominant hand (low hand on the bat). However, this was not the case in the present study, as no differences were found in batting and fielding statistics based on hand dominance.
Catchers had the longest RTS time of all position groups at 198 days. The increased RTS time is likely due to the demand placed on the thumb MCP joint for catching and throwing the baseball after each pitch. It is also possible that the small sample size favored injuries at the end of the season versus the beginning of the season, leading to a longer RTS time through the off-season. Further studies are needed to assess the biomechanical effect of thumb UCL repair on throwing mechanics in baseball players.
By using controls who were matched in terms of age, MLB experience, and performance, the current study was able to accurately make performance data comparisons for case players against controls at the same junction of their career. Simply comparing a player to himself may not account for rapid improvements (or regressions) in performance that are prevalent among similar players in the league.
We found no significant postoperative performance score differences when case participants were compared with post–index date matched controls, for all 3 positions studied. Infielders had a significantly lower WAR compared with preoperatively, with the player contributing to nearly 1 less win per season following surgery. Catchers and outfielders also had decreased WAR postoperatively and post–index date, but this finding did not reach statistical significance. This indicates that thumb UCL tear and subsequent repair likely did not have a significant detrimental influence on the development and performance of these players after they achieved RTS. Postoperative decrease in performance may be attributable to the natural deterioration of one’s career.
No pitchers were identified who underwent thumb UCL repair. This may be attributable to the pitchers’ limited exposure to fielding or batting that would place the thumb at risk for injury. American League pitchers do not bat, whereas National League pitchers bat in fewer games than position players, as they only play every 5 days. When they do play, pitchers have low on-base percentages, further limiting their exposure to injury from sliding into base.
This study has limitations. The use of publicly available data to identify players who underwent thumb UCL repair is prone to selection, reporting, and observer bias. However, this method of data acquisition has been used in multiple previous studies.1,4,12,15,19 In this study, career length was not adjusted for “time missed” for players who underwent thumb UCL repair. Their time in the league was in fact longer than reported; however, their seasons spent playing (ie, career length) after surgery are accurate. Inherent to this type of study, multiple unknown confounding variables exist, such as no direct physical contact or access to medical records to corroborate diagnosis. The use of public data limits the ability to determine the chronicity and severity of the injury or the presence of a Stener lesion. We were also unable to reliably determine whether any patient had a repair or reconstruction of the thumb UCL. Heterogeneity of surgeons, surgeon skill, or surgical technique is an additional limitation. Other limitations include the absence of patient-reported outcomes, incomplete follow-up, and unknown career length for players still in the MLB. Also, the small number of players increases the risk of beta error in the present study.
Conclusion
One hundred percent of MLB players achieved RTS after thumb UCL repair, with in-season players returning at an average of 8 weeks. Players who underwent thumb UCL repair played in a similar number of games per season and had similar career lengths in the MLB as controls. Infielders had a significantly lower postoperative WAR compared with preoperatively, but we found no significant postoperative performance score differences when compared with postindex matched controls. We found no significant performance differences between surgery on dominant and nondominant hands.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: P.C.M. is on the speaker’s bureau/is a paid presenter for Vericel. J.D.H. receives research support from DePuy and Smith & Nephew; is a paid consultant for NIA Magellan and Smith & Nephew; receives royalties from SLACK Inc; and is a paid presenter or speaker for Smith & Nephew and Ossur.
Ethical approval was not sought for the present study.
References
- 1. Amin NH, Old AB, Tabb LP, Garg R, Toossi N, Cerynik DL. Performance outcomes after repair of complete Achilles tendon ruptures in National Basketball Association players. Am J Sports Med. 2013;41(8):1864–1868. [DOI] [PubMed] [Google Scholar]
- 2. Associated Press. Houston Astros star Carlos Correa could miss eight weeks. New York Times, July 19, 2017 https://www.nytimes.com/2017/07/19/sports/houston-astros-carlos-correa-thumb-injury.html?mcubz=0. Accessed August 15, 2017.
- 3. Camp CL, Curriero FC, Pollack KM, et al. The epidemiology and effect of sliding injuries in major and minor league baseball players. Am J Sports Med. 2017;45(10):2372–2378. [DOI] [PubMed] [Google Scholar]
- 4. Cerynik DL, Lewullis GE, Joves BC, Palmer MP, Tom JA. Outcomes of microfracture in professional basketball players. Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1135–1139. [DOI] [PubMed] [Google Scholar]
- 5. Chhor KS, Culp RW. Baseball commentary “thumb ligament injuries: RCL and UCL.” Hand Clin. 2012;28(3):371–372. [DOI] [PubMed] [Google Scholar]
- 6. Derkash RS, Matyas JR, Weaver JK, et al. Acute surgical repair of the skier’s thumb. Clin Orthop Relat Res. 1987;216:29–33. [PubMed] [Google Scholar]
- 7. Dinowitz M, Trumble T, Hanel D, Vedder NB, Gilbert M. Failure of cast immobilization for thumb ulnar collateral ligament avulsion fractures. J Hand Surg Am. 1997;22(6):1057–1063. [DOI] [PubMed] [Google Scholar]
- 8. Downey DJ, Moneim MS, Omer GE., Jr Acute gamekeeper’s thumb: quantitative outcome of surgical repair. Am J Sports Med. 1995;23(2):222–226. [DOI] [PubMed] [Google Scholar]
- 9. Engelhardt JB, Christensen OM, Christiansen TG. Rupture of the ulnar collateral ligament of the metacarpophalangeal joint of the thumb. Injury. 1993;24(1):21–24. [DOI] [PubMed] [Google Scholar]
- 10. Erickson BJ, Harris JD, Cole BJ, et al. Performance and return to sport after anterior cruciate ligament reconstruction in National Hockey League players. Orthop J Sports Med. 2014;2(9):2325967114548831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Erickson BJ, Harris JD, Cvetanovich GL, et al. Performance and return to sport after anterior cruciate ligament reconstruction in male Major League Soccer players. Orthop J Sports Med. 2013;1(2):2325967113497189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Erickson BJ, Harris JD, Heninger JR, et al. Performance and return-to-sport after ACL reconstruction in NFL quarterbacks. Orthopedics. 2014;37(8):e728–e734. [DOI] [PubMed] [Google Scholar]
- 13. Harris JD, Erickson BJ, Bach BR, Jr, et al. Return-to-sport and performance after anterior cruciate ligament reconstruction in National Basketball Association players. Sports Health. 2013;5(6):562–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Heyman P. Injuries to the ulnar collateral ligament of the thumb metacarpophalangeal joint. J Am Acad Orthop Surg. 1997;5(4):224–229. [DOI] [PubMed] [Google Scholar]
- 15. Jack RA, Evans DC, Echo A, et al. Performance and return to sport after sports hernia surgery in NFL players. Orthop J Sports Med. 2017;5(4):2325967117699590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Johnson JW, Culp RW. Acute ulnar collateral ligament injury in the athlete. Hand Clin. 2009;25(3):437–442. [DOI] [PubMed] [Google Scholar]
- 17. Jones MH, England SJ, Muwanga CL, et al. The use of ultrasound in the diagnosis of injuries of the ulnar collateral ligament of the thumb. J Hand Surg Br. 2000;25(1):29–32. [DOI] [PubMed] [Google Scholar]
- 18. Lee AT, Carlson MG. Thumb metacarpophalangeal joint collateral ligament injury management. Hand Clin. 2012;28(3):361–370. [DOI] [PubMed] [Google Scholar]
- 19. Namdari S, Baldwin K, Anakwenze O, Park M-J, Huffman GR, Sennett BJ. Results and performance after microfracture in National Basketball Association athletes. Am J Sports Med. 2009;37(5):943–948. [DOI] [PubMed] [Google Scholar]
- 20. Ritting AW, Baldwin PC, Rodner CM. Ulnar collateral ligament injury of the thumb metacarpophalangeal joint. Clin J Sport Med. 2010;20(2):106–112. [DOI] [PubMed] [Google Scholar]
- 21. Samora JB, Harris JD, Griesser MJ, Ruff ME, Awan HM. Outcomes after injury to the thumb ulnar collateral ligament—a systematic review. Clin J Sport Med. 2013;23(4):247–254. [DOI] [PubMed] [Google Scholar]
- 22. Su WK. Performance-based outcomes following lumbar discectomy in professional athletes in the National Football League. Spine. 2010;35(12):1247–1251. [DOI] [PubMed] [Google Scholar]
- 23. Werner BC, Belkin NS, Kennelly S, et al. Injuries to the collateral ligaments of the metacarpophalangeal joint of the thumb, including simultaneous combined thumb ulnar and radial collateral ligament injuries, in National Football League athletes. Am J Sports Med. 2017;45(1):195–200. [DOI] [PubMed] [Google Scholar]
- 24. Werner BC, Hadeed MM, Lyons ML, et al. Return to football and long-term clinical outcomes after thumb ulnar collateral ligament suture anchor repair in collegiate athletes. J Hand Surg Am. 2014;39(10):1992–1998. [DOI] [PubMed] [Google Scholar]