Abstract
Purpose
We report a case of erlotinib-associated severe recalcitrant bilateral keratouveitis after uneventful corneal ethylenediaminetetraacetic acid (EDTA) chelation in a patient with non-small cell lung cancer (NSCLC); discontinuation of erlotinib led to complete resolution.
Observations
An elderly person presented with band keratopathy (BSK) of undetermined etiology in the both eyes, associated with foreign body sensation and constant tearing. The patient was on oral erlotinib treatment 150 mg PO daily for 1 year for NSCLC status post radiation therapy. Corneal EDTA chelation was performed in both eyes under topical anesthesia for BSK. Four days after surgery, the patient presented with severe pain in both eyes. Slit lamp evaluation revealed 5 mm × 7 mm epithelial defect with clear margins in the right eye and 6 × 7 mm epithelial defect with thick central corneal infiltrate in the left eye. Hypopyon was noticed in both eyes and intense inflammation obscured the details of anterior segment. Intense antibiotic treatment was initiated. After discussion with the oncology services, oral erlotinib was temporarily discontinued. This resulted in resolution of keratitis and hypopyon in both eyes, within one week.
Conclusions
and importance: Systemic use of erlotinib suppresses local immunity, facilitates infection and enhances inflammatory reaction in the eye. Clinicians should be cautious and plan any ocular interventional treatment in collaboration with oncology team to prevent adverse outcomes.
Keywords: Erlotinib, Band keratopathy, Corneal chelation, Keratouveitis
1. Introduction
Erlotinib (Tarceva; Genetech Inc, San Francisco, CA), a reversible tyrosine kinase inhibitor that selectively blocks the epidermal growth factor receptor (EGFR), is commonly used as a first line chemotherapy agent for non-small cell lung cancer (NSCLC) and pancreatic cancer. Trichomegaly, dry eyes and delayed corneal wound healing1, 2, 3 are noted with the use of erlotinib.
We report a case of erlotinib-associated severe recalcitrant bilateral keratouveitis after uneventful corneal ethylenediaminetetraacetic acid (EDTA) chelation in a patient with NSCLC. Discontinuation of erlotinib led to complete resolution of both keratitis and uveitis.
2. Case report
An elderly patient, in 7th decade of life presented with band keratopathy of undetermined etiology in both eyes, associated with annoying foreign body sensation and constant tearing. The patient was on oral Erlotinib treatment 150 mg daily for 1 year for NSCLC status post radiation therapy. Patient’s other medical problems included biopsy confirmed sarcoidosis, chronic obstructive pulmonary disease, hypertension, type II diabetes mellitus, osteoarthritis and gastroesophageal reflux disease. The patient was pseudophakic in both eyes with end-stage glaucoma. The patient’s best corrected visual acuity (BCVA) was 20/50 in the right eye and light perception in the left. Intraocular pressure was 10 mmHg in the right and 5 mmHg in the left. Slit lamp biomicroscopy examination (SLE) showed bilateral interpalpebral band keratopathy.
Under topical anesthesia, EDTA was applied after removal of corneal epithelia; calcium plaques were scraped off uneventfully in both eyes. Bandage contact lenses (CL) were applied along with topical vigamox and 1% pred forte QID for postoperative care.
Four days after surgery, the patient presented with severe pain in both eyes. BCVA was hand motion at face in the right eye and light perception in the left. SLE revealed 5 mm × 7 mm epithelial defect with clear margins in the right eye and 6 × 7 mm epithelial defect with thick central corneal infiltrate in the left. Hypopyon was noticed in both eyes (right 1 mm, left <1 mm), and intense inflammation obscured the details of anterior segment. Corneal scraping was performed on both eyes and send for microbiological evaluation (gram staining, KOH slide evaluation and cultures). Ultrasound did not reveal vitritis in either eye. Intense antibiotic treatment was initiated (topical fortified vancomycin and tobramycin alternating every hour and oral doxycyclin 100 mg BID PO). Concurrent erlotinib use was of concern but oral erlotinib could not be discontinued per recommendation of oncology services.
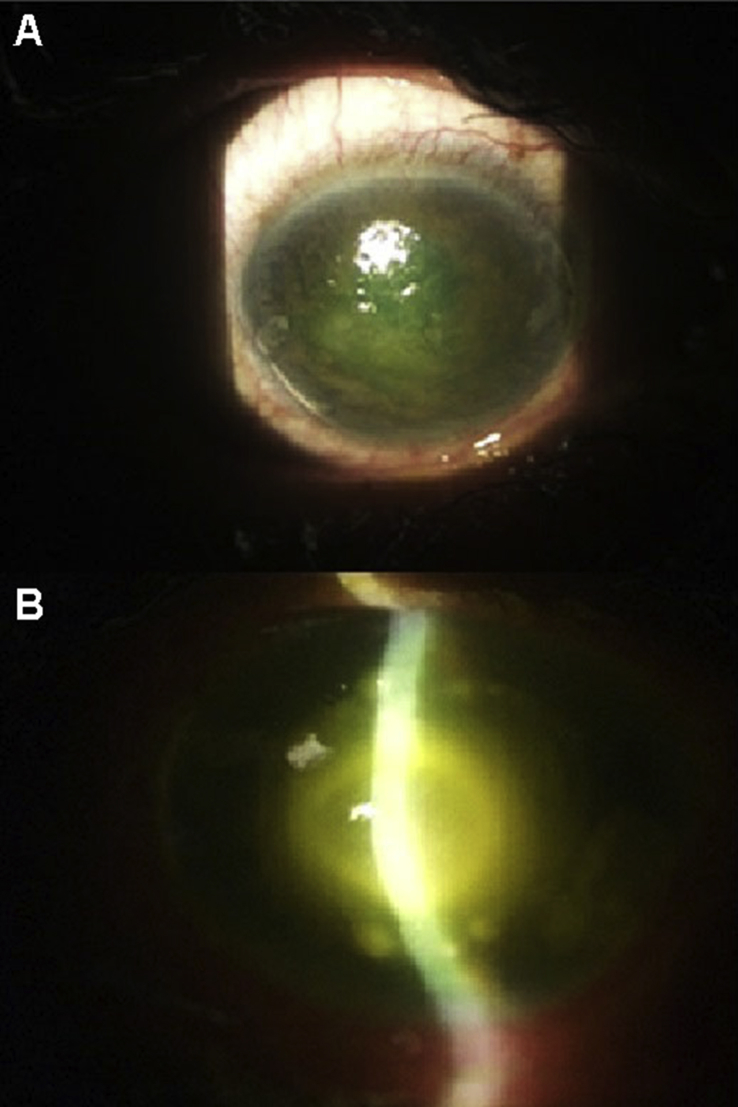
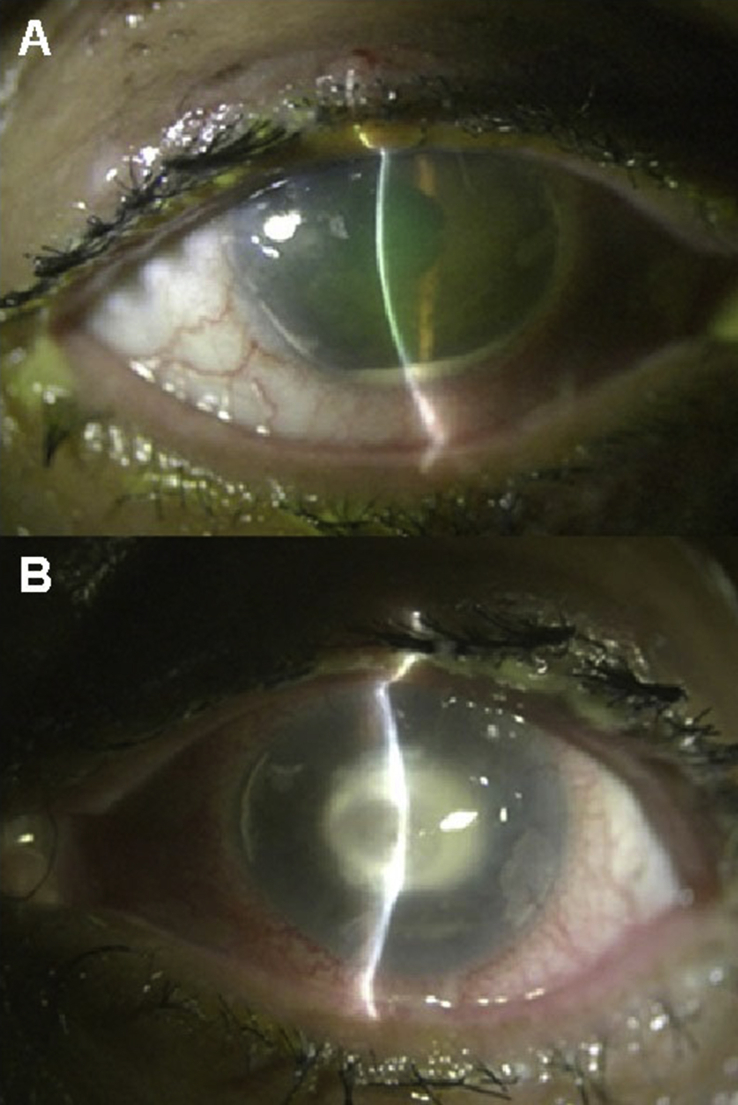
One week later, the left eye developed new satellite corneal infiltrates and thinning of the stroma in the central area despite antibiotic therapy (Fig. 1A–B). Culture reports from the corneal scraping were negative. Non-healing corneal epithelial defect, as well as persistent hypopyon in the anterior chamber were still noted three weeks after the surgery in both eyes despite intensive antibiotic and antifungal treatment (Fig. 2A–B).
Fig. 1.
Post op day 15. (A) The right eye showed corneal epithelial defect measuring about 6 × 4 mm without associated corneal infiltrates. (B) The left eye presented with central corneal infiltrate, stromal thinning and multiple small satellite infiltrates around the central ulcer.
Fig. 2.
Post op day 21. (A) Anterior chamber hypopyon was noted in the right eye with persistent corneal epithelial defect but no corneal infiltrates. (B) The left eye presented with dense central corneal infiltrates and stromal thinning.
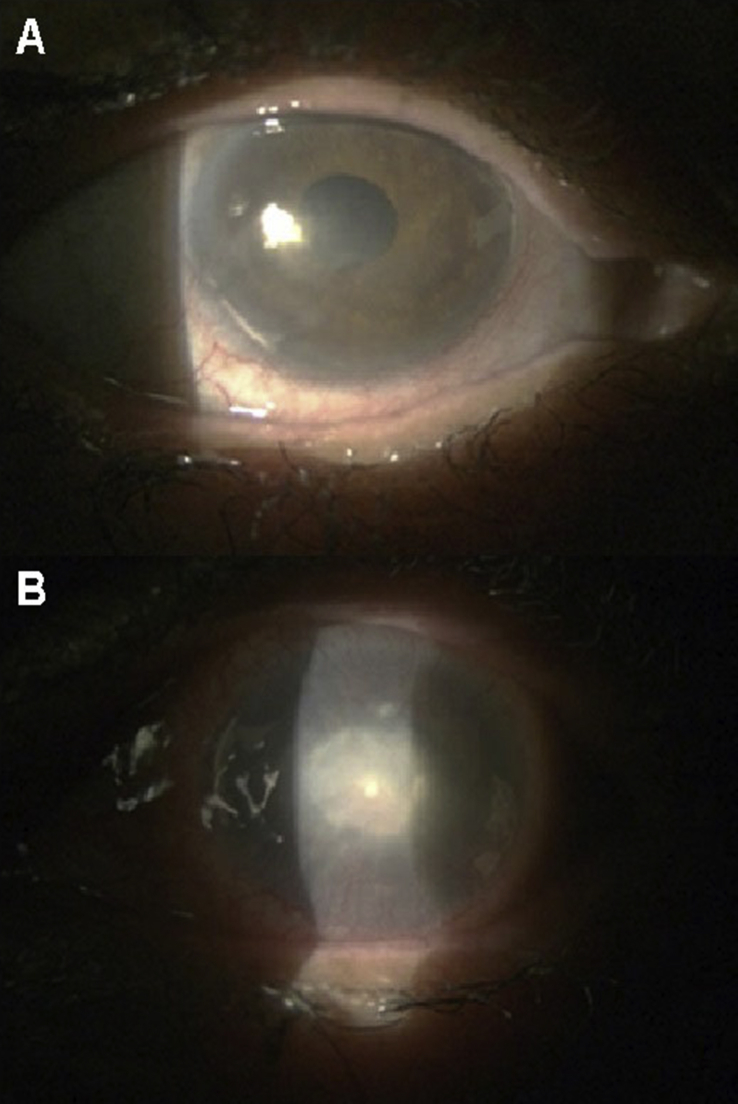
After further discussion with the oncology services, oral erlotinib was discontinued. Subsequently discontinuation of erlotinib, lead to resolution of keratitis, as well as hypopyon resolved in both eyes, in one week. BCVA improved to 20/50 in the right eye and remained light perception in the left (Fig. 3A–B).
Fig. 3.
Post op day 35. (A) The right eye showed healed corneal epithelial defect with trace stromal scar in the central area. (B) The left eye had dense central stromal scar with surrounding neovascularization.
3. Discussion
Erlotinib (Tarceva), a reversible tyrosine kinase inhibitor (selective blocker of EGFR), is commonly used as a first line chemotherapy agent for NSCLC.4 However, erlotinib induces ocular complications including trichomegaly and delayed corneal wound healing.1 Erlotinib violates ocular immune status, and induces inflammatory anterior uveitis.5, 6, 7 It may also suppress local immunity and facilitate ocular infection through suppression of human beta defensin 2 and 3, natural defense against Staphylococcus epidermidis.8 In addition, erlotinib impairs T-cell-mediated immune response both in vitro and in vivo through inhibition of T cell proliferation and activation via down-regulation of the c-Raf/ERK cascade and Akt signaling pathway.9 Rao V et al.10 reported a case of bilateral acquired toxoplasmic retinochoroiditis during erlotinib therapy. Erlotinib inhibits epidermal growth factor receptor–induced activation of STAT, which impairs host resistance to Toxoplasma gondii.10 The clinical course was atypical in our case and despite two weeks of intensive topical antibiotics treatment, keratitis was recalcitrant in both eyes. The patient developed recurrent corneal infiltrates with severe anterior uveitis, which was an atypical clinical presentation for infectious keratouveitis. We believe systemic use of erlotinib impaired local immunity and facilitated keratitis in both eyes. In addition, it exacerbated uveitis in the right eye through alteration of immune status. Discontinuation of erlotinib resulted in complete clinical recovery for both eyes.
4. Conclusion
In summary, systemic use of erlotinib suppresses local immunity, facilitates infection and enhances inflammatory reaction in the eye. Clinicians should be cautious and plan any ocular interventional treatment in collaboration with oncology team to prevent adverse outcomes.
4.1. Informed consent
Not obtained. Personal identifying information was removed from this report as informed consent to publish such information was not obtained.
Conflict of interest
None.
References
- 1.Zhang G., Basti S., Jampol L.M. Acquired trichomegaly and symptomatic external ocular changes in patients receiving epidermal growth factor receptor inhibitors: case reports and a review of literature. Cornea. 2007;26:858–860. doi: 10.1097/ICO.0b013e318064584a. [DOI] [PubMed] [Google Scholar]
- 2.Johnson K.S., Levin F., Chu D.S. Persistent corneal epithelial defect associated with erlotinib treatment. Cornea. 2009;28:706–707. doi: 10.1097/ICO.0b013e31818fdbc6. [DOI] [PubMed] [Google Scholar]
- 3.Morishige N., Hatabe N., Morita Y., Yamada N., Kimura K., Sonoda K.H. Spontaneous healing of corneal perforation after temporary discontinuation of erlotinib treatment. Case Rep. Ophthalmol. 2014;5:6–10. doi: 10.1159/000358082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Triano L.R., Deshpande H., Gettinger S.N. Management of patients with advanced non-small cell lung cancer: current and emerging options. Drugs. 2010;70:167–179. doi: 10.2165/11532200-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 5.Lim L.T., Blum R.A., Cheng C.P., Hanifudin A. Bilateral anterior uveitis secondary to erlotinib. Eur. J. Clin. Pharmacol. 2010;66:1277–1278. doi: 10.1007/s00228-010-0873-7. [DOI] [PubMed] [Google Scholar]
- 6.Ali K., Kumar I., Usman-Saeed M. Erlotinib-related bilateral anterior uveitis. BMJ Case Rep. 2011;24 doi: 10.1136/bcr.03.2011.3988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumar I., Ali K., Usman-Saeed M., Saeed M.U. Follow-up of erlotinib related uveitis. BMJ Case Rep. 2012;14 doi: 10.1136/bcr.12.2011.5418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park K., Ommori R., Imoto K., Asada H. Epidermal growth factor receptor inhibitors selectively inhibit the expressions of human β-defensins induced by Staphylococcus epidermidis. J. Dermatol. Sci. 2014;75:94–99. doi: 10.1016/j.jdermsci.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 9.Luo Q., Gu Y., Zheng W., Wu X., Gong F., Gu L., Sun Y., Xu Q. Erlotinib inhibits T-cell-mediated immune response via down-regulation of the c-Raf/ERK cascade and Akt signaling pathway. Toxicol. Appl. Pharmacol. 2011;251:130–136. doi: 10.1016/j.taap.2010.12.011. [DOI] [PubMed] [Google Scholar]
- 10.Rao V., Schneider E., Proia A.D., Fekrat S. Development of bilateral acquired toxoplasmic retinochoroiditis during erlotinib therapy. JAMA Ophthalmol. 2014;132:1150–1152. doi: 10.1001/jamaophthalmol.2014.1088. [DOI] [PubMed] [Google Scholar]