Abstract
Purpose
To report a case of regained corneal sensation and function in a patient with neurotrophic keratopathy due to direct damage to the long ciliary nerves by performing a corneal neurotization procedure using ipsilateral supraorbital nerve. Surgical technique is described in detail as well as a review of the literature on corneal neurotization.
Observations
A patient with devastating corneal anesthesia and poor visual acuity refractory to other treatments underwent a new surgical technique involving an ipsilateral supraorbital nerve transfer to the surrounding limbus to restore corneal sensation. At 8 months follow up, there was resolution of corneal stromal opacification documented with photographs and greatly improved corneal sensation by testing with a wisp of cotton in all 4 quadrants. Her visual acuity had improved, and at two years she was stable with even more improvement in visual acuity and ocular surface health.
Conclusions and importance
We present the first successful case of corneal neurotization with ipsilateral supraorbital nerve in a patient with corneal anesthesia from a local injury to the long ciliary nerves. Our case demonstrates that the described method of corneal neurotization is a viable option for patients with recalcitrant neurotrophic keratopathy and an intact ipsilateral frontal nerve.
Keywords: Neurotrophic keratopathy, Cornea, Corneal neurotization, Long ciliary nerves, Corneal anesthesia
1. Introduction
Normal sensation of the cornea is provided by innervation from the ophthalmic division of the trigeminal nerve, and is required for initiating the blink reflex, preserving epithelial integrity, and maintaining limbal stem cell function.1, 2 Failure to provide adequate sensation is termed corneal anesthesia, which can be subdivided into acquired or congenital causes. Congenital corneal anesthesia is extremely rare, with acquired forms most commonly resulting from infection, inflammatory processes, trauma, neoplasia, or iatrogenic disease.3
The insensate cornea results in a clinical condition known as neurotrophic keratopathy (NK), also referred to as neurotrophic keratitis. NK is a degenerative disease of the cornea caused by an impairment of corneal sensory innervation, characterized by decreased or absent corneal sensitivity resulting in epithelial keratopathy, ulceration, and perforation.1, 3 Treatment options are limited, with many treatment modalities failing to preserve vision and leading to recalcitrant progression.
Neurotization is the process of transferring a healthy donor nerve segment to a tissue to re-establish either motor or sensory innervation.4 There are few reports on corneal neurotization in literature performed on patients with anesthetic corneas secondary to intracranial pathology.4, 5, 6, 7 Previous reports described contralateral supraorbital or supratrochlear nerve transfers to the cornea or re-innervation using sural nerve grafts anastomosed to supratrochlear nerve in patients with concurrent trigeminal and facial nerve palsies or congenital corneal anesthesia.4, 5, 6, 7
2. Case report
A 61-year-old healthy female was referred to our Oculoplastic Surgery service for evaluation of burning and irritation in her left eye that was unresponsive to conservative management. Her ocular symptoms began following retinal detachment surgery in the left eye involving an encircling scleral buckle, dense peripheral retina endolaser, and pars plana vitrectomy 6 months prior to presentation to our service. She also underwent an uncomplicated phacoemulsification with insertion of posterior chamber intraocular lens surgery 3 months prior to her evaluation by our service. Her cataract surgery was followed by a tapering course of non-steroidal anti-inflammatory and antibiotic drops over a month. Patient reported worsening of her symptoms following cataract extraction. The patient provided written consent for publication of personal information including medical record details and photographs.
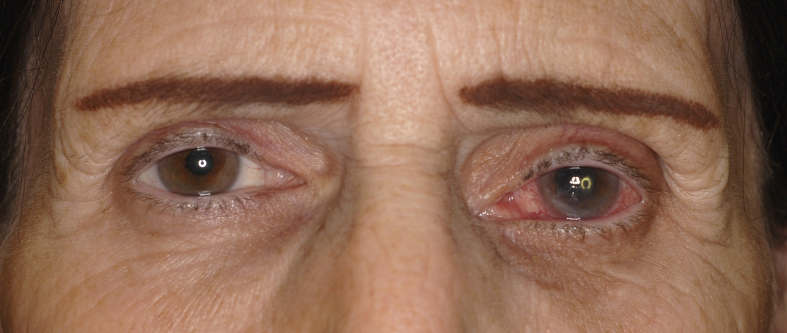
On presentation, her best-corrected visual acuity (BCVA) in the left eye was 20/200. She had absent corneal sensation and blink in all four quadrants by testing with a wisp of cotton. On examination, she had anterior stromal opacification, inferior neovascularization, and an epithelial defect (Fig. 1). Her dilated fundus examination was notable for a flat macula with dense peripheral laser scars outside of the vascular arcades. Her external exam was notable for a medial canthal tendon dystopia due to a childhood injury and intact sensation to light touch over her scalp.
Fig. 1.
Pre-operative photograph at initial presentation showing conjunctival injection, corneal opacification, and peripheral neovascularization in the left eye with best-corrected visual acuity (BCVA) of 20/200 at this visit.
To maintain corneal integrity, the patient underwent lateral tarsorrhaphy and placement of a gold weight in her upper eyelid. She improved postoperatively, with complete healing of the corneal epithelial defect, but with persistent stromal scarring. Her visual acuity continued to worsen to count fingers at one foot. After exhausting most known treatment options, it was decided to proceed with the corneal neurotization procedure.
The surgical technique is a variant of previously reported corneal neurotization procedures and will be described in detail in the following paragraphs.
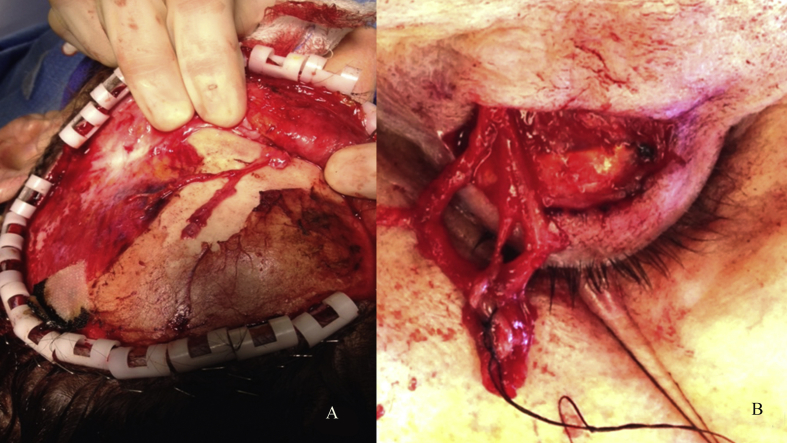
The procedure began by making a hemicoronal incision just behind the hairline from mid-line to the auricular helix. Sharp and blunt dissection was carried out in the subgaleal plane and laterally over the deep temporal fascia. Dissection was carried inferiorly to release the temporal line of fusion, and then continued until 2 cm above the superior orbital rim. At this level the periosteum was incised, and subperiosteal dissection carried to the superior orbital rim. The dissection of the deep branch of the supraorbital nerve was then carried cephalad from the supraorbital notch. Three branches of the nerve were isolated and severed 6 cm from the supraorbital notch (Fig. 2a).
Fig. 2.
A. Intraoperative photograph of the isolated supraorbital nerve. B. An intraoperative photograph showing supraorbital nerve branches tunneled through an upper eyelid crease incision.
An upper eyelid incision was made and the nerve fibers were tunneled into the palpebral incision (Fig. 2b). A blepharotomy medial to the medial horn of the levator aponeurosis was then performed. The nerves were further tunneled through the blepharotomy incision into the superior conjunctival fornix.
A conjunctival incision was made at the 12 o'clock 7 mm above the corneal scleral limbus, and a blunt abdominal needle was used to access the space under Tenon's capsule. The branches of the nerves were placed in the sub-Tenon's space 360° around the limbus. The conjunctiva was then closed to completely cover the nerves. An amniotic membrane graft was then sutured to the surface of the eye with interrupted 8-0 polyglactin suture. No complications were noted during the procedure or during her post-operative recovery period.
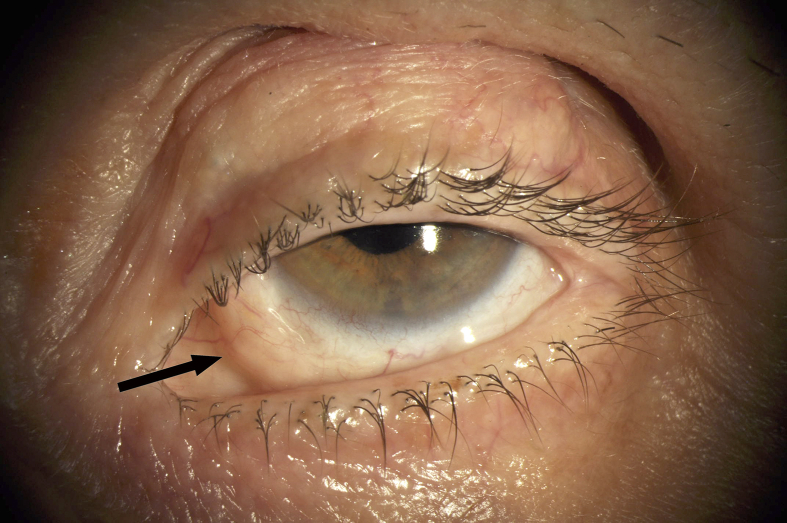
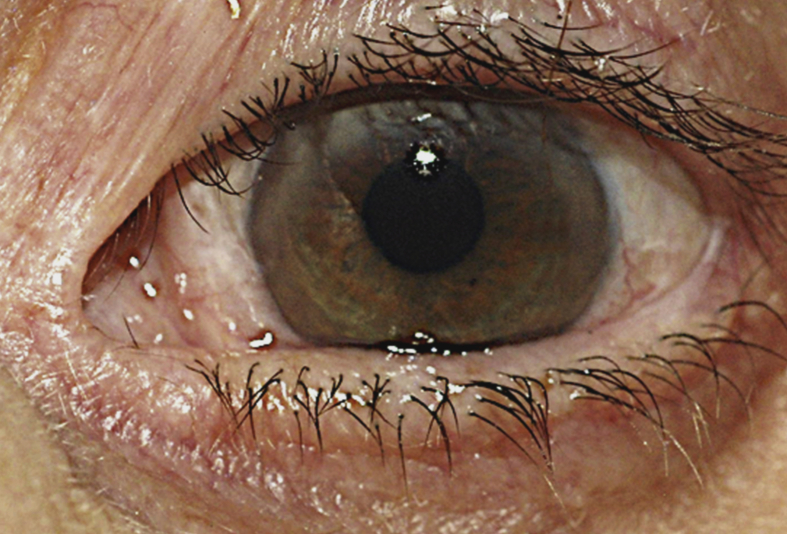
At eight months follow up, patient's BCVA improved to 20/100 with resolution of corneal stromal opacification and greatly improved corneal sensation by testing with a wisp of cotton in all 4 quadrants (Fig. 3). Her scalp sensation was completely restored. She had no evidence of synkinesis. No complications were noted during her post-operative recovery. Given the significant improvement in her ocular surface her tarsorrhaphy was severed and gold weight was removed. At a two-year follow-up, the patient reported continued ocular comfort and improved vision. Her BCVA improved to 20/30, and slit lamp examination showed a clear and well-lubricated cornea. No epithelial staining was noted with lissamine green or fluorescein. There was persistence of an intact corneal sensation. A very noticeable finding was the presence of an induced blink with corneal contact by a wisp of cotton (Fig. 4).
Fig. 3.
At 8-month postoperative follow up there is resolution of corneal opacification, improvement of corneal sensation, and visual acuity. Medially, a branch of the supraorbital nerve is seen deep to the bulbar conjunctiva (arrow).
Fig. 4.
At a 2-year postoperative follow up the cornea remains clear with intact sensation. The best-corrected visual acuity (BCVA) of the left eye at this visit was 20/30.
3. Discussion
The insensate cornea represents a difficult diagnosis to treat, with various treatments giving patients only temporary relief and eventually leading to poor outcomes. Additionally, the current surgical techniques for NK focus on protecting the cornea, and have minimal to no effect on improving corneal sensation.3
Corneal neurotization is a novel approach to obtain a definitive treatment for the condition. The first report of corneal neurotization in literature was described in 2009 by Terzis et al.,6 where six patients with unilateral facial and trigeminal palsies underwent direct neurotization of the cornea using the contralateral supraorbital and supratrochlear branches of the ophthalmic division of the trigeminal nerve, with the average time to reestablish corneal sensibility being 2.8 years.6 The etiologies for trigeminal neuropathy included intracranial pathology including a meningioma, acoustic neuromas, and skull base trauma. Half of the patients were found to have improved visual acuity, and all eyes showed improved corneal health and sensibility. Complications included one subgaleal hematoma requiring evacuation and an asymptomatic subconjunctival neuroma that did not require treatment.6 Allevi et al. described a case of a woman with acquired unilateral V and VII cranial nerve palsies following removal of a vestibular schwannoma who successfully regained corneal sensibility after direct corneal neurotization with the contralateral supraorbital and supratrochlear nerves, and subsequently underwent successful penetrating keratoplasty 6 months later.7 The authors used a similar technique for corneal neurotization described by Terzis et al. No complications were reported. Another study by Elbaz et al. reported the use of a segment of the medial cutaneous branch of the sural nerve with end-to-side coaptation of the graft to an isolated contralateral supratrochlear nerve using transverse upper lid incisions.4, 5 They performed the procedure on four children and one adult with corneal anesthesia from a variety of CNS pathologies including posterior fossa tumor, basal skull fracture, and cerebellar hypoplasia.4, 5 All patients had markedly improved corneal sensation at 6 months with no corneal anesthesia-related complications since the surgery.4
In contrast to other reports, our patient had isolated corneal anesthesia from local damage to the long ciliary nerves following intraocular procedures. Since the ipsilateral frontal nerve was still intact, we were able to use her ipsilateral supraorbital nerve to directly neurotize the cornea.4, 5, 6, 7 Patients with multiple cranial nerve palsies from neurosurgical interventions, trauma, or tumors have more proximal nerve damage necessitating the use of the contralateral sensory nerves for successful neurotization. The ability to use an ipsilateral sensory nerve decreases the size of the scalp incision and dissection needed for exposure. This is in contrast to the original technique described by Terzis,6 where a bicoronal incision was required to perform contralateral neurotization. Although Elbaz et al. demonstrated successful corneal neurotization without making a scalp incision using sural nerve grafts on a small number of patients, the failure of interpositional nerve grafts to provide appropriate innervation is well known.9, 10 In addition, our technique avoids the donor site morbidity associated with harvesting sural nerve autograft, and reliance on the nerve graft to provide appropriate conduit for sensory nerve regeneration.4, 5 Complications of autologous nerve grafts are well known and include formation of neuromas, scarring, and permanent loss of nerve function.8 We do not believe that a well-designed hemicoronal incision with appropriately executed surgical technique carries significant morbidity. In our experience, there is a rapid return of scalp sensation and the scar is inconspicuous behind the hairline. The use of amniotic membrane graft is also unique to our technique. We believe it serves to protect the corneal epithelium in the immediate postoperative period before the re-establishment of corneal sensibility. We also describe the first case of corneal neurotization performed solely by a team of ophthalmologists.
Our patient's vision and corneal sensation improved at 8 months after surgery, with continued improvement at a 2 year follow up, consistent with the report by Elbaz et al.9 Our study is limited by the fact that the corneal sensation was evaluated by physical examination alone. Measure of corneal sensibility using esthesiometer as well as the study of the morphological parameters, including nerve imaging, would have offered further insights into the mechanisms of corneal reinnervation.6, 11, 12
4. Conclusions
To our knowledge we present the first successful case of corneal neurotization with the ipsilateral supraorbital nerve utilizing eyelid and hemicoronal incisions in a patient with corneal anesthesia from a local injury to the long ciliary nerves. Our case demonstrates that the described method of corneal neurotization is a viable option for patients with recalcitrant neurotrophic keratopathy and an intact ipsilateral frontal nerve.
References
- 1.Garcia-Hirschfeld J., Lopez-Briones L.G., Belmonte C. Neurotrophic influences on corneal epithelial cells. Exp. Eye Res. 1994;59:597–605. doi: 10.1006/exer.1994.1145. [DOI] [PubMed] [Google Scholar]
- 2.Ueno H., Ferrari G., Hattori T., Saban D.R. Dependence of corneal stem/progenitor cells on ocular surface innervation. Invest Ophthalmol. Vis. Sci. 2012;53:867–872. doi: 10.1167/iovs.11-8438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mantelli F., Nardella C., Tiberi E., Sacchetti M. Congenital corneal anesthesia and neurotrophic keratitis: diagnosis and management. BioMed Res. Int. 2015 Sept 16 doi: 10.1155/2015/805876. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elbaz U., Bains R., Zuker R.M., Borschel G.H. Restoration of corneal sensation with regional nerve transfers and nerve grafts: a new approach to a difficult problem. JAMA Ophthalmol. 2014;132:1289–1295. doi: 10.1001/jamaophthalmol.2014.2316. [DOI] [PubMed] [Google Scholar]
- 5.Bains R.D., Elbaz U., Zuker R. Corneal neurotization from the supratrochlear nerve with sural nerve grafts: a minimally invasive approach. Plast. Reconstr. Surg. 2015;135:397–400. doi: 10.1097/PRS.0000000000000994. [DOI] [PubMed] [Google Scholar]
- 6.Terzis J.K., Dryer M.M., Bodner B.I. Corneal neurotization: a novel solution to neurotrophic keratopathy. Plast. Reconstr. Surg. 2009;123:112–120. doi: 10.1097/PRS.0b013e3181904d3a. [DOI] [PubMed] [Google Scholar]
- 7.Allevi F., Fogagnolo P., Rossetti L., Biglioli F. Eyelid reanimation, neurotisation, and transplantation of the cornea in a patient with facial palsy. BMJ Case Rep. 2014 doi: 10.1136/bcr-2014-205372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sabongi R.G., Fernandes M., Dos Santos J.B. Peripheral nerve regeneration with conduits: use of vein tubes. Neural Regen. Res. 2015;4:529–533. doi: 10.4103/1673-5374.155428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tomita K., Nishibayashi A., Yano K., Hosokawa K. Differential reanimation of the upper and lower face using 2 interpositional nerve grafts in total facial nerve reconstruction. Plastic Reconstr. Surg. Glob. Open. 2015;3(10):e544. doi: 10.1097/GOX.0000000000000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoke A. Mechanisms of Disease: what factors limit the success of peripheral nerve regeneration in humans? Nat. Clin. Pract. Neurol. 2006;2:448–454. doi: 10.1038/ncpneuro0262. [DOI] [PubMed] [Google Scholar]
- 11.Lambiase A., Sacchetti M., Mastropasqua A., Bonini S. Corneal changes in neurosurgically induced neurotrophic keratitis. JAMA Ophthalmol. 2013;131:1547–1553. doi: 10.1001/jamaophthalmol.2013.5064. [DOI] [PubMed] [Google Scholar]
- 12.Muller R.T., Pourmirzaie R., Pavan-Longston D., Cavalcanti B.M. In vivo confocal microscopy demonstrates bilateral loss of endothelial cells in unilateral herpes simplex keratitis. Invest Ophthalmol. Vis. Sci. 2015;58:4899–4906. doi: 10.1167/iovs.15-16527. [DOI] [PMC free article] [PubMed] [Google Scholar]