Abstract
Tissue diagnosis with vitreous and/or retinal biopsy usually confirms the diagnosis of primary vitreoretinal lymphoma. Multiple imaging modalities like fundus fluorescein angiography, fundus autofluorescence, and optical coherence tomography have been used to support the diagnosis of vitreoretinal lymphoma. We report a case of a 74-year-old lady diagnosed with primary vitreoretinal lymphoma showing a novel fluorescein angiographic finding of capillary dropout. We hypothesize that this clinical finding on the fluorescein angiogram may be due to the occlusion of the retinal vasculature by the malignant tumor cells. This finding also suggests the possible intraocular invasion of the malignant lymphomatous cells into the inner retinal layers.
Keywords: Vitreoretinal lymphoma, Capillary dropout, Fluorescein angiography
Established Facts
• Fluorescein angiography findings described for vitreoretinal lymphomas include retinal pigment epithelium granularity, staining, and late leakage.
• These findings are mainly due to the location of the lymphomatous infiltrates underneath the retinal pigment epithelium.
Novel Insights
• Capillary dropout on fluorescein angiography is a novel finding seen in vitreoretinal lymphomas.
• The presence of capillary dropouts on fluorescein angiography may suggest lymphomatous invasion into the inner retinal layers.
Introduction
Primary vitreoretinal lymphoma (VRL) is a rare malignancy with an aggressive clinical course. It is usually considered as a subset of primary central nervous system lymphoma. Often masquerading as idiopathic uveitis, differential diagnosis should include infectious and noninfectious etiologies, particularly conditions like sarcoidosis, tuberculosis, viral retinitis, and syphilis [1]. Given the aggressive nature and poor prognosis associated with this malignancy, prompt diagnosis of VRL is critical to ensure appropriate referral and treatment [2]. Tissue diagnosis with vitreous and/or retinal biopsy confirms the diagnosis. Multiple imaging modalities like fundus fluorescein angiography (FFA), fundus autofluorescence (FAF), and optical coherence tomography (OCT) have been used to support the diagnosis of VRL. We report a case of primary VRL showing a novel finding of localized capillary dropouts on FFA.
Case Report
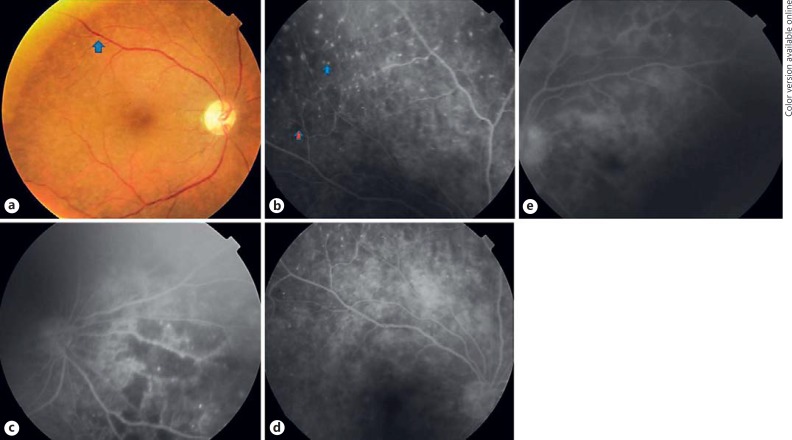
A 74-year-old female was referred to the uvea clinic of a tertiary eye care institution with symptoms of gradual painless deterioration in vision in both eyes for 3 years. She was being treated as a case of vitritis with oral steroids for a long duration. On further enquiry, there was no past history of eye pain, redness, trauma, or fever. There was no history of tuberculosis or tuberculosis contact. She denied any neurological symptoms such as headache, nausea, or vomiting. There was no systemic history of diabetes or hypertension. On examination, her best-corrected visual acuity was counting fingers at 1 m and near vision <N36 in both eyes. Intraocular pressure by Goldmann applanation tonometry in both eyes was 9 mm Hg. Anterior segment examination was normal with no aqueous chamber cells or flare. Cataract was present in both eyes. Fundus examination of both eyes showed a hazy media and vitritis 3+ in both eyes. The disc was seen hazily in both eyes. Ophthalmic ultrasound of both eyes showed a moderate number of moderately reflective homogenous echoes in the vitreous cavity with an attached retina. In view of non-resolving vitritis, she underwent diagnostic and therapeutic vitrectomy in both eyes. The vitreous sample was sent for cytopathology examination to our in-house accredited laboratory. Cytological analysis of the vitreous sample showed large round atypical lymphocytes with scanty cytoplasm and irregular vesicular nuclei. Immunohistochemistry showed CD20 positivity suggestive of a B-cell lymphoid neoplasm (Fig. 1). A diagnosis of primary VRL was established. Magnetic resonance imaging (MRI) of the brain revealed no central nervous system lymphoma. Whole body positron emission tomography scan was normal. Two weeks following vitrectomy, her visual acuity improved to 6/12 in both eyes. Anterior segment examination and intraocular pressure were normal. Fundus examination showed a clear media with multiple deep, light yellow spots dispersed across the entire fundus (Fig. 2a). Further imaging with FFA and OCT was done. FFA showed multiple pinpoint hyperfluorescent spots spread across the entire fundus with hypofluorescent areas interspersed in between. Late-phase angiogram of the right eye showed a well-defined area of capillary dropouts across the retina and a large area nasal to the optic disc and extending inferonasally (Fig. 2b-e). There were no features of inflammation like disc leakage, cystoid macular edema, or vessel wall staining noted in both eyes. Angiographic features of vascular occlusions and diabetic retinopathy were absent. OCT examination showed multiple small pigment epithelial detachments in both eyes. No macular thickening was noted. The patient was treated with multiple injections of intravitreal methotrexate in both eyes. Her last follow-up was at 1 year post-treatment and her visual acuity was maintained at 6/12 in both eyes. There were no features of disease reactivation in either eye. MRI of the brain was normal.
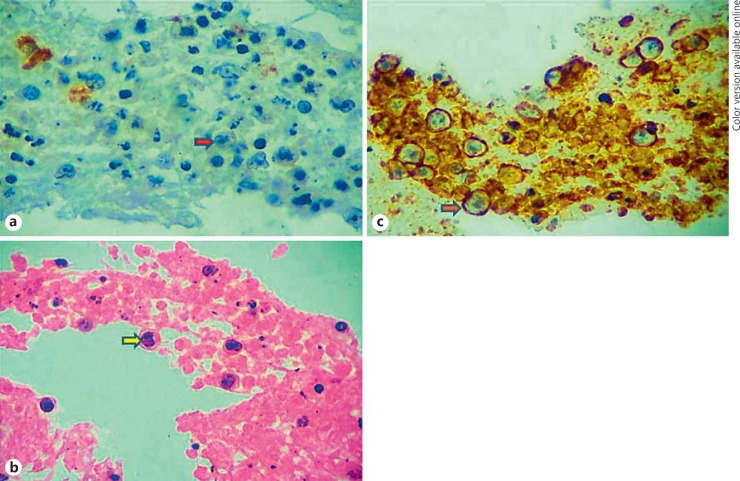
Fig. 1.
Cytopathology images of the patient. a, b Smears with hematoxylin-eosin and Giemsa stains show moderately cellular lymphoid cell population with abundant atypical lymphoid cells which are large, hyperchromatic with the chromatin less darker, prominent nucleoli, and scanty cytoplasm. Also seen are mature, small- and intermediate-sized lymphocytes accompanying these atypical lymphoid cells. The background shows fibrinous material. No granuloma is seen. c Immunohistochemistry shows atypical lymphoid cells with CD20 membrane positivity (orange arrow with blue outline).
Fig. 2.
Color fundus and fluorescein angiogram findings in a patient with primary vitreoretinal lymphoma. a Color fundus image of the right eye showing multiple pinpoint deep, light yellow lesions spread across the retina. b Early-phase fluorescein angiogram image of the right eye showing multiple hyperfluorescent spots across the retina (blue arrow with blue outline) and multiple focal areas of capillary dropouts (red arrow with blue outline). c Large areas of capillary dropout seen nasal to the optic disc and extending inferonasally in the right eye. d Late-phase fluorescein angiogram image of the right eye showing diffuse granularity over the entire fundus. There is no flower petal leakage at the macula or disc leakage noted in the right eye. e Early-phase fluorescein angiogram image of the left eye showing diffuse granularity across the retina with no cystoid macular edema or disc leakage.
Discussion
Diagnosis in VRL is a major challenge for ophthalmologists. The disease typically masquerades as chronic intermediate and/or posterior uveitis in aged patients and it is unresponsive to corticosteroid therapy [3]. Diagnostic vitrectomy for cytologic analysis with immediate handling is essential for the diagnosis of VRL. In primary VRL, the most common findings were related to sub-retinal pigment epithelium lymphomatous infiltrates that created focal pigment epithelial detachments leading to abnormal near-infrared reflectance imaging, FAF, FFA, and indocyanine green angiography signals [4, 5, 6, 7]. Velez et al. [7] described the characteristic fluorescein angiographic features in primary VRL [8]. The most common angiographic characteristics included disturbances at the level of the retinal pigment epithelium, such as granularity, blockage, and late staining. These changes correlated well to histopathological findings of lymphoma cells located between the retinal pigment epithelium and Bruch's membrane. Perivascular staining or leakage and cystoid macular edema were rare. In our case, fluorescein angiography findings showed granularity and focal areas of capillary dropouts. We did not find any report of capillary dropout being described in patients with VRL. The possible explanation for this angiographic finding is due to the intraocular invasion of the lymphomatous cells into the inner retinal layers and subsequent blockage of the retinal vasculature by these tumor cells. To add, there were no findings suggestive of vascular occlusions, diabetic retinopathy, or ocular inflammation like disc leakage, macular leakage, or perivascular leakage in our patient.
To conclude, capillary dropouts on fluorescein angiography is a novel finding noted in patients with VRL. In addition to other findings like presence of vitritis on clinical examination, presence of intraretinal hyperreflective lesions on SD-OCT images, and presence of hypoautofluorescent lesions on FAF, the presence of capillary dropouts on FFA may also suggest lymphomatous invasion into the inner retinal layers.
Statement of Ethics
Written informed consent has been obtained from the patient.
Disclosure Statement
The authors have no conflicts of interest.
References
- 1.Chan CC, Buggage RR, Nussenblatt RB. Intraocular lymphoma. Curr Opin Ophthalmol. 2002;13:411–418. doi: 10.1097/00055735-200212000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Raparia K, Chang CC, Chévez-Barrios P. Intraocular lymphoma: diagnostic approach and immunophenotypic findings in vitrectomy specimens. Arch Pathol Lab Med. 2009;133:1233–1237. doi: 10.5858/133.8.1233. [DOI] [PubMed] [Google Scholar]
- 3.Levasseur SD, Wittenberg LA, White VA. Vitreoretinal lymphoma: a 20-year review of incidence, clinical and cytologic features, treatment, and outcomes. JAMA Ophthalmol. 2013;131:50–55. doi: 10.1001/jamaophthalmol.2013.569. [DOI] [PubMed] [Google Scholar]
- 4.Ishida T, Ohno-Matsui K, Kaneko Y, Tobita H, Shimada N, Takase H, Mochizuki M. Fundus autofluorescence patterns in eyes with primary intraocular lymphoma. Retina. 2010;30:23–32. doi: 10.1097/IAE.0b013e3181b408a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Casady M, Faia L, Nazemzadeh M, Nussenblatt R, Chan CC, Sen HN. Fundus autofluorescence patterns in primary intraocular lymphoma. Retina. 2014;34:366–372. doi: 10.1097/IAE.0b013e31829977fa. [DOI] [PubMed] [Google Scholar]
- 6.Fardeau C, Lee CP, Merle-Béral H, Cassoux N, Bodaghi B, Davi F, Lehoang P. Retinal fluorescein, indocyanine green angiography, and optic coherence tomography in non-Hodgkin primary intraocular lymphoma. Am J Ophthalmol. 2009;147:886–894. doi: 10.1016/j.ajo.2008.12.025. 894.e1. [DOI] [PubMed] [Google Scholar]
- 7.Velez G, Chan CC, Csaky KG. Fluorescein angiographic findings in primary intraocular lymphoma. Retina. 2002;22:37–43. doi: 10.1097/00006982-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Mapelli C, Invernizzi A, Barteselli G, Pellegrini M, Tabacchi E, Staurenghi G, Viola F. Multimodal imaging of vitreoretinal lymphoma. Ophthalmologica. 2016;236:166–174. doi: 10.1159/000447412. [DOI] [PubMed] [Google Scholar]