Abstract
Purpose of review
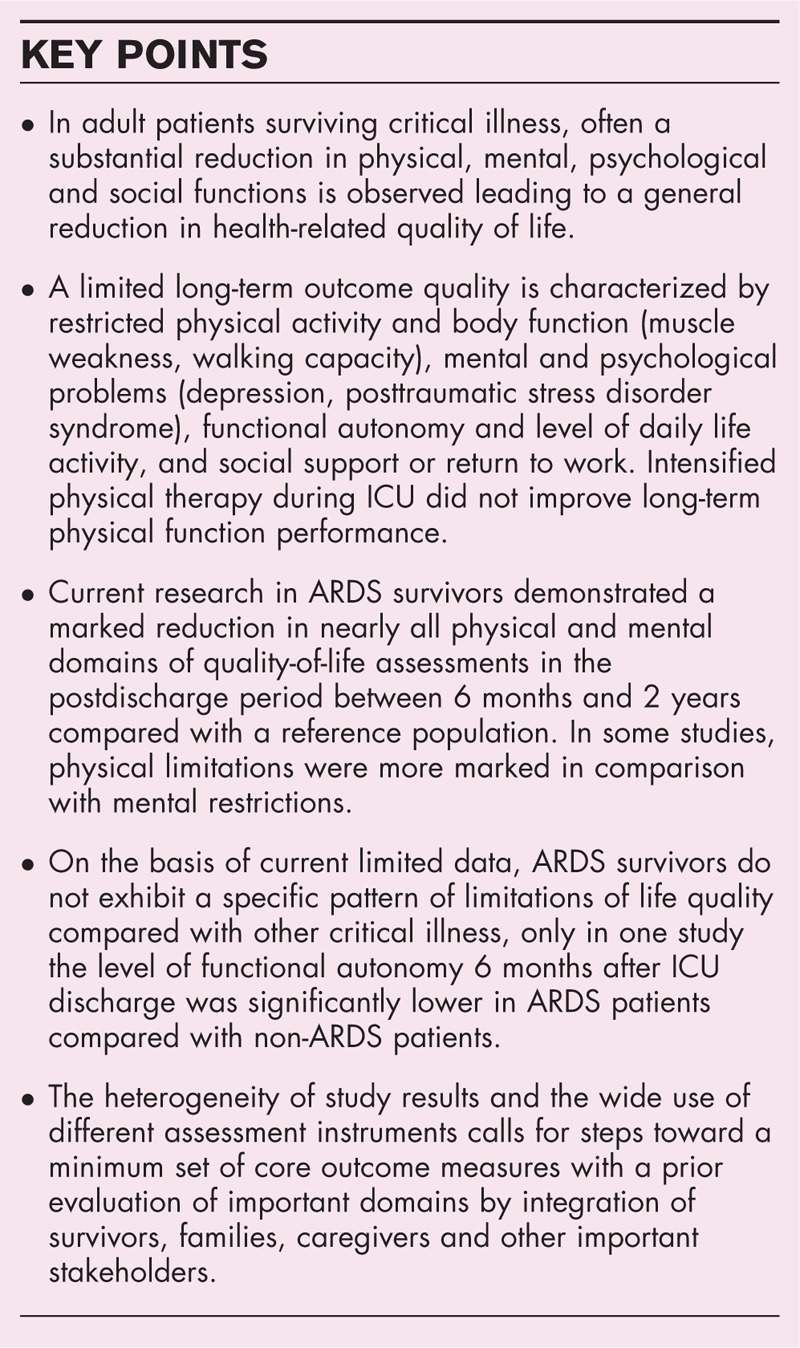
To review the current research data on long-term outcome and health-related quality of life in survivors of the acute respiratory distress syndrome (ARDS) and to compare these findings with those from non-ARDS patients surviving critical illness.
Recent findings
Between 6 months and 2 years after discharge from ICU, survivors of ARDS present with substantial impairments of the levels of body function (muscle strength, walking capacity and/or physical activity (physical SF-36 score). In contrast to non-ARDS patients from surgical ICUs, a standardized intensified physical therapy during early course of illness in ARDS patients could not show an improvement of long-term physical function performance. Furthermore, a substantial part of further ARDS patients suffer from depression (26–33%), anxiety (38–44%) or posttraumatic stress disorder (22–24%). In general, the level of functional autonomy and daily life activities was reduced, and in one study, 6 months after ICU-discharge this level was significantly lower in ARDS patients compared with non-ARDS patients. In a recent study, 44% of ARDS survivors were jobless 1 year after critical illness, whereas half of previously employed patients returned to work within 4 months after hospital discharge. General health-related quality of life was significantly reduced compared with a matched population in all studies.
Summary
Surviving ARDS is associated with a long-term substantial reduction in health-related quality of life and such a reduction does not differ from findings in patients surviving other critical illness. In further research, a special attention should be paid to prevention measures of the ‘post intensive care syndrome’ as well as to patient important domains, which might better explain the patient's and families’ demands.
Keywords: acute respiratory distress syndrome, health-related quality of life, joblessness, muscle weakness, outcome, posttraumatic stress disorder
INTRODUCTION: OUTCOME AFTER CRITICAL ILLNESS: OUTCOMES, ASSESSMENTS, AND SCIENTIFIC CONSTRUCTS
Survival of critical illness is often associated with sequelae of mental, physical, social and functional impairments after hospital discharge. In a recent review of qualitative studies on patient outcomes after critical illness [1▪], themes extracted from the studies were categorized according to PROMIS (Patient-Reported Outcomes Measurement Information System) domains. The main finding was that ICU survivors experience impairments across all PROMIS domains: global satisfaction with life (independence, acceptance, positive outlook), mental health (anxiety, depression, posttraumatic stress disorder symptoms), physical health (physical status, activities of daily life, fatigue, muscle weakness) social health and the ability to participate in social roles and activities. Active participation in social roles (friends or family relationships, hobbies, social activities) were found to be limited in patients surviving critical illness in a range of restriction qualities and quantities depending on the study patient selection. The complex and varying sequelae after critical illness have been combined to a special entity ‘post intensive care syndrome’[2], which often manifests as a combination of cognitive, psychological, and physical signs and symptoms.
In recent years the terms ‘quality of life’ (QoL) or ‘health-related quality of life’ (HrQoL) received a growing interest in intensive care research, whereas ‘historical’ outcomes for a ‘good’ survival (physical function scores, walking tests, spirometry) were put into the background. Nevertheless, ‘quality of life’ is a complex construct containing individual aspects of ‘happy to live’ as a result of multidimensional perceptions of somatic, psychological, and social variables. Numerous instruments to assess outcomes in survivors of critical illness were developed and applied over the past 40 years. In a systematic review [3], a total of 250 different instruments (questionnaires, phone or personal interviews, physical examinations, proxy interviews, chart interviews, neuro-cognitive tests) were identified. The heterogeneity in outcome measurement makes it difficult to draw meaningful and robust conclusions for clinical practice. Patient important or reported outcome assessments have been set in the focus of scientific research [4▪,5]. Such a new focus reflects a paradigm change from ‘clinically relevant’ to ‘patient important’ aspects of medicine accounting for the individual patient's values and preferences. At present, patient important outcome assessments are increasing in prospective randomized studies. Furthermore, aspects of daily living, autonomy or independence, return to work, and social participation are of increasing importance and interest for studies on long-term outcome after critical illness. In this review, relevant current research results regarding PROMIS domains in ARDS survivors are introduced and interpreted, and – if possible – compared with findings from patients surviving general non-ARDS critical illness. Aspects of (long-term) mortality are not in the focus of this review.
Box 1.
no caption available
LONG-TERM OUTCOME AFTER ACUTE RESPIRATORY DISTRESS SYNDROME
Physical status/body function
In a study by Biehl et al.[6] the 6-month functional status of ARDS survivors was examined, and it was found that the physical component score of the Short Form (SF)-12 was significantly lower compared with general population findings (P < 0.001), but these scores were comparable between ARDS patients (32.8 ± 12.3) and non-ARDS patients (37.8 ± 12.3, P = 0.11). In a study from China [7], the outcomes of ARDS survivors with extracorporeal membrane oxygenation (ECMO) were compared with those of ARDS survivors not receiving ECMO during ICU treatment. Although presenting with more severe illness, 1 year later ECMO patients were comparable in terms of physical functioning [6-min walking test (6MWT), physical SF-36] to ARDS-patients without ECMO, but the physical SF-36 score was significantly lower in both groups (72/68) compared with the general population (81.9). In the same study, pulmonary function tests were not significantly different between ECMO and non-ECMO survivors, in general presenting with a mild reduction compared with the general population. The amount and impact of post-ICU muscle weakness in 156 ARDS-survivors was investigated by Dinglas et al.[8▪]. Muscle strength was assessed with the Medical Research Council (MRC) sum score (standardized manual muscle testing), which defines a sum score less than 48 as post-ICU muscle weakness. At hospital discharge, 38% of ARDS survivors had muscle weakness. The median (IQR) MRC sum score was significantly lower for those who died during the 5-year follow-up [44 (36–52)] versus survivors [51 (46–58); P < 0.001]. Persisting long-term muscle weakness was observed in 50% of patients.
These findings are in line with reports in a general ICU population, wherever weakness and persistent reduction of motor function are found [9▪] and correlated with a sustained muscle atrophy 6 months after discharge from ICU. Interestingly, pathophysiological mechanisms which are found to be correlated with muscle atrophy during onset of critical illness [10] normalized at 6 months after ICU discharge. However, a decreased satellite cell content may indicate an impaired regenerative capacity of the atrophic muscle.
Early mobilization therapy has been mentioned in order to prevent or attenuate physical function impairment in critically ill patients [11]. However, as studies showed an improved physical function associated to protocol-based early mobilization in a surgical ICU cohort [12], this could not be proven in patients with acute respiratory failure. Two studies investigated the impact of a standardized intensified physical therapy during early course of illness in patients with acute respiratory failure with respect to physical function performance up to 6 months after discharge from ICU [13,14]. Both studies could not show an improved long-term physical function performance in this group of patients.
Mental and cognitive status
A substantial reduction in mental, cognitive and psychological functions has been noticed by various studies in survivors of critical illness. In a cross-sectional study [15] the Mini Mental State Examination (MMSE) was assessed in 242 survivors of acute respiratory failure at 6 and 12 months posthospital discharge and the results were compared with detailed neuropsychological tests (Wechsler Adult Intelligence Scale, Neurobehavioral Cognitive Status Examination). At 12 months, 13% of patients had MMSE-assessed deficits, whereas 71% had impairments based on neuropsychological tests; the correlations between MMSE results and corresponding neuropsychological tests were weak. The authors recommend to interpret MMSE scores in such a population with caution. The study by Wang et al.[7] demonstrated no differences in the mental component score of the SF-36 in ECMO-ARDS patients (79.3 ± 15.7) and the non-ECMO-ARDS patients (78.5 ± 22.5), and the results of both groups were similar to the general population scores (78.8). In the study by Biehl et al.[6] no significant differences were observed for the mental component of SF-12 between critically ill survivors with and without ARDS.
In a meta-analysis from 2015 [16], the incidence of posttraumatic stress disorders (PTSD) in a population of survivors of critical illness was found to range from 22 to 50%. In ARDS survivors, the prevalence of PTSD ranged from 22 to 24% in a 2-year follow-up setting [17▪], and additionally the prevalence of supra threshold general anxiety (range 38–44%) and depression (range 26–33%) was comparable to the corresponding prevalences in a group of critically ill patients without ARDS [18]. The incidence of psychiatric syndromes in 1-year ARDS survivors was investigated in a United States national multicenter study [19▪]. Psychiatric symptoms were evaluated by Hospital Anxiety and Depression Scale (HADS), and a total of 416 of 629 patients (66%) were identified with substantial symptoms in at least one domain. The majority of patients had symptoms in all three psychiatric domains simultaneously. Interestingly, greater severity of illness or ICU length of stay were not associated with psychiatric symptoms, but younger age, unemployment, female sex, and alcohol use were.
Daily activity and functional autonomy
The baseline functional status reflects the ability to exercise activities of daily living. A well investigated instrument to measure daily life capacity and functional autonomy is the Barthel Index. In the study by Biehl et al.[6] in ARDS survivors 6 months after ICU-discharge, the level of functional autonomy – assessed by Barthel Index – was significantly lower in ARDS patients (82.3 ± 22.9) compared with non-ARDS-patients (89.6 ± 23.2, P = 0.007). Chan et al.[20] investigated possible associations of body functions and structures (spirometry, manual muscle training, hand grip strengths), physical measures (6MWT), and participation in daily life (Index of Activities of Daily Living; IADL) 6 months after surviving ARDS with later (1 year) HrQoL assessments, and they found that the level of activities of daily life more closely reflected the patient's QoL than measures of body functions and structures.
Social support, return to work
The amount of social support and/or the feeling of being ‘socially healthy’ (changes in friends or family relationships, enjoying being with people, not feeling like a burden, ability to participate in social roles) is an important aspect of quality of life, but studies investigating social health after critical illness are rare [1▪]. In ARDS patients, no study on aspects of social health was published in recent years.
The possibility and timing of return to work is an important indicator for quality of life. Myhren et al.[21] assessed the rate of patients surviving critical illness, who returned to work. Among patients who were in work or school pre-ARDS, 55% had returned to work or school at 1-year follow up. In a recent analysis [22▪], the factors associated with return to work and the amount of lost earnings were investigated in 922 ARDS survivors from 43 United States ARDSNet hospitals over a 12-month longitudinal post-ICU period. In total, 44% of these survivors were jobless 1 year after critical illness, whereas half of previously employed patients returned to work within 4 months after hospital discharge. Lost earnings were complained by 71% of all ARDS survivors. The most important variables associated with post-ARDS joblessness were hospital length of stay and age.
Health-related quality of life
In a large secondary analysis of a prospective randomized study on the effects of high-frequency oscillatory ventilation in ARDS-patients (OSCAR-trial), HrQoL was assessed in 795 patients 1-year post-ICU [23▪]. Survivors of ARDS reported significant lower HrQoL than the age-matched and sex-matched reference population. This finding was more marked in younger patients less than 65 years (Table 1). In a small prospective study from China [7], the HrQoL of ARDS survivors treated with ECMO (n = 24) was compared with those ARDS patients without ECMO (n = 48), and the main finding was that ECMO and non-ECMO survivors had a similar quality of life assessed by EuroQol questionnaire 1-year postdischarge, but compared with the general population, both groups showed significant lower values. Bienvenu et al.[17▪] investigated several outcomes (depression, anxiety, posttraumatic stress disorder, HrQoL) after acute lung injury in a 2-year longitudinal study. In 95% of patients, they found at least one psychopathological symptom, and the physical domain of SF-36 was reduced. In a multivariate analysis, better physical functioning during recovery was associated with a better subsequent remission of psychiatric symptoms. In the study by Biehl et al.[6] 6 months HrQoL and functional status of ARDS survivors were compared with patients at risk who did not suffer from ARDS. Both groups had significantly (P < 0.001) lower values of SF-12 compared with general US population, but in ARDS and non-ARDS patients no 6-month postdischarge differences in SF-12 results were observed. Accordingly, in the study from Myhren et al.[21] compared with sex-adjusted and age-adjusted data from the general Norwegian population in survivors of critical illness, significant lower values were assessed 1 year after discharge among all components of physical and mental health (SF-36).
Table 1.
Important recent studies on health-related quality of life after surviving acute respiratory distress syndrome
| Reference/cohort profile | Assessment post ICU | Number of patients | SF-12, bSF-36 physical | SF-12, bSF-36 mental | EQ-5D | Significant findings |
| Bienvenu et al. [17▪]ARDS survivors | Two years | 186 | 39 ± 13 | Majority had significant anxiety, depression, PTSD. Better physical functioning during recovery was associated with better remission of psychiatric symptoms | ||
| Marti et al. [23▪]ARDS patients less than 65 yearsARDS patients at least 65 years matched referenceLess than 65 yearsAt least 65 years | One yearOne year | 795 | 0.58 ± 0.38a0.58 ± 0.38a0.85 ± 0.060.77 ± 0.20 | High postdischarge costs and relatively HrQoL life in ARDS survivors. The difference of low HrQoL compared with reference population values was more marked in younger patients | ||
| Brown et al. [24]ARDS | Six months | 616 | Median 0.77IQR 0.51–0.83 | Pre-illness functional independence and life style factors (obesity, tobacco) were associated with worse HrQoL, but not severity of acute illness. | ||
| Biehl et al. [6]ARDSNon-ARDS | Six months Six months | 2641 | 32.8 ± 12.337.8 ± 12.3 | 49.7 ± 12.251.3 ± 10.7 | ARDS patients had poorer baseline functional status compared with non-ARDS patients. Decreased HrQoL and functional status were explained by baseline condition with similar recovery in ARDS and non-ARDS | |
| Myhren et al. [21]Critical illness versus matched reference | One year | 194 | Lower in all physical scores (P < 0.05) | lower in all mental scores (P < 0.05) | Less posttraumatic stress and optimism were predictors of higher HrQoL and return to work. Half of patients had returned to work | |
| Wang et al. [7] bARDS-ECMOARDS non-ECMOMatched reference | One yearOne year | 2448 | 72.0 ± 20.668.0 ± 22.681.9 | 79.3 15.778.5 22.578.8 | EQ5D-VAS81.5 ± 12.079.1 ± 15.0 | ARDS patients showed reduced HrQoL compared with the general population. Comparable outcomes between ECMO and non-ECMO patients |
SF-12/36, Short Form-12/36, EQ-5D, EuroQual-Questionnaire, VAS, Visual Analog Scale.
aSignificance P < 0.05.
bQuestionnaire SF-36 (instead SF-12).
CONCLUSION
The cause, pathophysiologic manifestation, and clinical course in ARDS patients might be different from those entities of other critical diseases, although a major intersection may exist (sepsis, oncologic comorbidity, trauma). The hypothesis of a different and characteristic pattern of long-term outcome sequelae after surviving ARDS might be derived from specific aspects of ARDS:
ARDS is characterized by ‘vulnerable’ lung parenchyma, and mechanical ventilation might be more injurious than in other critical illness.
Hypoxemia is a specific complication in ARDS, and surviving patients might be specifically exposed to negative effects.
ARDS patients receive more ‘sophisticated’ therapy (ECMO, prone position, muscle relaxation, sedation) which might influence long-term outcome.
On the other hand, ARDS is an heterogeneous bundle of symptoms, and ARDS is not seen as a disease with a univocal and straightforward trajectory of treatment and recovery [25]. ARDS rather remains a syndrome composed of a multifaceted means of diagnoses, and determined by different causes with as many different clinical manifestations. Furthermore, in clinical practice ARDS remains underrecognized by clinicians. All these arguments might explain the findings from the above-mentioned studies that ARDS survivors do not present with further (or other) long-term outcome of physical or psychological sequelae. Only in one study [6], a trend towards lower SF-36 scores and a lower Barthel Index were found in ARDS patients compared with survivors of other critical illnesses.
The heterogeneity of study results and the wide use of different assessment instruments for investigation of HrQoL in survivors of ARDS calls for an initial step towards a minimum set of core outcome measures with a prior evaluation of important domains by means of an integration of survivors, families, caregivers and other important stakeholders [26,27▪,28,29].
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1▪.Hashem MD, Nallagangula A, Nalamalapu S, et al. Patient outcomes after critical illness: a systematic review of qualitative studies following hospital discharge. Crit Care 2016; 20:345. [DOI] [PMC free article] [PubMed] [Google Scholar]; A comprehensive and careful systematic review of the wide range of mental, physical, and social sequelae after critical illness, underlining the necessity of ‘core’ outcome variables.
- 2.Rawal G, Yadav S, Kumar R. Postintensive care syndrome: an overview. J Transl Int Med 2017; 5:90–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Turnbull AE, Rabiee A, Davis WE, et al. Outcome measurement in ICU survivorship research from 1970 to 2013: a scoping review of 425 Publications. Crit Care Med 2016; 44:1267–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4▪.Shah HA, Dritsaki M, Pink J, et al. Psychometric properties of patient reported outcome measures (PROMs) in patients diagnosed with acute respiratory distress syndrome (ARDS). Health Qual Life Outcomes 2016; 14:15. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study reports on patient reported outcome measures and weights the importance and differences of PROM's versus ‘traditional’ outcome parameters.
- 5.Gaudry S, Messika J, Ricard JD, et al. Patient-important outcomes in randomized controlled trials in critically ill patients: a systematic review. Ann Intensive Care 2017; 7:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Biehl M, Kashyap R, Ahmed AH, et al. Six-month quality-of-life and functional status of acute respiratory distress syndrome survivors compared with patients at risk: a population-based study. Crit Care 2015; 19:356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang ZY, Li T, Wang CT, et al. Assessment of 1-year outcomes in survivors of severe acute respiratory distress syndrome receiving extracorporeal membrane oxygenation or mechanical ventilation: a prospective observational study. Chin Med J (Engl) 2017; 130:1161–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8▪.Dinglas VD, Aronson Friedman L, Colantuoni E, et al. Muscle weakness and 5-year survival in acute respiratory distress syndrome survivors. Crit Care Med 2017; 45:446–453. [DOI] [PMC free article] [PubMed] [Google Scholar]; Important study evaluating the association of post-ICU weakness and associated trajectories of weakness over 5-years follow-up.
- 9▪.Dos Santos C, Hussain SN, Mathur S, et al. MEND ICU Group, RECOVER Program Investigators, Canadian Critical Care Translational Biology Group. Mechanisms of chronic muscle wasting and dysfunction after an intensive care unit stay. A pilot study. Am J Respir Crit Care Med 2016; 194:821–830. [DOI] [PubMed] [Google Scholar]; Investigation on the mechanisms of muscle weakness using sophisticated instruments (electromyography, nerve stimulation, muscle biopsy) with histologic, cellular and molecular analyses opening insights in the pathophysiology of ICU-aquired muscle weakness.
- 10.Zhu X, Kny M, Schmidt F, et al. Secreted frizzled-related protein 2 and inflammation-induced skeletal muscle atrophy. Crit Care Med 2017; 45:e169–e183. [DOI] [PubMed] [Google Scholar]
- 11.Bein T, Bischoff M, Brückner U, et al. S2e guideline: positioning and early mobilisation in prophylaxis or therapy of pulmonary disorders: revision 2015: S2e guideline of the German Society of Anaesthesiology and Intensive Care Medicine (DGAI). Anaesthesist 2015; 64 (Suppl 1):1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schaller SJ, Anstey M, Blobner M, et al. International Early SOMS-guided Mobilization Research Initiat. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet 2016; 388:1377–1388. [DOI] [PubMed] [Google Scholar]
- 13.Moss M, Nordon-Craft A, Malone D, et al. Randomized trial of an intensive physical therapy program for patients with acute respiratory failure. Am J Respir Crit Care Med 2016; 193:1101–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morris PE, Berry MJ, Files DC, et al. Standardized rehabilitation and hospital Length of stay among patients with acute respiratory failure: a randomized clinical trial. JAMA 2016; 315:2694–2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pfoh ER, Chan KS, Dinglas VD, et al. NIH NHLBI ARDS Network. Cognitive screening among acute respiratory failure survivors: a cross-sectional evaluation of the Mini-Mental State Examination. Crit Care 2015; 19:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parker AM, Sricharoenchai T, Raparla S, et al. Posttraumatic stress disorder in critical illness survivors: a metaanalysis. Crit Care Med 2015; 43:1121–1129. [DOI] [PubMed] [Google Scholar]
- 17▪.Bienvenu OJ, Colantuoni E, Pedro A, et al. Co-occurrence of and remission from general anxiety, depression, and posttraumatic stress disorder symptoms after acute lung injury: a 2-year longitudinal study. Crit Care Med 2015; 43:642–653. [DOI] [PMC free article] [PubMed] [Google Scholar]; Extensive and prolonged study on psychiatric symptoms in surviving ARDS patients on a large data base.
- 18.Rattray J. Life after critical illness: an overview. J Clin Nurs 2014; 23:623–633. [DOI] [PubMed] [Google Scholar]
- 19▪.Huang M, Parker AM, Bienvenu OJ, et al. National Institutes of Health, National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Network. Psychiatric symptoms in acute respiratory distress syndrome survivors: A 1-year national multicenter study. Crit Care Med 2016; 44:954–965. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study illustrates the co-occurrence regarding socioeconomic variable and ‘life-style’ patterns on the incidence of psychiatric symptoms.
- 20.Chan KS, Aronson Friedman L, Dinglas VD, et al. Are physical measures related to patient-centred outcomes in ARDS survivors? Thorax 2017; 72:884–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myhren H, Ekeberg Ø, Stokland O. Health-related quality of life and return to work after critical illness in general intensive care unit patients: a 1-year follow-up study. Crit Care Med 2010; 38:1554–1561. [DOI] [PubMed] [Google Scholar]
- 22▪.Kamdar BB, Huang M, Dinglas VD, et al. National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Network. Joblessness and lost earnings after acute respiratory distress syndrome in a 1-year national multicenter study. Am J Respir Crit Care Med 2017; 196:1012–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]; Study on joblessness and earning loss after surviving ARDS showing the general healthcare dimension of this patient group.
- 23▪.Marti J, Hall P, Hamilton P, et al. One-year resource utilisation, costs and quality of life in patients with acute respiratory distress syndrome (ARDS): secondary analysis of a randomised controlled trial. J Intensive Care 2016; 4:56. [DOI] [PMC free article] [PubMed] [Google Scholar]; The focus on 1-year resource utilization of ARDS survivors combined with HrQoL parameters gives important insights. A multivariable analysis weights the findings.
- 24.Brown S, Emily Wilson E, Presson AP, et al. with the National Institutes of Health NHLBI ARDS Network. Predictors of 6-month health utility outcomes in survivors of acute respiratory distress syndrome. Thorax 2017; 72:311–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rezoagli E, Fumagalli R, Bellani G. Definition and epidemiology of acute respiratory distress syndrome. Ann Transl Med 2017; 5:282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dodoo-Schittko F, Brandstetter S, Blecha S, et al. Determinants of quality of life and return to work following acute respiratory distress syndrome. Dtsch Arztebl Int 2017; 114:103–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27▪.Dinglas VD, Chessare CM, Davis WE, et al. Perspectives of survivors, families and researchers on key outcomes for research in acute respiratory failure. Thorax 2017; doi: 10.1136/thoraxjnl-2017-210234. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]; The aspects of sequelae and attitudes of families and caregivers is addressed in this study, stimulating for further research.
- 28.Iwashyna TJ, Walsh TS. Interplay of physiology, social, familial and behavioural adaptation in the long-term outcome of ARDS. Thorax 2017; 72:872–873. [DOI] [PubMed] [Google Scholar]
- 29.Herridge MS, Moss M, Hough CL, et al. Recovery and outcomes after the acute respiratory distress syndrome (ARDS) in patients and their family caregivers. Intensive Care Med 2016; 42:725–738. [DOI] [PubMed] [Google Scholar]


