Abstract
PURPOSE:
The purpose of this study was to measure the prevalence of incontinence-associated dermatitis (IAD) among incontinent persons in the acute care setting, characteristics of IAD in this group, and associations among IAD, urinary, fecal, and dual incontinence, immobility, and pressure injury in the sacral area.
DESIGN:
Descriptive and correlational analysis of data from a large database of IAD, and pressure injuries of sacral area and heels.
SUBJECTS AND SETTING:
The sample comprised 5342 adult patients in acute care facilities in 36 states representing all regions of the United States. Facilities used a variety of products for prevention of IAD and sacral area pressure injuries.
METHODS:
Data were collected for use in a national quality improvement study evaluating current practices related to the prevention of IAD and pressure injuries affecting the sacral area and heels. Data were exported to a spreadsheet, and triple checked for accuracy before being imported to a statistical analysis software program. Descriptive statistics were used to describe prevalence rates for incontinence, types of incontinence, IAD, characteristics of IAD, and pressure injuries. Multivariate logistic regression analysis was conducted on the end point of facility-acquired sacral/buttock pressure injury and the risk factors of immobility and type of incontinence.
RESULTS:
More than one-third of patients (n = 2492 of 5342 patients; 46.6%) were incontinent of urine, stool, or both. The overall prevalence rate of IAD was 21.3% (1140/5342); the prevalence of IAD among patients with incontinence was 45.7% (1140/2492). Slightly more than half of the IAD was categorized as mild (596/1140, 52.3%), 27.9% (318/1140) was categorized as moderate, and 9.2% (105/1140) was deemed severe. In addition, 14.8% (169/1140) of patients with IAD also had a fungal rash. The prevalence of pressure injury in the sacral area among individuals with incontinence was 17.1% (427/2492), and the prevalence of full-thickness pressure injury in this population was 3.8% (95/2492). Multivariate analysis revealed that both presence of IAD (odds ratio [OR], 4.56; 95% confidence interval [CI], 3.68-5.65) and immobility (OR, 3.56; 95% CI, 2.73-4.63) was associated with a significantly increased likelihood of developing a sacral pressure injury. Multivariate analysis also revealed that presence of IAD (OR, 2.65; 95% CI, 1.74-4.03) and immobility (OR, 6.05; 95% CI, 3.14-11.64) was associated with a significantly increased likelihood of developing full-thickness sacral pressure injury.
CONCLUSION:
Our study findings are consistent with prior research, supporting a clinically relevant association between IAD and pressure injury of the sacral area. This risk persists even after controlling for presence of immobility, suggesting that IAD functions as an independent risk factor for pressure injury occurrence.
Keywords: Acute care, Incidence, Incontinence, Incontinence-associated dermatitis, Pressure injury, Prevalence
INTRODUCTION
Incontinence-associated dermatitis (IAD) is characterized by erythema and edema of the surface of the skin, sometimes accompanied by serous exudate, erosion, or secondary cutaneous infection.1,2 It is also classified as a form of moisture-associated skin damage that occurs when the skin is exposed to urinary, fecal, or dual urinary and fecal incontinence.3 Despite a growing body of research, there is a need for additional empiric data current regarding the epidemiology of IAD in various health care settings. The largest studies to date focusing on IAD prevalence and incidence have been in the long-term care setting. Bliss and colleagues4 analyzed data from the Minimum Data Set (MDS) and reported a 5.7% prevalence of IAD in nursing home residents. More recently, Bliss and colleagues5 combined data from 2 electronic databases, the MDS and Practitioners Orders, and reported a 5.5% incidence of IAD in a group of 10,713 nursing home residents newly diagnosed with incontinence and without IAD. In both studies, researchers used indirect indicators for IAD because the MDS and Practitioners databases do not specifically query data regarding this prevalent and clinically relevant form of skin damage. Boronat-Garrido and colleagues6 evaluated 3406 German nursing home residents with urinary, fecal, or dual incontinence and reported an IAD point prevalence of 5.2%.
Evidence concerning the prevalence of IAD in the acute care setting is especially sparse. Junkin and Selekof7 investigated IAD prevalence in 2 studies enrolling 976 and 608 acute care patients in a community-based and teaching hospital in the United States, respectively. The prevalence of IAD in these studies was 27% in the original study that enrolled 976 acutely ill adults and 20% in the second study that enrolled 608 subjects. The second study was performed after introduction of a premoistened cloth for prevention and treatment of IAD. Campbell and colleagues8 assessed IAD prevalence in a group of 376 patients at a teaching hospital in Brisbane, Australia. They reported a 42% prevalence of IAD among incontinent patients. Two studies were identified that reported IAD occurrences in the acute care setting, but both studies were conducted in single intensive care units and neither reported facility-wide IAD prevalence.9,10
Our literature review identified 2 additional studies that evaluated IAD occurrence in settings other than acute or long-term care facilities. Long and colleagues11 reported a 22.8% point prevalence of IAD and a 7.6% incidence rate based on direct observation of 171 patients cared for in a single long-term acute care unit in the United States. Rohwer and colleagues12 evaluated IAD occurrence in community-dwelling individuals with fecal or dual fecal and urinary incontinence as part of a comparative trial evaluating the effect of dietary fiber on fecal incontinence. More than half (52.5%) of 189 subjects reported recurring episodes of typically mild-to-moderate IAD. Relatively small sample sizes in all but the long-term care settings, as well as differences in methods used to identify IAD, may have produced the wide variability of reported prevalence rates in these studies. In contrast, prevalence rates in the larger studies in the long-term care setting revealed considerably less variability (5.2%-5.7%), possibly reflecting the power of larger, multisite studies when reporting epidemiology of a condition such as IAD.4,5
Houwing and colleagues13 analyzed 14 tissue biopsies from patients with lesions deemed to be pressure injuries and moisture lesions (now referred to as IAD) and found histopathologic evidence of distinctive etiologies for these lesions, with biopsies from pressure injuries revealing evidence of ischemia and biopsies from IAD revealing inflammation. Nevertheless, multiple studies have demonstrated a statistically significant association between incontinence, IAD occurrence, and risk of pressure injury.14–18 Demarré and colleagues14,15 conducted a secondary analysis of a randomized clinical trial that enrolled 610 patients and compared the effect of 2 pressure‑redistributing support surfaces on pressure injury prevention. They found that IAD was significantly associated with development of partial-thickness pressure injuries (odds ratio [OR], 2.99; 95% confidence interval [CI], 1.2-7.5; P = .001). Beeckman and colleagues16 pooled data from 58 studies and found a statistically significant correlation in univariate models between urinary incontinence and any pressure injury (OR, 1.92; 95% CI, 1.54-2.38) and dual incontinence and pressure injury (OR, 4.99; 95% CI, 2.62-9.5; P < .05). Their meta-analysis was consistent with the findings of Demarré's group, and it identified a statistically significant relationship between IAD and full-thickness pressure injuries. Lachenbruch and coworkers17 analyzed observations of 176,689 patients cared for in acute care facilities from 2013 to 2014. They found that more than half of these patients (53%; n = 92,889) were incontinent. Similar to prior studies with smaller sample sizes, they found that urinary, fecal, and dual incontinence increased the likelihood of developing partial- or full-thickness pressure injuries. This association persisted for all pressure injuries (4.1% of continent patients vs 6.3% of incontinent patients) and in patients with facility-acquired pressure injuries (1.6% vs 6%, respectively).
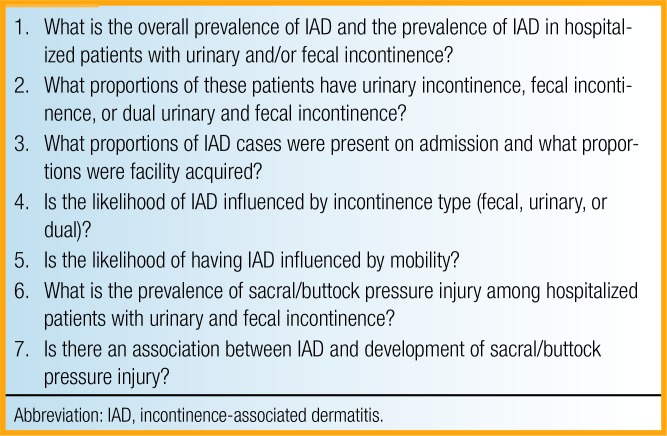
The purpose of this study was to measure the prevalence of IAD among incontinence persons in the acute care setting, characteristics of IAD in this group, and associations among IAD, urinary incontinence, fecal incontinence, dual incontinence, immobility, and pressure injury in the sacral area. Study aims were to (1) measure the prevalence of IAD in the acute care setting including facility-acquired IAD versus IAD present on admission; (2) describe the clinical characteristics of IAD; (3) analyze the relationship among IAD, urinary incontinence, fecal incontinence, dual incontinence, and immobility; and (4) evaluate the relationship between IAD and facility-acquired pressure injury in the sacral area. Box 1 lists the 7 research questions addressed in this study.
BOX 1.
Research Questions
METHODS
We performed descriptive and correlation analysis of data from a large database used to guide quality improvement related to prevention of IAD and pressure injury in the sacral area. The IAD prevalence database is maintained by Sage Products (Cary, Illinois) to provide information about IAD and pressure injuries of the heel and sacral areas. Data were collected exclusively by frontline and wound care specialty practice nurses employed by each of the participating facilities. Facilities used a variety of products to prevent IAD and pressure injuries of the sacral area. The clinical units in each hospital were selected by the wound care nurses as high risk for pressure injury and included both critical care and general adult patient care units. No identifying patient information was recorded. Study procedures were reviewed and approved by the Schulman Institutional Review Board, a national institutional review board (Cincinnati, Ohio).
Instrument
A data collection form was developed by a group of clinical consultants for use in a national quality project evaluating current practices related to the prevention of IAD and pressure injuries affecting the sacral area. The form queried the number of patients in each unit where data were collected, the number of patients deemed immobile (unable to move without assistance), the number of patients who were incontinent, and the type of incontinence (urinary, fecal, or dual). The form also queried the number of patients with IAD, whether IAD was present on admission or had developed during the patient's hospital course, the severity of IAD (ranked as mild, moderate, or severe), and presence of fungal rash. No specific instrument was used to judge IAD severity, mild IAD was characterized by erythema of the skin, and moderate-to-severe IAD was characterized by erosion of the skin with or without fungal rash. The form also included items regarding the presence of pressure injuries in the sacral area (including the buttocks), pressure injury stage, and whether the pressure injury was present on admission or developed during the hospital stay. No protected health information data were collected, and all data were aggregated into reports to facilitate both IAD and pressure injury prevention and stimulate quality improvement efforts among participating facilities. It should be noted that survey fields were not mandatory; therefore, some data were not completed for all patients. Nurses did not receive specific training before completing the form.
Data were exported to a spreadsheet and triple checked for accuracy before being imported to the statistical analysis software program. All data will remain stored on a password‑protected server in a confidential and secure location for 10 years.
Study Procedures
Participating facilities were provided with unit-based data collection forms in a paper or digital form, depending on local preference. Each facility then performed the survey on a single day. Data collectors also provided information regarding the participating facility including the number of beds, date of data collection, and type of unit. Data were collected between January 2011 and June 2014.
Data Analysis
Statistical analyses were conducted using SAS software (SAS 9.4; SAS Institute Inc, Cary, North Carolina). Descriptive statistics were analyzed using frequency and percentage of the cohort. Missing data values are noted in the tables. As a point-prevalence study, rates were calculated as number of patients with present on admission, facility-acquired IAD, and facility-acquired pressure injuries (numerator) divided by the total number of patients observed during the 1 day of data collection (denominator). Any discrepancies in numerators and denominators on more advanced analyses are attributed to missing data. Logistic regression analysis was conducted using the outcome variable facility-acquired sacral/buttock pressure injury and the risk factors of immobility and type of incontinence. Potential risk factors, IAD, immobility, and type of incontinence were assessed for multicollinearity. In the presence of multicollinearity, the one found to be more related to the end point was used in the modeling process to ensure independence. Factors with univariate P values ≤ .1 were then considered in the full model. Backward elimination methods were used to complete the final multivariable model, removing the least significant factor, rerunning, and repeating until only statistically significant factors with at least 1 significant category comparison remained in the model with P values ≤ .05. In the final modeling, multiple models were run to allow for presentation of all comparisons, via indicator variables, of multilevel factors such as type of incontinence.
RESULTS
One hundred eighty-nine hospitals, representing 36 states located in all 4 geographic regions of the United States (Northeast, Midwest, South, and West), participated in the study. These facilities used a variety of products and interventions for prevention of IAD and pressure injuries of sacral injuries. Data were collected for 5342 adult patients. Almost half (n = 2492/5342; 46.6%) of the patients had urinary, fecal, or dual incontinence. The prevalence of IAD among persons with any type of incontinence was 45.7% (1140/2492). Incontinence-associated dermatitis was present on admission in 25.1% (286/1140) of patients; 73% (832/1140) acquired IAD during the hospital course. The clinical characteristics of IAD were documented and found 52.3% (596/1140) were mild, 27.9% (318/1140) were moderate, and 9.2% (105/1140) were severe, with 14.8% (169/1140) also having a fungal rash. The prevalence of facility-acquired pressure injury in the sacral area among individuals with incontinence was 17.1% (427/2492), and the prevalence of facility-acquired full-thickness pressure injury was 3.8% (95/2492).
IAD and Incontinence Type
Patients with fecal incontinence alone were significantly more likely to experience IAD than those with urinary incontinence alone (44.7% vs 29.7%; χ2= 18.5; P < .001). Similarly, patients with dual incontinence were more likely to experience IAD than were those with urinary incontinence (49.2% vs 29.7%; χ2= 38.4; P < .001). Mobility also influenced the likelihood of IAD; patients who were immobile were significantly more likely to experience IAD than were mobile patients (39.9% vs 7.4%; χ2= 755.3; P < .001). Patients with IAD were also more likely to experience a facility-acquired pressure injury of the sacral area compared to those without IAD (32.3% vs. 6.3%; χ2= 436.4; P < .001). Patients with IAD were also more likely to experience a facility-acquired full-thickness sacral pressure injury compared to those without IAD (6.4% vs 1.5%; χ2= 66.7; P < .001).
IAD and Pressure Injury
We examined patients who experienced facility-acquired sacral pressure injury (7.5%, 300/3693) to evaluate associations with type of incontinence and immobility (Table 1). Both immobility and type of incontinence were significantly related to sacral facility-acquired pressure injury. Patients who were immobile were almost 3.5 times more likely to develop facility-acquired sacral pressure injury than those who were mobile (12.1% vs 3.2%; OR, 3.304, 95% CI, 2.377-4.593; P < .0001). Multivariate analysis also revealed that patients with dual incontinence were more likely to develop facility‑acquired sacral pressure injury compared with those with urinary incontinence, fecal incontinence, or no incontinence (OR, 1.626; 95% CI, 1.187-2.226, P = .002). Even after adjusting for immobility, the association between IAD and prevalence of facility-acquired pressure injury in the sacral area remained statistically significant (Table 2).
TABLE 1. Multivariate Logistic Regression Model of Risk Factors for Pressure Injury.
| Comparison | χ2 Test Statistic | P Value | OR (95% CI) | ||
|---|---|---|---|---|---|
| Immobile vs not immobile | 50.6 | <.0001 | 3.304 (2.377-4.593) | ||
| Urine vs none | 0.01 | .9999 | – | – | |
| Fecal vs none | 1.8 | .1843 | – | – | |
| Dual vs none | 9.2 | .0020 | 1.626 (1.187-2.226) | ||
| Fecal vs urine | 0.8 | .3633 | – | – | |
| Dual vs urine | 3.4 | .0659 | – | – | |
| Dual vs fecal | 1.7 | .1953 | – | – |
Abbreviations: CI, confidence interval; OR, odds ratio.
TABLE 2. Multivariable Logistic Regression Model and Sacral/Buttock Pressure Injury.
| Factor | χ2 Test Statistic | P Value | OR (95% CI) |
|---|---|---|---|
| IAD | 833.1 | <.001 | 4.56 (3.68-5.65) |
| Immobility | 191.5 | <.001 | 3.56 (2.73-4.63) |
Abbreviations: CI, confidence interval; IAD, incontinence-associated dermatitis; OR, odds ratio.
Because of challenges associated with differential identification of IAD and partial-thickness (stage 2) pressure injuries, we analyzed the relationships among IAD, immobility, and facility-acquired full-thickness pressure injuries. Both IAD and immobility were statistically significant factors related to prevalence of full‑thickness pressure injury in the sacral area. After adjusting for immobility, IAD remained statistically significant (Table 3).
TABLE 3. Multivariable Logistic Regression Model and Full-Thickness Sacral/Buttock Pressure Injury.
| Factor | χ2 Test Statistic | P Value | OR (95% CI) |
|---|---|---|---|
| IAD | 20.8 | <.001 | 2.65 (1.74-4.03) |
| Immobility | 28.9 | <.001 | 6.05 (3.14-11.64) |
Abbreviations: CI, confidence interval; IAD, incontinence-associated dermatitis; OR, odds ratio.
DISCUSSION
We examined the prevalence and clinical characteristics of IAD and its relationship to sacral pressure injuries in 5342 patients in 189 acute care facilities in 36 US states. The overall prevalence was 21.3%, and IAD occurred in 45.7% of patients who were incontinent of stool or urine. The overall prevalence of IAD is similar to Junkin and Selekof,7 who reported prevalence rates of 27% and 20% in 2 studies of hospitalized patients. The differences in their studies may be attributable to institution of a structured skin care program that included use of a premoistened cloth with cleanser, emollient-based moisturizer, and dimethicone-based skin protectant in the second study that reported the lower (20%) prevalence of IAD. Our prevalence rate of IAD among patients with incontinence is also similar to Campbell and colleagues,8 who assessed 376 patients in a single acute care facility in Queensland and reported a 42% prevalence of IAD among patients with incontinence.
Incontinence-associated dermatitis occurred in patients with urinary, fecal, and dual incontinence; nevertheless, patients with fecal or dual incontinence were significantly more likely to experience IAD than were patients with urinary incontinence alone (P < .001). Our findings are similar to prior studies in multiple health care settings that found that individuals with fecal incontinence were more likely to experience IAD than those with urinary incontinence alone.16–18 Nevertheless, we found that 29.7% of patients with IAD had urinary incontinence alone. This observation reinforces the findings of Gray,19 who reported a 23.7% prevalence rate for IAD among 260 patients treated at an outpatient urology service.
The vast majority of IAD (73%) developed following hospital admission. We believe this is the first study to distinguish IAD occurrences present on admission from facility-acquired cases. Additional research is needed to more clearly understand the factors that account for IAD occurrences following hospital admission.
We evaluated relationships between IAD and pressure injury using both univariate and multivariable analyses. Univariate analyses revealed relationships among IAD, immobility, and sacral pressure injury. Multivariate logistic regression analysis found that whereas all 3 conditions were related, IAD acts an independent risk factor for sacral pressure injury, and IAD acted as a risk factor for development of facility-acquired partial- and full-thickness ulcers. Our findings are consistent with those of others who have found that IAD is associated with an increased risk of pressure injury.16–18 However, our results build on these studies by evaluating the relationship between patients with incontinence and IAD rather than incontinence alone to determine the nature of the relationship between all pressure injuries and full-thickness pressure injuries. Additional research is needed to more clearly understand the relationship between IAD and pressure injury, including the relative timing of IAD and pressure injury occurrences. Research using an in vivo model is also needed to understand the relationship between IAD and full-thickness pressure injury in particular.
Strengths and Limitations
We believe ours is the largest study published measuring IAD prevalence in the acute care setting. We analyzed findings from more than 5000 adult patients at 36 facilities located throughout the United States. Our study also builds on prior research evaluating the relationship between IAD and pressure injury. Limitations of this secondary database analysis include missing data from the electronic surveys. Since completion of survey fields were not mandatory, some fields were left blank, which may have influenced calculations of IAD prevalence. In addition, participants did not receive standardized training in assessment of IAD and pressure injury and they did not measure IAD severity using a validated instrument, which may have influenced categorization of severity and stage of these lesions. Data were acquired from a wide variety of facilities of varying sizes and community settings. These facilities used a variety of interventions and products to achieve these goals, and this variability may have influenced findings.
CONCLUSION
We analyzed data in 5342 adults cared for in acute care facilities across the United States and found an overall IAD prevalence rate of 21.3% and a rate of 45.7% among patients with urinary, fecal, or dual incontinence. We also found a significant association between IAD and facility-acquired pressure injury of the sacral area. This risk persists even after controlling for presence of immobility, suggesting that IAD functions as an independent risk factor for pressure injury occurrence.
Footnotes
Dr Giuliano is an employee of Sage Products, LLC, Cary, Illinois.
Dr. Gray is a clinical consultant for Sage Products, LLC, Cary, Illinois.
REFERENCES
- 1.Gray M, Beeckman D, Bliss DZ, et al. Incontinence associated dermatitis: a comprehensive review and update. J Wound Ostomy Continence Nurs. 2012;39(1):61–74. [DOI] [PubMed] [Google Scholar]
- 2.Beeckman D, van Damme N, Schoonhoven L, et al. Interventions for preventing and treating incontinence associated dermatitis in adults. Cochrane Database Syst Rev. 2016;11:CD011627. 10.1002/14651858.CD011627.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gray M, Black JM, Baharestani MM, et al. Moisture-associated skin damage: overview and pathophysiology. J Wound Ostomy Continence Nurs. 2011;38(3):233–241. [DOI] [PubMed] [Google Scholar]
- 4.Bliss DZ, Zehrer C, Savik K, Thayer D, Smith G. Incontinence-associated skin damage in nursing home residents: a secondary analysis of a prospective, multicenter study. Ostomy Wound Manage. 2006;52(12):46–55. [PubMed] [Google Scholar]
- 5.Bliss DZ, Mathiason MA, Gurvich O, et al. Incidence and predictors of incontinence associated skin damage in nursing home residents with new onset incontinence. J Wound Ostomy Continence Nurs. 2017;44(2):165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boronat-Garrido X, Kottner J, Schmitz G, Lahmann N. Incontinence-associated dermatitis in nursing homes: prevalence, severity, and risk factors in residents with urinary and/or fecal incontinence. J Wound Ostomy Continence Nurs. 2016;43(6):630–635. [DOI] [PubMed] [Google Scholar]
- 7.Junkin J, Selekof JL. Prevalence of incontinence and associated skin injury in the acute care inpatient. J Wound Ostomy Continence Nurs. 2007;34(3):260–269. [DOI] [PubMed] [Google Scholar]
- 8.Campbell JL, Coyer FM, Osborne SR. Incontinence-associated dermatitis: a cross-sectional prevalence study in the Australian acute care hospital setting. Int Wound J. 2016;13(3):403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bliss DZ, Savik K, Thorson MA, et al. Incontinence-associated dermatitis in critically ill adults: time to development, severity, and risk factors. J Wound Ostomy Continence Nurs. 2011;38(4):433–445. [DOI] [PubMed] [Google Scholar]
- 10.Driver DS. Perineal dermatitis in critical care patients. Crit Care Nurse. 2007;27(4):42–46; quiz 47. [PubMed] [Google Scholar]
- 11.Long MA, Reed LA, Dunning K, Ying J. Incontinence-associated dermatitis in a long-term acute care facility. J Wound Ostomy Continence Nurs. 2012;39(3):318–327. [DOI] [PubMed] [Google Scholar]
- 12.Rohwer K, Bliss DZ, Savik K. Incontinence-associated dermatitis in community-dwelling individuals with fecal incontinence. J Wound Ostomy Continence Nurs. 2013;40(2):181–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Houwing RH, Arends JW, Canninga-van Dijk MR, Koopman E, Haalboom JR. Is the distinction between pressure ulcers and moisture lesions justifiable? A clinical-pathological study. Skinmed. 2007;6(3):113–117. [DOI] [PubMed] [Google Scholar]
- 14.Demarré L, Beeckman D, Vanderwee K, et al. Multi-stage versus single-stage inflation and deflation cycle for alternating low pressure air mattresses to prevent pressure ulcers in hospitalized patients: a randomized-controlled clinical trial. Int J Nurs Stud. 2012;49(4):416–426. [DOI] [PubMed] [Google Scholar]
- 15.Demarré L, Verhaeghe S, Van Hecke A, et al. Factors predicting the development of pressure ulcers in an at-risk population who receive standardized preventive care: secondary analyses of a multicentre randomised controlled trial. J Adv Nurs. 2015;71(2):391–403. [DOI] [PubMed] [Google Scholar]
- 16.Beeckman D, Van Lancker A, Van Hecke A, Verhaeghe S. A systematic review and meta-analysis of incontinence-associated dermatitis, incontinence, and moisture as risk factors for pressure ulcer development. Res Nurs Health. 2014;37(3):204–218. [DOI] [PubMed] [Google Scholar]
- 17.Lachenbruch C, Ribble D, Emmons K, VanGilder C. Pressure ulcer risk in the incontinent patient: analysis of incontinence and hospital-acquired pressure ulcers from the International Pressure Ulcer Prevalence™ Survey. J Wound Ostomy Continence Nurs. 2016;43(3):235–241. [DOI] [PubMed] [Google Scholar]
- 18.Kottner J, Blume-Peytavi U, Lohrmann C, Halfens R. Associations between individual characteristics and incontinence-associated dermatitis: a secondary data analysis of a multi-centre prevalence study. Int J Nurs Stud. 2014;51(10):1373–1380. [DOI] [PubMed] [Google Scholar]
- 19.Gray M. Incontinence associated dermatitis: relationship to urinary incontinence. J Wound Ostomy Continence Nurs. 2012;39(suppl 3S):S5–S6; abstract 6012. [DOI] [PubMed] [Google Scholar]