Abstract
PURPOSE:
To evaluate the impact of a postdischarge ostomy support program as an adjunct to nurse-led ostomy care on preventable healthcare utilization.
DESIGN:
A cross-sectional study.
SUBJECTS AND SETTING:
A postdischarge support program offered by an ostomy product's manufacturer provides persons living with an ostomy with patient-centered and easily accessible assistance. Individuals who underwent ostomy surgery within 18 months prior to the survey date were selected from an ostomy patient database maintained by the ostomy patient support program provider. Of 7026 surveys sent to program enrollees, 493 (7%) responded, compared with 225 (5%) out of 4149 surveys sent to individuals in a comparison group. The 2 groups were similar in demographics. A majority of the survey respondents were female (60% of program enrollees vs 55% of respondents in the comparison group). Among the program enrollees, 44% had colostomy, 43% had ileostomy, 10% had urostomy, and 4% had at least 2 types of ostomy surgery compared with 52%, 32%, 12%, and 4% of the respondents in a comparison group, respectively.
METHODS:
The study compared hospital readmission and emergency room (ER) visit rates attributable to ostomy complications between program enrollees and respondents in the comparison group. The event rates were measured in 2 study periods: within the first month of discharge and after the first month of discharge. Eligible individuals received an online survey that included the following domains: characteristics of ostomy surgery; readmissions and ER visits within the first month or after the first month of discharge, including reasons for preventable events; and level of health care access. Multivariate logistic regressions controlling for covariates were applied to investigate associations between program enrollment and ostomy-related readmission or ER visit rates.
RESULTS:
Logistic regression analyses showed that, when compared with respondents in the comparison group, program enrollees had a significantly lower likelihood of being readmitted and visiting the ER due to ostomy complications after the first month of hospital discharge and up to 18 months postdischarge (odds ratio [OR] = 0.45; 95% confidence interval [CI], 0.27-0.73; and OR = 0.37; 95% CI, 0.22-0.64, respectively).
CONCLUSIONS:
Findings suggest that enrolling patients in the postdischarge ostomy support program provides an effective approach to reducing preventable healthcare utilization.
Keywords: Avoidable hospital readmission, Colostomy, Complications, Education, Healthcare utilization, Hospital readmission, Ileostomy, Ostomy, Postdischarge program, Stoma, Support, Urostomy
INTRODUCTION
Many patients diagnosed with diverticulitis,1 colon cancer, inflammatory bowel disease, urothelial cancers, and nonmalignant lower urinary tract dysfunction undergo ostomy surgery.2 In the United States, as many as 100,000 Americans undergo ostomy operations each year.3 For many, creation of an ostomy surgery provides a welcome relief from debilitating symptoms, but management of a fecal or urinary stoma also presents significant challenges.4,5 For instance, Bare and colleagues5 reported that limited knowledge in ostomy management and the selection of a proper ostomy system can have an impact on patient outcomes. Typically, patients are sent back to community care within 1 week of ostomy creation.6 A majority of these individuals experience life adjustment difficulties7 and postoperative complications.8 Such postoperative complications often lead to unexpected hospital readmissions9 and may also result in emergency room (ER) visits. According to US hospital readmission statistics from the Healthcare Cost and Utilization Project (HCUP),10 ileostomies and other fecal ostomies had the second highest 30-day readmission rates. These healthcare utilization events are costly and frequently preventable with better patient education and self-care empowerment.2,11,12
Previous research has found that postoperative educational programs, including education checklists, visiting nurse services, and educational materials, are associated with lower rates of readmission due to postoperative complications.6,13,14 The American College of Surgeons (ACS) Ostomy Home Skills kit14 is an educational tool that contains a stoma practice model and a booklet with information on operation and home skills. Three versions of the ACS kit have been developed for persons undergoing colostomy, ileostomy, and urostomy. The ACS kit provides training for self-care skills to assist persons living with an ostomy with their preparation and optimal recovery14; they are associated with a decrease in ER visit rates after an ostomy operation.15 Despite this promising evidence, many people with an ostomy still experience difficulties related to their stoma while they are recovering at home and often seek other compatible, readily available support, such as Internet information and social support, to enhance self-care.16,17
A patient-tailored, postdischarge support program (Coloplast Care; Coloplast, Minneapolis, Minnesota) has been developed in an effort to provide persons living with an ostomy with patient-centered and easily accessible assistance.18 Enrollment in the program is free for anyone living with an ostomy regardless of the type of ostomy pouching system he or she currently uses for general disease state and lifestyle support. However, product-specific advice is limited to the patient support program provider's products. This support program provides and extends postoperative education provided by WOC nurses and other providers. While persons living with an ostomy can enroll in the program before their ostomy surgery, most join the program postoperatively and are enrolled by a healthcare professional with the individual's consent. Once enrolled, persons living with an ostomy receive assistance from the support program via 3 core components. A team of trained program advisors actively contact persons living with an ostomy by phone to provide lifestyle advice, as well as practical and emotional support. The program advisors also help address concerns regarding locating an ostomy supplier, product access, and questions that may arise pre- or postsurgery. A support program provides a discreet travel kit that includes requested product samples, a stoma-measuring guide, scissors, a mirror for use during product application, an accessory kit, instructions for use, a marking pen, and instructional DVD. The program also provides enrolled individuals access to monthly wellness education addressing lifestyle issues, such as returning to normal daily living, traveling with an ostomy, and engaging in outdoor activities. While this program aims to improve health-related quality-of-life transition after ostomy surgery and to prevent postoperative complications, little is known as to whether it decreases preventable healthcare utilization over time.
The aim of this study was to determine the impact of the support program on the occurrence of avoidable hospital readmission and ER visits following ostomy surgery. Specifically, I sought to assess the impact of the postdischarge support program on preventable healthcare utilization occurring during 2 study periods: (1) within the first month of hospital discharge, and (2) after the first month of hospital discharge (defined as at least 30 days after discharge until the survey date) to study the long-term effect. The maximum period from hospital discharge until the survey date was 18 months. While the ACS kit is not part of the patient support program, previous studies exist that evaluate whether the ACS kit was associated with reducing hospitalizations without investigation of readmissions and ER visits.15 Therefore, a secondary aim was to determine whether the use of the ACS kit influenced ostomy-related hospital readmissions and ER visits.
METHODS
A cross-sectional online survey study was conducted to collect data related to experience living with an ostomy. The survey approach was chosen for 2 reasons. The online survey enabled us to gather information about race, ethnicity, and level of education19 that may contribute to the likelihood of hospital readmission and/or ER visits. A survey was used to collect these data because they were not available in other data sources we had access to, such as administrative claims data. Second, the survey permitted me to gather data on persons living with an ostomy with various health benefits and insurance plans, resulting in higher generalizability.
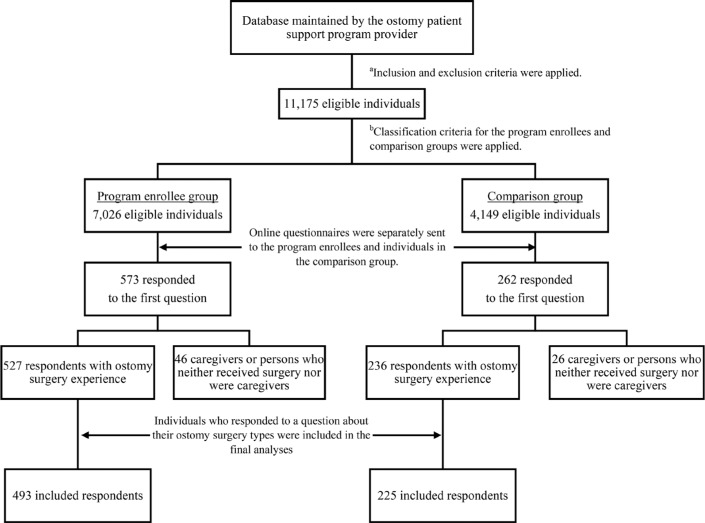
An overview of subject recruitment and responses is presented in the Figure. Individuals were eligible for the study if they were at least 18 years of age at the time of the survey, were able to read English, were a resident in 50 US states and the District of Columbia, and had an e-mail address available in the ostomy patient database maintained by the ostomy patient support program provider. This study included individuals with all types of ostomy surgery: colostomy, ileostomy, urostomy, and multiple stomas. To minimize recall bias and focus on patients with a new stoma, individuals were included if their ostomy surgery date was within 18 months prior to the survey date. Individuals were excluded if their survey date was not recorded in the database or if they did not provide consent to receive an e-mail from the program provider.
Figure 1.
An overview of the survey procedure and the patient flow. aInclusion criteria include being 18 years of age at the time of the survey, able to read English, a resident in 50 US states and the District of Columbia, and having an e-mail address in the ostomy patient database. Exclusion criteria include no record of the survey date in the database or no consent to receive an e-mail from the program provider. bClassification criteria for the program enrollee group include having at least 2 months of communication with a program advisor during the 12-month period following ostomy surgery and receiving program wellness education resources provided by a program advisor. The individuals were categorized into the comparison group if they subscribed to a company-generated newsletter but had neither communicated with a program advisor nor received program wellness education.
An E-mail address and the surgery date for eligible individuals were retrieved from the database without any other personally identifiable information. I then classified them into either the program enrollee group or the comparison group, using the following criteria. Program enrollees were required to have at least 2 months of communication with a program advisor during the 12-month period following ostomy surgery to ensure adequate engagement with a program advisor. Program enrollees were also required to receive program wellness education resources provided by a program advisor. Respondents were categorized as members of the comparison group if they voluntarily subscribed to a company-generated newsletter but did not communicate with a program advisor or receive program wellness education in the 12 months following ostomy surgery.
Questionnaires
Two separate questionnaires were generated using the online survey tool Wufoo (SurveyMonkey Inc, Palo Alto, California). To ensure that this study included only survey respondents who had undergone ostomy surgery, the first question of the survey asked respondents to select one of the following options that best described them: “I am a person who received ostomy surgery,” “I am a caregiver who provides assistance to a person who received ostomy surgery,” or “I am neither a person who received ostomy surgery nor a caregiver.” Respondents who indicated that they were a caregiver who provided assistance to a person living with an ostomy or that they were neither a person living with an ostomy nor a caregiver were directed to the end of the survey. Their data were not included in this study.
Each survey comprised 51 questions, and the survey took approximately 10 minutes to complete. The survey included items that queried demographics data and characteristics of ostomy surgery, the number of hospital readmissions and ER visits within the first month of discharge, and the number of ER visits and hospital admissions more than 1 month following hospital discharge that led to creation of their ostomy. The survey also queried reasons for preventable ER visits or hospital readmissions, whether they received and utilized the ACS kit, level of healthcare access, and demographic data.
Items related to demographic data queried age, which was categorized into: 3 age ranges (18 to 50 years, 51 to 70 years, or 71 years or older); gender (male or female); race (white or nonwhite); and the highest level of education (at least a bachelor's degree obtained or less than a bachelor's degree obtained). Ostomy surgery–related items queried ostomy type (colostomy, ileostomy, or urostomy), and medical condition leading to ostomy creation (colon cancer, diverticulitis, inflammatory bowel disease, trauma, and/or other reasons).
To determine if a hospital readmission occurred in each study period (within the first month of discharge and after the first month of discharge), participants were asked if they returned and stayed in a hospital at least overnight (yes or no). They also reported if they needed to go to the ER within each study period (yes or no) and provided the reason(s) for readmission or visiting the ER. The reasons for these healthcare utilization events included dehydration, surgical site infection, or other issues related to ostomy surgery (urosepsis, urinary tract infections, bleeding around the stoma, skin erosions, dehydration, malnutrition, and other issues not related to ostomy surgery). Respondents were asked if they received the ACS kit; an image of the kit was provided within the online survey to enhance recognition. If yes, they were asked if they used the materials inside the kit to familiarize themselves with stoma and ostomy supplies (yes or no).
Questions about level of healthcare access included whether a person living with an ostomy visited an ostomy clinic after surgery (yes or no), had home health nurse visits after surgery (yes or no), had insurance coverage for ostomy supplies (yes or no), and received other patient support programs (yes or no).
Study Procedures
In May 2016, an invitation e-mail with the objectives and importance of the study was sent to potential participants. If they agreed to participate in the survey, they were invited to click on the link to the survey questionnaire within the e-mail. Two follow-up e-mails were sent 1 and 2 weeks apart after the first survey e-mail to those who did not respond to the initial survey. This study employed an anonymous survey procedure. Specifically, no personal information, such as name, date of birth, or address, was collected in order to assure privacy and encourage greater disclosure of ostomy-related information.20 The institutional review board (IRB) determination submission of this study was reviewed by the University of Minnesota's IRB, and it determined that full board review was not required. Completion of the survey was interpreted as consent for study participation. Participation in the research survey was voluntary, and respondents were free to exit the survey at any time.
Data Analysis
The outcome (dependent) variables in this study were hospital readmission and ER visits due to ostomy-related postoperative complications occurring within 2 study periods: (1) within the first month of discharge, and (2) after the first month of hospital discharge. These events were operationally defined as preventable healthcare utilization. The ostomy-related readmissions and ER visits were calculated from respondent-reported reasons for readmitting or visiting the ER. These outcomes were recoded as a dichotomous variable (yes or no). The secondary outcome, whether persons with ostomies received and used the ACS kit for repetitive practice of ostomy self-care, was also recoded as a dichotomous outcome (yes or no). Patient characteristics were reported using descriptive analyses. The χ2 test was used to assess differences in the characteristics of the survey respondents in the program enrollee and comparison groups.
Multivariate logistic regression (MLR) analyses were performed to estimate the effect of the postdischarge support program on the rates of ostomy-related hospital readmissions and ER visits. These analyses were used to (1) account for covariates likely to confound the relationship between enrolling in the postdischarge support program and the 2 outcomes, and (2) balance the distribution of characteristics between program enrollees and respondents in the comparison group. Covariates were age, gender, race, the highest level of education, ostomy type, medical condition requiring ostomy surgery, visiting an ostomy clinic after surgery, having home health nurse visits, having insurance coverage for ostomy supplies, and receiving other patient support programs. Whether persons living with an ostomy received and utilized the ACS kit was also included in the models, as this study aimed to demonstrate its effect on ostomy-related hospital readmission and ER visits. Respondents with all 3 types of ostomy surgery were considered in all analyses. All statistical tests were 2-tailed using a significance level of .05 and carried out using Statistical Analysis System (SAS, version 9.3; SAS Institute Inc, Cary, North Carolina).
RESULTS
Of 7026 surveys sent to postdischarge support program enrollees, 493 (7%) responded to the survey, compared with 225 (5%) out of 4149 surveys sent to individuals in the comparison group. Table 1 compares characteristics of program enrollee and comparison groups. A higher proportion of program enrollees were younger than 51 years (P < .0001) and held at least a bachelor's degree compared to respondents in the comparison group (P = .02). Forty percent of program enrollees received and utilized the ACS kit to familiarize themselves with stoma care, compared with 18% of counterparts not enrolling in the program (P < .0001). Colon cancer was the most common medical condition requiring ostomy surgery in both groups (30% vs 26%, P = .03). There were no statistically significant differences in gender, race, whether persons living with an ostomy visited an ostomy clinic after surgery, had home health nurse visits after surgery, or received other patient support programs.
TABLE 1. Baseline Characteristics of Respondents in the Post-Discharge Support Program and Comparison Groups.
| Characteristics | Postdischarge Support Program Enrollees, n (%) | Comparison Group, n (%) | Pa,b |
|---|---|---|---|
| Demographics | |||
| Age range | n = 433 | n = 205 | <.0001 |
| 18-50 y | 120 (28) | 22 (11) | |
| 51-70 y | 248 (57) | 114 (56) | |
| ≥71 y | 65 (15) | 69 (34) | |
| Gender | n = 430 | n = 205 | .29 |
| Male | 174 (40) | 92 (45) | |
| Female | 256 (60) | 113 (55) | |
| Race | n = 433 | n = 205 | .44 |
| White | 391 (90) | 181 (88) | |
| Nonwhite | 42 (10) | 24 (11) | |
| Highest level of education obtained | n = 403 | n = 184 | .02 |
| At least a bachelor's degree | 183 (45) | 65 (35) | |
| Less than a bachelor's degree | 220 (55) | 119 (65) | |
| Characteristics of ostomy surgery | n = 493 | n = 225 | .05 |
| Type of ostomy surgery | 216 (44) | 117 (52) | |
| Colostomy | 211 (43) | 72 (32) | |
| Ileostomy | 47 (10) | 27 (12) | |
| Urostomy | 19 (4) | 9 (4) | |
| At least 2 types of ostomy surgery | |||
| Medical condition requiring ostomy surgery | n = 493 | n = 225 | .04 |
| Colon cancer | 150 (30) | 58 (26) | |
| Diverticulitis | 67 (14) | 37 (16) | |
| Ulcerative colitis | 54 (11) | 21 (9) | |
| Crohn disease | 51 (10) | 12 (5) | |
| Trauma | 12 (2) | 11 (5) | |
| Inflammatory bowel disease | 10 (2) | 2 (1) | |
| Other reasons | 149 (30) | 84 (37) | |
| Level of healthcare access | .49 | ||
| Visited an ostomy clinic after surgery | n = 467 | n = 208 | |
| Yes | 229 (49) | 96 (46) | |
| No | 238 (51) | 112 (54) | |
| Had home health nurse visits after surgery | n = 467 | n = 208 | .26 |
| Yes | 364 (78) | 170 (82) | |
| No | 103 (22) | 38 (18) | |
| Had insurance coverage for ostomy supplies | n = 461 | n = 206 | .54 |
| Yes | 421 (91) | 191 (93) | |
| No | 40 (9) | 15 (7) | |
| Received and utilized the ACS kit | n = 461 | n = 206 | <.0001 |
| Yes | 183 (40) | 39 (18) | |
| No | 278 (60) | 167 (81) | |
| Received other patient support programs | n = 436 | n = 206 | .14 |
| Yes | 137 (31) | 53 (26) | |
| No | 299 (69) | 153 (74) | |
Abbreviation: ACS, American College of Surgeons.
aThe χ2 test compares values between the program enrollee and comparison groups.
bFigures in bold indicate statistical significance at α= .05.
Table 2 reports rates of ostomy-related readmissions and ER visits within the first month of discharge and after the first month of hospital discharge. A significantly lower proportion of program enrollees experienced hospital readmission within the first month of discharge due to ostomy-related reasons (17% vs 25%, P = .03). For events occurring after the first month of hospital discharge, both the proportions with hospital readmissions and ER visits were significantly lower in the program enrollee group versus the comparison group (16% vs 24%, P = .02; 12% vs 21%, P = .001, respectively).
TABLE 2. Comparison of Ostomy-Related Healthcare Utilization Rates Occurring Within the 2 Study Periodsa.
| Period | Healthcare Utilization | Postdischarge Support Program Enrollees, n (%) | Comparison Group, n (%) | Pb,c |
|---|---|---|---|---|
| Within the first month of discharge | Readmission | n = 489 | n = 223 | .03 |
| Yes | 85 (17) | 55 (25) | ||
| No | 404 (83) | 168 (75) | ||
| ER visit | n = 483 | n = 221 | .57 | |
| Yes | 100 (21) | 50 (23) | ||
| No | 383 (79) | 171 (77) | ||
| After the first month of discharge | Readmission | n = 480 | n = 219 | .02 |
| Yes | 78 (16) | 52 (24) | ||
| No | 402 (84) | 167 (76) | ||
| ER visit | n = 478 | n = 217 | .001 | |
| Yes | 56 (12) | 46 (21) | ||
| No | 422 (88) | 171 (79) |
Abbreviation: ER, emergency room.
aTwo study periods: (1) within the first month of discharge, and (2) after the first month of discharge until the survey date.
bThe χ2 test compares the quality of proportions between the program enrollee and comparison groups.
cFigures in bold indicate statistical significance at α= .05.
Table 3 summarizes results of the MLR analyses for the outcomes of interest. Enrolling in the postdischarge support program was associated with lower hospital readmission and ER visit rates due to ostomy-related complications occurring after the first month of hospital discharge. When accounting for demographics, characteristics of ostomy surgery and level of healthcare access, the adjusted odds ratio (aOR) of having hospital readmission occurring after the first month of hospital discharge was 55% lower in the program enrollee group compared with the comparison group (aOR = 0.45; 95% confidence interval [CI], 0.27-0.73). When compared with respondents in the comparison group, program enrollees had significantly lower odds of visiting the ER after the first month of discharge (aOR = 0.37; 95% CI, 0.22-0.64). Likewise, after controlling for demographics, characteristics of ostomy surgery, and level of healthcare access, using the ACS kit was associated with significantly lower hospital readmission and ER visit rates occurring within the 2 study periods.
TABLE 3. Adjusted Odds Ratios for Ostomy-Related Healthcare Utilization Occurring Within the 2 Study Periodsa From Multivariate Logistic Regression Analysesb.
| Variables | aOR (95% CI)c | |||
|---|---|---|---|---|
| Within the First Month of Discharge | After the First Month of Discharge | |||
| Readmission | ER Visits | Readmission | ER Visits | |
| A postdischarge support program | ||||
| Enrolled | 0.82 (0.50-1.36) | 0.97 (0.60-1.58) | 0.45 (0.27-0.73)d | 0.37 (0.22-0.64)d |
| Not enrolled | 1.00 | 1.00 | 1.00 | 1.00 |
| Received and utilized the ACS kit | ||||
| Yes | 0.58 (0.34-0.98)e | 0.50 (0.31-0.83)e | 0.58 (0.34-0.99)e | 0.39 (0.20-0.74)e |
| No | 1.00 | 1.00 | 1.00 | 1.00 |
Abbreviations: ACS, American College of Surgeons; aOR, adjusted odds ratio; CI, confidence interval; ER, emergency room.
aTwo study periods: (1) within the first month of discharge, and (2) after the first month of discharge until the survey date.
bAll models were adjusted for age, gender, race, the highest level of education, ostomy type, a medical condition requiring ostomy surgery, whether persons living with an ostomy visited an ostomy clinic after surgery, had home health nurse visits, had insurance coverage for ostomy supplies, and received other patient support programs.
cThe finding is statistically significant if the 95% CI does not include aOR = 1.
dPersons living with an ostomy who enrolled in a support program had significantly lower odds of ostomy-related healthcare utilization than their counterparts in the comparison group.
ePersons living with an ostomy who utilized the ACS kit had significantly lower odds of ostomy-related healthcare utilization than their counterparts who did not utilize the kit.
DISCUSSION
This cross-sectional study provides insight into the impact of an easily accessible, postdischarge support program on preventable healthcare utilization, namely, ostomy-related hospital readmission and ER visits. The support program was associated with fewer hospital readmissions and ER visits owing to ostomy-related postoperative complications. Specifically, the likelihood of hospital readmission due to ostomy-related issues after the first month of discharge for persons living with an ostomy who enrolled in the support program is 55% lower than the likelihood for persons with an ostomy in the comparison group.
Our findings are congruent with previous research that found significant improvement in ostomy adjustment and complications when persons with an ostomy received nurse telephone follow-up.21 Persons with an ostomy face physical and psychological challenges and economic and personal concerns as they adjust to the stoma.22–24 An advisor of the support program actively calls program enrollees to address their needs, provide customized product samples, and help develop their personalized ostomy routine. Our experience suggests that regular communication with a program advisor helps persons living with an ostomy master self-care skills that translate into a decrease in long-term hospital readmissions and ER visits due to ostomy complications.
According to the Wound, Ostomy and Continence Nurses (WOCN) Society/American Society of Colon and Rectal Surgeons (ASCRS) and WOCN/American Urological Association (AUA) Clinical Practice Guidelines for Ostomy Surgery, persons living with an ostomy should have access to an ostomy nurse specialist, specifically a certified WOC nurse, whenever possible.25,26 However, persons living with the condition may experience access barriers due to geographic distance, posing a hospital readmission risk.2 Patients with chronic conditions who live in remote areas are more vulnerable to preventable hospitalizations during life transitions and major life changes.27 As an easily accessible resource, a postdischarge support program that includes active engagement with a program advisor and one-on-one support can help persons with an ostomy overcome access challenges and facilitate postoperative nursing care.
Along with the favorable findings of the support program, findings indicate that using the ACS kit was associated with decreased ER visits, which occurred within 30 days from the discharge date and after the first month of discharge. The effect of the ACS kit is important since persons living with an ostomy who used the kit to familiarize themselves with their stoma care had 61% lower odds of visiting the ER 1 month after hospital discharge due to ostomy-related postoperative complications. This finding is consistent with previous research by Heneghan,15 who found that persons with an ostomy who did not use the ACS kit are twice as likely as their counterparts who used the kit to visit the ER in the 2 weeks after hospital discharge following creation of a stoma. Use of the kit was also associated with a 42% reduction in hospital readmission rates within the first month of discharge and after the first month of discharge. Use of the ACS kit should be encouraged prior to ostomy surgery whenever possible and by the time of hospital discharge in all cases.
Aside from the benefits of tailored support from the postdischarge support program and the ACS kit, findings revealed that 21% of respondents in the comparison group experienced an ostomy-related readmission or an ER visit within the first month of discharge and after the first month of hospital discharge, up to 18 months postdischarge. These rates are higher than those described in a retrospective review conducted in a single medical center.12 Messaris and colleagues12 reported that the 60-day readmission rate was 17% among patients who underwent colon and rectal resections resulting in an ileostomy. It is plausible that respondents in this study reflect samples that are representative of a larger population. Even though the rates of ostomy-related readmissions and ER visits from this current study are alarmingly high and confirm the need for better management of postoperative complications,28 the rates also suggest room for improvement in avoiding unnecessary utilization among persons living with an ostomy who did not receive the full benefits of the patient support program.
STRENGTHS AND LIMITATIONS
There are 3 main limitations in this study. Data were collected using a cross-sectional design capable of demonstrating associations, but not a causality, between enrolling in the postdischarge support program and hospital readmission and ER visits. Nevertheless, MLR analyses were employed to reach justifiable inferences by adjusting for measured covariates confounding the relationship between the postdischarge support program and preventable healthcare utilization. Second, because of the relatively low survey response rates (7% for program enrollees and 5% for respondents in the comparison group), results are vulnerable to selection bias that may negatively affect generalizability of findings.29 Despite the small response rates, the number of respondents from both the program enrollee and comparison groups exceeded required sample size; thus, this study achieved adequate statistical power to detect the differences between the 2 groups. Third, this study relied on patient-reported information. Although the maximum recall period for questions in the survey was less than 18 months before the survey date, the respondents might not have remembered events that occurred in the past.
While this study provided important implications for managing ostomy care, these results were only a demonstration of the postdischarge support program and the ACS kit effect. The program we evaluated is designed to supplement care that persons living with an ostomy received from their providers. Future research should explore the impact of the program in combination with WOC nurse–delivered support interventions on avoidable healthcare utilization. By investigating their amplifying effects, the discovery of complementary strategies is likely to result in advances in postdischarge care for people with ostomies.
CONCLUSIONS
Study findings suggest that the postdischarge support program reduced the likelihood of hospital readmissions and ER visits due to postoperative complications. Such a support program is a readily available resource that could be used as an adjunct to standardized preoperative and postoperative ostomy education to decrease the incidence of preventable healthcare utilization and to optimize evidence-based practice in ostomy care. Study findings also support early use of the ACS kit in persons undergoing ostomy surgery.
ACKNOWLEDGMENTS
This study was supported by Coloplast Corp. The author thanks Angeline M. Carlson, PhD, Professor at Department of Pharmaceutical Care & Health Systems, College of Pharmacy, University of Minnesota, and Director of Health Economics and Outcomes Research at Data Intelligence Consultants, LLC, for critical review of study proposal and data interpretation. The author expresses her gratitude to the employees at Coloplast Corp: Martin Nottmeier, Alan Au, Sonia McDonough, Margaret Gardner-Westmark, and Henrik Fisker Würgler, for data collection and survey distribution, and Zenia Størling, for editorial assistance in the preparation of the manuscript. The author also greatly appreciates Janet Stoia-Davis, RN, CWOCN CFCN, Stoia Consultants, for scientific review of the survey questionnaire and the manuscript. Coloplast Corp had no role in the data analysis.
Footnotes
Preliminary results of this study were presented as a poster presentation at 20th International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Annual European Congress in November 2017.
Ms Rojanasarot was a graduate trainee at Coloplast Corp during the study period.
REFERENCES
- 1.Wieghard N, Geltzeiler CB, Tsikitis VL. Trends in the surgical management of diverticulitis. Ann Gastroenterol. 2015;28(1):25–30. [PMC free article] [PubMed] [Google Scholar]
- 2.Hendren S, Hammond K, Glasgow SC, et al. Clinical practice guidelines for ostomy surgery. Dis Colon Rectum. 2015;58(4):375–387. [DOI] [PubMed] [Google Scholar]
- 3.Ostomy Guidelines Task Force; Goldberg M, Aukett LK, et al. Management of the patient with a fecal ostomy: best practice guideline for clinicians. J Wound Ostomy Continence Nurs. 2010;37(6):596–598. [DOI] [PubMed] [Google Scholar]
- 4.The National Institute of Diabetes and Digestive and Kidney Diseases. Ostomy surgery of the bowel. https://www.niddk.nih.gov/health-information/health-topics/digestive-diseases/ostomy-surgery-bowel/Pages/ez.aspx. Published August 2014. Accessed September 20, 2017.
- 5.Bare K, Drain J, Timko-Progar M, et al. Implementation of an evidence-based and content validated standardized ostomy algorithm tool in home care: a quality improvement project. J Wound Ostomy Continence Nurs. 2017;44(3):262–266. [DOI] [PubMed] [Google Scholar]
- 6.Nagle D, Pare T, Keenan E, Marcet K, Tizio S, Poylin V. Ileostomy pathway virtually eliminates readmissions for dehydration in new ostomates. Dis Colon Rectum. 2012;55(12):1266–1272. [DOI] [PubMed] [Google Scholar]
- 7.Pittman J, Rawl SM, Schmidt CM, et al. Demographic and clinical factors related to ostomy complications and quality of life in veterans with an ostomy. J Wound Ostomy Continence Nurs. 2008;35(5):493–503. [DOI] [PubMed] [Google Scholar]
- 8.Robertson I, Leung E, Hughes D, et al. Prospective analysis of stoma-related complications. Colorectal Dis. 2005;7(3):279–285. [DOI] [PubMed] [Google Scholar]
- 9.Sheetz KH, Waits SA, Krell RW, et al. Complication rates of ostomy surgery are high and vary significantly between hospitals. Dis Colon Rectum. 2014;57(5):632–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weiss AJ, Elixhauser A, Steiner C. Readmissions to U.S. hospitals by procedure, 2010. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb154.pdf. Published April 2013. Accessed September 20, 2017.
- 11.Wick EC, Shore AD, Hirose K, et al. Readmission rates and cost following colorectal surgery. Dis Colon Rectum. 2011;54(12):1475–1479. [DOI] [PubMed] [Google Scholar]
- 12.Messaris E, Sehgal R, Deiling S, et al. Dehydration is the most common indication for readmission after diverting ileostomy creation. Dis Colon Rectum. 2012;55(2):175–180. [DOI] [PubMed] [Google Scholar]
- 13.Hardiman KM, Reames CD, McLeod MC, Regenbogen SE. Patient autonomy-centered self-care checklist reduces hospital readmissions after ileostomy creation. Surgery. 2016;160(5):1302–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American College of Surgeons. Skills programs. https://www.facs.org/education/patient-education/skills-programs. Published 2016. Accessed September 20, 2017.
- 15.Heneghan K. Surgical Patient Educational Skills Program Effectively Prepares Patients to Confidently Manage Their Post-operative Recovery. Chicago, IL: Division of Education, American College of Surgeons; 2012. [Google Scholar]
- 16.Bonill-de-las-Nieves C, Celdrán-Mañas M, Hueso-Montoro C, et al. Living with digestive stomas: strategies to cope with the new bodily reality. Rev Lat Am Enfermagem. 2014;22(3):394–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Richbourg L, Thorpe JM, Rapp CG. Difficulties experienced by the ostomate after hospital discharge. J Wound Ostomy Continence Nurs. 2007;34(1):70–79. [DOI] [PubMed] [Google Scholar]
- 18.Coloplast Corp. Welcome to Coloplast® Care. http://www.coloplast.us/ostomy-care/. Published 2016. Accessed September 20, 2017.
- 19.Andersen R. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 20.Murdoch M, Simon AB, Polusny MA, et al. Impact of different privacy conditions and incentives on survey response rate, participant representativeness, and disclosure of sensitive information: a randomized controlled trial. BMC Med Res Methodol. 2014;14:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang JE, Wong FK, You LM, et al. Effects of enterostomal nurse telephone follow-up on postoperative adjustment of discharged colostomy patients. Cancer Nurs. 2013;36(6):419–428. [DOI] [PubMed] [Google Scholar]
- 22.Dabirian A, Yaghmaei F, Rassouli M, Tafreshi MZ. Quality of life in ostomy patients: a qualitative study. Patient Prefer Adherence. 2010;5:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nichols TR. Health-related quality of life in community-dwelling persons with ostomies: the physical functioning domain. J Wound Ostomy Continence Nurs. 2015;42(4):374–377. [DOI] [PubMed] [Google Scholar]
- 24.Nichols TR. Quality of life in persons living with an ostomy assessed using the SF36v2: mental component summary: vitality, social function, role-emotional, and mental health. J Wound Ostomy Continence Nurs. 2016;43(6):616–622. [DOI] [PubMed] [Google Scholar]
- 25.Salvadalens G, Hendern S, McKenna L, et al. WOCN Society and ASCRS position statement on preoperative stoma site marking for patients undergoing urostomy surgery. J Wound Ostomy Continence Nurs. 2015;42(3):240–252. [DOI] [PubMed] [Google Scholar]
- 26.Salvadalena G, Hendern S, McKenna L, et al. WOCN Society and AUA position statement on preoperative stoma site marking for patients undergoing urostomy surgery. J Wound Ostomy Continence Nurs. 2015;42(3):253–256. [DOI] [PubMed] [Google Scholar]
- 27.Brundisini F, Giacomini M, DeJean D, Vanstone M, Winsor S, Smith A. Chronic disease patients' experiences with accessing health care in rural and remote areas. Ont Health Technol Assess Ser. 2013;13(15):1–33. [PMC free article] [PubMed] [Google Scholar]
- 28.Kassin MT, Owen RM, Perez S, et al. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012;215(3):322–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kukull WA, Ganguli M. Generalizability: the trees, the forest, and the low-hanging fruit. Neurology. 2012;78(23):1886–1891. [DOI] [PMC free article] [PubMed] [Google Scholar]