Abstract
Objective
Previous studies conducted in Japan targeted only mothers who cared for children with disabilities, and lacked reference subjects, such as mothers of children without disabilities. The aim of this study was to examine the association between raising one or two children with a disability and maternal psychological distress compared to mothers of children without a disability, and to assess differences among partnered mothers living with grandparent(s), partnered mothers without grandparent(s), and single mothers.
Methods
This study utilized data from the Comprehensive Survey of Living Conditions (CSLC) in 2010. We merged the data of the children (aged six and over), mothers, and fathers. This study obtained 33,739 study subjects as a triad of a child (33,110 children without disabilities and 629 children with disabilities), mother, and father. The Japanese version of Kessler 6 (K6) was used to assess the psychological distress of mothers. Multivariate logistic regression was performed to assess the independent association of a child with a disability on maternal psychological distress after controlling for the basic characteristics of the children, mothers, and households.
Results
This study reported that raising one or two children with disabilities was significantly related to maternal psychological distress (odds ratio: 1.72 for one child, 2.85 for two children) compared to mothers of children without disability. After stratifying the analyses by family structure, significant associations remained among mothers in two-parent families but not for mothers in three-generation families and single mothers due to a small number of children with disabilities in these families.
Conclusions
This study reported the significant association between raising a child with a disability and maternal psychological distress in comparison to mothers of children without disabilities. Attention should be paid to not only single mothers, but also partnered mothers in two-parent families who have a child with a disability. It is important for health professionals to focus on the mental health of every mother of a child with a disability and to assess their needs for psychological support.
Keywords: Children with disabilities, Mothers, Psychological distress, Family structure, Japan
Highlights
-
•
This study examined the association between raising a child with a disability and maternal psychological distress.
-
•
We compared differences among mothers of child with or without disability using a population-based survey.
-
•
Raising one or two children with a disability had a significant association with maternal psychological distress.
-
•
Significant associations remained among mothers in only two-parent families.
-
•
It is important for health professionals to focus on mental health of every mother of child with a disability.
1. Background
Raising a child with a disability is an unexpected experience for parents (Raina et al., 2005). Caring for a child with a disability, depending on the type of disability, can result in physical health problems, mental health problems, and time or financial burdens on mothers (Raina et al., 2005, Bourke et al., 2008, Brehaut et al., 2004, Estes et al., 2013, Lee, 2013, Montes and Halterman, 2008, Montes and Halterman, 2008, Nes et al., 2014, Parish et al., 2012; Raina et al., 2005). In particular, maternal mental health is important for both mothers and children because poor maternal mental health is related to unfavorable parenting practices (McLennan and Kotelchuck, 2000, Minkovitz et al., 2005), child health problems (Ferro and Speechley, 2009, Schwebel and Brezausek, 2008), and poor school performance (Shen et al., 2016).
Mothers play a major role in childrearing, regardless of the presence or absence of a disability. Supporting mothers is a public issue because Japanese society faces a proliferation of nuclear and dual-income families. Paternal involvement in childrearing remains to a small extent in the present circumstances. For example, the parental leave obtainment rate was only 2.0% of full-time working fathers (The Ministry of Health Labour and Welfare, 2012), and fathers seldom commit to household chores and childrearing tasks (i.e., only 39 minutes per week in dual-income families) (Statistics Bureau, 2011). Therefore, mothers may experience further negative influence on their mental health in addition to ordinary childrearing tasks.
Previous studies conducted in Japan targeted only mothers who cared for children with disabilities and lacked reference subjects, such as mothers of children without disabilities (Yamaguchi et al., 2005, Yatsugi et al., 2013, Toki et al., 2010, Yamaoka et al., 2015). Furthermore, these studies did not consider the possibility of having multiple children with disabilities in a household. Comparison with general childrearing situation is needed to understand the magnitude of mental problems related to raising one or more children with disabilities and to provide specific supporting measurements in addition to general parenting support. Therefore, this study aimed to assess the relationship between raising single or multiple children with disabilities and the mental health of mothers compared mothers of children without disabilities using population-based data in Japan.
2. Method
2.1. Data source
Data for this study, were drawn from the Comprehensive Survey of Living Conditions (CSLC) (The Ministry of Health, 2011), which was conducted by the Ministry of Health, Labour and Welfare in 2010. The CSLC is a nationally representative survey of households that has been conducted every three years since 1986, with smaller annual surveys in the intervals. The CSLC employs a stratified random cluster sampling method based on the Census. The Census in 2005 surveyed 982,000 enumeration districts (EDs) throughout Japan, of which each ED included approximately 50 households. The 2010 CSLC randomly selected 5530 EDs, and all household members in the selected EDs became study subjects, except for individuals who were hospitalized or institutionalized for long periods. The enumerator collected the self-administered questionnaire by visiting all households. The 2010 CSLC surveyed 289,363 households and collected questionnaires from 229,785 households (response rate: 79.4%), which comprised 609,019 household members.
2.2. Study sample
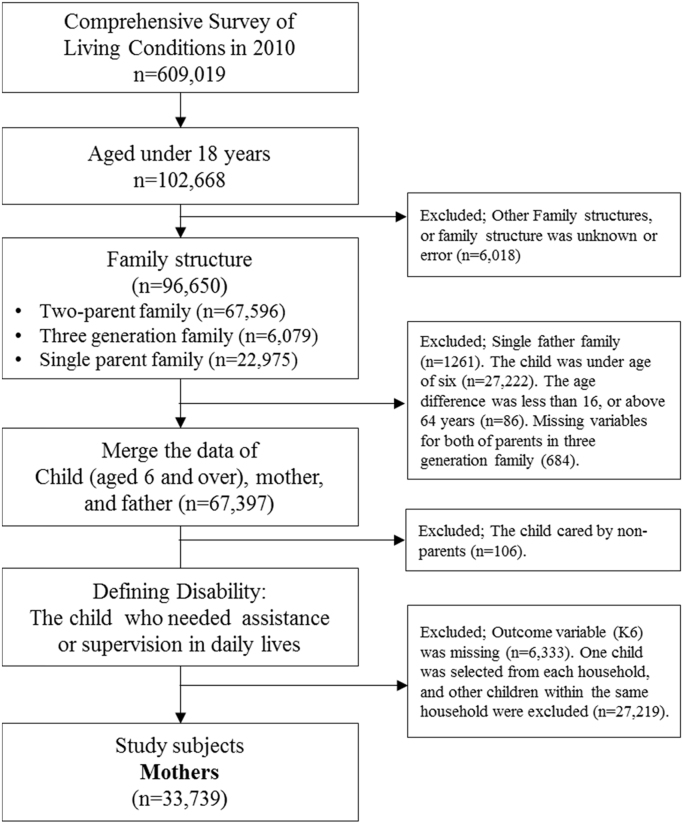
The flow chart (Fig. 1) shows how samples were extracted to determine the study subjects. First, we extracted children who were under the age of 18 from the total CSLC sample (n=102,668). Second, the CSLC coded family structures as two-parent families, three-generation families, families with single mothers, and others. Other types of family structures or households without family structure data were excluded (n=6018) because it was impossible to determine the parent-child relationships in families with several adult couples, single adults, and children living in the same household. There were 96,650 children with three types of family structures. Third, we excluded single-father families (n=1261) because the outcome variable of the study was maternal psychological distress. In addition, this study aimed to compare the households of children with disabilities and those without disabilities. We used the question that inquired about disability status for children aged six and over. The content of this question is explained in the subsection “explanatory variable”. Because of the targeting age in this question, children under the age of six were excluded (n=27,222). Before merging each set of data for the children, mothers, and fathers, we excluded the outliers of age differences—over the age of 64 or under the age of 16 (n=86)—and children without age data for both the mothers and fathers in three-generation families (n=684). In this manner, we merged the data of the children, mothers, and fathers (n=67,379). This study targeted the psychological distress level of mothers who were caring for children with or without disabilities. Therefore, we excluded children with disabilities who were not being cared for by parents (n=106) and mothers without outcome variables (n=6333). Last, we selected one child per household to eliminate the possibility of repeated measures for the same mothers and fathers, and excluded other children from the same household (n=27,219). In households where none of the children had disabilities, the youngest child was selected. In households where all the children had disabilities, the child with the most severe disability was selected. In households where some children did have disabilities and other children did not have disabilities, the child who was the youngest and had a more severe disability was selected. The severity of a child's disability is explained in the subsection “explanatory variable”. Finally, we obtained 33,739 mothers as a study subjects and triads of a child, mother, and father, including 33,110 children without disabilities and 629 children with disabilities.
Fig. 1.
Flow chart of study samples.
2.3. Mental health measures
Maternal mental health was assessed by the Japanese version of the Kessler 6 (K6) scale (Furukawa et al., 2008). The K6 score, a simple screening tool with six items, ranges from 0 to 24 with a 5-point scale (0–4) for each item, and a higher total score indicates more severe mental health conditions. Non-specific psychological distress is the core dimension that people with a wide range of mental disorders have typically experienced (Kessler et al., 2002). Kessler et al. originally developed the K6 to identify non-specific psychological distress among the general population (Kessler et al., 2002, Kessler et al., 2010). Sakurai et al. reported that the optimal cutoff point on K6 was 4/5 for screening mood and anxiety disorders in self-reported questionnaires (sensitivity 100%, specificity 68.7%) using community residents in Japan (Sakurai, Nishi, Kondo, Yanagida & Kawakami, 2011). The present study employed a cutoff point of 4 or 5 and higher in the K6 score to assess non-specific psychological distress because CSLC used a self-administered questionnaire. A K6 score of 5 and higher was coded ‘1’ to express the presence of psychological distress and ‘0’ otherwise.
2.4. Explanatory variables
The child's disability status was an explanatory variable in the current study. To define whether a child had a disability, we used responses to the question that inquired about disability status for children aged six and over: “Does he/she need assistance or supervision?” This question targeted children aged six and over to avoid general parenting assistance or supervision toward infants and preschoolers. Children aged six and over who received a response of “Yes” to this question were operationally categorized as a “child with disability”. The number of children with a disability in the same household was used to assess the extent of association between raising them and maternal psychological distress.
In terms of the severity of disabilities, we utilized a subsequent question from the questionnaire to ask about four levels of the child's dependence in their daily life. The mildest level (Level 1) indicated that a child did have any type of disability but could go out by oneself. Level 2 indicated a child who was independent at home but needed assistance to go out. Level 3 represented a child that needed assistance in their daily life, mainly stayed in bed, and maintained a sitting position. The severest level (Level 4) indicated a child who was bedridden and needed help for all of their daily activities, such as egestion, meals, and changing clothes. The severity of disabilities was used to select one child if there were multiple children in the same household.
2.5. Covariates
Possible covariates were used from the questionnaire, such as the characteristics of a child (sex, age, outpatient visits, activity limitation), parents (age, educational attainment, and working status), and household (family structure, house ownership, number of children, population of city, and monthly household expenditure). The question for the outpatient visits was the following: “Do you currently make regular outpatient visits to hospitals, clinics, Japanese traditional massage therapists, acupuncturists, moxacautery practitioners, Judo orthopedists, or regular home visits by a physician?” If the child visits regularly to any kind of health care facility, the outpatient visits was coded as ‘1’, or otherwise ‘0’. The question for activity limitation was the following: “Have you ever become bedridden or experienced the inability to perform usual activities due to health problems, such as being absent from work or school or not being able to perform housekeeping tasks at least one day during last month?” If the child had answered positively to these conditions at least one day in the last month, the activity limitation was coded as ‘1’ and ‘0’ otherwise. The educational attainment of parents was divided into two categories: high educational attainment indicated graduation from vocational school, technical college, university, or postgraduate school, and low educational attainment indicated graduation from primary school, junior high school, or high school. The working status of parents was coded as ‘1’ for having any type of job and ‘0’ for jobless. The status of having a job included a person who worked and attended school at the same time or worked for a self-owned business. Jobless status indicated a person who attended school or performed household chores without engaging in a job. Family structure was categorized into four groups: family with two parents and child's grandparent(s), family with two parents, family with one parent and child's grandparent(s), and family with one parent (i.e., single mother family). The population of the city was also considered as one of the covariates because living in an urban city might influence maternal psychological distress, and it was divided into two categories with a threshold of 150,000. The total household monthly expenditure was categorized into either below the 25th percentile or the 25th percentile and above after dividing it by the square root of the number of family members to standardize the effect of family size. Below the 25th percentile of total household monthly expenditure was coded as ‘1’ for lower household expenditure and ‘0’ otherwise.
2.6. Statistical analysis
We firstly conducted univariate analysis to describe the associations between covariates and maternal psychological distress. We used Student's t-test for the continuous variables (age), the χ2 test for dichotomous variables (sex, outpatient visits, activity limitation, maternal and paternal educational attainment, working status, family structure, homeownership, lower household expenditure, population of the city), and the Wilcoxon rank sum test for nonparametric variables (number of children without disability in the household).
Secondly, we conducted a multivariable logistic regression to assess the association between the presence and number of children with a disability and maternal psychological distress after controlling for the basic characteristics of the children (age, sex, number of children with a disability). Child's outpatient visits and activity limitation were not included into the multivariable logistic regression because it might mediate the dependent variable. In the next step, we entered confounding factors (maternal educational attainment and working status, house ownership, monthly expenditure, and family structure) into the model. Among family structure, partnered mothers living with the child's grandparent(s) was defined as the reference group. Because the coefficients of correlation between the age of the child and mother, child and father, and mother and father were relatively high (0.66, 0.61, and 0.82), we added only the age of the child as a confounder into the model. Paternal variables were not added to the model because there were single mothers.
Lastly, we stratified into three subgroups: partnered mothers living with grandparent(s), partnered mothers without grandparent(s), and single mothers both of with and without grandparent(s). Multivariable logistic regression was performed among partnered mothers with the confounding factors of the child, mother, household, and also father (i.e., educational attainment and working status). In the multivariable logistic regression for single mothers, we added the variable of co-residence with the child's grandparent(s) instead of paternal variables. The analyses were performed with complete cases for all variables in the models. We used STATA/MP, version 14 (Stata Corp LP, College Station, TX, USA) for all analyses.
3. Results
Table 1 shows the characteristics of the children, households, mothers, and fathers and their associations with maternal psychological distress. One-third of mothers had experienced psychological distress during the last month (n=11,729, 34.7%). Of the 33,739 subjects, 1.8% of mothers (n=594) had one child with a disability, and 0.10% of mothers (n=35) had two children with a disability in their household. The majority of mothers were partnered mothers in two-parent families living without the child's grandparent(s) (68.3%). The proportion of single mothers was 10.5%, including co-residence with grandparent(s) (3.3%) and without co-residence (7.2%). The proportion of mothers having a child with a disability was not significantly different among partnered mothers (1.87%) and single mothers (1.93%). However, the proportion of co-residence with grandparent(s) was significantly lower among families with one or two disabled children (16.2%) compared to families without (24.7%) (p<0.001, these results are not presented in Table 1).
Table 1.
Association between maternal psychological distress (K6 score⩾5) and characteristics of child, mother, father, and household.
| Total (n=33,739) |
K6 score<5 (n=22,010) |
K6 score⩾5 (n=11,729) |
|||||||
| n | (%) | n | (%) | n | (%) | p value for Chi-square test | |||
| Child | Age (range: 6–17) | (mean, SD) | 33,739 | (10.5, 3.5) | 22,010 | (10.4, 3.5) | 11,729 | (10.6, 3.5) | <0.001† |
| (n=33,739) | Sex | Male | 17,223 | 51.0% | 11,208 | 50.9% | 6015 | 51.3% | 0.528 |
| Female | 16,516 | 49.0% | 10,802 | 49.1% | 5714 | 48.7% | |||
| Outpatient visits | No | 26,091 | 80.7% | 17,361 | 82.2% | 8730 | 78.0% | <0.001 | |
| Yes | 6227 | 19.3% | 3758 | 17.8% | 2469 | 22.1% | |||
| Activity limitation | No | 27,826 | 88.8% | 18,416 | 89.9% | 9410 | 86.8% | <0.001 | |
| Yes | 3510 | 11.2% | 2078 | 10.1% | 1432 | 13.2% | |||
| Disability | No | 33,110 | 98.1% | 21,691 | 98.6% | 11,419 | 97.4% | <0.001 | |
| Yes | 629 | 1.9% | 319 | 1.4% | 310 | 2.6% | |||
| Mother | Age (range:23–80) | (mean, SD) | 33,739 | (41.0, 5.8) | 22,010 | (41.0, 5.8) | 11,729 | (41.1, 5.9) | 0.559† |
| (n=33,739) | Education attainmenta | High | 15,601 | 50.3% | 10,446 | 51.5% | 5155 | 47.9% | <0.001 |
| Low | 15,433 | 49.7% | 9820 | 48.5% | 5613 | 52.1% | |||
| Working status | Yes | 23,613 | 70.1% | 15,446 | 70.3% | 8167 | 69.7% | 0.319 | |
| No | 10,085 | 29.9% | 6540 | 29.7% | 3545 | 30.3% | |||
| Father | Age (range: 23–71) | (mean, SD) | 30,179 | (43.5, 6.7) | 20,054 | (43.4, 6.7) | 10,125 | (43.7, 6.8) | <0.001† |
| (n=30,179) | Education attainmenta | High | 13,817 | 49.4% | 9407 | 50.6% | 4410 | 47.0% | <0.001 |
| Low | 14,167 | 50.6% | 9191 | 49.4% | 4976 | 53.0% | |||
| Working status | Yes | 29,355 | 98.1% | 19,584 | 98.5% | 9771 | 97.4% | <0.001 | |
| No | 570 | 1.9% | 305 | 1.5% | 265 | 2.6% | |||
| Household | Two parents with grandparents | 7145 | 21.2% | 4744 | 21.6% | 2401 | 20.5% | <0.001 | |
| (n= 33,739) | Two parents without grandparents | 23,034 | 68.3% | 15,310 | 69.6% | 7724 | 65.9% | ||
| Single parent with grandparents | 1119 | 3.3% | 687 | 3.1% | 432 | 3.7% | |||
| Single parent without grandparents | 2441 | 7.2% | 1269 | 5.8% | 1172 | 10.0% | |||
| House ownership | No | 8529 | 25.3% | 5199 | 23.6% | 3330 | 28.4% | <0.001 | |
| Yes | 25,210 | 74.7% | 16,811 | 76.4% | 8399 | 71.6% | |||
| Number of children | (median, IQR) | 33,739 | (2, 1–2) | 22,010 | (2, 1–2) | 11,729 | (2, 1–2) | 0.012‡ | |
| (range) | (1–13) | (1–13) | (1–10) | ||||||
| Number of children with disability | None | 33,110 | 98.1% | 21,691 | 98.6% | 11,419 | 97.4% | <0.001 | |
| One | 594 | 1.8% | 305 | 1.4% | 289 | 2.5% | |||
| Two | 35 | 0.10% | 14 | 0.06% | 21 | 0.18% | |||
| Population of city | <150,000 | 16,756 | 49.7% | 10,882 | 49.4% | 5874 | 50.1% | 0.263 | |
| ⩾150,000 | 16,983 | 50.3% | 11,128 | 50.6% | 5855 | 49.9% | |||
| Monthly expenditureb | ⩾25%tile | 24,580 | 76.2% | 16,079 | 76.3% | 8501 | 75.9% | 0.446† | |
| <25%tile | 7687 | 23.8% | 4992 | 23.7% | 2695 | 24.1% | |||
χ^2 test.
t-test.
Wilcoxson rank sum test.
High education attainment is for person graduated from university, college, or vocational school. Low educational attainment is for person graduated from junior high school or high school.
Monthly expenditure was divided by the square root of number of persons in the household.Missing value: Outpatient visit (n= 1421), Activity limitation (n=2403), Maternal educational attainment (n=2705), Maternal working status (n=41), Paternal educational attainment (n=2195), Paternal working status (n=254), and Monthly Expenditure (n=1472).
Table 2 shows the multivariable logistic regression analysis for the psychological distress of mothers. Raising a child with a disability was significantly associated with maternal psychological distress (crude odds ratio (OR) 1.78, 95% confidence interval (95%CI) 1.51-2.09 for one child with a disability; OR 2.90, 95%CI 1.47-5.70 for two children with a disability). After controlling for the characteristics of the mother and household, the adjusted OR (AOR) was still significantly associated (AOR 1.72, 95%CI 1.44-2.05 for one child with a disability; AOR 2.85, 95%CI 1.28-6.34 for two children with a disability).
Table 2.
The relationship between having a child with a disability and maternal psychological distress.
| All mothers | All mothers | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
n=33,769 |
n=29,868 |
||||||||
| OR | 95%CI | OR | 95%CI | ||||||
| Child with disability | Age | 1.02 | 1.01–1.03 | 1.02 | 1.01–1.03 | ||||
| Male | 1.01 | 0.96–1.06 | 1.01 | 0.97–1.06 | |||||
| One child with disability at home | 1.78 | 1.51–2.09 | 1.72 | 1.44–2.05 | |||||
| Two children with disability at home | 2.90 | 1.47–5.70 | 2.85 | 1.28–6.34 | |||||
| Mother | Low education attainment | 1.11 | 1.05–1.16 | ||||||
| Not working | 1.06 | 1.01–1.12 | |||||||
| Household | Number of children without disability | 1.003 | 0.98–1.03 | ||||||
| Have house ownership | 0.83 | 0.78–0.89 | |||||||
| Lower household expenditure | 0.98 | 0.93–1.04 | |||||||
| Family structurea | Partnered mothers without grandparents | 0.97 | 0.91–1.03 | ||||||
| Single mother with grandparents | 1.20 | 1.04–1.38 | |||||||
| Single mother only | 1.60 | 1.44–1.79 | |||||||
The numbers of object were changed due to complete-case analyses.
Reference: Partnered mothers with grandparents
Table 3 shows the stratified analyses among the three subgroups of mothers. Among partnered mothers living with grandparent(s), the proportions of having one child or two children with disability were 87 (1.4%) and 3 (0.048%). Raising a child with a disability was not significantly associated with psychological distress (AOR, 95%CI: 1.34, 0.84-2.13). The odds ratio for having two children with a disability could not be obtained due to the small sample size of the explanatory variable. Among partnered mothers living without grandparent(s), 446 mothers had one child (2.2%) and 24 mothers had two children with a disability (0.12%). The AOR remained 1.80, with significance (95%CI: 1.47–2.21), for one child, and 2.84 for two children with a disability (95%CI: 1.14–7.07). Among single mothers, 61 mothers had one child with a disability (2.0%), and eight mothers had two children with a disability (0.26%). Raising one or two children with a disability was not significantly associated with psychological distress (AOR, 95%CI: 1.42, 0.81–2.47 for one child; 4.43, 0.51–38.7 for two children with a disability).
Table 3.
The relationship between having a child with a disability and maternal psychological distress by family structure.
| Partnered mothers with grandparents | Partnered mothers without grandparents | Single mothers | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
n= 6214 |
n= 20,362 |
n= 3043 |
|||||||||||
| OR | 95%CI | OR | 95%CI | OR | 95%CI | ||||||||
| Child with disability | Age | 1.02 | 1.01–1.04 | 1.02 | 1.01–1.03 | 0.98 | 0.96–1.001 | ||||||
| Male | 1.04 | 0.94–1.16 | 1.03 | 0.97–1.10 | 0.87 | 0.76–1.01 | |||||||
| One child with disability at home | 1.34 | 0.84–2.13 | 1.80 | 1.47–2.21 | 1.42 | 0.81–2.47 | |||||||
| Two children with disability at home | – | – | 2.84 | 1.14–7.07 | 4.43 | 0.51–38.7 | |||||||
| Mother | Low education attainment | 1.08 | 0.96–1.21 | 1.06 | 0.99–1.13 | 1.05 | 0.90–1.22 | ||||||
| Not working | 1.10 | 0.97–1.26 | 1.03 | 0.97–1.10 | 1.71 | 1.38–2.12 | |||||||
| Father | Low education attainment | 1.05 | 0.93–1.17 | 1.13 | 1.06–1.20 | ||||||||
| Not working | 1.55 | 1.09–2.19 | 1.75 | 1.41–2.16 | |||||||||
| Household | Number of children without disability | 1.02 | 0.96–1.08 | 1.01 | 0.98–1.03 | 0.94 | 0.86–1.03 | ||||||
| Have house ownership | 0.78 | 0.56–1.08 | 0.87 | 0.82–0.93 | 0.67 | 0.56–0.80 | |||||||
| Lower household expenditure | 0.91 | 0.80–1.03 | 0.96 | 0.89–1.04 | 1.06 | 0.91–1.23 | |||||||
| Living with grandparents | 0.83 | 0.69–1.00 | |||||||||||
The numbers of object were changed due to complete-case analyses.
4. Discussion
To the best of our knowledge, this study was the first to report a significant association between raising a child with a disability and maternal psychological distress compared to mothers of children without disabilities based on a nationwide survey in Japan. In addition, the risk for psychological distress of mothers differed among family structures.
4.1. Raising a child with a disability compared to raising a healthy child
In Table 2, raising a child with a disability was significantly related to maternal psychological distress after controlling for confounding factors. Lee (2013) reported a literature review of 28 studies that examined the stress levels, well-being, and sleep problems of mothers of children with developmental disabilities. Five studies compared the differences between mothers of children with disabilities and children with typical development (Bourke-Taylor et al., 2012, Eisenhower et al., 2005, Estes et al., 2009, Gray et al., 2011, Montes and Halterman, 2007). Among them, only one study, conducted by Montes and Halterman (2007), used population-based study subjects in the United States and reported that mothers of children with autism were twice as likely to experience poorer mental health than mothers of children without autism (OR, 95%: 2.42, 1.31-4.45) after controlling for the child’s social skills and demographic background. In addition, Brehaut et al. (2009). reported that the caregivers of children with health problems were more likely to experience depressive symptoms (OR, 95%: 2.48, 1.40–4.40) compared to the caregivers of healthy children according to population-based data in Canada after controlling for the characteristics of the child, mother, and household. The current study found a smaller point estimate (AOR, 95%CI: 1.72, 1.44–2.05) for one child with a disability compared to previous population-based studies. The possible reasons were that we could not sufficiently control for the children's behavior or social skills variables and lacked a clear definition of the child's disability, such as a clinical diagnosis. The survey used in this study was originally not aimed to examine child's disability and caregiving situations. Adequate variables are needed to evaluate the conditions of children and parents in a nationwide survey to target caregivers in Japan.
Having two children with a disability resulted in an elevated point estimate (AOR, 95%CI: 2.85, 1.28–6.34). The present study revealed a gradient relationship between increase numbers of children with a disability and maternal mental health compared to the mothers of children who did not need constant care in Japan. Being a single parent had an independent effect on maternal psychological distress, as shown in Table 2; however, the effect of having a child with a disability remained after adjusting for the family composition. Therefore, it is important for health professionals to focus on the mental health of every mother of a child with a disability and to assess their needs for psychological support.
4.2. Differences according to family structure
Previous study reported that single mothers experienced poorer mental health compared to partnered mothers(Cairney, Boyle, Offord & Racine, 2003; Colton, Janzen & Laverty, 2015). It was consistent with this study shown in Table 2. Single mother was 1.60 times likely to experience psychological distress compared to partnered mothers with grandparent(s). After stratified analyses in Table 3, the mothers in two-parent families showed significant associations with having one or two children with a disability and psychological distress. However, there were no significant associations between mothers in three generation family and single mothers. For one reason, this might be due to the small number of children with disabilities. In this study, 446 mothers had one child with a disability and 24 mothers had two children with a disability among two-parent families. Among two-parent families living with child's grandparents, 87 mothers had one child with a disability, but only three mothers had two children with a disability. Among single mothers, 61 mothers had one child and eight mothers had two children with a disability. Since the stratified analyses led to small numbers of explanatory variable, we could not obtain statistical significance between maternal psychological distress and the increase numbers of children with disability in comparison with other children. Further research should include larger number of children with a disability to compare maternal mental health in detailed familial situations, such as using multiple years of data from CSLC.
In terms of family structure, this study showed similar proportions of single mother among children with a disability (11.0%) and children without a disability (10.5%). According to nationwide researches, the proportion of single parenthood was higher among children with a disability or health problems compared to other children in Canada (22.5% vs 16.3%) (Brehaut et al., 2009), UK (34.1% vs 25.6%) (Blackburn, Spencer & Read, 2010), and US (47.3-60.1% vs 41.5-49.1%) (Szilagyi et al., 2003). On the other hand, co-residence with grandparent(s) was significantly lower when a child had a disability (16.2%) compared to a child without disability (24.7%) in Japan. Traditionally, the proportion of elderly people living with their adult children is much higher than in Western countries, which is approximately 40% among households with elderly in Japan (The Ministry of Health Labour and Welfare, 2013, Kono, 2000). However, the tradition of intergenerational co-residence has been decreasing due to social and economic changes, such as the increase in women's educational attainment and employment (Kono, 2000). Therefore, it is important to assess the mental health of single or partnered mothers who have a child with a disability and do not live with children's grandparents.
4.3. Limitations and further implications
The present study had several limitations. First, this study was a cross-sectional study that did not reveal the causal mechanism between the child's disability and the mental health of mothers. Careful considerations are needed to interpret results in this study. Raina et al. (2004). suggested a multidimensional model that included not only a single relationship but also multiple relationships between caregivers’ health and burden of care for children with a disability. According to that model, as a possible underlying mechanism, children's impairment is related to caregiving demands and perceptions for formal care services and the self-perception of caregivers. Further research is needed to include variables of the children's detailed health conditions, perceptions of caregivers, service utilization, social support, and actual childrearing situations, such as paternal involvement in child care, to examine the mechanisms of the relationships between maternal mental health and a child's disability. In terms of practical implications, health professionals should assess the health conditions of the caregivers and provide advice for the use of a formal care service to cope with their needs and to eliminate psychological distress.
Second, the definition of disability in this study assessed the care-needed status using functional impairment. It was originally developed for the elderly, closely correlated with the functional independence measure (FIM), and widely used for certification of long-term care for the elderly (Tsuboi, Murakami, Kurumadani, Shimizu, and Fujiwara (2002)). The impairment is one of important concept in the International Classification of Functioning, Disability, and Health (ICF) (World Health Organization, 2001) in despite of medical diagnosis for disorders or diseases. The variable of activity limitation used in this study represented whether the child had an experience of being bedridden or absent from school during last month. We did not employ the activity limitation to define disability status of children because it might reflect acute conditional changes rather than usual chronic conditions. Therefore, the operational definition in this study targeted broad range of non-specific disability status, such as developmental disabilities, intellectual delays, or physical impairment. One systematic research (van der Lee, Mokkink, Grootenhuis, Heymans and Offringa (2007)) reported there was no international consensus about the definition of chronic health conditions in childhood. For example, previous studies (Brehaut et al., 2009, Kohen et al., 2007;) used broad inclusion criteria using activity limitations, functional problems, clinical diagnoses, or elevated service use. The children we targeted in this study required care in addition to general parenting care. Caregivers of children with health problems experience common challenges and life experiences in despite of the specific diagnosis (Kohen et al., 2007). Further research is needed to use the various criteria as previous studies to broadly evaluate maternal mental health and children's health conditions. In addition, we excluded children younger than six because the survey asked only about children aged six and over to define the disability. Further research should examine the situation among mothers of younger children with and without disabilities.
Third, we performed a complete case analysis in multiple logistic regressions. The numbers of objects in Table 2, Table 3 decreased due to missing values. The proportions of missing values ranged from 0.1% to 8.0% for the variables of maternal and paternal educational attainment, working status, and monthly expenditure. We could not employ multiple imputation methods because of the data merging process (i.e., single mothers lacked all paternal variables). There is a possibility that bias exists because the confounders were not adequately controlled and we assessed specific characteristics which only appeared among subjects with complete answers to questions. The next analysis will consider more statistical methods, including multiple imputation and data linkage.
Lastly, we compared the differences among mothers living with a partner, a partner and grandparents, or alone. However, we excluded other types of family structures due to the inability to define the child-parent relationships in complicated families, i.e., several married couples and unmarried adults living together with several children. The socioeconomic situation and social support among them may be different from that of typical two-parent, single-parent, or three-generation families. A sophisticated strategy is needed to define the child-parent relationships within the household survey in future studies.
5. Conclusion
This study reported the significant association between raising a child with a disability and maternal psychological distress in comparison to mothers who raised a child without disability using a population-based survey in Japan. The association of raising a child with a disability and maternal mental health varied according to the number of children with a disability and the family composition. Attentions should be paid to not only single mothers but also partnered mothers in two-parent families who have a child with a disability. It is important for health professionals to focus on the mental health of every mothers of a child with a disability in different family structures, and to assess their needs for psychological support.
Acknowledgments
We would like to thank the members of the Department of Health Services Research, the University of Tsukuba, and the co-authors for their contribution to the data collection, the data analysis process and their help with drafting this manuscript. This study was supported by the Ministry of Health, Labour and Welfare (H27-seisaku-senryaku-012).
References
- Blackburn C.M., Spencer N.J., Read J.M. Prevalence of childhood disability and the characteristics and circumstances of disabled children in the UK: secondary analysis of the family resources survey. BMC Pediatrics. 2010;10:21. doi: 10.1186/1471-2431-10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourke J., Ricciardo B., Bebbington A., Aiberti K., Jacoby P., Dyke P.…Leonard H. Physical and mental health in mothers of children with Down syndrome. The Journal of pediatrics. 2008;153(3):320–326. doi: 10.1016/j.jpeds.2008.02.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourke-Taylor H., Pallant J.F., Law M., Howie L. Predicting mental health among mothers of school-aged children with developmental disabilities: the relative contribution of child, maternal and environmental factors. Research in Developmental Disabilities. 2012;33(6):1732–1740. doi: 10.1016/j.ridd.2012.04.011. [DOI] [PubMed] [Google Scholar]
- Brehaut J.C., Kohen D.E., Garner R.E., Miller A.R., Lach L.M., Klassen A.F. Health among caregivers of children with health problems: findings from a Canadian population-based study. American Journal of Public Health. 2009;99(7):1254–1262. doi: 10.2105/AJPH.2007.129817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brehaut J.C., Kohen D.E., Raina P., Walter S.D., Russell D.J., Swinton M.…Rosenbaum P. The health of primary caregivers of children with cerebral palsy: how does it compare with that of other Canadian caregivers? Pediatrics. 2004;114(2):e182–e191. doi: 10.1542/peds.114.2.e182. [DOI] [PubMed] [Google Scholar]
- Cairney J., Boyle M., Offord D.R., Racine Y. Stress, social support and depression in single and married mothers. Social Psychiatry and Psychiatric Epidemiology. 2003;38(8):442–449. doi: 10.1007/s00127-003-0661-0. [DOI] [PubMed] [Google Scholar]
- Colton T., Janzen B., Laverty W. Family structure, social capital, and mental health disparities among Canadian mothers. Public Health. 2015;129(6):639–647. doi: 10.1016/j.puhe.2015.03.023. [DOI] [PubMed] [Google Scholar]
- Eisenhower A.S., Baker B.L., Blacher J. Preschool children with intellectual disability: syndrome specificity, behaviour problems, and maternal well-being. Journal of Intellectual Disability Research. 2005;49(Pt 9):657–671. doi: 10.1111/j.1365-2788.2005.00699.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estes A., Munson J., Dawson G., Koehler E., Zhou X.H., Abbott R. Parenting stress and psychological functioning among mothers of preschool children with autism and developmental delay. Autism : The International Journal of Research and Practice. 2009;13(4):375–387. doi: 10.1177/1362361309105658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estes A., Olson E., Sullivan K., Greenson J., Winter J., Dawson G. Parenting-related stress and psychological distress in mothers of toddlers with autism spectrum disorders. Brain Development. 2013;35(2):133–138. doi: 10.1016/j.braindev.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferro M.A., Speechley K.N. Depressive symptoms among mothers of children with epilepsy: a review of prevalence, associated factors, and impact on children. Epilepsia. 2009;50(11):2344–2354. doi: 10.1111/j.1528-1167.2009.02276.x. [DOI] [PubMed] [Google Scholar]
- Furukawa T.A., Kawakami N., Saitoh M., Ono Y., Nakane Y., Nakamura Y.…Kikkawa T. The performance of the Japanese version of the K6 and K10 in the world mental health survey Japan. International Journal of Methods in Psychiatric Research. 2008;17(3):152–158. doi: 10.1002/mpr.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray K.M., Piccinin A.M., Hofer S.M., Mackinnon A., Bontempo E.D., Einfeld S.L.…Tonge B.J. The longitudinal relationship between behavior and emotional disturbance in young people with intellectual disability and maternal mental health. Research in Developmental Disabilities. 2011;32(3):1194–1204. doi: 10.1016/j.ridd.2010.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J., Hiripi E., Mroczek D.K., Normand S.L.…Zaslavsky A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Green J.G., Gruber M.J., Sampson N.A., Bromet E., Cuitan M.…Zaslavsky A.M. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO world mental health (WMH) survey initiative. International Journal of Methods in Psychiatric Research. 2010;19(Suppl 1):S4–S22. doi: 10.1002/mpr.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohen D.E., Brehaut J.C., Garner R.E., Miller A.R., Lach L.M., Klassen A.F. Conceptualizing childhood health problems using survey data: a comparison of key indicators. BMC Pediatrics. 2007;7:40. doi: 10.1186/1471-2431-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kono M. The impact of modernisation and social policy on family care for older people in Japan. Journal of Social Policy. 2000;29(2):181–203. [Google Scholar]
- Lee J. Maternal stress, well-being, and impaired sleep in mothers of children with developmental disabilities: a literature review. Research in Developmental Disabilities. 2013;34(11):4255–4273. doi: 10.1016/j.ridd.2013.09.008. [DOI] [PubMed] [Google Scholar]
- van der Lee J.H., Mokkink L.B., Grootenhuis M.A., Heymans H.S., Offringa M. Definitions and measurement of chronic health conditions in childhood: a systematic review. JAMA. 2007;297(24):2741–2751. doi: 10.1001/jama.297.24.2741. [DOI] [PubMed] [Google Scholar]
- McLennan J.D., Kotelchuck M. Parental prevention practices for young children in the context of maternal depression. Pediatrics. 2000;105(5):1090–1095. doi: 10.1542/peds.105.5.1090. [DOI] [PubMed] [Google Scholar]
- Minkovitz C.S., Strobino D., Scharfstein D., Hou W., Miller T., Mistry K.B. Maternal depressive symptoms and children’s receipt of health care in the first 3 years of life. Pediatrics. 2005;115(2):306–314. doi: 10.1542/peds.2004-0341. [DOI] [PubMed] [Google Scholar]
- Montes G., Halterman J.S. Psychological functioning and coping among mothers of children with autism: a population-based study. Pediatrics. 2007;119(5):e1040–e1046. doi: 10.1542/peds.2006-2819. [DOI] [PubMed] [Google Scholar]
- Montes G., Halterman J.S. Association of childhood autism spectrum disorders and loss of family income. Pediatrics. 2008;121(4):e821–e826. doi: 10.1542/peds.2007-1594. [DOI] [PubMed] [Google Scholar]
- Montes G., Halterman J.S. Child care problems and employment among families with preschool-aged children with autism in the United States. Pediatrics. 2008;122(1):e202–e208. doi: 10.1542/peds.2007-3037. [DOI] [PubMed] [Google Scholar]
- Nes R.B., Hauge L.J., Kornstad T., Kristensen P., Landolt M.A., Eskedal L.T.…Vollrath M.E. The impact of child behaviour problems on maternal employment: a longitudinal cohort study. Journal of Family and Economic Issues. 2014;35:351–361. doi: 10.1007/s10834-013-9378-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parish S.L., Rose R.A., Dababnah S., Yoo J., Cassiman S.A. State-level income inequality and family burden of U.S. families raising children with special health care needs. Social Science Medicine (1982) 2012;74(3):399–407. doi: 10.1016/j.socscimed.2011.10.035. [DOI] [PubMed] [Google Scholar]
- Raina P., O’Donnell M., Rosenbaum P., Brehaut J., Walter S.D., Russell D.…Wood E. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. 2005;115(6):e626–e636. doi: 10.1542/peds.2004-1689. [DOI] [PubMed] [Google Scholar]
- Raina P., O’Donnell M., Schwellnus H., Rosenbaum P., King G., Brehaut J.…Wood E. Caregiving process and caregiver burden: conceptual models to guide research and practice. BMC Pediatrics. 2004;4:1. doi: 10.1186/1471-2431-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakurai K., Nishi A., Kondo K., Yanagida K., Kawakami N. Screening performance of K6/K10 and other screening instruments for mood and anxiety disorders in Japan. Psychiatry and Clinical Neurosciences. 2011;65(5):434–441. doi: 10.1111/j.1440-1819.2011.02236.x. [DOI] [PubMed] [Google Scholar]
- Schwebel D.C., Brezausek C.M. Chronic maternal depression and children’s injury risk. Journal of Pediatric Psychology. 2008;33(10):1108–1116. doi: 10.1093/jpepsy/jsn046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen H., Magnusson C., Rai D., Lundberg M., Lê-Scherban F., Dalman C. Associations of parental depression with child school performance at age 16 years in Sweden. JAMA Psychiatry. 2016;73(3):239–246. doi: 10.1001/jamapsychiatry.2015.2917. [DOI] [PubMed] [Google Scholar]
- Statistics Bureau, Ministry of Internal Affairs and Communications. 2011 Survey on Time Use and Leisure Activities (Table 14). 2012; 〈http://www.stat.go.jp/data/shakai/2011/gaiyou.htm〉. Accessed 03.08.16.
- Szilagyi P.G., Shenkman E., Brach C., LaClair B.J., Swigonski N., Dick A.…Lewit E.M. Children with special health care needs enrolled in the State Children’s Health Insurance Program (SCHIP): patient characteristics and health care needs. Pediatrics. 2003;112(6 Pt 2):e508. [PubMed] [Google Scholar]
- The Ministry of Health Labour and Welfare. Comprehensive Survey of Living Conditions (2010). 2011; 〈http://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa10/dl/gaikyou.pdf〉. Accessed 30.03.15.
- The Ministry of Health Labour and Welfare. Comprehensive Survey of Living Conditions (2013). 2013; 〈http://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa13/index.html〉 Accessed 03/08, 2016.
- The Ministry of Health Labour and Welfare. Longitudinal Survey of Newborns in the 21st Century (2010 Cohort). 2012; 〈http://www.mhlw.go.jp/toukei/saikin/hw/shusshoujib/01/index.html〉. Accessed 06/11, 2016.
- Toki M., Washio M., Furukawa A., Narita H., Yokogushi K., Ishiai S. Investigating parental caregiver burden for children with disabilities using a Japanese version of the Zarit Caregiver Burden Interview (J-ZBI) Japanese Journal of Rehabilitation Medicine. 2010;47:396–404. [Google Scholar]
- Tsuboi A., Murakami T., Kurumadani H., Shimizu J., Fujiwara N. Relationship between criteria for evaluating the degree of independence of deisabled elderly persons in perfoming activities of daily living. The Journal of Japanese Occupational Therapy Association. 2002;21(5):455–462. [Google Scholar]
- World Health Organization (2001). International Classification of Functioning, Disability and Health: ICF. 〈http://psychiatr.ru/download/1313?view=name=CF_18.pdf〉 Accessed 28.07.16.
- Yamaguchi S., Takataya K., Ogiwara T. Study of mental health and its related factors including burden on caregivers of children/persons with severe motor and intellectual disabilities. Yamanashi Nursing Journal. 2005;4(1):41–47. [Google Scholar]
- Yamaoka Y., Tamiya N., Moriyama Y., Sandoval Garrido F.A., Sumazaki R., Noguchi H. Mental health of parents as caregivers of children with disabilities: based on Japanese nationwide survey. PloS One. 2015;10(12):e0145200. doi: 10.1371/journal.pone.0145200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yatsugi S., Suzukamo Y., Izumi S. Productive social activities in mothers of intellectually disabled children moderate the relationship between caregiver burden and self-rated health. [Nihon koshu eisei zasshi] Japanese Journal of Public Health. 2013;60(7):387–395. [PubMed] [Google Scholar]