Abstract
Popliteal artery entrapment syndrome is a rare cause of peripheral vascular disease, often affecting young adults. Multiple studies have shown that osteochondromas can cause vascular injury. Intermittent compression, pseudoaneurysm, thrombosis, distal embolism, and venous thrombosis have all been described as possible complications. Here we present a case of popliteal arterial entrapment type IV with an associated tibial osteochondroma.
Osteochondromas or exostoses are benign bone tumors that arise from the metaphysis of growth plates. These lesions are typically asymptomatic and found incidentally during adolescence or childhood. Osteochondromas may occur as solitary lesions or as familial multiple hereditary osteochondromas. Most often, the distal femur, proximal humerus, and proximal tibia are involved. The cartilaginous cap of this tumor is soft and pliable; however, over time, it will ossify, becoming rigid and firm. This bone protuberance can then cause vascular complications that include pseudoaneurysm, thrombosis, and popliteal entrapment.1, 2, 3 Here we describe a case of type IV popliteal artery entrapment syndrome (PAES), defined as the presence of the axial popliteal artery deep to the popliteus muscle or fibrous bands, that caused arterial thrombosis associated with a tibial osteochondroma. Informed consent for publication of this case report was obtained.
Case report
A 27-year-old man complaining of a several-month history of right lower extremity coolness was seen by his primary care physician. He works as a farmer and does not participate in long-distance running or heavy exercise; however, he tends his fields on the farm and commonly squats to milk cows. The patient stated that approximately 10 days before presentation, he developed pain in his right foot with walking, along with progressively increased coolness in his right leg. Before this acute foot claudication, he noticed that while sleeping, he would develop pain in his right foot as well. With this worsening pain and concern with the temperature change, he presented to his primary care physician for evaluation.
On physical examination, he was found to have a cool right lower extremity and no palpable dorsalis pedis or posterior tibial arterial pulses. Doppler examination produced a faint monophasic posterior tibial signal. No sensory deficits were noted on examination. Computed tomography showed a patent popliteal artery with occlusion of the anterior tibial artery just above the ankle joint, along with occlusion of the peroneal and posterior tibial arteries at the midcalf and an incidental pedunculated osteochondroma arising from the right proximal medial tibia. The patient was then referred to a vascular surgeon for evaluation. There were increased velocities noted on the duplex ultrasound evaluation with provocative maneuvers in the proximal tibial vessels and occlusion of the distal tibial vessels. With the patient's occlusion of his infrapopliteal vessels, angiography was recommended with potential for therapeutic thrombolysis.
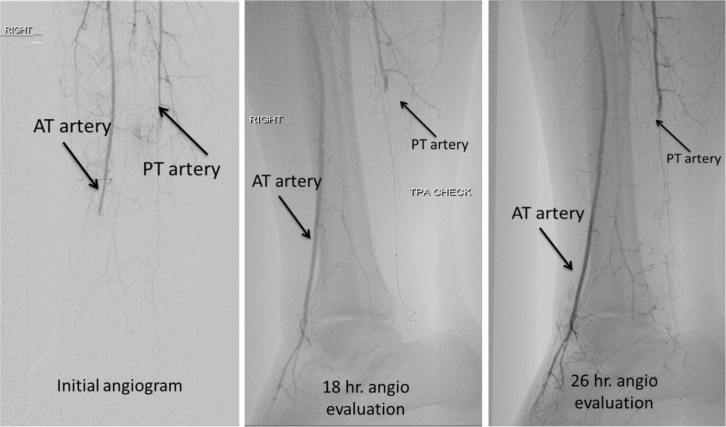
The patient underwent angiography, which again demonstrated the occlusion of the anterior tibial, posterior tibial, and peroneal arteries. Catheters were then delivered to the anterior tibial and posterior tibial arteries to allow tissue plasminogen activator infusion (Fig 1). To rule out proximal embolization as a source of the embolization, cardiac evaluation was performed. Transthoracic and transesophageal echocardiography did not demonstrate any valvular masses, vegetations, or intracardiac thrombi, and there were no shunts. Results of hematology hypercoagulable laboratory workup, including antiphospholipid antibody, lupus anticoagulant, and cardiolipin antibody, were negative. On an 18-hour and 26-hour angiogram, after beginning of the arterial lysis, the posterior tibial artery remained occluded, and the anterior tibial artery opened up with good flow into the dorsalis pedis (Fig 1). With the posterior tibial artery remaining occluded in spite of increased dose, lysis was stopped, and the patient was started on anticoagulation. Further imaging was performed to look for potential causes of thrombosis.
Fig 1.
Left, Initial angiogram with occluded anterior tibial (AT), posterior tibial (PT), and dorsalis pedis arteries. Center, The 18-hour angiogram shows reconstitution of flow in AT and dorsalis pedis arteries. TPA, Tissue plasminogen activator. Right, The 26-hour angiogram shows continued occlusion of the PT artery.
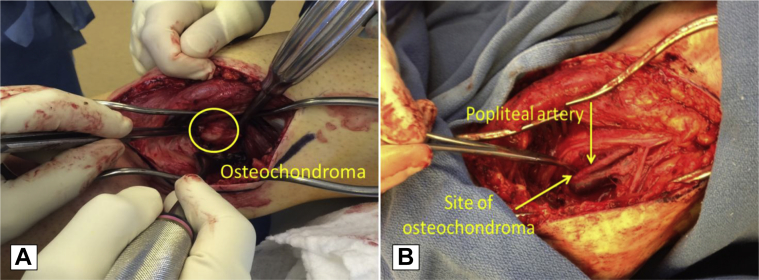
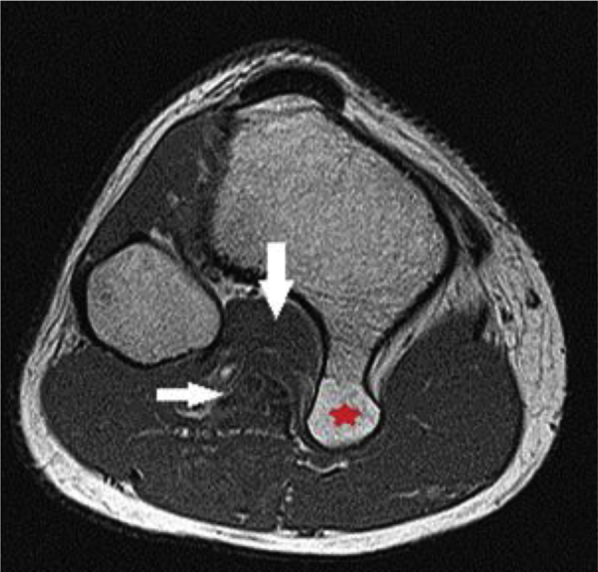
The patient underwent magnetic resonance angiography (MRA) with active dorsiflexion and plantar flexion to evaluate for potential popliteal entrapment as the patient's pulse would diminish with plantar flexion. There was evidence of a popliteal vein wall thickening. This lesion had significant mass effect on the adjacent medial gastrocnemius and popliteus muscles, creating a relatively crowded appearance of the neurovascular bundle in the intermuscular region between the lateral gastrocnemius and popliteus muscles (Fig 2). With the active maneuvers performed, there was no evidence of compression; however, with the patient's history and physical examination findings of diminished Doppler signals with plantar flexion, it was suspected that certain activities would cause compartment compression secondary to the osteochondroma. The patient was referred to an orthopedic surgeon for resection of the pedunculated osteochondroma. The patient underwent operative exploration with resection of the osteochondroma and also release of fibrous bands that arose from the popliteus muscle extending across the popliteal artery, confirming the type IV popliteal arterial entrapment (Fig 3). Postoperatively, he had no symptoms of claudication or rest pain with a palpable dorsalis pedis pulse and a Doppler signal of the posterior tibial artery from retrograde flow.
Fig 2.
Cross-sectional magnetic resonance angiography (MRA) of the right knee shows the tibial osteochondroma (star); right arrow, popliteal vessels; down arrow, popliteus muscle.
Fig 3.
Intraoperative image showing the popliteal fossa before (A) and after (B) resection of the osteochondroma.
Discussion
PAES was first described by Stuart in 1879 as a variation of the course of the popliteal artery.4 PAES evolves from an embryologic development whereby there is growth of the popliteal artery with union of the superficial popliteal artery and its lower segment, along with the growth of the gastrocnemius muscles. During embryologic development, the popliteal artery will have two segments; one passes anterior and one posterior to the popliteus muscle. The posterior segment then will typically regress and allow the growth of the anterior popliteal artery, thus preventing compression.5 At this same time, the gastrocnemius muscles are migrating toward their final attachments on the lateral and medial epicondyles of the femur. Gibson et al5 described anomalous patterns in which the popliteal grew through the medial heads of the gastrocnemius, causing compression, from postmortem studies. In our patient, there were fibrous bands from the popliteus muscle and osteochondroma. This correlated with a type IV popliteal entrapment.
To date, multiple studies have looked at vascular complications from osteochondromas, including intermittent compression, pseudoaneurysm, thrombosis, distal emboli, and venous thrombosis or compression.1, 2, 3, 6, 7, 8, 9, 10, 11, 12, 13, 14 Enlargement of the osteochondroma can lead to compression of the vascular structures, leading to arterial or venous thrombus with subsequent distal embolization. Eschelman et al7 found that 68% of vascular injuries were pseudoaneurysms secondary to what has been proposed as the osteochondroma's cartilaginous cap ossifying and then the pulsatile nature of the artery rubbing against it, causing damage. Thrombosis or distal embolism occurred in 4.5% to 13% of patients.1, 7 The vascular structures of the popliteal fossa are tethered proximally at Hunter canal and distally at the trifurcation, leading to limited mobility. Osteochondromas can cause displacement and damage to the vessel walls, leading to complications due to the limited mobility of the vascular structures.
In our patient, the osteochondroma in association with the popliteus muscle fibrous bands caused entrapment with thrombosis. With young patients who present with vascular problems, a high index of suspicion is needed because of the potential devastating complications that may occur. A thorough workup is necessary as young patients do not have the typical atherosclerotic risk factors. When PAES is suspected, MRA with provocative flexion and extension maneuvers can be done to elicit compression. Sensitivity of provocative magnetic resonance imaging or MRA is 94%, and provocative arteriography has 97% sensitivity.5 Although these tests are sensitive, they are not 100% sensitive; therefore, patients may have PAES and not demonstrate it on such provocative maneuvers, as our patient did. Thus, as stated, when seeing a young patient with vascular insult, you must have a high index of suspicion for PAES.
From the Midwestern Vascular Surgical Society
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Vaseur M.A., Fabre O. Vascular complications of osteochondromas. J Vasc Surg. 2000;31:532–538. [PubMed] [Google Scholar]
- 2.Holzapfel B.M., Seppel G., Wagner R., Kenn W., Meffert R. Popliteal entrapment syndrome caused by fibular osteochondroma. Ann Vasc Surg. 2011;25:982.e5–982.e10. doi: 10.1016/j.avsg.2011.02.044. [DOI] [PubMed] [Google Scholar]
- 3.Guy N.J., Shetty A.A., Gibb P.A. Popliteal artery entrapment syndrome: an unusual presentation of a fibular osteochondroma. Knee. 2004;11:497–499. doi: 10.1016/j.knee.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 4.Anderson Stuart T.P. Note on a variation in the course of the popliteal artery. J Anat Physiol. 1879;13(Pt 2):162. [PMC free article] [PubMed] [Google Scholar]
- 5.Gibson M.H., Mills J.G., Johnson G.E., Downs A.R. Popliteal entrapment syndrome. Ann Surg. 1977;185:341–348. doi: 10.1097/00000658-197703000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Henry J.C., Mouawad N.J., Phieffer L., Go M.R. Tibial osteochondroma inducing popliteal artery compression. J Vasc Surg. 2015;61:1595–1598. doi: 10.1016/j.jvs.2013.10.105. [DOI] [PubMed] [Google Scholar]
- 7.Eschelman D.J., Gardiner G.A., Deely D.M. Osteochondroma: an unusual cause of vascular disease in young adults. J Vasc Interv Radiol. 1995;6:605–613. doi: 10.1016/s1051-0443(95)71144-7. [DOI] [PubMed] [Google Scholar]
- 8.Marret O., Goueffic Y., Pistorius M.A., Patra P., Chaillou P. Popliteal artery thrombosis secondary to exostosis of the tibia. Ann Vasc Surg. 2001;15:696–698. doi: 10.1007/s10016-001-0014-y. [DOI] [PubMed] [Google Scholar]
- 9.Matsuhita M., Nishikimi N., Sakurai T., Nimura Y. Pseudoaneurysm of the popliteal artery caused by exostosis of the femur: case report and review of the literature. J Vasc Surg. 2000;32:201–204. doi: 10.1067/mva.2000.105679. [DOI] [PubMed] [Google Scholar]
- 10.Argin M., Biverglu S., Arkun R., Parildar M. Solitary osteochondroma causing popliteal pseudoaneurysm that presented as a mass lesion. Diagn Interv Radiol. 2007;13:190–192. [PubMed] [Google Scholar]
- 11.Hemli J.M., Barakate M.S., Puttaswamy V., Appleberg M. Popliteal artery compression by a tibia osteochondroma with associated thrombosis and distal embolization. Aust N Z J Surg. 2000;70:459–461. doi: 10.1046/j.1440-1622.2000.01848.x. [DOI] [PubMed] [Google Scholar]
- 12.Socrate A.M., Locati P., Fusco U. Osteochondroma of the tibia and popliteal stenosis. Minerva Cardioangiol. 2000;48:317–321. [PubMed] [Google Scholar]
- 13.Shore R.M., Poznaski A.K., Anandappa E.C., Dias L.S. Arterial and venous compromise by an osteochondroma. Pediatr Radiol. 1994;24:39–40. doi: 10.1007/BF02017658. [DOI] [PubMed] [Google Scholar]
- 14.Smits A.B., vd Pavoordt H.D., Moll F.L. Unusual arterial complications caused by an osteochondroma of the femur or tibia in young patients. Ann Vasc Surg. 1998;12:370–372. doi: 10.1007/s100169900170. [DOI] [PubMed] [Google Scholar]