Abstract
Breast cancer (BC) is a disease that has improved prospects for survival if detected and treated early. Delayed help-seeking behavior, with poor survival as a consequence, is an important public health issue in the Middle East. More than 75% of breast cancer patients in the United Arab Emirates (UAE) seek medical advice after experiencing a sign or symptom of the disease and many seek such advice late. Our aim was to explore factors influencing delayed presentation for treatment after self-discovery of symptoms consistent with breast cancer in Arab women in the United Arab Emirates (UAE), and to explore facilitators and barriers of women’s health seeking behavior in the complex religiously dominated society of the UAE. A qualitative descriptive approach using semi-structured interviews was used. We interviewed nineteen BC survivors aged 35–70 who have experienced delayed presentation to treatment after symptomatic recognition of BC. The time interval between initial experience of symptoms consistent with BC, and taking action to seek medical help was between three months to three years. The key themes that emerged from the interviews were varying responses to symptom recognition, fear of societal stigmatization, and concerns regarding abandonment by spouse because of BC. Culture has a strong influence on the decisions of women in the UAE society. The lack of awareness about signs and symptoms of BC and routine screening has an important effect on symptom appraisal and subsequently decision making regarding options for treatment.
Keywords: Breast cancer, Presentation delay, In depth interviews, Health seeking behavior
Highlights
-
•
Lack of awareness about breast health, screening, signs/symptoms and risk factors.
-
•
Culture/societal values have great influence on women׳s attitudes and behaviors.
-
•
Support of healthcare providers may reduce likelihood of delay.
1. Introduction
Delays between recognition of symptoms suggesting breast malignancy and seeking help or advice from healthcare professionals vary between different communities and countries (O׳Mahony & Hegarty, 2009). Various factors such as culture, gender roles and socio-economic status influence the decision making of women to seek medical attention (O׳Mahony & Hegarty, 2009). BC is a disease that has improved prospects for survival if detected and treated early. Any delay in presentation for symptomatic BC is associated with larger tumors, more advanced stages of disease and consequently poorer prospects for survival (Richards, Westcombe, Love, Ramirez, & Johns, 1999). Delay in BC treatment has been categorized into:
-
a)
Patient delay-defined as waiting three or more months to seek help (e.g. consulting a physician) after self-discovery of breast signs or symptom;
-
b)
Provider delay-defined as one month or more from the time of first patient visit to the physician and the beginning of treatment (Pack & Gallo, 1938).
Among the top ten sites for cancer diagnosed in the United Arab Emirates (UAE), BC is at the top of the list. It constitutes 43% of cancers diagnosed among females and 25% of all cases of cancer (Cancer Registry Report, 2012). It is the second leading cause of death among women with an incidence rate of approximately 38 per 100,000 (Cancer Registry Report, 2012). The annual incidence is more than 130 new cases of BC diagnosed in the emirate of Abu Dhabi (Cancer Registry Report, 2012). Despite having access to the national screening programs and the coverage of cancer screening by the health insurance, only around 75% of BC patients in the United Arab Emirates (UAE) seek medical advice after experiencing a sign or symptom of the disease (Cancer Registry Report, 2009). The introduction of mandatory health insurance in 2007 in the emirate of Abu Dhabi has provided all residents access to high quality care (Taher, Al Neyadi, & Sabih, 2008). Late detection of BC has historically led to significant increases in mortality. Female adult nationals between 40 and 69 are being given an option for BC screening as part of their insurance card renewal process. For non-UAE nationals, screening campaigns have helped in early detection of BC, however, screening is not performed on an organized basis and some insurance companies do not cover screening cost (Taher et al., 2008). Some preventive medicine centers provide free screening, but its availability is not widely publicized.
In the Middle East, late diagnosis has been attributed to the lack of knowledge about BC, and to the limited access to information on screening programs (Altwalbeh et al., 2015, Lodhi et al., 2010). However, there is scant published literature from this region on the reasons for delayed presentation of female BC (Lannin et al., 1998). There has been also little comparison between communities and countries about similarities and differences in reasons for such delays.
The aim of our study was to explore factors influencing delayed presentation for advice in BC patients, and their health seeking behavior regarding treatment after self-discovery of symptomatic breast disease among Arab women in the United Arab Emirates. The results can contribute to improvement of the standards and quality of BC screening for early detection and prompt follow-up in the UAE.
2. Methods
2.1. Design
A qualitative approach using thematic analysis was used to explore UAE women׳s reasons for delay in seeking advice for BC symptoms, and their help seeking trajectories. The process involved in-depth confidential person-to-person interviews. This was the preferred method for acquiring data, as it involved questions that may be perceived to be ‘sensitive’ (Kvale, 1996).
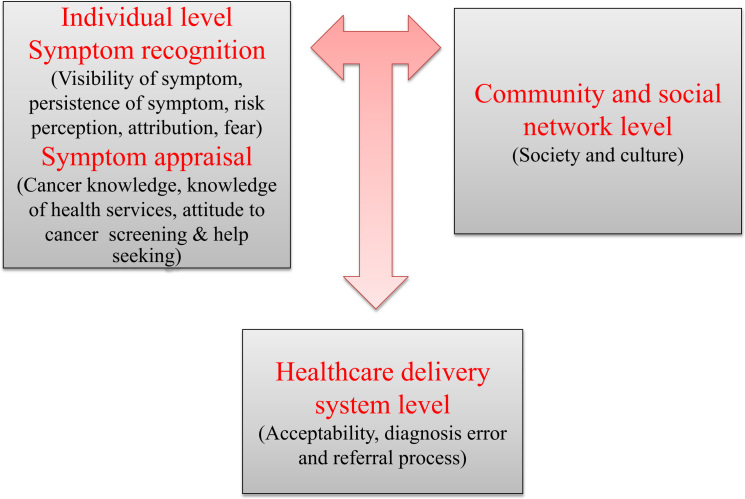
Many help seeking models have been developed to understand why women delay in seeking clinical help (Andersen et al., 1995, Bish et al., 2005, De Nooijer et al., 2003, Facione et al., 2002, O׳Mahony et al., 2010, Reifenstein, 2007, Rauscher et al., 2010). The constructs of these models can be used in the development of new models appropriate for another culture (Unger-Saldaña & Infante-Castañeda, 2011). In this study, a conceptual framework was used to guide the analysis based on two previously developed models: the understanding delayed presentation model by Bish et al. (2005) and the grounded model of seeking help for breast symptoms (GMHSB) by Unger-Saldaña and Infante-Castañeda (2011). The framework shows the interactions of the BC patient at three levels, (a) the individual level; including symptom recognition and symptom appraisal, (b) the community and social network level, and (c) the healthcare delivery system level (Fig. 1). The first level uses four aspects identified in Bish et al., (2005) model: (1) knowledge and symptom appraisal, (2) attitude to help seeking, (3) disclosure of symptoms and (4) intention to seek help. These four aspects interact together to influence patient behavior. At level one, the individual evaluates and interprets the recognized symptom(s) and her perception as being sick or unwell as a prelude to seeking help. At the second level, the social and community network is represented within the environment. This includes the woman׳s family, her husband (for married women), neighbors and friends. The interaction of the first two levels: the individual level and the community-social network level in the environment guides the woman in decision making, i.e. whether to seek help or to ignore the symptom(s). In the UAE, we assume that there are no issues with access to healthcare due to the presence of primary health services in the community and the wide coverage of health insurance of different services including cancer screening and treatment. If the woman decides to seek help, then the third level; the healthcare services utilization (healthcare delivery level) will influence the two previous levels. The third level includes aspects such as acceptability and satisfaction of the health services by women, errors in diagnosis and the referral process.
Fig. 1.
Conceptual framework (the help seeking model).
2.2. Study setting
United Arab Emirates (UAE) is a fast developing country with an estimated population of 9.35 million (Trading Economics/World Bank, 2014), located in the southeastern corner of the Arabian Peninsula. It was formed in 1971 as a federation of seven emirates – with Abu Dhabi and Dubai being the two most well-resourced and developed. Abu Dhabi is the capital of the UAE, with an estimated population of 2.58 million residents, 18% are UAE-nationals (Health Statistics, 2012). The basic elements of the traditional UAE society are an emphasis on the importance of Islam, the tribe and the family. The tribe and family values influence the society and continue to shape the beliefs and behavior of UAE nationals and UAE residents of Arabic origin (Peck, 1986). This component of UAE society is patriarchal, with men being the main decision makers and heads of the households. The head of the family is usually the eldest male (Augustin, 2002). Women wear black garments (termed ‘abayas’) and hijabs to cover their heads and sometimes their faces also. The city of Al Ain is the second biggest city in the emirate of Abu Dhabi. The Health Authority - Abu Dhabi (HAAD) is responsible for the regulation of health care in the emirate of Abu Dhabi. All citizens have health insurance which covers a range of health services including oncology care. Tawam hospital in Al Ain was designated as the main referral oncology hospital in the UAE in February 1983 (Tadmouri & Al-Sharhan, 2004).
2.3. Selection and recruitment of participants
Participants were either UAE nationals or non-national women of Arabic origin presenting with BC symptoms between January 2010 and December 2011 at Tawam Hospital. Criteria for selection: Women who had advanced stage at diagnosis suggesting late presentation (stage IIB or III, or IV based on the AJCC 5th edition (American Joint Committee, 1997)). To reduce recall bias, only women who were diagnosed more recent (i.e. in 2010 and 2011) were included. The participants were mainly BC survivors and women who were undergoing treatment or follow up.
A list of all eligible participants was generated from Tawam hospital patient records. Purposive and snowball sampling of BC survivors was conducted by the principal investigator. Selected women were asked to identify potential participants from their community. This enabled participation of a diverse range of perspectives and facilitated the inclusion of women from different age groups, ethnicity and educational status. Sampling was continued until data saturation was attained. Our sample included women from the Breast Center, Radiotherapy, Oncology clinic, local BC support groups and from Tawam hospital database.
Recruitment was carried out via telephone calls after extracting their phone numbers from the Tawam hospital database. The principal investigator called the women. Two further attempts were made to contact non-responders to the initial phone call. Following agreement to participate, the participants had several follow-up phone conversations with the interviewer to improve interviewer-participant rapport and to help retain interest and participation in the research. The interviewer visited women who were under treatment in Tawam hospital several times before the conduction of the interview to establish trust relationship and rapport. Women who agreed to be interviewed were asked to choose a convenient venue of their choice for the face-to-face interview.
Ethical approval was obtained from the Al Ain Medical District Human Research Ethics Committee. Written consent was obtained from all participants prior to the interview.
2.4. The interviews
Nineteen women were recruited, sampling was continued till data/thematic saturation was reached. In-depth interviews were conducted using a semi-structured interview guide by the principal investigator who was a female. The interview guide traced the journey of the patient from discovery of symptom(s) of breast disease to their present state of health. All interviews were conducted in the Arabic or English language based on each participant׳s preference. The duration of interviews ranged from 60 to 120 min. Interviews were audio-taped and transcribed. Provisions were made for participants to be referred for primary care if psychological or physical distress was detected during the interviews.
The audio-recordings were transcribed verbatim by the principal investigator. For the Arabic interviews, translation to English and back translation was done by the principal investigator followed by analysis of all the interview data (in English). A quality control check on a random selection of four transcripts was implemented by another investigator to ensure accuracy in the transcription of the audio taped interviews.
Location of the interviews: conducting the interviews in the participants׳ homes was initially considered but later found to be not feasible, as an additional layer of approval from the husband or head of family was required. The interviews were therefore conducted in Tawam hospital during their follow up or treatment visit and that was considered convenient to the participant. This was perceived to be a non-threatening environment for the interviews with the participants as all of them were still visiting the hospital for follow-up and participating in the local support group of BC survivors.
2.5. Data analysis
All transcribed data were read by the principal investigator several times to obtain familiarity with the information provided. The data were analyzed using the thematic framework analysis method (Ritchie & Lewis, 2003). A priori defined themes and emerging key points were identified from the adopted thematic framework. An approach involving first cycle coding and second cycle coding was used to identify emerging codes (Saldana, 2009). The principal investigator did the first cycle of coding and another investigator did the second cycle of coding. Coded responses and the views and ideas of all participants were then grouped and classified according to the priori defined themes. To avoid bias, three transcripts were analyzed separately by two independent researchers (JNWL and TCAW). Any disagreement was discussed to reach consensus of themes.
2.6. Trustworthiness
During data collection, participants were visited several times in the hospital before, during and after conducting the interviews to establish good rapport and to allow women to have sufficient confidence in the principal investigator and the interview method to completely discuss their experiences. Some interviews were conducted more than once to allow for more productive discussion and to ensure that what was said by the woman was well understood by the principal researcher. A second quality control check was to use coding of three randomly selected sets of interview information, to be coded separately by a different researcher with extensive experience of women issues and qualitative research methodology. The second researcher was not involved in the data collection. It was reassuring to note that the codes generated by both researchers were similar. After the interviews were conducted by the PI, participants who were available and agreed (n=8) were asked to verify the findings.
The individual interview approach was deemed to be suitable and effective by the principal investigator and the study participants. The participants felt that their privacy and confidentiality were protected. They felt free to discuss personal experiences on sensitive issues such as the influence of culture on behavior and on their personal relationship with their spouse and family members.
3. Results
3.1. Sample characteristics
A total of 19 women were interviewed, all were Muslims, twelve women were UAE nationals and seven were non-nationals of Arabic origin from Iraq, Egypt, Jordan, Tunisia and Palestine. Their characteristics are shown in Table 1. Age ranged from 35 to 68 years. Eighteen (95%) women indicated that they had previously heard of BC and three (16%) women had a positive family history of BC (i.e. BC in a close relative). The education level of participants ranged from illiteracy to university level. Most of the women in our study never had BC screening (N=16) prior to being diagnosed. The time interval between symptom discovery and seeking medical help ranged from three months to three years (Table 1).
Table 1.
Characteristics of the interviewed women.
| Case no. | Age | Marital status | Education | Employment status | Ethnicity | Family history of BC | Had breast cancer screening before | Health insurance coverage | Stage | Interval between symptom discovery and diagnosis (in months) |
| 1. | 36 | Single | University | Employed | Other Arab national | Yes | Never | Full coverage (screening+treatment) | IIB | 3–5 |
| 2. | 40 | Married | High school | Employed | UAE national | Yes | Never | Full coverage (screening+treatment) | IIB | >24 |
| 3. | 36 | Single | Diploma | Employed | UAE national | No | Never | Full coverage (screening+treatment) | III | >24 |
| 4. | 50 | Single | Diploma | Employed | UAE national | No | Yes | Full coverage (screening+treatment) | IIB | 3–5 |
| 5. | 36 | Single | High school | Unemployed | Other Arab national | No | Never | Exempted from payment | III | 6–10 |
| 6. | 36 | Widow | Diploma | Employed | UAE national | No | Yes | Full coverage (screening+treatment) | IIB | 3–5 |
| 7. | 36 | Married | High school | Unemployed | UAE national | No | Never | Full coverage (screening+treatment) | IIB | 3–5 |
| 8. | 40 | Married | High school | Employed | UAE national | No | Never | Full coverage (screening+treatment) | III | 3–5 |
| 9. | 45 | Married | High school | Employed | UAE national | No | Never | Full coverage (screening+treatment) | IIB | 11–12 |
| 10. | 47 | Single | No formal education | Unemployed | UAE national | No | Never | Full coverage (screening+treatment) | IIB | 3–5 |
| 11. | 48 | Married | High school | Employed | Other Arab national | No | Never | Full coverage (screening+treatment) | III | 11–12 |
| 12. | 36 | Married | University | Unemployed | UAE national | Yes | Never | Full coverage (screening+treatment) | III | 3–5 |
| 13. | 55 | Married | No formal education | Unemployed | UAE national | No | Never | Full coverage (screening+treatment) | IIB | >24 |
| 14. | 55 | Married | High school | Employed | Other Arab national | No | Yes | Exempted from payment | IIB | 3–5 |
| 15. | 60 | Married | No formal education | Unemployed | Other Arab national | No | Never | Exempted from payment | IIB | 13–18 |
| 16. | 60 | Married | University | Employed | Other Arab national | No | Never | Exempted from payment | III | >24 |
| 17. | 65 | Married | No formal education | Unemployed | UAE national | No | Never | Full coverage (screening+treatment) | III | 3–5 |
| 18. | 67 | Married | High school | Retired | UAE national | No | Never | Full coverage (screening+treatment) | III | >24 |
| 19. | 68 | Married | University | Retired | Other Arab national | No | Never | Exempted from payment | III | 19–24 |
3.2. Identified themes
The three main themes identified through the process of thematic analysis were: (1) symptom recognition and appraisal, (2) role of community and social network and (3) healthcare delivery system. These are presented with illustrative quotes in the following sections.
3.2.1. Symptom recognition
3.2.1.1. Visibility and persistence of symptom
BC symptoms vary from lumps to skin changes and nipple bleeding. Despite the visibility and the classical presentation of BC symptoms, five of interviewed women misinterpreted the warning signs.
“Around two years ago…. I noticed a lump… like a small peanut….I only felt it when I touched my breast, I am not currently breastfeeding but I thought it was something related to an old breast milk as I breast fed all my children, frozen old milk or something….’’ (Case 3).
The persistence of the symptom was sometimes the reason to draw the woman׳s attention to the presence of disease, and this motivated them to seek evaluation and treatment.
“I was breastfeeding and I noticed my breast is getting hard with a lump, I thought it is from milk accumulation, I ignored it and continued breastfeeding for a while ….but then the lump was not going away; my breast was getting larger and larger every time I look….only then I realized that something might be going wrong with me ….’’ (Case 5).
The signs of BC were attributed by participants to other diseases or to an event that happened prior to the symptom discovery. One of the women interviewed thought that the breast lump was due to a fall she had prior to discovering it. This attribution contributed to a long delay in seeking medical attention, until symptoms of advanced disease appeared.
“Well… around a year and a half ago I noticed a lump in my breast… I was thinking it is from a fall I had previously…. All the doctors were upset from me… they were saying where have you been hiding with this huge bleeding breast, you should have come earlier….I said to them I was treating myself by myself…..I thought it was a trauma related symptoms…I was putting ointments and taking pain killers to cope with it…’’ (Case 18).
3.2.2. Symptom appraisal
3.2.2.1. BC knowledge and risk perception
Some of the women did not know about relevant BC symptoms and signs, screening procedures and treatment options.
“I heard of cancer before…blood cancer, brain cancer, lung cancer……. but I never thought it can come in the breast…I was surprised when they informed me’’ (case 13).
The participants did not view themselves as at risk for BC. Education level did not appear to influence their behavior in regards to measures for early detection of BC.
Interviewer: “Have you had mammography before?’’
“Never, never because I am ….years old and married, I have 5 children; I do not take any medicine except the glucophage tablet for my diabetes……. I am very very healthy, so I did not go for the screening….I mean why should I… I used to do pap smear ……many times, I was concerned about cervical cancer but BC…. never suspected it. I was telling myself why should I go for checking if I am not feeling anything’’ (case 19).
3.2.2.2. Knowledge of health services and attitudes regarding seeking help
A lack of knowledge about healthcare services available for BC screening and treatment was mentioned by some of the women interviewed. This lack of knowledge contributed to delay in seeking advice regarding BC.
“I was feeling my breasts regularly, I felt a small lump…but I did not know where to go….. I asked my neighbor and she didn’t know as well….. She advised me to read holy Quran and apply olive oil to it…. I did that for a couple of years….’’ (Case 9).
Three women thought that cancer required the experience of serious symptoms such as pain, vomiting or bleeding. They did not consider a painless lump to be anything serious that required urgent attention.
“I don׳t go to the doctor to ask for unnecessary tests, you do not go to a doctor if you are ok; you have to be in extreme pain or complaining of something to go and see a doctor…..’’ (Case 11).
3.2.3. Community and social network
3.2.3.1. Breast cancer stigma
Three women expressed their difficulties and hardships with day to day activities even before experiencing cancer. Many felt that they had to fulfill multiple roles in regards to their families and to society. They felt pressure because they were expected to be role models in their society and cancer is thought to be affecting this role, and the negative attitude of community members to them once they developed the disease.
“Our old ladies used to say stress …. you know the relationships and troubles which happen in life… all this stress is one of the contributing factors to cancer especially in the Middle East … because women in the Middle East suffer in silence over a lot of things … for example, I knew women who have family, who have children … then the husband goes and he marries another woman.. She reaches the depth of despair that my husband is married to another woman… the husband comes home for one night… Do you see the children going astray, the boys are not being controlled … they have no control because he has another family or two families… The wives get stressed, they go crazy and they end up with some form of illness and usually BC, this is what I have actually observed ….’’ (Case 2).
The women expressed concerns about stigma and prejudice towards the whole family because of BC. Women with BC therefore often preferred to stay at home and suffer in silence as they did not want their families to ‘pay the price’ of having a family member with BC.
“When there is a family history of BC, the older women keep it quiet the whole family keep it quiet because we are worried about our daughters prospects for getting married… we are worried about our younger sisters getting married, and we are worried about getting a bad name in our family or people staying away from us … because people are afraid of ‘catching’ the disease, we keep quiet and we do not say that we have cancer through the generations of this family … we are all afraid psychologically to come forward and frightened to come forward to say I have a lump.. Because we are worried about our image and our families… we are worried if our husbands would still want us… we are worried about whether we are still able to produce children…worries and worries….. This is what makes us hide’’ (Case 4).
Most of the women shared the view that cancer was not a popular topic to talk about in their society or even within the family. It is a sensitive topic surrounded by shame and silence.
“Although I knew about cancer, I never heard of somebody talking of BC not even cancer, nobody was allowed to talk about it, you just look at their eyes and you will see the fear and vagueness…you will just know…’’ (Case 12).
Another aspect which emerged in the interviews is the way society views BC survivors. Members of society do not want to talk about cancer survivors, not because they are ashamed of them, but because of the inadvertent bad publicity. Most of the participants disclosed that nobody around them knew about their cancer diagnosis and they would rather keep quiet and not share this news with anybody because they do not know how people around them would react to the information. Others were convinced that they will be treated badly and that their families will suffer with them as well.
“Because here in our culture people look to you differently if you have cancer, I didn׳t tell anybody….I did not want them to look at me this way…. my whole family will be affected’’ (Case 7).
Some were isolated from society because people do not want to visit them as they are afraid of the cancer being contagious, or they were in fear of being under the ‘evil eye’ (in Arabic culture, the ‘evil eye’ is a symbol for envy and jealousy from the sick person regarding the health of a well person. This is believed to bring bad luck and the occurrence of the disease). These misconceptions and a lack of general awareness about the nature of cancer and what is known or not known about its causation made most of the women keep their disease undercover and some do not seek medical attention even when they have relevant signs or symptoms of BC.
“People will say do not visit auntie (me)…. she has cancer because you do not want to catch it, the bad eye will fall on you do not go and visit her …’’ (Case 2).
Another participant talked about a painful experience she had as a result of people knowing what she was suffering from during her treatment.
“I just finished chemical therapy and I went to visit somebody in her house, she had some other guest, four women. While sitting with them, my head cover moved a little and some of the bald patches on my head were revealed. They looked at me and laughed and started whispering to each other, I could not take it, I left immediately and went home, I was crying all night long. I told my sisters that I did not want to see that look from people and that׳s why I isolated myself away from them and since then I don׳t visit anybody….’’ (Case 8).
Some participants expressed the idea that the society considers them guilty and having cancer is a payback for the sins and mistakes made during their life.
“My husband and family said to me….oh you must have done something in your life and it came back on you…. what did you do? This is to pay for your sins’’ (Case 4).
3.2.3.2. Fear of being abandoned by husband
An informant talked about the relationship she had with her husband after she was diagnosed and how he was living with her under the same roof but not as a married couple.
“My husband completely changed, I have been married for 10 years; I was diagnosed a few years ago and since then he was pretty much on his own. It is because of cancer….I suppose he tried to support me in whatever way he could… But I would never let him see me down; I will never let him see that he broke me’’ (Case 9).
Another woman disclosed information about the intimate relationship between her and her husband.
“The change was mainly sexually, we never sleep together after I was diagnosed, we just live in the same house and we tolerate each other. I did the full breast reconstruction and I was happy ….he wasn׳t ….actually he never saw them (my new breasts)….you see the husbands supporting their wives in TV only, in romantic movies but not in real life…this is the truth’’ (Case 2).
3.2.4. Healthcare system
The religious and cultural embargo on restricting contact between the sexes contributed to delay in seeking help. The breast is culturally considered a reproductive organ and therefore a sensitive issue. A woman delayed for 8 months because she did not want a male physician to examine her.
“I felt a lump in my breast, I went to the health center in my village and they only had one doctor… a male doctor…of course I went back home without checking and I forgot about it… few years later… the BC campaign came to our village and I was diagnosed and referred to the hospital’’ (Case 13).
Errors in diagnosis can cause false reassurance regarding the seriousness of breast symptoms or signs. Two women experienced delays because of inaction by healthcare provider.
“I went to the hospital, they said there is nothing to worry about and the lump is from milk production. So I did not check further, the tumor was smaller… Three years later, the tumor became very big, I went to another hospital and they said you have cancer…’’ (Case 16).
Some delays were due to lack of action of healthcare providers after a diagnosis was made, particularly in waiting to be referred to a regional oncology center for commencement of treatment.
“I went at the beginning of the year and they did for me the x-ray which squeezes the breast. They said I have cancer and that they will refer me to the hospital… I waited for their call but nobody called me for 6 or 7 months…’’ (Case 5).
4. Discussion
Despite advancements in BC treatment, well-established screening services in the emirate of Abu Dhabi, and the availability of health coverage, there is still a considerable lack of awareness from women about breast health, regular screening, and BC signs/symptoms and predisposing factors. This study provides an understanding of women׳s help-seeking behavior and factors influencing the time interval between presentation of symptoms and seeking medical treatment. Unlike other studies, it puts more emphasis on the social and cultural dimensions of this issue. It reveals cultural and religious aspects of BC and the distinct way United Arab Emirates society reacts to BC. This study is consistent with other studies (Burgess et al., 2001, Unger-Saldaña and Infante-Castañeda, 2011) in that breast lump was the most common symptom reported by women and often perceived to be non-serious. Not perceiving painless breast lumps as a threat to life was also seen among Saudi women (Altwalbeh et al., 2015) and therefore delaying seeking help reflects the lack of knowledge in regards to BC and its presentation. This initial symptom did not raise enough concern for prompt follow up. Some women compared it with previous knowledge and experiences (Khakbazan, Roudsari, Taghipour, & Pour, 2014). The attribution of the symptom to common conditions and experience is a factor in causing delay (Smith et al., 2005, Unger-Saldaña and Infante-Castañeda, 2011). However, similar to a study conducted in Ethiopia (Dye, Bogale, Hobden, et al., 2012), changes in the nature of symptoms over time alerted the attention of women and motivated them to seek medical attention. For example, a woman who had a breast lump for two years was motivated by the occurrence of bleeding to seek medical attention. It describes the social norms of the society with regard to expectation from women and how they should behave if confronted with BC. Society expected women to suffer in silence and to behave as a role model for other women. The picture of a role model should not be distorted by BC.
There have been few studies in the Middle East exploring factors influencing late presentation or delay or help-seeking behavior for BC (Alhurishi, Lim, Potrata, & West, 2011). All of them used quantitative research methods to examine late presentation, and most examined only patient-related factors (Abdel-Fatah et al., 1999, Elzawawy, 1991, Elzawawy, 1999, Harirchi et al., 2005, Montazeri et al., 2003, Stapleton et al., 2011). A lack of knowledge was not the only reason for delay; a complex array of personal, social, and cultural factors appears to influence a woman׳s decision on how soon to ask for appropriate clinical advice (Khakbazan et al., 2014).
Our study shows that cultural and societal beliefs have a great effect on women׳s attitudes and behaviors towards symptoms recognition, appraisal, screening and presentation for medical treatment. Fear about society reaction to women with BC, and failing to meet community expectations about health and disease strongly influenced decision making more than the fear of death from impending disease. This fear held the women back from seeking medical advice and imposed an attitude of silence. Culturally, cancer is often stigmatized at times and our study found that this negatively influenced symptom disclosure and social interaction. In contrast, other studies (Abdullah et al., 2013, Burgess et al., 2001, Lam et al., 2009, Lu et al., 2010, O׳Mahony et al., 2011, Unger-Saldaña and Infante-Castañeda, 2011) reported that symptom disclosure and social interaction was perceived as supportive and led to informal and emotional support.
Our study found a link between screening and delay in seeking medical advice. Attending regular BC screening aid in the self-awareness process and helped women understand the seriousness of their condition, three women in our study had BC screening before and knew about BC, this knowledge prompted them to seek advice earlier than other women in the study. Screening helped women evaluate the condition properly and women who understood the seriousness of their condition, tried to seek medical care to confirm the diagnosis (Adam and Soutar, 2003, Taib et al., 2011).
Similar to studies conducted in Muslim countries, talking about breast as a sexual reproductive organ is culturally taboo (Babu, Samari, Cohen, et al., 2011). Fatality is also a concern and a reason for delay resulting from the perception of incurability of cancer (Sabih et al., 2012, Taib et al., 2011). In our study, some women suggested feeling inferior to men in the community and being less powerful, as their role in the family obliges them to please their husbands. The husband׳s relationship with a woman diagnosed with BC is a very sensitive issue. The attitude of husbands and the perspective of men in regards to women with BC was not addressed in our study. However, some aspects of the intimate relationship of women with their husbands was explored in our study. Our study provided an opportunity for women with BC to openly talk about their feelings, behavior and relationships.
4.1. Thematic framework (the help seeking model)
Few qualitative studies have been conducted in the Arab world. All of these studies were merely descriptive in nature and lacking a theoretical framework (Abdel-Fatah et al., 1999, Harirchi et al., 2005, Ramirez et al., 1999, Richards et al., 1999, Unger-Saldaña and Infante-Castañeda, 2009). The majority of BC delay (BCD) research has an empirical scientific approach and has described mainly its relation to survival, factors associated to patient delay, and provider delay factors (Bairati et al., 2006, De Nooijer et al., 2001, Katapodi et al., 2005). Most studies that include theoretical frameworks base their analysis on psychological theories to explain the patients reasoning for delayed presentation (Bish et al., 2005, Lim, 2011). Contextual social and health system characteristics have been ignored by most researchers investigating BCD. The illness behavior theory can enrich the understanding of BCD through its social and psychological aspects of health it accounts for.
The two models adopted in this study (the understanding delayed presentation model by Bish et al. (2005) and the grounded model of seeking help for breast symptoms (GMHSB) by Unger-Saldaña and Infante-Castañeda (2011)) allow for different combination of factors at various levels to explain delay. Especially in our setting in the UAE, many factors play different roles in the woman׳s journey of disease, and a dynamic model that allows possible interaction between different factors at various levels was adopted in this study in an attempt to understand this delay.
The understanding delayed presentation model acknowledges that delay in help seeking for BC symptoms is influenced by a complex interaction of demographic, clinical, cognitive, behavioral and social factors. However, the model concentrates on the patient delay and does not discuss the system delay and the role of caregivers in this process. On the other hand, the GMHSB is a well-constructed model, however, the structural characteristics of the health system in Mexico is overrepresented in the model as a result of over discussing it by interviewees and this was mentioned by the authors as a limitation of the model. There was an interest to know the applicability of the model in a different setting where the financial burden on patients is limited or nonexistent. The UAE health system is thought to be of interest, as all residents and national citizens of the UAE enjoy excellent health coverage and the financial aspect plays a small or limited role in the decision making of women to seek help. Another limitation of the model discussed by the authors, is the fact that interviewees who were purposefully selected for their study were privileged in their ability to reach or access the public cancer hospital, many others due to different circumstances were not able to access the hospital. Therefore women interviewed are not representative of the uninsured Mexican population. To overcome these limitations, our participants were chosen purposefully from the regional oncology center at the end of their treatment.
5. Strengths and limitations
This is one of the few qualitative studies on BC in the Middle East and describes the reasons for delay in seeking treatment. It explores different aspects of the complex health seeking behavior of UAE national and non-national Arab women. The findings will facilitate comparisons with the experience in other countries in the Middle East (e.g. Saudi Arabia, Qatar, Bahrain, and Oman) and other Muslim countries in Asia (e.g. Malaysia, Brunei, and Indonesia). The interdisciplinary nature of the research team allowed a different perspective analysis. As our study examined a small number of patients who presented at the Tawam Hospital in Abu Dhabi, a caution must be exercised before extrapolating the findings to other emirates of the UAE. However, using the thorough description of the research context would aid in the transferability of data. Also our study is subject to recall bias as women were asked to give narrations of their past experience. Another limitation could be that we only interviewed women who were stage IIB and III and majority had formal education. Further verification of these findings may be obtained from medical records, discussions with family members or through focus group discussions.
6. Implications for future research
In order to appropriately quantify the extent of screening awareness among women, a population-based epidemiological study is recommended. A separate study to measure the effect of breast health counseling and to explore the role of healthcare providers on BC screening and early detection could reveal useful findings in improving BC screening and care in the UAE. Community level awareness as a primary effort to begin changing social/cultural norms and practices toward BC could be useful.
7. Conclusion
Our findings suggest that culture has a great effect on the decision making of women with BC. The lack of awareness about signs and symptoms of BC and routine screening has a major effect on symptom appraisal and consequently informed decision making. However, national efforts are needed to address specific benefits of early detection and to increase the awareness about these benefits.
-
•
In the Middle East, it has been commonly assumed that late diagnosis of BC is due to a lack of knowledge and insufficient information about screening programs.
-
•
There is a lack of research findings on the reasons behind delayed presentation of female BC.
Funding
This study was supported by a grant from United Arab Emirates University, College of Medicine and Health Sciences.
Acknowledgment
We thank Tawam Hospital staff (Breast Center, Oncology Clinic & Radiotherapy Department) for their help and support in facilitating the conduction of this study and all study participants for their honest input.
References
- Abdel-Fatah M., Anwar M., Mari E., El Shazly M., Zaki A., Bedwani R. Patient and system related diagnostic delay in breast cancer. European Journal of Public Health. 1999;9:15–19. [Google Scholar]
- Abdullah A., Abdullah K.L., Yip C.H., Teo, Taib N.A., Nj C.J. The decision-making journey of Malaysian women with early breast cancer: A qualitative study. Asian Pacific Journal of Cancer Prevention. 2013;14:7143–7147. doi: 10.7314/apjcp.2013.14.12.7143. [DOI] [PubMed] [Google Scholar]
- Adam, D., & Soutar G. N. (2003). The impact of self-discovered breast changes: Some qualitative evidence. In Proceedings of the Australian and New Zealand Marketing Academy Conference (ANZMAC) (pp. 1920–1927).
- Alhurishi, S., Lim, J., Potrata, B., & West, R. (2011). Factors influencing late presentation for breast cancer in the Middle East: A systematic review. Asian Pacific Journal of Cancer Prevention, 12(6), 1597–1600. 〈http://www.ncbi.nlm.nih.gov/pubmed/22126505〉 Retrieved 11.12.12. [PubMed]
- Altwalbeh D., El Dahshan M., Yassin R. Factors influencing delayed presentation of breast cancer among Saudi women. International Journal of Science and Research. 2015;1:4. [Google Scholar]
- American Joint Committee . 5th edition. Lippincott-Raven; Philadelphia, New York: 1997. AJCC cancer staging manual. [Google Scholar]
- Andersen B.L., Cappioca J., Roberts D.C. Delay in seeking a cancer diagnosis: Delay stages and psychophysiological comparison processes. British Journal of Social Psychology. 1995;34:34–52. doi: 10.1111/j.2044-8309.1995.tb01047.x. [DOI] [PubMed] [Google Scholar]
- Augustin B. 2nd edition. Children׳s Press; 2002. United Arab Emirates. [Google Scholar]
- Babu G.R., Samari G., Cohen S.P., Mahapatra T., Wahbe R.M., Mermash S. Breast cancer screening among females in Iran and recommendations for improved practice: A review. Asian Pacific Journal of Cancer Prevention. 2011;12:1647. [PubMed] [Google Scholar]
- Bairati I., Fillion L., Meyer F.A., Hery C., Larochelle M. Women׳s perceptions of events impeding or facilitating the detection, investigation and treatment of breast cancer. European Journal of Cancer Care. 2006;15(2):183–193. doi: 10.1111/j.1365-2354.2005.00635.x. [DOI] [PubMed] [Google Scholar]
- Bish A., Ramirez A., Burgess C., Hunter M. Understanding why women delay in seeking help for breast cancer symptoms. Journal of Psychosomatic Research. 2005:321–326. doi: 10.1016/j.jpsychores.2004.10.007. [DOI] [PubMed] [Google Scholar]
- Burgess C., Hunter M.S., Ramirez A.J. A qualitative study of delay among women reporting symptoms of breast cancer. British Journal of General Practice. 2001;51(473):967–971. [PMC free article] [PubMed] [Google Scholar]
- Cancer Registry Report (2009). Annual report. Tawam Hospital.
- Cancer Registry Report (2012). Annual report. Tawam Hospital.
- De Nooijer J., Lechner L., De Vries H. Help-seeking behaviour for cancer symptoms: Perceptions of patients and general practitioners. Psycho-oncology. 2001;10(6):469–478. doi: 10.1002/pon.535. [DOI] [PubMed] [Google Scholar]
- De Nooijer J., Lechner L., de Vries H. Social psychological correlates of paying attention to cancer symptoms and seeking medical help. Social Science & Medicine. 2003;56:913–920. doi: 10.1016/s0277-9536(02)00098-9. [DOI] [PubMed] [Google Scholar]
- Dye T.D., Bogale S., Hobden C., Tilahun Y., Deressa T., Reeler A. Experience of initial symptoms of breast cancer and triggers for action in Ethiopia. International Journal of Breast Cancer. 2012;2012 doi: 10.1155/2012/908547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elzawawy A. Vol. 1. International Atomic Energy Agency/TECDOC; 1991. Delay in seeking medical advice by breasts cancer patients presenting with a breast lump; pp. 35–42. [Google Scholar]
- Elzawawy A. Delay in seeking medical advice by breast cancer patients presenting with breast lump. Cancer Strategy. 1999;1:16–19. [Google Scholar]
- Facione N.C., Miasckowski C., Dodd M.J., Paul S.M. The self-reported likelihood of patient delay in breast cancer: New thoughts for early detection. Preventive Medicine. 2002;34:397–407. doi: 10.1006/pmed.2001.0998. [DOI] [PubMed] [Google Scholar]
- Harirchi I., Ghaemmaghami F., Karbakhsh M., Moghimi R., Mazaherie H. Patient delay in women presenting with advanced breast cancer: an Iranian study. Public Health. 2005;119:885–891. doi: 10.1016/j.puhe.2004.11.005. [DOI] [PubMed] [Google Scholar]
- Health Statistics (2012). 〈www.haad.ae/statistics〉. Accessed 12.11.14.
- Katapodi M., Facione N., Humphreys J., Dodd M. Perceived breast cancer risk: heuristic reasoning and search for a dominance structure. Social Science & Medicine. 2005;60(2):421–432. doi: 10.1016/j.socscimed.2004.05.014. [DOI] [PubMed] [Google Scholar]
- Khakbazan Z., Roudsari R.L., Taghipour A., Pour R.O. Appraisal of breast cancer symptoms by Iranian women: Entangled cognitive, emotional and socio-cultural responses. Asian Pacific Journal of Cancer Prevention. 2014;15(1):8135–8142. doi: 10.7314/apjcp.2014.15.19.8135. [DOI] [PubMed] [Google Scholar]
- Kvale S. 4th edition. SAGE Publication; 1996. Interviews: An Introduction to Qualitative Research Interviewing. [Google Scholar]
- Lam W., Tsuchiya M., Chan M., Chan S.W., Or A., Fielding R. Help-seeking patterns in Chinese women with symptoms of breast disease: A qualitative study. Journal of Public Health. 2009;31:59–68. doi: 10.1093/pubmed/fdn088. [DOI] [PubMed] [Google Scholar]
- Lannin, D. R., Mathews, H. F., Mitchell, J., Swanson, M. S., Swanson, F. H., & Edwards, M. S. (1998). Influence of socioeconomic and cultural factors on racial differences in late-stage presentation of breast cancer. Journal of American Medical Association, 279(22), 1801–1807. Retrieved from 〈http://www.ncbi.nlm.nih.gov/pubmed/9628711〉. [DOI] [PubMed]
- Lim, J. N. W. (2011). Empirical comparisons of patient delay and help seeking models for breast cancer: Fitness of models for use and generalization. Asian Pacific Journal of Cancer Prevention, 12(6), 1589–1595. Retrieved from 〈http://www.ncbi.nlm.nih.gov/pubmed/22126504〉. [PubMed]
- Lodhi, F., Ahmad, B., Shah, S., & Naeem, M. (2010). Determinants of delayed presentation in breast cancer, APMC, 4, 9–16. Retrieved from 〈http://www.pmc.edu.pk/Downloads/apmc/apmc_v4n1/3-Determinants of Delayed Presentation in Breast Cancer.pdf〉.
- Lu M.H., Lin H.R., Lee M.D. The experiences among older Taiwanese women facing a new diagnosis of breast cancer. Cancer Nursing. 2010;33:398–405. doi: 10.1097/NCC.0b013e3181d72c45. [DOI] [PubMed] [Google Scholar]
- Montazeri A., Ebrahimi M., Mehrdad N., Ansari M., Sajadian A. Delayed presentation in breast cancer: A study in Iranian women. BMC Womens Health. 2003:3–4. doi: 10.1186/1472-6874-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O׳Mahony M., Hegarty J., McCarthy G. Women׳s help seeking behaviour for self discovered breast cancer. European Journal of Oncology Nursing. 2010:1–9. doi: 10.1016/j.ejon.2010.10.011. [DOI] [PubMed] [Google Scholar]
- O׳Mahony M., Hegarty J., McCarthy G. Women׳s help seeking behaviour for self-discovered breast cancer symptoms. European Journal of Oncology Nursing. 2011;15:410–418. doi: 10.1016/j.ejon.2010.10.011. [DOI] [PubMed] [Google Scholar]
- O׳Mahony M M., Hegarty J. Help seeking for cancer symptoms: A review of the literature. Oncology Nursing Forum. 2009;36(4):E178–E184. doi: 10.1188/09.ONF.E178-E184. [DOI] [PubMed] [Google Scholar]
- Pack G.T., Gallo J.S. The culpability for delay in the treatment of cancer. American Journal of Cancer. 1938;33:443e462. [Google Scholar]
- Peck M. Taylor & Francis; 1986. The United Arab Emirates: A venture in unity. [Google Scholar]
- Ramirez A., Westcombe A., Burgess C., Sutton S., Littlejohns P., Richards M. Factors predicting delayed presentation of symptomatic breast cancer: A systematic review. Lancet. 1999;353:1127–1131. doi: 10.1016/s0140-6736(99)02142-x. [DOI] [PubMed] [Google Scholar]
- Rauscher G.H., Ferrans C., Kaiser K., Campbell R.T., Calhoun E.E., Warnecke R.B. Misconceptions about breast lumps and delayed medical presentation in urban breast cancer patients. Cancer Epidemiology, Biomarkers & Prevention. 2010;19:640–647. doi: 10.1158/1055-9965.EPI-09-0997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reifenstein K. Care-seeking behaviours of African American women with breast cancer symptoms. Research in Nursing & Health. 2007;30:542–557. doi: 10.1002/nur.20246. [DOI] [PubMed] [Google Scholar]
- Richards M.A., Westcombe A.M., Love S.B., Ramirez A., Johns P. Little. Influence of delay on survival in patients with breast cancer: A systematic review. Lancet. 1999;353:1119–1126. doi: 10.1016/s0140-6736(99)02143-1. [DOI] [PubMed] [Google Scholar]
- Ritchie J., Lewis J. SAGE Publications Ltd.; London: 2003. Qualitative research practice. [Google Scholar]
- Sabih W., Taher J., El Jabari C., Hajat C., Adib S., Harrison O. Barriers to breast cancer screening and treatment among women in emirate of Abu Dhabi. Ethnicity Disease. 2012;22:148–154. [PubMed] [Google Scholar]
- Saldana J. 2nd edition. SAGE Publications Ltd.; 2009. The coding manual for qualitative researcher. [Google Scholar]
- Smith L.K., Pope C., Botha J.L. Patients׳ help-seeking experiences and delay in cancer presentation: A qualitative synthesis. Lancet. 2005;366:825–831. doi: 10.1016/S0140-6736(05)67030-4. [DOI] [PubMed] [Google Scholar]
- Stapleton J., Mullan P., Dey S., Hablas A., Gaafar R., Siefeldin I.A. Patient-mediated factors predicting early- and late-stage presnetation of breast cancer in Egypt. Psycho-Oncology. 2011;20:532–537. doi: 10.1002/pon.1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tadmouri G.O., Al-Sharhan M. United Arab Emirates; 2004. Cancers in the United Arab Emirates, genetic disorders in the Arab World; pp. 59–61. [Google Scholar]
- Taher, J., Al Neyadi, G., & Sabih W. (2008). Community profile summary of findings. 〈http://www.haad.ae〉 Retrieved on 05.01.14.
- Taib N.A., Yip C.H., Low W.Y. Recognizing symptoms of breast cancer as a reason for delayed presentation in Asian women—The psycho-socio-cultural Model for breast symptom appraisal: Opportunities for intervention. Asian Pacific Journal of Cancer Prevention. 2011;12:1601–1608. [PubMed] [Google Scholar]
- Trading Economics/World Bank (2014). 〈http://www.tradingeconomics.com/united-arab-emirates/population〉 Accessed on 12.11.14.
- Unger-Saldaña K., Infante-Castañeda C. Delay of medical care for symptomatic breast cancer: A literature review. Salud Pública de México. 2009;51(S2):S270–S285. doi: 10.1590/s0036-36342009000800018. [DOI] [PubMed] [Google Scholar]
- Unger-Saldaña K., Infante-Castañeda C.B. Breast cancer delay: A grounded model of help-seeking behavior. Social Science & Medicine. 2011;72(7):1096–1104. doi: 10.1016/j.socscimed.2011.01.022. [DOI] [PubMed] [Google Scholar]