Abstract
This study examined the interrelationship of race and socioeconomic status (SES) upon infant birthweight at the individual and neighborhood levels within a Midwestern US county marked by high Black infant mortality. The study conducted a multi-level analysis utilizing individual birth records and census tract datasets from 2010, linked through a spatial join with ArcGIS 10.0. The maternal population of 2861 Black and White women delivering infants in 2010, residing in 57 census tracts within the county, constituted the study samples. The main outcome was infant birthweight. The predictors, race and SES were dichotomized into Black and White, low-SES and higher-SES, at both the individual and census tract levels. A two-part Bayesian model demonstrated that individual-level race and SES were more influential birthweight predictors than community-level factors. Specifically, Black women had 1.6 higher odds of delivering a low birthweight (LBW) infant than White women, and low-SES women had 1.7 higher odds of delivering a LBW infant than higher-SES women. Moderate support was found for a three-way interaction between individual-level race, SES and community-level race, such that Black women achieved equity with White women (4.0% Black LBW and 4.1% White LBW) when they each had higher-SES and lived in a racially congruous neighborhood (e.g., Black women lived in disproportionately Black neighborhood and White women lived in disproportionately White neighborhood). In sharp contrast, Black women with higher-SES who lived in a racially incongruous neighborhood (e.g., disproportionately White) had the worst outcomes (14.5% LBW). Demonstrating the layered influence of personal and community circumstances upon health, in a community with substantial racial disparities, personal race and SES independently contribute to birth outcomes, while environmental context, specifically neighborhood racial congruity, is associated with mitigated health risk.
Keywords: Birth outcomes, Low birthweight, Racial disparity, Race, Socioeconomic status, Income, Neighborhood racial density, Racial congruity, United States
Highlights
-
•
Individual-level race and socioeconomic status (SES) were more influential than community-level factors.
-
•
Maternal Black race was associated with 1.6 greater odds of low birthweight.
-
•
Maternal poverty was associated with 1.7 greater odds of low birthweight.
-
•
Higher-SES Black women in White neighborhoods had the worst outcomes, 14.5% LBW.
-
•
Higher-SES Black women in Black neighborhoods had the best outcomes. 4.0% LBW.
Introduction
Racial health disparities have grown in the U.S., even as overall population health indicators have improved (Diez Roux, 2012, Orsi et al., 2010, U.S. Department of Health and Human Services, 2014). Health differences adversely affecting racial-ethnic minorities is most evident in the area of maternal-child health, where birth outcomes (birthweight and gestation, infant mortality) are particularly sensitive to health risk, and the cost of early health problems is expressed across the lifespan (Alio et al., 2009, Centers for Disease Control and Prevention, 2012, Lu and Halfon, 2003, Smedley et al., 2003, World Health Organization, 2014). The United States ranks 56th out of 224 nations in infant mortality, despite being one of the highest per capita healthcare spenders in the world (Central Intelligence Agency (CIA), 2014). This high mortality is driven by disproportionately high death rates among racial-ethnic minorities, particularly Black infants. Within the United States, Black infants die at 2.2 times higher rate than White infants (11.6 and 5.2 deaths per 1000 live births, respectively); a gap that has remained consistent even though overall infant mortality has trended steadily downward (Murphy et al., 2013, Orsi et al., 2010). The brunt of such inequities are borne by Black populations, but disparities take a toll on all, as gaps between the least and the most advantaged affect the health of those at every strata (Cooper et al., 2013, Eudy, 2009, Oishi et al., 2011).
The social determinants of health theory, adopted by health agencies across the globe, explains racial inequity as the end result of social institutions that systematically disadvantage minorities (Krieger, 2014, Link and Phelan, 1995, Smedley et al., 2003). Within this framework, social exclusion from economic participation and power is a major vehicle for institutionalized racism in the U.S. (David, 2007, Krieger, 2014, Popay et al., 2008). Poverty is experienced by 2.6 times more Blacks than Whites, extreme intergenerational poverty is more common among Blacks (Bloome, 2014), and racially segregated Black neighborhoods consistently have greater concentrations of poverty (McLeod and Nonnemaker, 2000, Osypuk et al., 2009). Living in segregated, high poverty communities further compounds the effect of individual poverty through exposure to distressed physical environments (pollution, dilapidated housing, zoning), fragmented social networks (social support, norms, crime, political power) and limited health-related resources (health care, nutrition, recreation, transportation) (Cook et al., 2009, Derose et al., 2011, Kramer and Hogue, 2008, Williams and Collins, 2001, Ziersch et al., 2005).
Poverty at the individual- or community-level, however, does not account for the entirety of racial health differences. While some studies have found that Blacks’ health improves apace with wealth increases, and with moves to higher-income neighborhoods, many others have reported that Blacks receive less health benefit from socioeconomic gains than Whites, and that for Black populations, health risk remains significantly elevated regardless of income level (Fuller-Thomson et al., 2009, Harding, 2003, Hayward et al., 2000, LaVeist, 2005; Nepomnyaschy, 2009; Nicklett, 2011; Pollack et al., 2013).
The same community structures that have been shown to constrain health and health choices possess the capacity to correct these disparities through socio-cultural empowerment and through equitable distribution of resources (Berkman & Kawachi, 2000). For instance, ethnic enclaves, the clustering of racial-ethnic groups within the same neighborhood, can buffer negative health consequences through political solidarity, social support and resource sharing (Ludwig et al., 2012; Vinikoor, Kaufman, MacLehose, & Laraia, 2008). Environmental context such as this has been shown to vary widely in communities across the nation, a variation that Black health outcomes are particularly sensitive to (Kramer and Hogue, 2008, Messer et al., 2006). Health scientists have examined the dynamic of race and socioeconomic status (SES) between individuals and communities using a variety of measures, including the congruity of an individual's income level (based upon race, education and marital status) with their neighbors (Collins et al., 1997, Pickett et al., 2005, Vinikoor et al., 2008, Kramer and Hogue, 2008, Pais et al., 2012), residential racial segregation (Massey & Denton, 1988), and statistical approaches such as principal component analysis or propensity score to depict the racial-income configuration (Harding, 2003, Schempf et al., 2009). Many of these health studies have used regression approaches to isolate the relative contributions of race and socioeconomic status; fewer have explicitly examined their interaction, either within or across levels. Residential mobility studies, which have focused upon the interaction of race and socioeconomic status, have consistently documented a dampened effect for upward-income movement by racial minorities (Pais et al., 2012), but with little focus upon the health outcomes associated with these patterns, and with mixed findings among the few health-related studies that do exist (Bruch, 2014, McFarland and Smith, 2009).
To secure racial-minority populations large enough to be investigated, community impact studies have examined ecological context within densely-populated urban centers such as New York City or Chicago (Grady, 2006, Pickett et al., 2005) using census tracts as the unit of analysis, or have selected macro units of analysis (state, county, metropolitan statistical areas) as their sample (Kramer & Hogue, 2008; Walton, 2009). Their generalizability to smaller communities and rural areas, where minorities are fewer in number and more geographically scattered remains unclear (White and Borrell, 2011, Yang and Matthews, 2015). In light of increasing numbers of racial minorities, their growing dispersal (Perez and Hirschman, 2009, Reardon et al., 2009), and the lack of research examining how race, socioeconomic status and neighborhood residence culminate into health, this is an important area of study. The goals of the current investigation were to examine the interrelationship of race and socioeconomic status upon infant birthweight at the individual and the census tract levels within a mid-sized, mixed urban-rural county in the Midwest; one marked by large racial disparities and high Black infant mortality rates.
Methods
The study was a multi-level analysis utilizing individual birth records and census tract datasets from 2010, joined using geographic information systems (GIS). Permission and access to the birth records data were provided by the Michigan Department of Community Health Vital Records and Health Statistics Section. Institutional Review Board approval was provided by Western Michigan University Human Subjects Institutional Review Board.
Setting
The study was conducted within Kalamazoo County located in Michigan, a Midwestern state within the United States. The study county has a population of 252,074 within a mix of rural and urban communities (Kalamazoo County Health and Community Services Department, 2013). More importantly for the purposes of this study, the county's maternal population is comparable to the nation's on race (18.4% Black compared to15.9% national Black, but with a high Black infant mortality rate (18.7 IMR per 1000 live births among Black women, 2006–2010 period) and high racial disparity (Black to White IMR disparity ratio of 3.5, 2006–2010 five-year moving average) (Centers for Disease Control and Prevention, 2012, Michigan Department of Community Health, 2014). The racial disparity in this community is substantially higher than in the State of Michigan (Black-White disparity ratio of 2.7) and the Nation (Black-White disparity ratio of 2.2) (Centers for Disease Control and Prevention, 2012, Michigan Department of Community Health, 2014).
Sample population
The study utilized nested populations of individuals residing within census tracts. The individual-level study sample was drawn from the population of 3119 women who were county residents when they gave birth in 2010. Exclusion criteria included multiple gestation birth, maternal race other than Black or White and having a non-geocodable address. After exclusion, the final individual-level population was 2861. Individual-level birth records were geo-coded using maternal address, and then linked to census tract (downloaded from the Michigan Geographic Data Library) in ArcGIS10.0. Census tracts commonly serve as proxies for neighborhood community units (Krieger et al., 2003, Ross and Mirowsky, 2001, Roux, 2003). Within this study, the community sample was the 57 census tracts within the county in 2010. The challenges to geocoding and successfully using geocoded data for health applications have been discussed extensively elsewhere (Goldberg & Jacquez, 2012). In this study, the primary challenges were incomplete or missing address information and reporting of post-office boxes in place of street address. The final study sample of 2861 women delivered 190 infants (6.6%) whose birthweight fell under the low birthweight (LBW) threshold of 2500 g. Black women accounted for 19.2% (n=550) of the final study population and White women 80.8% (n=2311). A little less than half (47.7%, n=1363) delivered an infant under Medicaid insurance, and the remaining 52.3% (n=1495) had private insurance.
Data collection and measures
Individual-level birth record data were obtained from the Michigan Department of Community Health Vital Records Division in 2012; final analyses were conducted 2014–2015. The following variables were abstracted from the 2010 birth records dataset for study use: Maternal address, infant birthweight, maternal race, and whether delivery was Medicaid-paid.
Outcome variable
Of the three most common birth outcome measures (birthweight, prematurity and mortality), birthweight is the most optimal measure for this investigation: it is a leading risk factor for mortality but with higher prevalence numbers, it represents two morbidity processes (gestation and intrauterine growth), and it is measured with greater reliability and accuracy than gestational age (Ma and Finch, 2010, Martin et al., 2015, Wilcox, 2001). Birthweight was measured in grams, and was further operationalized into two distinct outcomes, which were subsequently modeled together: (1) a dichotomous measure of LBW or not and (2) for all births within the not-LBW category, the actual continuous measure of birthweight, in grams. The dichotomous LBW measure was operationalized as birthweights below 2500 g coded as “LBW,” and birthweights at or above 2500 g coded as “above-LBW-threshold.” The continuous birthweight measure was operationalized as the actual birthweight, in grams, among all births occurring within the above-LBW-threshold sub-category. This combined-measure approach was implemented in order to simultaneously retain the precision of the continuous measure, while reducing the influence of extreme outliers at the low-end of the distribution without having to exclude them entirely from the analysis (Talge, Mudd, Sikorski, & Basso, 2014).
Predictor variables
Four predictor variables were used: race and socioeconomic status (SES) at the individual-level, and race and SES at the community-level. At the individual-level, predictors were dichotomized into Black or White (maternal race) and low-income or higher-income (derived from the Medicaid-paid birth variable, a proxy for maternal SES). Medicaid-paid birth was considered “low income,” while non-Medicaid, private insurance births were categorized as “higher-income.” At the community-level, predictors were abstracted from census tract data downloaded from the American Community Survey (http://www.census.gov/acs) for a five-year estimate (2006–2010) of race and SES. Community-level predictors were dichotomized into poverty-concentration or not (SES) and Black-concentration or not (race). The original downloaded measures were continuous (percent Black residents and percent of residents living below the Federal Poverty level). A cut-off for poverty was established at 20 percent for dichotomizing the SES variable, a threshold that has been previously validated to represent community-level poverty (Krieger et al., 2003). Similar to the approach used by other birth-outcome studies (Grady, 2006, Pickett et al., 2005, Vinikoor et al., 2008), racial dichotomization was based upon overall population prevalence; since we had 18.4% Blacks in the maternal population, a 20% threshold for neighborhood Black-concentration was implemented; an approach that offered the added benefit of maintaining operational consistency with the poverty measure. Given the study focus on the cumulative effects of race and SES, and the likelihood that traditional covariates (such as prenatal care, maternal disease and infection, maternal age, smoking) lay upon the causal pathway to birthweight, such control variables were not included in this analysis.
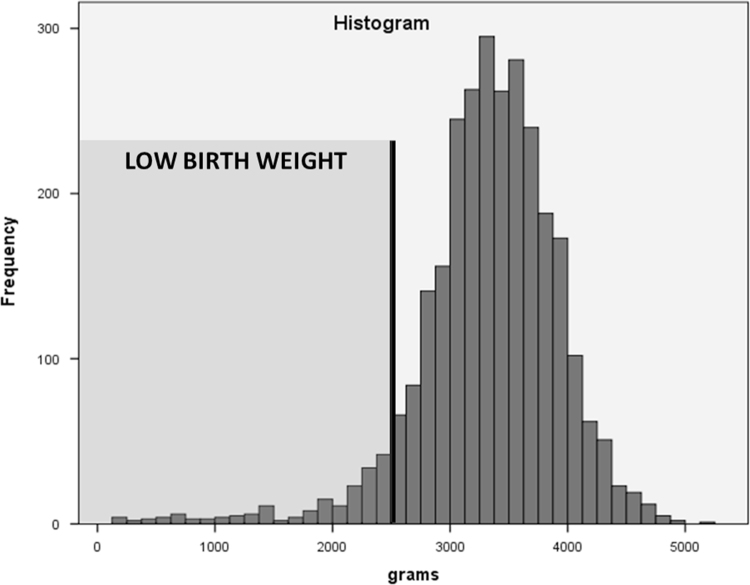
Statistical analysis
Bivariable relationships between predictors and between individual predictors and the outcome were assessed using Pearson Chi Square, using two-sided significance at the 95% confidence level. The multivariable relationship between individual-level and community-level race and SES were assessed using multilevel regression, with the following two- and three-way interaction terms testing specific relationships: (a) individual-level race and individual-level SES, (b) community-level race and community-level SES and (c) individual-level race, individual-level SES and community-level race. The histogram of birthweights in Fig. 1 shows longer left tails (left skewness) and this made standard regression technique with Gaussian distributional assumption unusable. This motivated the development of a two-part Bayesian statistical model. First we classified the birthweights into two groups: less than 2500 g that we designated as low birthweight (LBW) and greater than 2500 g. In our model, the chance of a mother having a LBW baby was modeled using probit link functions in terms race and SES variables. In the second part of the modeling, the birthweights at or above 2500 g were modeled using Truncated Normal Distribution, truncated at 2500 g. In order to have robust Bayesian inference, we set our prior distributions of regression coefficients noninformative (zero mean and 100 variance). By robust we mean that our inferences are not biased by subjectivity of the selection of priors. The technical details of our modeling approach and maps of the spatial correlation of the random intercepts for the individual-level main effects and interaction effects models can be found in the Appendix.
Fig. 1.
Histogram of Birth Weight Distribution.
Statistical inference was based on Bayesian credible intervals (CrI) computed as the 2.5th and 97.5th percentile of the posterior samples. Six models were explored for the analysis. The first model included only maternal race and SES, the second included only community level race and SES, the third model examined the interaction between maternal level race and SES, the fourth model examined the interaction between community level race and SES, and the fifth model included both the individual-level and the community-level terms. Lastly, the sixth model examined a three-way interaction between individual-level race, individual-level SES and community level race. The coefficients associated with the risk of LBW were transformed as odds ratios (OR). If the 95% credible interval for OR did not include 1, then an effect was concluded to be influential. Multicollinearity among predictors was assessed using variance inflation factor (VIF). The predictors in the models had VIF values below ten, indicating no multicollinearity (Fox & Monette, 1992). Assessment of model fitting was done using posterior predictive distribution capture rate. The full description of the model and results on the model validation can be found in the Appendix. SPSS was used to process the data and compute the chi-squared test. R (Team, 2014) and WINBUGS (Lunn, Thomas, Best, & Spiegelhalter, 2000) were used to implement the Bayesian two-part models.
Results
County, state and national characteristics
The study county, Kalamazoo MI, is similar to the state and to the nation on the primary outcome variable, low birthweight prevalence (Curtin et al., 2013, Martin et al., 2012, Michigan Department of Community Health, Division for Vital Records and Health Data Development, 2012, U.S. Census Bureau, 2014). Among women giving birth, Kalamazoo has the same proportion of White women as the state of Michigan and the nation as a whole, with slightly higher rates of Black women relative to other minority populations compared to the nation. The ratio of Black women giving birth relative to their population size is higher for Kalamazoo County (RR 1.46=18.4% delivering:12.6% population) than the state (RR 1.13=19.7%:17.4%) or nation (RR 1.17=15.9%:13.5%). Compared to the state and the nation, Kalamazoo County has the highest poverty indicators at both the community and maternal population levels (Table 1).
Table 1.
County, State and Nation on Selected Characteristics, 2010 Births.
| Maternal birth population | Kalamazoo county | Michigan | National | |
|---|---|---|---|---|
| N=3119% | N=114,531% | N=3,999,386% | ||
| LBW (<2500 g) | 8.1 | 8.4 | 8.1 | |
| Individual level predictors | Race: White | 76.8 | 76.2 | 76.7 |
| Race: Black | 18.4 | 19.7 | 15.9 | |
| Race: Other | 4.8 | 4.1 | 7.4 | |
| Medicaid-paid Birth | 47.8 | 45.4 | 44.9 | |
| Community Level predictors | Census tracts | N=57 | N= 2745 | N=73,172 |
| Average % | Average % | Average % | ||
| Race: White | 80.6, | 76.2 | 73.8 | |
| Race: Black | 12.6 | 17.4 | 13.5 | |
| Poverty | 20.8 | 18.2 | 16.3 |
Sources: Kalamazoo County statistics for individual-level (maternal birth population, percent low birthweight, percent by race and percent Medicaid) were derived from Michigan Department of Community Health, Division for Vital Records and Health Data Development, Live Birth File, 2010. National and Michigan statistics for individual-level (maternal birth population, percent low birthweight, percent by race and percent Medicaid) were drawn from published natality reports (Martin, 2012 NVSS; Curtin et al., 2013, NHVS). All statistics for community-level (average percent white and black residents, average percent living under the federal poverty rate) were extracted from exported American Community Survey data (http://www.census.gov/acs) using the five-year estimate (2006–2010).
Relationship between race and socioeconomic status (SES) among study population
Among the maternal study population, race and SES were statistically significantly associated with each other (χ2 (1)=387.919, p<.001). The relative rates of poverty among Black women were 2.2 times higher than White women: 85.4% (469/549) poverty among Black women compared to 38.7% (894/2309) poverty among White women.
The co-occurrence of race and SES was even more pronounced at the community-level. Eleven of fifty-seven census tracts had higher-density Black residents (20% or more residents were of Black race) and nineteen had higher-density poor residents (20% or more residents living at or below the federal poverty level). All eleven of the higher-density Black census tracts were in poverty areas, compared to eight of the thirty-eight higher-density White census tracts in poverty areas; a relative rate of 4.7 (100–21.5%).
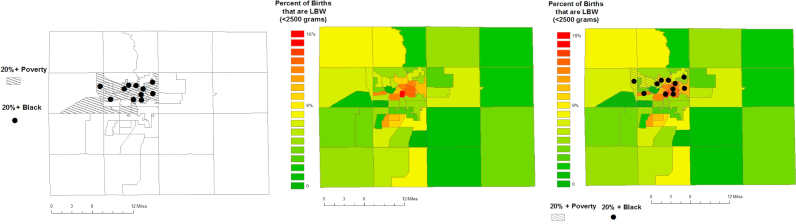
Distribution of race, SES and low birthweight concentrations across census tracts
The map in the first panel of Fig. 2 illustrates the concentration of poverty and Black race in neighborhoods at the urban core of Kalamazoo County. The middle map shows the variation of LBW prevalence, ranging from 0% to 18% of births, across the county, as well as the primary LBW hot spot, also in the urban core. A second LBW hot spot appears to be emerging in suburban communities south of the urban cluster. The final panel illustrates the overlap of concentrated poverty and Black residents in the larger, denser urban LBW cluster but not the smaller, suburban LBW cluster.
Fig. 2.
Spatial Distribution of Concentrated Poverty, Black Race and Low Birth Weight across Census Tracts in Kalamazoo County MI.
Analysis of race, SES and low birthweight
As a group, Black women were more likely to deliver low birthweight infants (10.9% Black LBW versus 5.6% White LBW, χ2 (1)=20.005, p<.001). When stratified by maternal poverty, low-SES White women had better outcomes than higher-SES Black women (7.7% low-SES White LBW vs 11.3% higher-SES Black LBW, χ2 (1)=20.067, p<.001). Further, while SES was associated with improved outcomes for White women (7.7% low-SES LBW to 4.3% higher-SES LBW, a reduction of 3.4%), it had no impact on outcomes for Black women as a group (10.9% low-SES LBW to 11.3% higher-SES LBW, a difference of 0.4%).
When neighborhood residence was taken into account, however, socioeconomic status showed benefit for both races: women fared the best when they had higher incomes and lived in racially-congruous neighborhoods (e.g., neighborhoods that had disproportionately high resident population of the same race as the individual). The lowest LBW prevalence were seen among higher-SES White women living in higher-White neighborhoods and among higher-SES Black women living in higher-Black neighborhoods. In fact, under these circumstances, Black women had the same birth outcomes as White women: 4.0% LBW and 4.1% LBW, respectively. Finally, while women in both races did poorer in non-racially-congruous neighborhoods, the worst combination was higher-SES Black women living in White neighborhoods, with a 14.5% LBW prevalence.
Bayesian multivariable modeling race and SES upon birthweight
As seen from the coefficients in Models 1 and 3 of Table 3, individual-level regression models, whether entered as independent main effects or as a single interaction term, produced the best posterior predictive distribution capture rates (95.27% and 95.01%, respectively), whereby maternal race and SES were each influential predictors of birthweight (based on 95% credible intervals). Adjusting for race, low SES was associated with 1.7 greater odds of LBW compared to higher SES. Adjusting for SES, being Black was associated with 1.6 times greater odds of LBW compared to being White. Adding community-level race and SES to the regression model as main effects (Model 2) or as a two-way community-level interaction (Model 4) had little impact; and did not add predictive value. Model 5, testing both two-way interactions together, had the lowest model fit statistics, indicating the most unstable regression. Finally, Model 6 tested the statistical influence of the three-way interaction effect of individual-level race, individual-level SES and community-level race upon birthweight, the relationships reported in Table 2. With the second lowest posterior predictive rate, this model has limited predictive power, likely influenced by the smaller cell sizes observed in Table 2's “Higher-SES Black column.” However, it is worth noting that the estimate for higher-SES Black women living in racially-congruous Black neighborhoods was the statistical equivalent of higher-SES White women living in racially-congruous White neighborhoods (the reference). In contrast, the estimate for higher-SES Black women living in White neighborhoods had the biggest point estimate difference from the reference group, although further testing should be completed to confirm this result. Given the level of similarity between results from the two parts of the Bayesian model, for parsimony only the probit model (LBW or not) is described in the main text of the manuscript. The truncated normal distribution model (actual birthweight grams) can be found in Table A5 in the Appendix. VIF assessment produced no evidence of multicollinearity among predictors.
Table 3.
Odds of delivering low birth weight infant: regression modeling individual- and community-level socio economic status and race.
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | ||
|---|---|---|---|---|---|---|---|
| Odds of LBW (logit): | Odds (95% CrI) | ||||||
| Individual SES | Higher-SES Women | (ref) | |||||
| Low-SES Women | 1.73 (1.27, 2.40) | ||||||
| Individual Race | White Women | (ref) | |||||
| Black Women | 1.59 (1.13, 2.22) | ||||||
| Community SES | Higher-SES Neighborhood | (ref) | |||||
| Low-SES Neighborhood | 0.99 (0.62, 1.52) | ||||||
| Community Race | White Neighborhood | (ref) | |||||
| Black Neighborhood | 1.58 (0.97, 2.64) | ||||||
| INTERACTION: Individual SES X Individual Race | Higher-SES White Women | (ref) | (ref) | ||||
| Low-SES White Women | 1.91 (1.35, 2.74) | 0.89 (3.61×10-9, 3.67×108) | |||||
| Higher-SES Black Women | 2.67 (1.15, 5.57) | 0.80 (0.47, 1.27) | |||||
| Low-SES Black Women | 2.71 (1.82, 3.97) | 1.05 (0.71, 1.55) | |||||
| INTERACTION: Community SES X Community Race | Higher-SES White Neighborhd | (ref) | (ref) | ||||
| Low-SES White Neighborhd | 1.26 (4.59×10-9,3.89×108) | 2.66 (1.22, 5.46) | |||||
| Higher-SES Black Neighborhd | 0.99 (0.61, 1.58) | 1.87 (1.30, 2.70) | |||||
| Low-SES Black Neighborhd | 1.57 (1.12, 2.21) | 2.65 (1.70, 4.15) | |||||
| INTERACTION: Individual SES X Individual Race X Community Race |
Higher SES White Women, in White Neighborhood | (ref) | |||||
| Low-SES White Women, in White Neighborhood | 1.99 (1.34, 2.96) | ||||||
| Higher-SES Black Women, in White Neighborhood | 3.87 (1.64, 8.27) | ||||||
| Low-SES Black Women, in White Neighborhood | 2.67 (1.59, 4.50) | ||||||
| Higher-SES White Women, in Black Neighborhood | 1.68 (0.66, 3.75) | ||||||
| Low-SES White Women, in Black Neighborhood | 2.10 (1.17, 3.64) | ||||||
| Higher-SES Black Women, in Black Neighborhood | 0.57 (0.03, 3.84) | ||||||
| Low-SES Black Women, in Black Neighborhood | 3.01 (1.87, 4.79) | ||||||
| [Model Fit]* | Posterior predictive distribution capture rate | 95.27% | 70.55% | 95.01% | 73.41% | 54.43% | 69.58% |
Higher rate values indicate better model fit.
Table 2.
Kalamazoo County Prevalence of Low Birth Weight, Stratified by Maternal SES, Maternal Race and Community Residence.
|
Low birth weight prevalence (with confidence interval) |
||||
|---|---|---|---|---|
|
White |
Black |
|||
| Low-SES | Higher-SES | Low-SES | Higher-SES | |
| Living in Higher SES Black Neighborhood | N=216 | N=99 | N=245 | N=25 |
| % | % | % | % | |
| 8.3 | 7.1 | 11.4 | 4.0 | |
| Living in Higher SES White Neighborhood | N=678 | N=1316 | N=224 | N=55 |
| % | % | % | % | |
| 7.5 | 4.1 | 10.3 | 14.5 | |
Notes: Three subjects are excluded due to missing Medicaid-status values.
Discussion
In a mid-sized community marked by high Black infant mortality, we observed the same association between being Black, being poor and living in a poor neighborhood that is seen in larger communities across the nation. Further, we found that individual-level race and socioeconomic status were more strongly associated with birthweight than were neighborhood-level racial and poverty factors. Study results regarding the proximal effect of individual-level race and SES upon birth outcomes, as well as the magnitude of these effects, is comparable to previous research, including another Michigan-based study by Debbink & Bader (Debbink and Bader, 2011, Grady, 2006). However, our study's non-significant result for community-level racial and economic factors stands in contrast to prior research (Kramer and Hogue, 2008, Pickett et al., 2005, Schempf et al., 2009, Vinikoor et al., 2008; Walton, 2009). Our weaker neighborhood effects could be a function of living in a smaller community; residential mobility researchers have shown that the dynamics between race, SES and neighborhood residence vary based upon population size and that, together, these factors collectively impact population health (Kramer and Hogue, 2008, Pais et al., 2012, Blanchard et al., 2004). Alternatively, our negligible neighborhood effect could be due to methodological features of the current study, potentially including the spatial unit of analysis used (census tract versus metropolitan area, region or state), the operationalization of key constructs (particularly the way race and SES were measured at the neighborhood level), or the smaller sample size, a natural outgrowth of examining this phenomenon in a mid-sized community.
While individual-level effects overshadowed community-level effects in the multivariable modeling, findings of racial equivalence in the three-way model suggest equity may have been achieved when Black women had the combined circumstances of higher incomes and residence in Black neighborhoods. Study women who were Black race, had non-Medicaid deliveries, and lived in census tracts with disproportionate Black residents had LBW prevalence of 4.0%, and were statistically similar to their White counterparts (non-Medicaid delivery, live in census tracts with disproportionate White residents) who had LBW prevalence of 4.1%. Similarly, another study by Grady (2010), in Detroit, Michigan, found that, controlling for neighborhood poverty, racial disparities in birth outcomes were reduced when Black women lived in more segregated Black neighborhoods. Multiple studies have documented the degree to which the physical, social, economic and political environment structures stress as well as protection, all of which subsequently interact with individuals’ circumstances to produce health behaviors and outcomes (Culhane and Elo, 2005, Grady, 2006, Kramer and Hogue, 2008, Schempf et al., 2009). Higher-SES families that live within disadvantaged neighborhoods have more buffering resources and mobility options than their neighbors, which can mitigate the health impact of their environment (Harding, 2003). While studies have yielded mixed evidence regarding the protectiveness conferred by ethnic enclaves (Ludwig et al., 2012; Morenoff, 2003; Pickett et al., 2005), current findings suggest that they may be protective if ones’ personal socioeconomic status within them is comparatively high. This is consistent with research showing that relative social and economic status are stronger predictors of health than objective measures of income and wealth (Adler & Snibbe, 2003; Adler, 2013; Smith & Huo, 2014). Researchers have found that perceptions of higher social status, regardless of objective SES measures, are associated with increased gray matter in the brain, more successful negotiation of life circumstances and less stress related physiological responses (Eisenberger, 2007, Gianaros et al., 2007).
This can work in reverse, as well. Experiencing relative deprivation, the perception of having fewer resources and lower social value compared to others can lead to social disenfranchisement, mental distress and ill health (Aneshensel, 2015, Pearlin, 2010, Smith and Huo, 2014). Regression modeling of birth outcomes clearly demonstrated that maternal race and socioeconomic status independently contributed risk to birth outcomes. After taking into account individual SES, Black women still had 1.6 greater odds of delivering a low birthweight infant than their White counterparts. A substantial body of research has documented that social stigma and racism account for much of the health disparities that persist after SES is taken into account (Aiello and Kaplan, 2009, Geronimus et al., 2006, Hatzenbuehler et al., 2013). The cumulative effect of social devaluation, covert as well as overt acts of discrimination, and the costs of code-switching (having to adapt speech, posture and ways of interacting for daily life within a white-dominated society) have been tied to physiological weathering and ill health (Aneshensel, 2015, Cross, 2012, Holzman et al., 2009, Sue et al., 2009).
The finding that the highest Black LBW prevalence (14.5%), and the greatest statistical gap in the three-way analysis, was experienced by higher SES Black women living in White neighborhoods further supports the notion that SES alone is not enough to counteract race-based disparities. Lewis (2015) identified several coping strategies implemented by Black professionals and college students: some stress-reducing, such as collective coping (leaning on one's support network), using ones’ voice as power and actively resisting Eurocentric standards (Brondolo et al., 2009, Cross, 2012, Lewis et al., 2015, Sue et al., 2009), and some stress-inducing, such as becoming desensitized and overcompensating (becoming Black superwoman) (Aneshensel, 2015, Holzman et al., 2009, Woods-Giscombe, 2010). Community-level studies have documented the pathways by which racial and socioeconomic residential congruity are linked to social support and well-being. In a randomized controlled trial of a housing vouchered move to a higher income neighborhood, Kessler et al. (2014) documented greater social isolation and psychological distress accompanying such a move, exacerbated when a social group is greatly outnumbered in the new environment (Kessler et al., 2014). Still other researchers have found that experiencing discrimination in isolation, as an individual rather than as a group, accelerates its weathering effect upon psychological and physical health (Aneshensel, 2015, Pearlin, 2010, Smith and Huo, 2014). While less research has been conducted regarding effective strategies for addressing racial stress and disempowerment, the following approaches have shown promise: practicing interpersonal responses to discrimination (Brondolo et al., 2009), stress-reduction skill building (Brondolo et al., 2009, Collins et al., 2004), culturally adapting healthcare delivery using community health workers, including racial congruity with provider and provider training in cultural respect (Anderson et al., 2015, Horvat et al., 2014, Lewin et al., 2010, Sue et al., 2009), and collective action that increases group solidarity, strengthens social networks and empowers political movement (Anderson et al., 2015, Aneshensel, 2015, Pearlin, 2010, Smith and Huo, 2014).
The health disadvantage that accompanied poverty in the study population is found throughout health research. Socioeconomic status, regardless of how it is measured (insurance status, education, household income, poverty level, wealth), has a strong graded relationship with maternal and fetal-infant health (intrauterine growth, prematurity, chronic disease, mortality, physical and mental health functioning) (Eudy, 2009, Harding, 2003, McLeod and Nonnemaker, 2000; Nepomnyaschy, 2009; Walton et al., 2009). The relatively high poverty rate within the study county compared to the state and the nation illustrates that maternal populations such as these may have elevated exposure to this psychosocial risk. The even higher poverty rate among Black study women (85.4%, 2.2RR) is consistent with disproportionate Black poverty observed throughout the nation and partially explains the poorer birth outcomes and infant mortality suffered by Black populations. Maternal-infant programs shown to mitigate health risks associated with poverty have accomplished this by increasing access to healthcare through universal insurance, home visiting providers and Federally Qualified Health Centers (Avellar et al., 2012, Khanani et al., 2010; Kothari, Zielinski, James, Charoth, & del Carmen Sweezy, 2014; Roman, Raffo, Zhu, & Meghea, 2014; Shi, Stevens, Wulu, Politzer, & Xu, 2004), improving nutrition through WIC (Avellar et al., 2012, Khanani et al., 2010, Kothari et al., 2014, Roman et al., 2014, Shi et al., 2004), increasing health literacy through community health workers (Anderson et al., 2015, Horvat et al., 2014, Lewin et al., 2010), and enhancing social support with peers and mentors (Avellar et al., 2012, Ickovics et al., 2007, Meghea et al., 2016).
Research documenting higher morbidity and mortality among Black populations, after accounting for SES, are plentiful, but few racial gaps are as wide as that in the study county. It has been suggested that the micro-systems created within mid-sized communities have differential impact upon its residents, particularly Black populations who may be more sensitized to environmental conditions, than those created within larger denser areas. Certainly, spatial proximity increases social interaction and the sharing of social institutions. Furthermore, studies have documented that racial segregation can vary based upon geographic scale, such that micro units, like census tracts, may generate different segregation indicators than larger, equally relevant, units of analysis, such as metropolitan area; both, in turn, may have their own independent effects upon health (Reardon et al., 2009). To date, much of the spatial analysis of maternal-infant health has focused upon more densely concentrated urban areas or larger geographic units of analysis (Kawachi and Berkman, 2003, Kramer and Hogue, 2008, Winkleby et al., 2006), and few of the discrimination-and-birth outcome studies include measures of neighborhood geography (Dole et al., 2003, Rankin et al., 2011, SlaughterAcey et al., 2016).
Limitations
The current study had many of the limitations associated with secondary analysis designs. Measures of the two key indicators, income and race, were crude, of single dimension and lacked gradation. There were no measures of internal states, such as experiences of stress or perceptions of racism, to link SES and race to birth outcomes, leaving these relationships to be inferred. Similarly, there were no measures of neighborhood features (pollution, dilapidated housing, public transportation, etc.); features that further reflect structured discrimination, but also can mediate the effects of institutionalized racism. The large interval observed in two cells of Table 3 (Models 4 and 5) may be due to an improper posterior probability distribution which suggests the prior distribution assumption needs to be investigated further. Finally, the individual and census tract sample size was smaller than comparable studies, which may have limited its statistical power and its ability to detect interaction effects.
Conclusion
This study adds to the literature by documenting the complex interaction of race, SES and neighborhood upon birth outcomes within a community that typifies large geographic swathes of the U.S. and that displays wide racial health disparities: individual-level race and socioeconomic status outweigh community-level factors regarding birth outcomes, maternal Black race and low socioeconomic status are independently associated with increased risk of low birthweight, and neighborhood racial congruity may be associated with risk-mitigation, while racial incongruity may be associated with risk-exacerbation.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ssmph.2016.09.011.
Contributor Information
Catherine L. Kothari, Email: catherine.kothari@med.wmich.edu.
Rajib Paul, Email: rajib.paul@wmich.edu.
Ben Dormitorio, Email: Benedict.Dormitorio@PAREXEL.com.
Fernando Ospina, Email: fernando@eracce.org.
Arthur James, Email: arthur.james2@osumc.edu.
Deb Lenz, Email: dllenz@kalcounty.com.
Kathleen Baker, Email: kathleen.baker@wmich.edu.
Amy Curtis, Email: amy.curtis@wmich.edu.
James Wiley, Email: james.wiley@ucsf.edu.
Appendix A. Supplementary material
Supplementary material
.
References
- Adler N.E., Snibbe A.C. The role of psychosocial processes in explaining the gradient between socioeconomic status and health. Current Directions in Psychological Science. 2003;12(4):119–123. [Google Scholar]
- Adler N.E. Health disparities: Taking on the challenge. Perspectives on Psychological Science: A Journal of the Association for Psychological Science. 2013;8(6):679–681. doi: 10.1177/1745691613506909. [DOI] [PubMed] [Google Scholar]
- Aiello A.E., Kaplan G.A. Socioeconomic position and inflammatory and immune biomarkers of cardiovascular disease: applications to the panel study of income dynamics. Biodemography and Social Biology. 2009;55(2):178–205. doi: 10.1080/19485560903382304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alio A.P., Richman A.R., Clayton H.B., Jeffers D.F., Wathington D.J., Salihu H.M. An ecological approach to understanding black-white disparities in perinatal mortality. Maternal and Child Health Journal. 2009;14:557. doi: 10.1007/s10995-009-0495-9. [DOI] [PubMed] [Google Scholar]
- Anderson L.M., Adeney K.L., Shinn C., Safranek S., Buckner-Brown J., Krause L.K. Community coalition-driven interventions to reduce health disparities among racial and ethnic minority populations (review) The Cochrane Collaboration. 2015;(6) doi: 10.1002/14651858.CD009905.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aneshensel C.S. Sociological inquiry into mental health: The legacy of leonard I. pearlin. Journal of Health and Social Behavior. 2015;56(2) doi: 10.1177/0022146515583992. [DOI] [PubMed] [Google Scholar]
- Avellar, S., Paulsell, D., SamaMiller, E., & DelGrosso, P.. (2012). Home visiting evidence of effectiveness review: Executive summary october 2012. Mathematica Policy Research Inc.
- Berkman L.F., Kawachi I., editors. Social epidemiology. Oxford University Press; New York: 2000. [Google Scholar]
- Blanchard T., Crossman J., Levin M. Multiple meanings of minority concentration: incorporating contextual explanations into the analysis of individual-level U.S. black mortality outcomes. Population Research and Policy Review. 2004;23:309. [Google Scholar]
- Bloome D. Racial inequality trends and the intergenerational persistence of income and family structure. American Sociological Review. 2014;79(6):1196. doi: 10.1177/0003122414554947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brondolo E., Gallo L.C., Myers H.F. Race, racism and health: Disparities, mechanism and interventions. Journal of Behavioral Medicine. 2009;32(1):1. doi: 10.1007/s10865-008-9190-3. [DOI] [PubMed] [Google Scholar]
- Bruch E.E. How population structure shapes neighborhood segregation. American Journal of Sociology. 2014;119(5):1221. doi: 10.1086/675411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2012). Infant mortality. Retrieved from: 〈http://www.cdc.gov/reproductivehealth/maternalinfanthealth/infantmortality.htm〉.
- Central Intelligence Agency (CIA). (2014). The world factbook. Retrieved from: 〈https://www.cia.gov/library/publications/the-world-factbook/rankorder/2091rank.html〉.
- Collins J.W., Jr, David R.J., Handler A., Wall S., Andes S. Very low birthweight in african american infants: The role of maternal exposure to interpersonal racial discrimination. American Journal of Public Health. 2004;94(12):2132. doi: 10.2105/ajph.94.12.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins J.W., Herman A.A., David R.J. Very-low-birthweight infants and income incongruity among african american and white parents in chicago. American Journal of Public Health. 1997;87(3):414. doi: 10.2105/ajph.87.3.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook B.L., McGuire T.G., Zuvekas S.H. Measuring trends in racial/ethnic health care disparities. Medical Care Research and Review. 2009;66(1):23. doi: 10.1177/1077558708323607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper D., McCausland W.D., Theodossiou I. Income inequality and wellbeing: The plight of the poor and the curse of permanent inequality. Journal of Economic Issues. 2013;47(4):939. [Google Scholar]
- Cross W.E., Jr. The enactment of race and other social identities during everyday transactions. In: Wijeyesinghe C.L., Jackson B.W. III, editors. New perspectives on racial indentity development. Second ed. New York University Press; New York, NY: 2012. [Google Scholar]
- Culhane J.F., Elo I.T. Neighborhood context and reproductive health. American Journal of Obstetrics and Gynecology. 2005:192. doi: 10.1016/j.ajog.2005.01.071. [DOI] [PubMed] [Google Scholar]
- Curtin S.C., Osterman M.J.K., Uddin S.F., Sutton S.R., Reed P.R. Vol. 62. Center for Disease Control and Prevention, National Center for Health Statistics; 2013. Source of payment for the delivery: births in a 33-state and district of columbia reporting area, 2010. (number 5) [PubMed] [Google Scholar]
- David R. Inequality matters: Infant mortality in the global village. Joint Center for Political and Economic Studies; Washington, D.C: 2007. [Google Scholar]
- Debbink M.P., Bader M.D.M. Racial residential segregation and low birth weight in Michigan’s metropolitan areas. American Journal of Public Health. 2011;101(9):1714. doi: 10.2105/AJPH.2011.300152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derose K.P., Gresenz C.R., Ringel J.S. Understanding disparities in health care addess, and reducing them, through a focus on public health. Health Affairs. 2011;30(10):1844–1851. doi: 10.1377/hlthaff.2011.0644. [DOI] [PubMed] [Google Scholar]
- Diez Roux A.V. Conceptual approaches to the study of health disparities. Annual Review of Public Health. 2012;33:41. doi: 10.1146/annurev-publhealth-031811-124534. doi:0163-7525/12/0421-0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dole N., Savitz D.A., HertzPicciotto I., SiegaRiz A.M., McMahon M.J., Buekens P. Maternal stress and pretern birth. American Journal of Epidemiology. 2003;157(1) doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- Eisenberger N.I. Using neuroimaging techniques to explore the relationship between social status and health. Social Cognitive and Affective Neuroscience. 2007;2(3):159–160. [Google Scholar]
- Eudy R.L. Infant mortality in the lower mississippi delta: Geography, poverty and race. Maternal and Child Health Journal. 2009;13(6):806–813. doi: 10.1007/s10995-008-0311-y. [DOI] [PubMed] [Google Scholar]
- Fox J., Monette G. Generalized collinearity diagnostics. Journal of the American Statistical Association. 1992;87(417):178–183. doi: 10.1080/01621459.1992.10475172. [DOI] [PubMed] [Google Scholar]
- Fuller-Thomson E., Nuru-Jeter A., Minkler M., Guralnik J.M. Black – white disparities in disability among older americans: Further untangling the role of race and socioeconomic status. Journal of Aging and Health. 2009;21(5):677. doi: 10.1177/0898264309338296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus A.T., Hicken M., Keene D., Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the united states. American Journal of Public Health. 2006;96(5):826. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianaros P.J., Horenstein J.A., Cohen S., Matthews K.A., Brown S.M., Flory J.D., Hariri A.R. Perigenual anterior cingulate morphology covaries with perceived social standing. Social Cognitive and Affective Neuroscience. 2007;2(3):161–173. doi: 10.1093/scan/nsm013. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg D.W., Jacquez G.M. Advances in geocoding for the health sciences. Spatial and Spatio-Temporal Epidemiology. 2012;3(1):1–5. doi: 10.1016/j.sste.2012.02.001. [DOI] [PubMed] [Google Scholar]
- Grady S.C. Racial disparities in low birthweight and the contribution of residential segregation: A multilevel analysis. Social Science Medicine. 2006:63. doi: 10.1016/j.socscimed.2006.08.017. [DOI] [PubMed] [Google Scholar]
- Grady S.C. Racial residential segregation impacts on low birth weight using improved neighborhood boundary definitions. Spatial and Spatio-temporal Epidemiology. 2010;1:239–249. doi: 10.1016/j.sste.2010.09.006. [DOI] [PubMed] [Google Scholar]
- Harding D.J. Counterfactual models of neighborhood effects: The effect of neighborhood poverty on dropping out and teenage pregnancy. American Journal of Sociology. 2003;109(3):676. doi:0002-9602/2003/10903-0004. [Google Scholar]
- Hatzenbuehler M.L., Phelan J.C., Link B.G. Stigma as a fundamental cause of population health inequalities. American Journal of Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward M.D., Miles T.P., Crimmins E.M., Yang Y. The significance of socioeconomic status in explaining the racial gap in chronic health conditions. American Sociological Review. 2000;65(6):910–930. Retrieved from: 〈 http://search.proquest.com.proxy2.cl.msu.edu.proxy1.cl.msu.edu/docview/215849319?accountid=12598〉. [Google Scholar]
- Holzman C., Eyster J., Kleyn M., Messer L.C., Kaufman J.S., Laraia Barbara A.…Elo Irma T. Maternal weathering and risk of preterm delivery. American Journal of Public Health. 2009;99(10) doi: 10.2105/AJPH.2008.151589. Retrieved from: 〈 http://search.proquest.com/docview/215095334?accountid=12598〉. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvat L., Horey D., Romios P., Kis-Rigo J. Cultural competence education for health professionals (review) The Cochrane Collaboration. 2014;(5) doi: 10.1002/14651858.CD009405.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ickovics J.R., Kershaw T.S., Westdahl C., Magriples U., Massey Z., Reynolds H., SchindlerRising S. Group prenatal care and perinatal outcomes. Obstetrics Gynecology. 2007 doi: 10.1097/01.AOG.0000275284.24298.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalamazoo County Health and Community Services Department. (2013). Health surveillance data book: Population. Retrieved from: 〈http://www.kalcounty.com/hsd/pdf_files/Sect1_1SurveillanceBook.pdf〉.
- Kawachi I., Berkman L.F., editors. Neighborhoods and health. Oxford University Press; New York: 2003. [Google Scholar]
- Kessler R.C., Duncan G.J., Gennetian L.A., Katz L.F., Kling J.R., Sampson N.A., Ludwig J. Associations of housing mobility interventions for children in high-poverty neighborhoods with subsequent mental disorders during adolescence. Journal of American Medical Association. 2014;311(9):937. doi: 10.1001/jama.2014.607. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Khanani I., Elam J., Hearn R., Jones C., Maseru N. The impact of prenatal WIC participation on infant mortality and racial disparities. American Journal of Public Health. 2010;100(S1):S204. doi: 10.2105/AJPH.2009.168922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kothari C.L., Zielinski R., James A., Charoth R.M., DelCarmenSweezy L. Improved birth weight for black infants: Outcomes of a health start program. American Journal of Public Health. 2014;104(S1) doi: 10.2105/AJPH.2013.301359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer M.R., Hogue C.R. Place matters: Variation in the black/white very preterm birth rate across U.S. metropolitan areas, 2002–2004. Public Health Reports. 2008;123:576. doi: 10.1177/003335490812300507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Discrimination and health inequities. International Journal of Health Services. 2014;44(4):643. doi: 10.2190/HS.44.4.b. [DOI] [PubMed] [Google Scholar]
- Krieger N., Chen J.T., Waterman P.D., Soobader M.J., Subramanian S.V., Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: the public health disparities geocoding project (US) Journal of Epidemiol Community Health. 2003;57:186. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist T.A. Disentangling race and socioeconomic status: A key to understanding health inequalities. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2005;82(2) doi: 10.1093/jurban/jti061. iii26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin S., MunabiBabigumira S., Glenton C., Daniels K., BoschCapblanch X., Vanwyk B.E., Scheel I.B. Lay health workers in primary and community health care for maternal and child health and the management of infections diseases (review) The Cochrane Collaboration. 2010;(3) doi: 10.1002/14651858.CD004015.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis T.T., Cogburn C.D., Williams D.R. Self-reported experiences of discrimination and health: Scientific advances, ongoing controversies, and emerging issues. Annual Review of Psychology. 2015:11. doi: 10.1146/annurev-clinpsy-032814-112728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995:80. [PubMed] [Google Scholar]
- Lu M.C., Halfon N. Racial and ethnic disparities in birth outcomes: A life-course perspective. Maternal and Child Health Journal. 2003;7(1):13. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
- Ludwig J., Duncan G.J., Gennetian L.A., Katz L.F., Kessler R.C., Kling J.R., Sanbonmatsu L. Neighborhood effects on the long-term well-being of low-income adults. Science. 2012;337(6101):1505–1510. doi: 10.1126/science.1224648. doi:337/6101/1505 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunn D.J., Thomas A., Best N., Spiegelhalter D. WinBUGS-a bayesian modelling framework: Concepts, structure, and extensibility. Statistics and Computing. 2000;10(4):325–337. [Google Scholar]
- Ma S., Finch B.K. Birth outcome measures and infant mortality. Population Research and Policy Review. 2010;29:865. [Google Scholar]
- Martin, J. A., Hamilton, B. E., Ventura, S. J., Osterman, M. J. K., Wilson, E. C., Mathews, T. J., & and Division of Vital Statistics. (2012). Births: Final data for 2010. [PubMed]
- Martin J.A., Osterman M.J.K., Kirmeyer S.E., Gregory E.C.W. Measuring gestational age in vital statistics data: trainsitioning to the obstetric estimate. National Vitatl Statistics Reports. 2015;64(5) [PubMed] [Google Scholar]
- Massey D.S., Denton N., A. The dimensions of residential segregation. Social Forces. 1988;67(2):281. [Google Scholar]
- McFarland M., Smith C.A. Segregation, race, and infant well-being. Population Research and Policy Review. 2009;30:467. [Google Scholar]
- McLeod J.D., Nonnemaker J.M. Poverty and child emotional and behavioral problems: Racial/ethnic differences in processes and effects. Journal of Health and Social Behavior. 2000;41(2):137–161. Retrieved from: 〈 http://search.proquest.com.proxy2.cl.msu.edu.proxy1.cl.msu.edu/docview/201672219?accountid=12598〉. [Google Scholar]
- Meghea C.I., You Z., Raffo J., Leach R.E., Roman L.A. Statewide medicaid enhanced prenatal care programs and infant mortality. Pediatrics. 2016;136(2) doi: 10.1542/peds.2015-0479. [DOI] [PubMed] [Google Scholar]
- Messer L.C., Kaufman J.S., Dole N., Savitz D.A., Laraia B.A. Neighborhood crime, deprivation and preterm birth. Annals of Epidemiology. 2006;16:455–462. doi: 10.1016/j.annepidem.2005.08.006. [DOI] [PubMed] [Google Scholar]
- Michigan Department of Community Health. (2014). Michigan infant death statistics january 1 through december 31, 2012. (Statistical Report). Michigan Department of Community Health.
- Michigan Department of Community Health. (2012). Division for vital records and health data development. Live birth file.
- Morenoff J.D. Neighborhood mechanisms and the spatial dynamics of birth weight1. American Journal of Sociology. 2003;108(5):976–1017. doi: 10.1086/374405. [DOI] [PubMed] [Google Scholar]
- Murphy S.L., Xu J., Kochanek K.D. Deaths: Final data for 2010. National Vital Statistics Report. 2013;61(4) [PubMed] [Google Scholar]
- Nepomnyaschy L. Socioeconomic gradients in infant health across race and ethnicity. Maternal and Child Health Journal. 2009;13(6):720–731. doi: 10.1007/s10995-009-0490-1. [DOI] [PubMed] [Google Scholar]
- Nicklett E.J. Socioeconomic status and race/ethnicity independently predict health decline among older diabetics. BMC Public Health. 2011;11:684. doi: 10.1186/1471-2458-11-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oishi S., Kesebir S., Diener E. Income inequiality and happiness. Psychological Science. 2011;22:1095–1100. doi: 10.1177/0956797611417262. [DOI] [PubMed] [Google Scholar]
- Orsi J.M., Margellos-Anast H., Whitman S. Black-white health disparities in the united states and chicago: A 15 year progress analysis. American Journal of Public Health. 2010;100(2):349. doi: 10.2105/AJPH.2009.165407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osypuk T.L., Galea S., McArdle N., Acevedo-Garcia D. Quantifying separate and unequal racial-ethnic distributions of neighborhood poverty in metropolitan america. Urban Affairs Review. 2009;45(1):25. doi: 10.1177/1078087408331119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pais J., South S.J., Crowder K. Metropolitan heterogeneity and minority neighborhood attainment: spatial assimilation or place stratification? Social Problems. 2012;59(2):258. doi: 10.1525/sp.2012.59.2.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin L.I. The life course and the stress process: Some conceptual comparisons. The Journals of Gerontology.Series B, Psychological Sciences and Social Sciences. 2010;65B(2):207–215. doi: 10.1093/geronb/gbp106. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez A.D., Hirschman C. The changing racial and ethnic composition of the US population: Emerging american identities. Population and Development Review. 2009;35(1):1–51. doi: 10.1111/j.1728-4457.2009.00260.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett K.E., Collins J.W., Masi C.M., Wilkinson R.G. The effects of racial density and income incongruity on pregnancy outcomes. Social Science Medicine. 2005;60(10):2229–2238. doi: 10.1016/j.socscimed.2004.10.023. [DOI] [PubMed] [Google Scholar]
- Pollack C.E., Cubbin C., Sania A., Hayward M., Vallone D., Flaherty B., Braveman P.A. Do wealth disparities contribute to health disparities within racial/ethnic groups? Journal of Epidemiology Community Health. 2013;67:439. doi: 10.1136/jech-2012-200999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popay J., Escorel S., Hernandez H., Johnston H., Mathieson L., Rispel L. Understanding and tackling social exclusion: final report to the WHO commission on social determinants of health from the social exclusion knowledge network. WHO Social Exclusion Knowledge Network. 2008 [Google Scholar]
- Rankin K.M., David R.J., Collins J.W.J. African american women’s exposure to interpersonal racial discrimination in public settings and preterm birth: The effect of coping behaviors. Ethnicity Disease. 2011;21(3):370. [PubMed] [Google Scholar]
- Reardon S.F., Farrell C.R., Matthews S.A., O’Sullivan D., Bischoff K., Firebaugh G. Race and space in the 1990s: Changes in the geographic scale of racial residential segregation, 1990–2000. Social Science Research. 2009;38(1):55–70. doi: 10.1016/j.ssresearch.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roman L., Raffo J.E., Zhu Q., Meghea C.I. A statewide medicaid enhanced prenatal care program impact on birth outcomes. JAMA Pediatrics. 2014;168(3) doi: 10.1001/jamapediatrics.2013.4347. [DOI] [PubMed] [Google Scholar]
- Ross C.E., Mirowsky J. Neighborhood disadvantage, disorder, and health. Journal of Health and Social Behavior. 2001:258–276. [PubMed] [Google Scholar]
- Roux A.D. The examination of neighborhood effects on health: Conceptual and methodological issues related to the presence of multiple levels of organization. Neighborhoods and Health. 2003:45–64. [Google Scholar]
- Schempf A., Strobino D., O’Campo P. Neighborhood effects on birthweight: An exploration of psychosocial and behavioral pathways in baltimore, 1995–1996. Social Science Medicine. 2009:68. doi: 10.1016/j.socscimed.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L., Stevens G., Wulu J.T., Politzer R.M., Xu J. America’s health centers: Reducing racial and ethnic disparities in perinatal care and birth outcomes. Health Services Research. 2004;39(6) doi: 10.1111/j.1475-6773.2004.00323.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SlaughterAcey J.C., SealyJefferson S., Helmkamp L., Caldwell C.H., Osypuk T.L., Platt R.W., Misra D.P. Racism in the form of micro agressions and the risk of preterm birth among black women. Annals of Epidemiology. 2016:26. doi: 10.1016/j.annepidem.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley B.D., Stith A.Y., Nelson A.R., editors. Unequal treatment: Confronting racial and ethnic disparities in health care. The National Academies Press; Washington, D.C: 2003. [PubMed] [Google Scholar]
- Smith H.J., Huo Y.J. Relative deprivation: How subjective experiences of inequality influence social behavior and health. Policy Insights from the Behavioral and Brain Sciences. 2014;1(1):231. [Google Scholar]
- Sue S., Zane N., NagayamaHall G.C., Berger L.K. The case for cultural competency in psychotherapeutic interventions. Annual Review of Psychology. 2009:60. doi: 10.1146/annurev.psych.60.110707.163651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talge N.M., Mudd L.M., Sikorski A., Basso O. United states birth weight reference corrected for implausible gestational age estimates. Pediatrics. 2014;133:844. doi: 10.1542/peds.2013-3285. [DOI] [PubMed] [Google Scholar]
- Team R.C. R Foundation for Statistical Computing; Vienna, Austria: 2014. R: A Language and Environment for Statistical Computing; p. 2013. [Google Scholar]
- U.S. Census Bureau. (2014). American community survey design and methodology, version 2.0.
- U.S. Department of Health and Human Services. (2014). Healthy people 2020 leading health indicators: Progress update. (Executive Summary). U.S. Department of Health and Human Services.
- Vinikoor L.C., Kaufman J.S., MacLehose R.F., Laraia B.A. Effects of racial density and income incongruity on pregnancy outcomes in less segregated communities. Social Science Medicine. 2008;66(2):255–259. doi: 10.1016/j.socscimed.2007.08.016. [DOI] [PubMed] [Google Scholar]
- Walton E. Residential segregation and birth weight among racial and ethnic minorities in the united states. Journal of Health and Social Behavior. 2009;50(4):427. doi: 10.1177/002214650905000404. [DOI] [PubMed] [Google Scholar]
- Walton M.A., Murray R., Cunningham R.M., Chermack S.T., Barry K.L., Booth B.M., Blow F.C. Correlates of intimate partner violence among men and women in an inner city emergency department. Journal of Addictive Diseases. 2009;28(4):366–381. doi: 10.1080/10550880903183018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K., Borrell L.N. Racial/ethnic residential segregation: Framing the context of health risk and health disparities. Health Place. 2011;17(2):438–448. doi: 10.1016/j.healthplace.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox A.J. On the importance - and the unimportance – of birth weight. International Journal of Epidemiology. 2001;30:1233. doi: 10.1093/ije/30.6.1233. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports. 2001;116:404. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkleby M., Cubbin C., Ahn D. Effect of cross-level interaction between individual and neighborhood socioeconomic status on adult mortality rates. American Journal of Public Health. 2006;96(12):2145. doi: 10.2105/AJPH.2004.060970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods-Giscombe C.L. Superwoman schema: african american women’s views on stress, strength and health. Qualitative Health Research. 2010;20(5):668. doi: 10.1177/1049732310361892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2014). Health status indicators. Retrieved from: 〈http://www.who.int/whosis/indicatordefinitions/en/〉.
- Yang T., Matthews S.A. Death by segregation: Does the dimension of racial segregation matter? PLoS One. 2015;10(9):e0138489. doi: 10.1371/journal.pone.0138489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziersch A.M., Baum F.E., MacDougall C., Putland C. Neighbourhood life and social capital: The implication for health. Social Science Medicine. 2005;60:71. doi: 10.1016/j.socscimed.2004.04.027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material