Abstract
Purpose
Knee osteoarthritis (OA) is a common disease, imposing a great burden through pain and decreased function. There are many therapeutic modalities including non-pharmacologic choices and oral, topical, and intra-articular medications. New studies have shown promising results for ozone application in knee OA. Our aim was to compare the effects of ozone therapy versus hyaluronic acid (HA) intra-articular injection in knee OA patients.
Methods
In this randomized clinical trial, a total of 174 patients with more than 3 months of chronic pain or swelling in the knee joints along with consistent imaging findings were enrolled and randomly allocated into two groups of HA and ozone, which were planned to undergo 3 weekly injections of HA (Hyalgan®) and 10 mL of a 30 μg/mL ozone solution, respectively. Patients were evaluated at baseline and 6 months after the last injection for pain, stiffness, and function using the visual analog scale (VAS) and the Western Ontario and McMaster Universities Arthritis Index (WOMAC) questionnaire.
Results
No major adverse events were detected in this study. Total WOMAC score decreased from 40.8±9.8 to 20.4±4.9 (p<0.01) in the ozone group and from 38.5±7.9 to 17.1±4.2 (p<0.01) in the HA group. A similar trend was observed in pain improvement according to VAS. Pain, stiffness, and function significantly improved in both the groups, but no between-group difference was found.
Conclusion
Although both ozone and HA can be effectively used for improving function and reducing pain in selected knee OA patients, neither of the two showed any superiority at 6-month follow-up.
Keywords: ozone, hyaluronic acid, knee osteoarthritis
Plain language summary
Knee osteoarthritis (OA) is a prevalent disease with many heterogeneous therapeutic choices. The only definite treatment is surgery, which is reserved for advanced stages. For those who are not candidates for surgery or if symptoms persist after non-invasive options, various intra-articular injections are available. Among them, corticosteroids, dextrose, normal saline, platelet-rich plasma (PRP), ozone, and hyaluronic acid (HA) are the most commonly used ones. Earlier studies have demonstrated inconsistent results with a small preference toward PRP and HA injections. Our aim in this trial was to discuss efficacy and safety of ozone intra-articular injection in mild to moderate knee OA patients, compared to HA (which is a well-known intra-articular supplement and its modest effects have been previously proved).
Introduction
Knee osteoarthritis (OA) is a progressive degenerative condition in which functional impairment is caused by mechanical forces against the joint, resulting in pain and decreased range of motion. Obese women above 50 years of age are the most vulnerable group.1 OA was the fourth most common cause of hospitalization in 2009 in the United States with a total cost of $42.3 billion per year.2 The prevalence of disease varies highly among different populations: from 19.3% in some rural areas of Iran to 2.8% in the Philippines. Approximately 43% of Iranian adults within the age of 50–60 years show radiographic findings of knee OA,3 which is far more prevalent than in the population of Framingham in Massachusetts (19%).4 Most common symptoms of OA include pain, stiffness, swelling, and crepitus, and it can occasionally lead to joint and limb deformity. Diagnosis is mainly based on this clinical picture.5,6 There is no unique cure for knee OA; however, there are several treatments such as acetaminophen, oral non-steroidal anti-inflammatory drugs (NSAIDs), topical creams, patches, and so on, which can help to achieve better pain management and higher mobility. Although these drugs have been proven to be helpful in short-term, evidence showing that such interventions could alter the degenerative process exist.7,8 Other complementary products such as glucosamine and chondroitin are also commonly used despite equivocal efficacy.9 Moreover, there are many non-pharmacologic choices that can relieve the patient’s symptoms, including exercise, shoe modification, assistive devices, laser, biofeedback and some physical agent modalities.10 The only definite treatment is surgery which is reserved for advanced stages.6 For those who are not a candidate for surgery or if symptoms persist after non-invasive options, various intra-articular injections are available. Among them, corticosteroids, dextrose, prolotherapy, normal saline (NS), platelet-rich plasma (PRP), ozone, and hyaluronic acid (HA) are the most commonly used.8,11–17 The latter is a natural mucopolysaccharide in the synovial joints, which might be destroyed secondary to knee OA.14 From a biochemical point of view, HA injection has an augmentative viscoelastic function and anti-inflammatory effect; hence, it has become a widespread topic of interest for non-surgical clinical trials.14,16,18
Although the precise physiologic events activated by intra-articular injection of HA are still unclear, there is a large body of evidence that has confirmed HA efficacy in the management of knee OA.8,12,14,19–26 Since the 1990s, HA had been proven to be more effective than oral NSAID alone; it was also approved in knee OA treatment by the US Food and Drug Administration in 1997.27 It has been well documented that HA injection is more effective in earlier stages of OA than in advanced disease.14,28 In 2013, a meta-analysis compared intra-articular injection of steroids and HA in patients with knee OA. They finally concluded that 3–5 weekly injections of HA would have a more persistent effect (up to 1 year) than corticosteroid injections (2–3 weeks).29 In addition, it should be noted that no major complication has been reported for HA injection.14,21,23
Another injectable material is ozone gas. There is some new evidence supporting the role of ozone injection in the management of knee OA symptoms. This gas is now available in a solution of oxygen ozone.6,30,31 In the last decades, many orthopedic centers in Europe have begun to treat knee OA patients with intra-articular or peri-articular ozone insufflation.32 Oxygen-ozone solution (O2-O3) can improve tissue oxygenation and inhibit inflammatory mediators mediated by the down-regulation of TNFα and TNFR2. Ozone therapy can also induce a moderate-intensity oxidative stress and inhibit inflammatory responses.30,31,33,34 Ozone also has a relatively moderate analgesic effect through phosphodiesterase A2 blockage.6 According to another study, oxygen-ozone injection could induce some histological changes in the joint and consequently lead to pain killing effects.35 Although the present data suggest that ozone causes neither acute nor chronic toxicity,31,32 there is an increased risk of some complications such as septic arthritis (SA) in any invasive articular procedure.36
Many randomized clinical trials have confirmed the efficacy and safety of ozone therapy in the management of lumbosacral disc herniation, failed back surgery syndrome, and shoulder disorders.31,37–40 Moreover, ozone has a good effect in managing symptoms after traumatic meniscal injuries.41 In 2011, Mishra et al reported a remarkable superiority in the use of ozone compared to steroid intra-articular injection in 46 knee OA patients during a 6-month follow-up. Ozone success rate was 90% after 6 months based on Western Ontario and McMaster Universities Arthritis Index (WOMAC).6 Considering the high costs and existing uncertainty, our aim in this study was to compare intra-articular ozone and HA safety and efficacy in improvement of pain, range of motion (ROM) and functional score among patients with knee OA in a 6-month follow-up.
Methods
This double-blind randomized clinical trial was conducted in the Physical medicine and rehabilitation (PM&R) clinic of Shahid Modarres Hospital in Tehran from January 2015 to January 2016. A written informed consent was obtained from each participant. This study was approved by the ethics committee of the Shahid Beheshti University of Medical Sciences, Tehran, Iran (No: IR.SBMU.RETECH.REC.1396.237) and also retrospectively registered in Iranian Registry of Clinical Trials Database (IRCT; IRCT2017041513442N16).
Inclusion criteria
All patients with the following conditions were included: aged between 45 and 75 years, symptomatic knee OA with the pain aggravated by weight bearing and symptoms lasting for at least 6 months despite conservative treatments. For patients with bilateral symptoms, injection was administered on the more symptomatic limb. Subjects were screened using the Kellgren–Lawrance radiologic scoring (KLS) system (scores ranging from 0 to 4 grades) and patients with a consistent radiographic KLS score of 2–3 were included.6
Exclusion criteria
Our exclusion criteria were history of trauma, surgery or any invasive procedure in the affected joint during the past 6 months, malalignment in lower limbs, and abnormal blood count or impaired coagulation tests. We also excluded pregnant women, patients who were under immunosuppressant treatments or those with an underlying systemic arthropathy (secondary OA). In addition, patients being treated with angiotensin-converting enzyme inhibitors (ACEI) and those with significant deficiency in glucose 6-phosphate dehydrogenase level were excluded.21,31
Interventions
Using an Ozomed® smartline machine (Kastner-Praxisbedarf GmbH, Medizintechnik, Germany), 10 cc of ozone was injected into the affected knee joint of patients in the ozone group as an oxygen-ozone solution with the precise concentration of 30 μg/mL. For the subjects in HA group, HA was injected as a 20 mg/2 mL solution of HA (Hyalgan®, a viscous product with a molecular weight of 500–730 kDa, containing purified natural hyaluronate in sodium chloride solution; Fidia Farmaceutici S.p.A., Abano Terme, Italy). Before injecting the main product, 2 cc of lidocaine 2% solution was injected in all patients, using a 22-G needle, through the classic approach (anteromedial in flexed knee position) in supine position and 90° flexion of knee under sterile conditions. In both groups weekly injections were performed for 3 consecutive weeks by a specialist physician in PM&R with a 15-year experience in the musculoskeletal injections’ field. It should be noted that the latter physician was not blinded because of the totally different nature of ozone and HA; however, patients and the examiner physician were blinded.
Ice pack application and having relative rest up to 48 hours after injection were advised to patients in both the groups, if needed. Patients were advised to implement lifestyle modification with regard to knee activities. Also participants were instructed to perform regular therapeutic exercise including hamstring stretching, as well as isotonic and multi-angular isometric quadriceps strengthening. In addition, one of the authors (senior PM&R resident) was responsible for monthly overseeing of exercise and lifestyle modification (including using elevator instead of stairs and avoiding squatting, contact sports, and so on) performance.
Outcome measurements
Patients were evaluated before treatment and 6 months after injections. Their pain and functional scores were assessed during an interview by a blinded senior medical resident using the visual analog scale (VAS) and Persian version of the WOMAC questionnaire. Primary evaluation of pain was performed with VAS (scale of 0–10, 0 for no pain and 10 means the worst pain ever).42 Secondary evaluation was done using WOMAC, with scores ranging from 0 to 4 (0= no pain/restriction, 1= mild pain/restriction, 2= moderate pain/restriction, 3= severe pain/restriction, and 4= very severe pain/restriction). The maximum scores for pain, stiffness, and physical function and total WOMAC were 20, 8, 68 and 96, respectively. It is scored on a Likert scale; lower total scores mean less symptoms and better function.43 All patients underwent three weekly injections and were finally evaluated 6 months after their last injection.
Data analysis
GPower software was used to estimate the sample size. The minimum number for each group was calculated as 65 (based on α=0.05 and β=0.2), and with the assumption of a 20% drop rate, we recruited 87 patients in each group. Analysis was done using Statistical Package for the Social Sciences (version 22.0; IBM Corporation, Armonk, NY, USA) by means of paired t-test and chi square test for quantitative and qualitative variables, respectively. The difference between efficacies of the two therapeutic methods was described as effect size (raw mean difference [RMD]) and analyzed using Mann–Whitney U test. A p-value <0.05 was considered as statistically significant.
Results
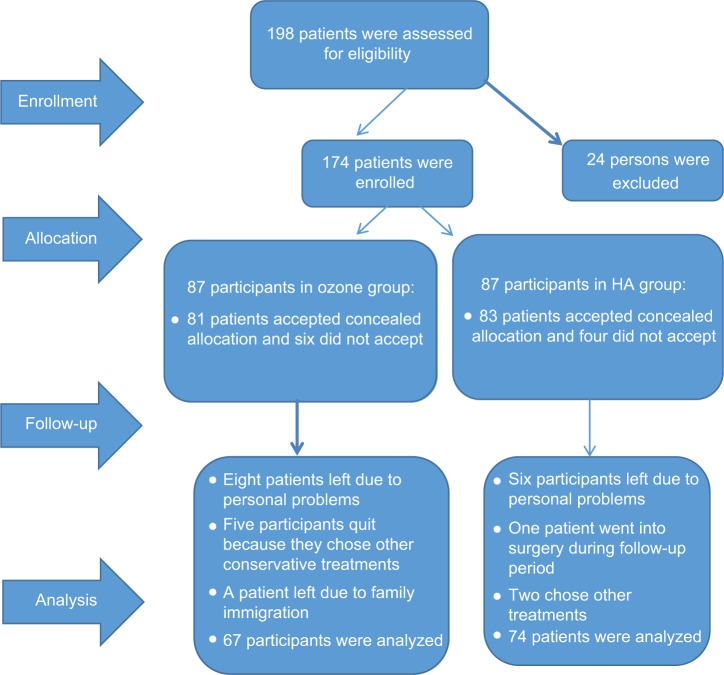
This randomized control trial (RCT) was conducted in Shahid Modarres Hospital from January 2015 to January 2016 in patients with primary knee OA who presented to PM&R clinic. A total of 174 consecutive participants who were eligible with regard to inclusion criteria were enrolled and then randomly divided into two groups using a computer-based randomization method; 87 persons in each of the ozone and HA groups. Despite their initial agreement with the study protocol and random allocation, 10 patients left the study because of dissatisfaction on concealed allocation. The study commenced with the remaining 164 participants, of whom 141 continued the study till the end, including 67 patients in the ozone group and 74 subjects in the HA group (Figure 1). Data gathered from the 23 participants who left the study were not analyzed. The reasons for their departure were personal problems or choosing other treatments and not occurrence of any complications or side effects related to the injections.
Figure 1.
Flow diagram of the study population.
Abbreviation: HA, hyaluronic acid.
Before treatment, both the groups were nearly similar with no significant difference in their demographic, anthropometric, or clinical variables (Table 1).
Table 1.
Demographic distribution and comparison of clinical variables in the two groups before treatment
| Group | Patients, n | Age (years) ± SD | Gender (F:M) | BMI (kg/m2) ± SD | WOMAC ± SD | VAS ± SD | OA grade (II:III) |
|---|---|---|---|---|---|---|---|
| Ozone | 67 | 58.1±6.4 | 50:17 (75%:25%) |
26.8±1.95 | 40.8±9.0 | 7.6±2.8 | 37:30 (56%:44%) |
| HA | 74 | 61.1±6.3 | 56:18 (77%:23%) |
28.6±1.65 | 38.5±8.0 | 7.1±3.2 | 40:34 (54%:46%) |
| p-value | – | 0.44 | 0.88 | 0.08 | 0.16 | 0.86 | 0.80 |
Abbreviations: SD, standard deviation; F, female; M, male; BMI, body mass index; WOMAC, Western Ontario and McMaster Universities Arthritis Index; VAS, visual analog scale; OA, osteoarthritis; HA, hyaluronic acid.
Based on our findings, the two treatments had been proven to be effective in improving functional score and reducing pain and stiffness in knee primary OA patients: WOMAC score in the ozone group decreased from 40.8 to 20.4 at 6-month follow-up (RMD =−20.4, p<0.01) and in the HA group, it decreased from 38.5 to 17.1 (RMD =−21.4, p<0.01). A similar trend was observed for VAS improvement; RMD =−5.0, p<0.05 in the ozone group and RMD =−4.1, p<0.05 in the HA group (Table 2).
Table 2.
VAS and WOMAC scores of the HA and ozone groups at the 6th month after injection
| Measure | Ozone therapy Before Mean ± SD |
After | Raw mean difference (SE) [95 % CI] |
HA therapy Before Mean ± SD |
After | Raw mean difference (SE) [95%CI] |
|---|---|---|---|---|---|---|
| VAS | 7.6±2.8 | 2.6±2.0 | −5.0 (0.2) [4.6–5.4] |
7.1±3.2 | 3.0±2.4 | −4.1(0.15) [3.8–4.4] |
| WOMAC Pain | 9.3±4.4 | 3.2±1.6 | −6.1 (0.2) [5.7–6.5] |
8.8±4.0 | 2.9±1.6 | −5.9 (0.2) [5.5–6.3] |
| WOMAC Stiffness | 2.3±2.4 | 1.1±1.6 | −1.2 (0.05) [1.1–1.3] |
2.1±1.6 | 1.1±0.8 | −1.0 (0.05) [0.9–1.1] |
| WOMAC Function | 29.2±7.0 | 16.1±4.2 | −13.1 (0.15) [12.8–13.4] |
27.6±6.6 | 13.1±3.2 | −14.5 (0.3) [13.9–15.1] |
| WOMAC Total | 40.8±9.0 | 20.4±5.0 | −20.4 (0.2) [20.0–20.8] |
38.5±8.0 | 17.1±4.2 | −21.4 (0.2) [21.0–21.8] |
Abbreviations: SE, standard error of mean; SD, standard deviation; CI, confidence interval; HA, hyaluronic acid; WOMAC, Western Ontario and McMaster Universities Arthritis Index; VAS, visual analog scale; OA, osteoarthritis; HA, hyaluronic acid.
Within three parts of the WOMAC questionnaire, the maximum amount of improvement for both the methods was observed in pain and stiffness. Although there was no statistical difference between the two therapeutic methods, improvement in VAS and two parts of WOMAC (pain and stiffness) was slightly better after ozone injection than for HA. But in total WOMAC score, the functional part was better for HA injection. However, the comparative analysis of the two treatments showed no significant difference in any of the clinical scores, at the 6-month follow-up, possibly due to small effect size or lack of a big enough sample size. Moreover, no major complications occurred in either of the two groups. The only adverse event was a mild flare reaction after the first injection, which was observed in five patients (two participants in the HA group and three in the ozone group). There was no statistical difference between the two groups regarding their post injection flare reactions.
Discussion
Our main objective in this RCT was to compare the efficacy and safety of ozone intra-articular injection versus the viscosupplement products in the management of pain and other OA symptoms in patients with mild to moderate knee OA.
There are several similar studies on short-term effects of ozone intra-articular injection.35,44 Some studies detected an obvious post injection decline in cytokines responsible for inflammation and OA progression.45 In an Indian study, researchers performed a cross-over study with two therapeutic methods in 46 patients with knee OA; a single injection of methyl-prednisolone versus three monthly ozone injections. After 6 months, the researchers observed an 80% response rate in the ozone group versus 60% in the steroid group.6 Other studies reported that ozone intra-articular injection had beneficial effects equal to that of hypertonic dextrose and was more effective than just air injection in the management of knee OA symptoms.39,46 Another trial in 2014 compared ozone and HA efficacy in two groups of 30 participants with knee OA. They finally found a strong improvement in both the groups compared to baseline; however, there were no significant differences between the two methods during a short-term follow-up.25
In all the previous studies that had compared ozone versus HA intra-articular injections, both the methods had been proven to be efficient in the management of pain and other symptoms; however, there are controversial results with regard to duration of pain-free period and effect size of each method. Longer follow-up like in an RCT performed in 2015 in Turkey which followed 102 patients in three groups (ozone, HA, and PRP) demonstrated a more persistent effect for HA compared to ozone.21 Another similar study with three groups of ozone, HA, and combination therapy found a higher improvement in clinical scores for the combination therapy compared to the two other groups in the 2-month follow-up.34 Also as mentioned before, authors in the Turkish study finally concluded that HA was more successful than ozone injection after the third-month follow-up. In contrast to our results, patients undergoing HA injection in that study showed a longer asymptomatic period, compared to the ozone group;21 whereas there are some studies with results similar to ours which have shown no significant difference between ozone and HA.6 Hence, according to the current study, although there was a considerable improvement in both the groups, no significant differences were observed in the efficacy and safety of the two methods.
Limitations
One of the most important limitations of our study was the single follow-up session, from which we could not estimate the time of onset for the therapeutic effects. The second shortcoming was not assessing the exact physical activity level in patients before and after intra-articular injections; this variable definitely could affect the amount of improvement and duration of symptom-free period. In addition, as another limitation, the current trial did not evaluate patients’ overall satisfaction as a final important variable. Future studies should strongly emphasize evaluating satisfaction, longer follow-up periods, larger sample size, matching physical activity level, and considering more objective outcome measures like magnetic resonance imaging to better clarify possible histologic changes in the articular surface.
Conclusion
Based on our results, although both ozone and HA can be effectively used for improving function, pain, and ROM in selected knee OA patients, neither of the two showed any superiority at 6-month follow-up. Improvement in all our outcome measures was quite similar between the two groups, and it seems appropriate to conclude that ozone injection can result in sufficient symptom relief (particularly in pain and stiffness) by at least 6 months. Hence, considering availability, accessibility, and cost–benefit trade-off, clinicians could make a choice between these intra-articular injections for each individual patient.
Acknowledgments
The abstract of this paper was presented at the 4th Biennial International Congress of Iranian Society of Knee Surgery, Arthroscopy and Sports Traumatology (ISKAST 2016) held at Tehran, Iran, May 17–20, 2016, and at the International Society of Physical and Rehabilitation Medicine World Congress (ISPRM 2016) held at Kuala Lumpur, Malaysia, May 29 to June 2, 2016, as poster presentations with interim findings.
Footnotes
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Richmond J, Hunter D, Irrgang J, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on the treatment of osteoarthritis (OA) of the knee. J Bone Joint Surg Am. 2010;92(4):990–993. doi: 10.2106/JBJS.I.00982. [DOI] [PubMed] [Google Scholar]
- 2.Murphy L, Helmick CG. The impact of osteoarthritis in the United States: a population-health perspective. Am J Nurs. 2012;112(3 Suppl 1):S13–S19. doi: 10.1097/01.NAJ.0000412646.80054.21. [DOI] [PubMed] [Google Scholar]
- 3.Tehrani-Banihashemi A, Davatchi F, Jamshidi AR, Faezi T, Paragomi P, Barghamdi M. Prevalence of osteoarthritis in rural areas of Iran: a WHOILAR COPCORD study. Int J Rheumatol Dis. 2014;17(4):384–388. doi: 10.1111/1756-185X.12312. [DOI] [PubMed] [Google Scholar]
- 4.Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185–199. doi: 10.1093/bmb/lds038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Busija L, Bridgett L, Williams SR, et al. Osteoarthritis. Best Pract Res Clin Rheumatol. 2010;24(6):757–768. doi: 10.1016/j.berh.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Mishra SK, Pramanik R, Das P, et al. Role of intra-articular ozone in osteo-arthritis of knee for functional and symptomatic improvement. Ind J Phys Med Rehabil. 2011;22(2):65–69. [Google Scholar]
- 7.Maricar N, Callaghan MJ, Felson DT, O’Neill TW. Predictors of response to intra-articular steroid injections in knee osteoarthritis: a systematic review. Rheumatology. 2013;52(6):1022–1032. doi: 10.1093/rheumatology/kes368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khoshbin A, Leroux T, Wasserstein D, et al. The efficacy of platelet-rich plasma in the treatment of symptomatic knee osteoarthritis: a systematic review with quantitative synthesis. Arthroscopy. 2013;29(12):2037–2048. doi: 10.1016/j.arthro.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 9.Towheed TE, Maxwell L, Anastassiades TP, et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev. 2005;2:CD002946. doi: 10.1002/14651858.CD002946.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Michael JW, Schlüter-Brust KU, Eysel P. The epidemiology, etiology, diagnosis and treatment of osteoarthritis of the knee. Dtsch Arztebl Int. 2010;107(16):152–162. doi: 10.3238/arztebl.2010.0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu PI, Diaz R, Borg-Stein J. Platelet-rich plasma. Phys Med Rehabil Clin N Am. 2016;27(4):825–853. doi: 10.1016/j.pmr.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Kanchanatawan W, Arirachakaran A, Chaijenkij K, et al. Short-term outcomes of platelet-rich plasma injection for treatment of osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1665–1677. doi: 10.1007/s00167-015-3784-4. [DOI] [PubMed] [Google Scholar]
- 13.Raeissadat SA, Rayegani SM, Babaee M, Ghorbani E. The effect of platelet-rich plasma on pain, function, and quality of life of patients with knee osteoarthritis. Pain Res Treat. 2013;2013:165967. doi: 10.1155/2013/165967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raeissadat SA, Rayegani SM, Hassanabadi H, et al. Knee osteoarthritis injection choices: platelet-rich plasma (PRP) versus hyaluronic acid (a one year randomized clinical trial) Clin Med Insights Arthritis Musculoskelet Disord. 2015;8:1–8. doi: 10.4137/CMAMD.S17894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rayegani SM, Raeissadat SA, Taheri MS, et al. Does intra articular platelet rich plasma injection improve function, pain and quality of life in patients with osteoarthritis of the knee? A randomized clinical trial. Orthop Rev (Pavia) 2014;6(3):5405. doi: 10.4081/or.2014.5405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raeissadat SA, Rayegani SM, Gharooi Ahangar A, Hassan Abadi P, Mojgani P, Gharooee Ahangar O. Efficacy of intra-articular injection of plasma rich in growth factor (PRGF) versus hyaluronic acid on pain and function of patients with knee osteoarthritis: a single blinded randomized clinical trial. Clin Med Insights Arthritis Musculoskelet Disord. 2017;10 doi: 10.1177/1179544117733452. 1179544117733452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raeissadat SA, Babaee M, Rayegani SM, et al. An overview of platelet products (PRP, PRGF, PRF, etc.) in the Iranian studies. Futur Sci OA. 2017;3(4):FSO231. doi: 10.4155/fsoa-2017-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miyakoshi N, Kobayashi M, Nozaka K, Okada K, Shimada Y, Itoi E. Effects of intraarticular administration of basic fibroblast growth factor with hyaluronic acid on osteochondral defects of the knee in rabbits. Arch Orthop Trauma Surg. 2005;125(10):683–692. doi: 10.1007/s00402-005-0052-y. [DOI] [PubMed] [Google Scholar]
- 19.Baltzer AWA, Moser C, Jansen SA, Krauspe R. Autologous conditioned serum (Orthokine) is an effective treatment for knee osteoarthritis. Osteoarthr Cartil. 2009;17(2):152–160. doi: 10.1016/j.joca.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 20.Curran MP. Hyaluronic acid (supartz®): a review of its use in osteoarthritis of the knee. Drugs Aging. 2010;27(11):925–941. doi: 10.2165/11205920-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 21.Duymus TM, Mutlu S, Dernek B, Komur B, Aydogmus S, Nur Kesiktas F. Choice of intra-articular injection in treatment of knee osteoarthritis: platelet-rich plasma, hyaluronic acid or ozone options. Knee Surg Sports Traumatol Arthrosc. 2016;25(2):485–492. doi: 10.1007/s00167-016-4110-5. [DOI] [PubMed] [Google Scholar]
- 22.Juni P, Reichenbach S, Trelle S, et al. Efficacy and safety of intraarticular hylan or hyaluronic acids for osteoarthritis of the knee: A randomized controlled trial. Arthritis Rheum. 2007;56(11):3610–3619. doi: 10.1002/art.23026. [DOI] [PubMed] [Google Scholar]
- 23.Kilincoglu V, Yeter A, Servet A, Kangal M, Yildirim M. Short term results comparison of intraarticular platelet-rich plasma (PRP) and hyaluronic acid (HA) applications in early stage of knee osteoarthritis. Int J Clin Exp Med. 2015;8(10):18807–18812. [PMC free article] [PubMed] [Google Scholar]
- 24.Kon E, Mandelbaum B, Buda R, et al. Platelet-rich plasma intra-articular injection versus hyaluronic acid viscosupplementation as treatments for cartilage pathology: From early degeneration to osteoarthritis. Arthroscopy. 2011;27(11):1490–1501. doi: 10.1016/j.arthro.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 25.Momen Zadeh S, Pour Farrokh M, Hashemi M, Barikani A. Comparison of intra-articular oxygen-ozone and hyaluronic acid prolotherapy on pain and disability of osteoarthritis patients. Res Med. 2014;38(1):32–36. [Google Scholar]
- 26.Wang CT, Lin J, Chang CJ, Lin YT, Hou SM. Therapeutic effects of hyaluronic acid on osteoarthritis of the knee. A metaanalysis of randomized controlled trials. J Bone Joint Surg Am. 2004;86-A(3):538–545. doi: 10.2106/00004623-200403000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Adams ME, Atkinson MH, Lussier AJ, et al. The role of viscosupplementation with hylan G-F 20 in the treatment of osteoarthritis of the knee: a Canadian multicenter trial comparing hylan G-F 20 alone, hylan G-F 20 with non-steroidal anti-inflammatory drugs (NSAIDs) and NSAIDs alone. Osteoarthr Cartil. 1995;3(4):213–225. doi: 10.1016/s1063-4584(05)80013-5. [DOI] [PubMed] [Google Scholar]
- 28.Filardo G, Kon E, Roffi A, Di Matteo B, Merli ML, Marcacci M. Plateletrich plasma: why intra-articular? A systematic review of preclinical studies and clinical evidence on PRP for joint degeneration. Knee Surg Sports Traumatol Arthrosc. 2015;23(9):2459–2474. doi: 10.1007/s00167-013-2743-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rodriguez-Merchan EC. Intra-articular injections of hyaluronic acid and other drugs in the knee joint. HSS J. 2013;9(2):180–182. doi: 10.1007/s11420-012-9320-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Manoto SL, Maepa MJ, Motaung SK. Medical ozone therapy as a potential treatment modality for regeneration of damaged articular cartilage in osteoarthritis. Saudi J Biol Sci. 2016 doi: 10.1016/j.sjbs.2016.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Velio Alvaro Bocci VA. Scientific and medical aspects of ozone therapy: state of the art. Arch Med Res. 2006;37(4):425–435. doi: 10.1016/j.arcmed.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 32.Borrelli E, Alexandre A, Iliakis E, Alexandre A, Bocci V. Disc herniation and knee arthritis as chronic oxidative stress diseases: the therapeutic role of oxygen ozone therapy. J Arthritis. 2015;4:161. [Google Scholar]
- 33.Sagai M, Bocci V. Mechanisms of action involved in ozone therapy: is healing induced via a mild oxidative stress? Med Gas Res. 2011;1(1):29. doi: 10.1186/2045-9912-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giombini A, Menotti F, Di Cesare A, et al. Comparison between intraarticular injection of hyaluronic acid, oxygen ozone, and the combination of both in the treatment of knee osteoarthrosis. J Biol Regul Homeost Agents. 2016;30(2):621–625. [PubMed] [Google Scholar]
- 35.Al-Jaziri AA, Mahmoodi SM. Pain killing effect of ozone-oxygen injection on spine and joint osteoarthritis. Saudi Med J. 2008;29(4):553–557. [PubMed] [Google Scholar]
- 36.Seyman D, Ozen NS, Inan D, Ongut G, Ogunc D. Pseudomonas aeruginosa septic arthritis of knee after intra-articular ozone injection. New Microbiologica. 2012;35(3):345–348. [PubMed] [Google Scholar]
- 37.Andreula C. Ozone therapy. Neuroradiology. 2011;53(Suppl 1):S207–S209. doi: 10.1007/s00234-011-0930-7. [DOI] [PubMed] [Google Scholar]
- 38.Apuzzo D, Giotti C, Pasqualetti P, Ferrazza P, Soldati P, Zucco GM. An observational retrospective/horizontal study to compare oxygen-ozone therapy and/or global postural re-education in complicated chronic low back pain. Funct Neurol. 2014;29(1):31–39. [PMC free article] [PubMed] [Google Scholar]
- 39.Hashemi M, Jalili P, Mennati Sh, et al. The effects of prolotherapy with hypertonic dextrose versus prolozone (intraarticular ozone) in patients with knee osteoarthritis. Anesth Pain Med. 2015;5(5):e27585. doi: 10.5812/aapm.27585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li JH, Zhou LX, Li GY, Cheng B. Treatment of middle-aged and aged patients with knee osteoarthritis of yang-deficiency induced cold-damp syndrome by ozone combined Chinese materia medica: a clinical research. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2013;33(4):471–475. [PubMed] [Google Scholar]
- 41.Wang B, Dong GZ, Ju YX, Yan CS. Case-control study on therapeutic effects of ozone and triamcinolone acetonide on the treatment of meniscal injury. Zhongguo Gu Shang. 2014;27(4):295–298. [PubMed] [Google Scholar]
- 42.Nadrian H, Moghimi N, Nadrian E, et al. Validity and reliability of the Persian versions of WOMAC Osteoarthritis Index and Lequesne Algofunctional Index. Clin Rheumatol. 2012;31(7):1097–1102. doi: 10.1007/s10067-012-1983-7. [DOI] [PubMed] [Google Scholar]
- 43.Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 44.Cardoso CC, Carvalho JC, Ovando EC, Macedo SB, Dall’Aglio R, Ferreira LR. Action of ozonized water in preclinical inflammatory models. Pharmacol Res. 2000;42(1):51–54. doi: 10.1006/phrs.1999.0646. [DOI] [PubMed] [Google Scholar]
- 45.Bocci V, Valacci G, Gorradeschi F, et al. Studies on the biological effects of ozone. Effects of the total antioxidant status and on interlukin-8 production. Mediat Inflamm. 1998;7(5):313–317. doi: 10.1080/09629359890820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ozone Injections Promising in Knee Osteoarthritis (ACR 2015 Annual Meeting) [Accessed November 3, 2016]. Available from: http://www.medscape.com/view-article/854482.