Abstract
Objective
To compare the magnitude of, and contributors to, income-related inequalities in oral health outcomes within and between Canada and the United States over time.
Methods
The concentration index was used to estimate income-related inequalities in three oral health outcomes from the Nutrition Canada National Survey 1970–1972, Canadian Health Measures Survey 2007–2009, Health and Nutrition Examination Survey I 1971–1974, and National Health and Nutrition Examination Survey 2007–2008. Concentration indices were decomposed to determine the contribution of demographic and socioeconomic factors to oral health inequalities.
Results
Our estimates show that over time in both countries, inequalities in decayed teeth and edentulism were concentrated among the poor and inequalities in filled teeth were concentrated among the rich. Over time, inequalities in decayed teeth increased and decreased for measures of filled teeth and edentulism in both countries. Inequalities were higher in the United States compared to Canada for filled and decayed teeth outcomes. Socioeconomic characteristics (education, income) contributed greater to inequalities than demographic characteristics (age, sex). As well, income contributed more to inequalities in recent surveys in both Canada and the United States.
Conclusions
Inequalities in oral health have persisted over the past 35 years in Canada and the United States, and are associated with age, sex, education, and income and have varied over time.
Keywords: Canada, United States, Oral health, Social determinants of health, Health status disparities, Income, Comparative study
Highlights
-
•
Highlights changes and contributors to oral health inequalities in Canada and the U.S. since 1970.
-
•
Provides a comparative framework for analysing income-related oral health inequalities.
-
•
Hypotheses-generating findings on contributors to income-related oral health inequalities.
1. Introduction
Inequalities in oral health are ubiquitous with their persistence recognised over time in both developing and developed countries (Sheiham, Conway, & Chestnutt, 2015). Income gradients in oral disease, for example, where disease increases with diminishing income, are not only detrimental for individuals but have significant implications for the population (Sheiham et al., 2015). In such cases, differences in oral health outcomes are often attributed to individual-level demographic and socioeconomic characteristics (Sisson, 2007). However, as individuals are embedded within social, economic, and political contexts, such structural factors cannot be ignored and must be understood in order to fully address inequalities as they may enable or prevent healthy lifestyle choices (Rose, 1985). These structural determinants of health outcomes and inequalities have been described as the degree of income inequality, labour market characteristics, insurance coverage of health care, public/private service delivery mix, accessibility of services, and the extent of inter-sectorial policies (Mackenbach, 2003). Importantly, where analyses of structural factors have been performed in the health and dental literature, comparative analyses of health outcomes in countries with different health care, social, and economic systems, enables an understanding of how societal factors may contribute to such inequalities (Bhandari et al., 2015, Guarnizo-Herreno et al., 2013a, Siddiqi et al., 2013b).
With similarities and differences in social, economic, and political contexts in Canada and the United States, it has been suggested that comparing these two countries holds important insights for understanding how structural determinants, such as social policies and economic resources, shape inequalities (Prus, 2011, Siddiqi and Hertzman, 2007). Cross-country comparative analyses have previously been performed using the Joint Canada-United States Survey of Health [JCUSH]; findings from these studies identify how societal differences have contributed to inequalities in self-rated health among individuals of different sociodemographic and socioeconomic characteristics (Siddiqi et al., 2013a, Siddiqi et al., 2013b, Prus, 2011). Longitudinal analyses of health outcomes between Canada and the United States have also revealed how changes in societal factors, such as the degree of income inequality, equality in the provision of social goods, and extent of social cohesiveness have influenced health inequalities (Siddiqi et al., 2013a, Siddiqi et al., 2013b).
In terms of oral health inequalities specifically, cross-country comparisons have been primarily performed across European countries (Bhandari et al., 2015, Guarnizo-Herreno et al., 2013a, Guarnizo-Herreno et al., 2013b, Bernabe and Sheiham, 2014, Guarnizo-Herreno et al., 2014, Listl, 2015, Manski et al., 2015, Guarnizo-Herreno et al., 2013a, Guarnizo-Herreno et al., 2013b). Indeed, to date, only one study has examined inequalities in oral health between Canada and the United States. Elani and colleagues (2012) compared the prevalence of oral health and disease within and between Canada and the United States by income, place of birth, and education. They found greater narrowing of absolute differences among place of birth, education, and income in Canada in comparison to the United States (Elani, Harper, Allison, Bedos, & Kaufman, 2012). However, by relying on simple measures to quantify and compare differences in outcomes among income groups and between countries, their findings only scratched the surface towards understanding contributors to income-related oral health inequalities. Our aim was to provide breadth and depth of understanding to the nature of oral health inequalities by identifying how structural- and individual-determinants may influence oral health inequalities through a comparative analysis within and between Canada and the United States.
2. Structural determinants of oral health within Canada and the United States
We hypothesised that structural determinants, such as the characteristics of oral health care systems, as well as social and economic conditions shape individual-level determinants and population-level oral health inequality. Table 1 provides a comparative framework outlining changes to oral health care systems, as well as social and economic conditions in Canada and the United States from the 1970s to 2000s.
Table 1.
Comparative framework to analyse oral health inequalities.
| Canada |
United States |
|||
|---|---|---|---|---|
| 1970s | 2000s | 1970s | 2000s | |
| Oral health system characteristics | ||||
| Major source of financing dental care | Out of pocket (OOP) and private insurance | |||
| Dental insurance coverage | a | 62% privately insured | a | 60% privately insured |
| 6% publicly insured | 5% publicly insured | |||
| 32% un-insured | 35% un-insured | |||
| Dental networks & reimbursement systems | Open | Open | Open | Open and Managed Care |
| Fee-for-service | Fee-for-service | Fee-for-service | Mix of fee-for-service and capitation | |
| Service delivery environment | Private practice | Predominately private practice with some non-traditional practice | Private practice | Predominately private practice with some non-traditional practice |
| Social and economic contexts | ||||
| Income distributionb, c | Gini (G): 0.304 | G: 0.321 | G: 0.316 | G: 0.378 |
| P90/P10: 4.1 | P90/P10: 4.1 | P90/P10: 4.8 | P90/P10: 5.9 | |
| (1976) | (2008) | (1974) | (2008) | |
| Employment Statusd | Full-time | Non-standard | Full-time | Non-standard |
| Unemployment rate (UR): 6.9% (1975) | UR: 6.1% (2008) | UR: 8.5% (1975) | UR: 5.8% (2008) | |
| Education (Percentage High school completion of population >25) | 37.7 (1976)e | 84.6 (2006)f | 64.1 (1976)g | 85.5 (2006)g |
Information not available.
OECD.Stats. 2015. Income distribution database. Retrieved from: http://www.oecd.org/std.
Gini coefficient of disposable income post (taxes and transfers); P90/P10 disposable income decile ratio
OECD.Stats. 2015. Unemployment rate aged 15 and over, all persons. Short-term Labour market Statistics. Retrieved from http://www.oecd.org/stde.
Statistics Canada. 1976. Population: demographic characteristics. Level of schooling by age groups. 1976 Census of Canada. Catalogue 92-827. Bulletin 2.8, Table 30.
Statistics Canada. 2006. Population: demographic characteristics. Level of schooling by age groups. 2006 Census of Canada. Catalogue no. 97-564-XCB2006009.
US Census Bureau. 1974-2002. March Current Population Survey 2003–2014. Annual Social and Economic Supplement to the Current population survey. http://www.census.gov/hhes/socdemo/education/data/cps/index.html.
2.1. Major sources of financing dental care
In both Canada and the United States, the major sources of financing dental care in the 1970s were predominantly through out-of-pocket payments, followed by private insurance payments (Health Canada, 2010; U.S. Department of Health and Human Services, 2000). It was not until the 1980s that private insurance started to compete with out-of-pocket payments to be the major source of dental care spending, which has continued to the 2000s (U.S. Department of Health and Human Services, 2000, Quiñonez et al., 2007). Despite this shift, trends in public financing of dental care have differed between Canada and the United States, with a decline in public spending on dental care experienced in Canada (20% to 5.3%) between 1970 and 2008 and an increase in the United States (5.4% to 7.3%) over the same time period (Canadian Institute for Health Information, 2012; Centers for Medicare and Medicaid Services, 2013). As of 2009, the public share of dental care expenditures is greater in the United States (9.5%) than Canada (5.4%) (Ramraj, Weitzner, Figueiredo, & Quiñonez, 2014).
2.2. Dental insurance coverage
Canada and the United States share similarities in dental insurance coverage. Neither country has a national mandate for public dental care coverage for adult social assistance recipients. In fact, individual jurisdictions (states, provinces, and territories) are responsible for determining and setting coverage to socially marginalised groups, with coverage often limited to emergency or basic dental services (Quiñonez et al., 2007, McGinn-Shapiro, 2008). As of the 2000s, Canada and the United States have comparable rates of individuals who are publicly, privately, and un-insured (Table 1).
2.3. Dental networks and reimbursement systems
In terms of dental provider networks and reimbursement systems, Canada and the United States have experienced differing trends over time. Initially, both countries operated through open-networks on fee-for-service reimbursement systems, where most individuals had the freedom to choose their provider. However, dentistry in the United States began to diverge from this model in the 1990s; employers began to offer manage care plans, which do not operate under fee-for-service reimbursement and require individuals to receive care from an approved list of providers (U.S. Department of Health and Human Services, 2000). In contrast to the United States, Canada׳s private dental care system has remained as an open fee-for-service system (Quiñonez et al., 2007).
2.4. Service delivery environments
The dominant model of dental care delivery in Canada and the United States in the 1970s was through traditional private practice settings. Alternate dental care delivery settings were present in Canada in the 1970s, such as the use of dental therapists for preventive and basic restorative services (Quiñonez et al., 2007). Not until the mid-1990s were independent allied dental professionals, namely independent dental hygienists, introduced in the United States (Perry, Freed, Kushman, 1994); this legislative change allowed dental hygienists to work without direct supervision from a dentist and occurred at a similar time in Canada (Quiñonez et al., 2007). In terms of accessibility of care, Federally Qualified Health Centres (FQHC) were introduced in the United States in the 1990s as a means to increase access to care for underserved communities; although public and safety net clinics exist in Canada, they are minor and a wide degree of variation in their presence exists across the country (Riedy, Ly, Ybarra, & Milgrom, 2007). Yet, at present, the majority of dental care delivery in both countries remains through traditional practice, with public and non-traditional practice settings becoming of increased interest and use more so in the United States than in Canada.
2.5. Income distribution
The ability to afford dental care is determined by the price of services and/or the amount of disposable income available to be able to pay for services; therefore the distribution of economic resources within society may affect access and the ability to meet oral health needs (Douglass & Cole, 1979). Over time, Canada has predominantly been more equal in terms of income inequality compared to the United States (Table 1). However, income inequality in Canada has risen, while the United States has sustained a steady rise since the 1970s, with comparable rates at present (Table 1).
2.6. Employment status
As dental insurance is often linked to employment-based benefits, changes in labour markets could also affect one׳s ability to afford oral health care. The number of standard full-time jobs started to decrease in the late 1980s in both countries, leading to more part-time, temporary jobs that often provide no health benefits, especially dental insurance (Bhatti et al., 2007, Blumberg and Work, 2004). Further, due to differences in social safety nets for unemployed populations, and their associated health benefits, unemployment rates in both countries may also impact income-related oral health inequalities. In the 1970s, higher unemployment rates were exhibited in the United States compared to Canada, and by 2008 unemployment rates fell to relatively equal size in both countries (Table 1).
2.7. Education
The level of educational attainment has also been attributed to differences in oral health outcomes between populations (Schwendicke et al., 2015). This may be related to differences in lifestyle choices among those of differing educational backgrounds (Galobardes, Lynch, & Smith, 2007). Importantly, measures of educational attainment between Canada and the United States reveal lower high school completion rates in Canada than the United States in the 1970s, with an overall rise and comparable completion rates by 2006 (Table 1).
2.8. Summary
As oral health outcomes are considered a result of social processes, comparing social and economic conditions in Canada and the United States over time provides insight into how these factors may influence inequalities in oral health. For example, provided the similarities in rates of dental coverage, education, employment status, and labour markets in Canada and the United States at present, the higher public share of dental care and presence of FQHCs in the United States may suggest less income-related oral health inequality in the United States than in Canada. As well, the rise in income inequality and labour market shifts may have resulted in an increase in inequalities in oral health in Canada since the 1970s. Thus, the aim of this research was to understand and explore how societal conditions influence the size of income-related oral health inequality through a comparative analysis of Canada and the United States over time.
3. Methodology
3.1. Study design and data sources
An observational study using data from two Canadian and two American cross-sectional national surveys at two time points was performed to examine the magnitude of and contributors to income-related oral health inequalities. The concentration index (CI) method was used to determine income-related inequality for three clinical oral health outcomes in each survey, and was subsequently decomposed to determine contributors to income-related oral health inequalities.
The Health and Nutrition Examination Survey 1971–1974 (HANES I) and the National Health and Nutrition Examination Survey 2007–2008 (NHANES) served as the two American sources and were publicly accessed through the Centre for Disease Control and Prevention website. The Nutrition Canada National Survey 1970–1972 (NCNS) and Canadian Health Measures Survey 2007–2009 (CHMS) served as the Canadian sources. The NCNS was accessed through Statistics Canada under the Data Liberation Initiative (DLI) license, and approval for the CHMS was granted by Statistics Canada and accessed through the Statistics Canada Research Data Centre at the University of Toronto.
Each survey used stratified multi-stage sampling designs to obtain nationally representative data. Demographic and oral health information was collected through household questionnaire and clinical examination. Both American surveys collected information from 32,000 non-institutionalized civilians in the United States ages 1–74 from 1971 to 1974 and 10,149 civilians 0–80 years from 2007 to 2008. The NCNS collected information from 19,590 participants ages 0–100 and excluded Indians in bands, persons living in institutions and military camps. The CHMS includes information from approximately 5,600 Canadians ages 6–79, excluding persons living on Indian Reserves or Crown lands, residents of institutions or remote regions, and full-time members of the Canadian Armed Forces.
3.2. Variables
3.2.1. Outcome variables
Oral health outcomes were obtained through clinical examination in all four surveys. Measures of edentulism (complete tooth loss) and decayed or filled teeth served as indicators of untreated and treated dental disease in our analyses. Three of the four surveys conducted individual tooth counts to assess the prevalence and severity of oral conditions, whereas the NHANES 2007–2008 performed a basic screening examination to assess the prevalence of oral conditions and diseases using a stop-after-first-encounter approach (Centers for Disease Control and Prevention, 2005). Due to this, all measures were transformed to binary outcomes for analysis.
3.2.2. Socioeconomic status
In order to measure inequalities in oral health, income served as a proxy measure for socioeconomic status. Alternative indicators such as educational attainment and occupational status were not consistently reported in ordinal format across surveys and therefore could not be used as a ranked measure of socioeconomic status that is needed to use the concentration index method. All four surveys reported household or family income in ordinal format. Total household income and household size were reported in the NHANES 2007–2008 and CHMS 2007–2009 surveys, and total family income and family size were reported in the NHANES 2007–2008, NCNS 1970–1972 and HANES I 1971–1974. Differences between family and household income rank variables were assessed using the NHANES 2007–2008 data set, and were found to be non-significant (Appendix A).
3.2.3. Explanatory variables
Socio-demographic and socioeconomic variables that were consistently reported across all surveys were incorporated into our analysis. Sex, age, and education served as controls and explanatory variables for understanding contributors to inequalities. Sex was dichotomized into male and female. Age groups were categorized into young adults (20-39), middle-aged adults (40–59), and older adults (60–74). Three age-sex groups were created in order to account for age-sex interactions. Educational attainment was reported as the highest level of education achieved by the head of household and dichotomized to “less than high school” and “high school or more”; the latter category include those with high school graduation or GED completion.
3.3. Analysis
Our analysis focused on individuals aged 20–74 years and excluded those who did not complete household questionnaires and/or clinical examinations or had missing data. Our full analysis sample comprised of dentate and edentulous individuals, and was used to estimate inequalities in edentulism. For estimation of inequalities in one or more decayed or filled teeth, edentulous individuals were excluded. To assess for homogeneity in explanatory variables (age, sex, education, income) across dentate and full (dentate+edentulous) samples chi-squared tests were performed; all values were non-significant (p>0.05), indicating lack of heterogeneity between samples.
In order to make comparisons across datasets, income variables were categorized into quintiles based on each survey׳s distribution of income. As the CI is based upon individual survey distribution, quintiles were formulated for each group to capture the true picture of income distribution at that time and place rather than control for inflation. To examine income gradients, each oral health outcome was compared across quintile, where family and household size served as controls. Estimates were generated through indirect standardisation using multivariate logit models. Dummy variables were produced for all socioeconomic, and control/predictor variables. To account for complex survey design and probability sampling, survey weights were reported for each dataset and are included in all analyses.
The CI was used to quantify the magnitude of income-related inequality for each health outcome, which is derived from a concentration curve (CC). The CC plots the cumulative proportion of individuals ranked by socioeconomic status along the x-axis against the total proportion of oral health along the y-axis; if all individuals in a population had an equal share of oral health, a diagonal line (line of equality) would be plotted. The CI is calculated as twice the area between the CC and the line of equality and ranges from −1 to +1. For measures of oral health, if all oral health is concentrated in the person with the highest socioeconomic level, the index will have a value of +1, whereas if oral health is concentrated in the person with the lowest socioeconomic level it will have a value of −1. Therefore, the closer the CC is to the diagonal and the closer the value is to 0, then the greater the equality for a given oral health measure (Wagstaff et al., 1991).
For binary health outcomes the possible values of the concentration index are limited by the mean (p) of the distribution and are equal to p-1 and 1-p, respectively (Wagstaff, 2005). As the mean increases, the range of possible values of the CI shrinks, which has implications for judging the health outcomes of a binary variable. Therefore, to permit comparison of the CI for binary outcomes with those of other outcomes the CI can be normalised so that the bounds will be between −1 and +1 (Wagstaff, 2005).
The CIs were derived using the convenient linear regression methods. Observed and expected CIs were calculated for each oral health outcome. The difference between the observed and expected CIs was calculated to produce avoidable concentration indices, which describe the magnitude of avoidable income-related inequality. The CIs can be multiplied by 75 to determine the percentage of the outcome variable that would need to be redistributed from the richer to the poorer half of the population in order for the CI to reach a value of zero (equality) (Koolman & van Doorslaer, 2004). The redistribution scheme is indicated for large samples that use convenient linear regression methods to compute the CI, where the percentage to be redistributed is equal to ¾ of the CI (Koolman & van Doorslaer, 2004).
Confidence intervals for CI values were based on the CI variance estimates from an unweighted convenient regression as described by Kakwani et al. (1997) (equation 21) (Kakwani et al., 1997). While there are tensions in the literature regarding the accuracy of the convenient regression to estimate the variance of the CI, we feel comfortable using this method for two reasons. First, not all our survey data contains sufficient information on the survey׳s sample design, which prevented using the bootstrap method (Doorslaer et al., 2004). Second, we estimated small Pearson correlations (r<0.5) between rank and observed outcomes variables. Given the Monte Carlo results of Chen et al. (2012), we felt more comfortable with the convenient regression approach to variance estimation (Chen et al., 2012). Then, we used the CI standard error (based on the variance estimate) to construct a 95% confidence interval.
The CIs for each outcome were then decomposed to determine the contribution of age, sex, education, and income to oral health inequalities. Decomposition of the concentration index reveals how far inequalities in health can be explained by the inequalities present in other explanatory variables, A variable׳s contribution to income-related inequality is based on: (i) a variable׳s effect on the outcome (elasticity), and (ii) how unequal the distribution of a given variable is across income(concentration index) (O׳Donnell & Wagstaff, 2008).
4. Results
4.1. Sample characteristics
Descriptive statistics for the full (dentate and edentulous) adult sample are presented in Table 2. The majority of participants are young to middle adult age (20–59), with equal representation among sexes, and across income quintiles. There was greater representation of participants with higher educational attainment (high school graduates) in both Canada and the United States in the 2000s compared to earlier surveys. The prevalence of one or more decayed teeth and edentulism was higher in Canada compared to the United States, with the prevalence of one or more filled teeth higher in the United States in the 1970s (Table 2). Over time, both countries experienced declines in the prevalence of decayed teeth and edentulism and subtle increases in the prevalence of one or more filled teeth.
Table 2.
Full adult analysis sample characteristics; weighted proportions (%).a
| Canada |
United States |
|||
|---|---|---|---|---|
| NCNS 1970–1972 |
CHMS 2007–2009 |
HANES I 1971-1975 |
NHANES 2007–2008 |
|
| n=10,411 | n=3,313 | n=12,608 | n=5,003 | |
| Age | ||||
| 20–39 yr | 55.8 | 39.3 | 45.8 | 40.8 |
| 40–59 yr | 31.9 | 42.8 | 36.9 | 42.1 |
| 60–74 yr | 12.3 | 17.9 | 17.3 | 17.1 |
| Sex | ||||
| Female | 53.2 | 49.4 | 52.7 | 51.2 |
| Male | 46.8 | 50.6 | 47.3 | 48.8 |
| Age/Sex | ||||
| Female 20–39 yr | 27.2 | 24.1 | 24.1 | 20.4 |
| Female 40–59 yr | 20.3 | 18.9 | 18.9 | 20.6 |
| Female 60–74 yr | 5.7 | 9.7 | 9.7 | 7.9 |
| Male 20–39 yr | 28.6 | 19.7 | 21.7 | 20.3 |
| Male 40–59 yr | 11.5 | 21.2 | 18.0 | 20.6 |
| Male 60–74 yr | 6.6 | 8.4 | 7.6 | 7.9 |
| Income | ||||
| Lowest | 10.6 | 23.8 | 15.8 | 13.9 |
| Lower middle | 23.6 | 18.9 | 10.1 | 28.2 |
| Middle | 19.7 | 16.8 | 28.0 | 14.9 |
| Upper middle | 27.5 | 12.5 | 24.0 | 19.7 |
| Highest | 18.4 | 28.0 | 22.1 | 20.2 |
| Educational attainment | ||||
| Less than high school | 69.2 | 8.9 | 36.7 | 18.7 |
| High school graduate | 30.8 | 91.1 | 63.3 | 81.3 |
| Oral health outcomes | ||||
| Presence of one or more decayed teeth | 61.2 | 21.6 | 46.8 | 21.3 |
| Presence of one or more filled teeth | 74.3 | 92.9 | 82.1 | 83.5 |
| Presence of edentulism | 23.1 | 5.6 | 15.5 | 4.9 |
Based on full (dentate and edentulous) adult population age 20–74 years.
4.2. Oral health inequalities
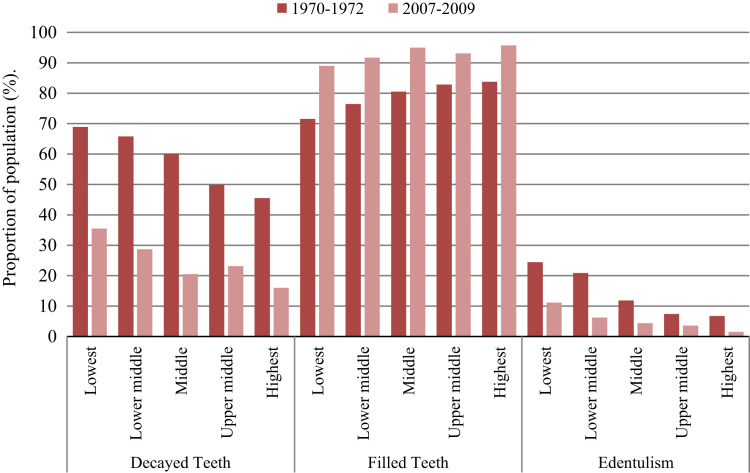
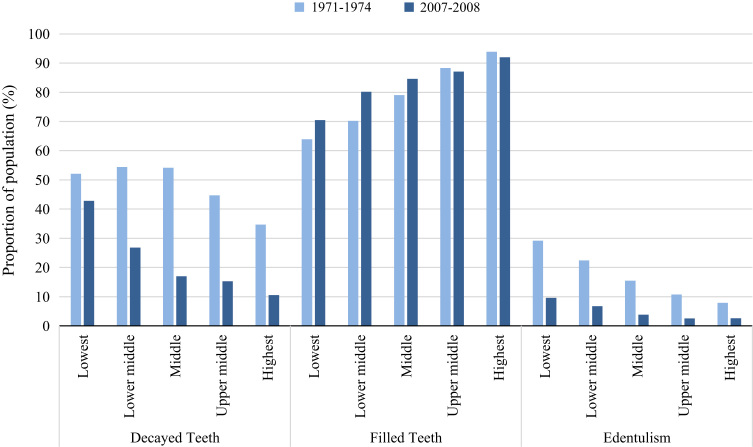
Income gradients for all oral health measures were greater in the United States compared to Canada (Fig. 1, Fig. 2). Since the 1970s, the absolute and relative differences between the highest and lowest income groups increased for one or more decayed and filled teeth outcomes in both countries, decreased for edentulism in both countries, and increased for relative differences in Canada (Table 3). When comparing the magnitude of inequalities in populations, the presence of one or more decayed teeth and edentulism is concentrated among the poor and the presence of one or more filled teeth is concentrated among the better off (Table 3). The CI revealed greater income-related inequalities in decayed and filled teeth in the United States than in Canada, whereas income-related inequalities in edentulism was greater in Canada in the 1970s.
Fig. 1.
Prevalence of oral health outcomes in Canada, by income quintile.
Fig. 2.
Prevalence of oral health outcomes in the United States, by income quintile.
Table 3.
Oral health inequalities in Canada and the United States (95% confidence intervals).
| Canada |
United States |
|||
|---|---|---|---|---|
| 1970s | 2000s | 1970s | 2000s | |
| One or more of decayed teeth | ||||
| Absolute Difference (%) | 10.40 | 19.50 | 17.40 | 32.30 |
| (7.96, 16.56) | (13.50, 25.50) | (13.07, 21.73) | (27.38,37.22) | |
| Relative Difference | 1.22 | 2.21 | 1.50 | 4.08 |
| (0.82 1.64) | (1.23, 4.00) | (0.98, 2.31) | (2.08, 8.01) | |
| Concentration Index | −0.158 | −0.164 | −0.160 | −0.209 |
| (−0.173,−0.139) | (−0.175,−0.145) | (−0.170,−0.150) | (−0.222,−0.196) | |
| Redistribution Requirement (%) | −11.83 | −12.30 | −12.00 | −15.70 |
| (−13.14,−10.56) | (−13.13,−10.88) | (−12.75,−11.29) | (−16.68,−14.72) | |
| One or more of filled teeth | ||||
| Absolute Difference | 12.24 | 10.70 | 30.00 | 21.50 |
| (12.17, 12.34) | (8.20, 11.20) | (26.64, 33.36) | (17.06, 25.94) | |
| Relative Difference | 0.85 | 0.92 | 0.68 | 0.77 |
| (0.62, 1.17) | (0.70, 1.25) | (0.50, 0.94) | (0.56, 1.05) | |
| Concentration Index | 0.076 | 0.053 | 0.227 | 0.106 |
| (0.059, 0.093) | (0.044, 0.061) | (0.218, 0.236) | (0.096, 0.115) | |
| Redistribution Requirement | 5.68 | 3.90 | 17.00 | 8.00 |
| (4.40, 6.97) | (3.30, 4.58) | (16.33, 17.72) | (7.18, 8.64) | |
| Presence of Edentulism | ||||
| Absolute Difference | 17.70 | 9.70 | 21.30 | 7.00 |
| (17.55, 18.75) | (7.00, 12.40) | (18.48, 24.12) | (3.44, 10.56) | |
| Relative Difference | 3.64 | 7.46 | 3.69 | 3.69 |
| (1.55, 8.56) | (2.36, 14.04) | (1.68, 8.11) | (0.94, 14.53) | |
| Concentration Index | −0.147 | −0.085 | −0.159 | −0.083 |
| (−0.163,−0.131) | (−0.094,−0.079) | (−0.167,−0.152) | (−0.093,−0.080) | |
| Redistribution Requirement | −11.00 | −6.40 | −11.90 | −6.20 |
| (−12.19,−9.81) | (−7.05,−5.93) | (−12.51,−11.40) | (−6.99,−5.99) | |
The percentage redistribution requirements for each oral health outcome by country and date are identified in Table 3, which indicates the percentage of the outcome to be redistributed across society in order to achieve equality. Negative values indicate that the outcome would have to be redistributed from lower income to higher income groups, and vice versa. Comparing Canada from 1970–2009, higher percentage redistribution requirements were exhibited in decayed and filled teeth outcomes in the 2000s (−12.3% and 3.9%) compared to the 1970s (−11.8% and 5.6%) (Table 3). In the United States, redistribution requirements increased for decayed teeth outcomes from −12.0% to −15.7% over time (Table 3). In the 2000s, redistribution requirements for decayed and filled teeth were larger in the United States, with relatively equal amounts of redistribution requirements in edentulism outcomes in both countries.
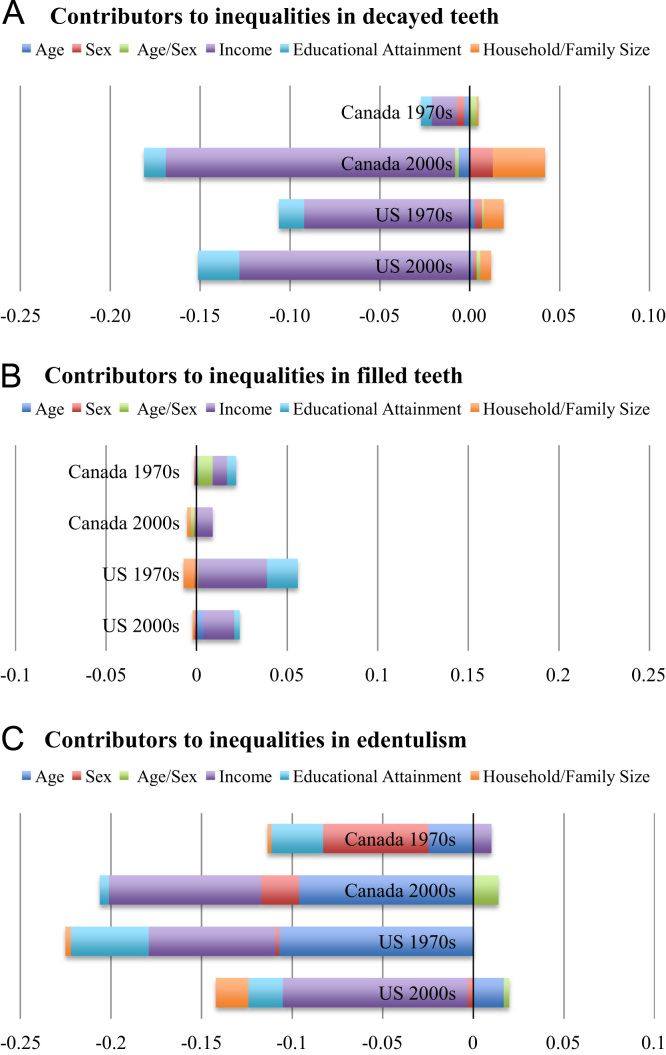
4.3. Contributors to oral health inequalities
The aggregate results from our decomposition analysis, which indicates contributors to income-related inequalities in each oral health outcome, are displayed in Fig. 3. Age contributed most to inequalities in edentulism compared to measures of decayed and filled teeth. Older adults also tended to be more representative of the worse-off (Table 4, Table 5, Table 6). Specifically, older adults in both countries tended to contribute more to inequalities in edentulism, with a lesser effect of age of inequalities in the 2000s (Table 6).
Fig. 3.
A–C. Decomposition results: contributors to oral health inequalities.
Table 4.
Contributors to inequalities in the presence of one or more decayed teeth.
| Canada |
United States |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1970s |
2000s |
1970s |
2000s |
||||||||||
| Elaa | CIb | Contrc | Elaa | CIb | Contrc | Elaa | CIb | Contrc | Elaa | CIb | Contrc | ||
| Age | 20-39yrd | ||||||||||||
| 40-59yr | −0.192 | 0.012 | −0.002 | 0.065 | 0.095 | 0.006 | −0.090 | 0.105 | −0.009 | −0.017 | 0.099 | −0.002 | |
| 60-74yr | −0.006 | 0.153 | −0.001 | 0.058 | −0.202 | −0.012 | −0.048 | −0.253 | 0.012 | −0.045 | −0.088 | 0.004 | |
| Sex | Femaled | ||||||||||||
| Male | 0.125 | 0.032 | −0.004 | 0.199 | 0.066 | 0.013 | 0.073 | 0.055 | 0.004 | 0.091 | 0.026 | 0.002 | |
| Age/Sex | Male 20-39yrd | ||||||||||||
| Male 40-59yr | 0.052 | −0.024 | −0.001 | −0.016 | 0.145 | −0.002 | −0.003 | 0.171 | −0.001 | 0.017 | 0.121 | 0.002 | |
| Male 60-74yr | 0.026 | 0.180 | 0.005 | 0.002 | −0.107 | 0.000 | −0.007 | −0.157 | 0.001 | 0.002 | −0.016 | <0.000 | |
| Income | Lowestd | ||||||||||||
| Lower Middle | −0.008 | 0.599 | −0.005 | −0.049 | −0.368 | 0.018 | −0.001 | −0.642 | 0.001 | −0.077 | −0.455 | 0.035 | |
| Middle | −0.005 | 0.184 | 0.001 | −0.091 | −0.010 | 0.001 | −0.012 | −0.269 | 0.003 | −0.090 | −0.027 | 0.002 | |
| Upper middle | −0.016 | −0.310 | −0.005 | −0.061 | 0.287 | −0.017 | −0.061 | 0.264 | −0.016 | −0.133 | 0.325 | −0.043 | |
| Highest | −0.006 | −0.802 | −0.005 | −0.230 | 0.708 | −0.163 | −0.104 | 0.759 | −0.079 | −0.167 | 0.733 | −0.122 | |
| Educational Attainment | <High schoold | ||||||||||||
| High school Grad | −0.119 | −0.049 | −0.006 | −0.381 | 0.031 | −0.012 | −0.103 | 0.132 | −0.014 | −0.314 | 0.073 | −0.023 | |
| Household/Family Size | −0.035 | −0.024 | 0.001 | 0.376 | 0.078 | 0.029 | 0.198 | 0.055 | 0.011 | 0.258 | 0.022 | 0.006 | |
Ela=Elasticity.
CI=Concentration Index.
Contr=Contribution.
Reference group.
Table 5.
Contributors to inequalities in the presence of one or more filled teeth.
| Canada |
United States |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1970s |
2000s |
1970s |
2000s |
||||||||||
| Elaa | CIb | Contrc | Elaa | CIb | Contrc | Elaa | CIb | Contrc | Elaa | CIb | Contrc | ||
| Age | 20–39 yrd | ||||||||||||
| 40–59 yr | −0.049 | −0.012 | 0.001 | 0.029 | 0.095 | 0.003 | −0.001 | 0.105 | <0.000 | 0.055 | 0.099 | 0.005 | |
| 60–74 yr | 0.002 | −0.153 | <0.000 | 0.010 | −0.202 | −0.002 | 0.001 | −0.253 | <0.000 | 0.014 | −0.088 | −0.001 | |
| Sex | Femaled | ||||||||||||
| Male | 0.045 | −0.032 | −0.001 | −0.008 | 0.066 | −0.001 | −0.023 | 0.055 | −0.001 | −0.043 | 0.026 | −0.001 | |
| Age/Sex | Male 20–39 yrd | ||||||||||||
| Male 40–59 yr | 0.015 | 0.024 | <0.000 | −0.013 | 0.145 | −0.002 | 0.003 | 0.171 | 0.001 | 0.003 | 0.121 | <0.000 | |
| Male 60–74 yr | −0.046 | −0.180 | 0.008 | −0.001 | −0.107 | <0.000 | −0.002 | −0.157 | <0.000 | 0.001 | −0.016 | <0.000 | |
| Income | Lowestd | ||||||||||||
| Lower Middle | 0.007 | −0.599 | −0.004 | 0.003 | −0.368 | −0.001 | 0.005 | −0.642 | −0.003 | 0.015 | −0.455 | −0.007 | |
| Middle | 0.007 | −0.184 | −0.001 | 0.005 | −0.010 | <0.000 | 0.030 | −0.269 | −0.008 | 0.011 | −0.027 | <0.000 | |
| Upper middle | 0.014 | 0.310 | 0.004 | 0.003 | 0.287 | 0.001 | 0.041 | 0.264 | 0.011 | 0.018 | 0.325 | 0.006 | |
| Highest | 0.011 | 0.802 | 0.009 | 0.012 | 0.708 | 0.008 | 0.050 | 0.759 | 0.038 | 0.025 | 0.733 | 0.019 | |
| Educational Attainment | <High schoold | ||||||||||||
| High school Grad | 0.103 | 0.049 | 0.005 | 0.012 | 0.031 | <0.000 | 0.129 | 0.132 | 0.017 | 0.037 | 0.073 | 0.003 | |
| Household/Family Size | −0.010 | 0.024 | <0.000 | −0.020 | 0.078 | −0.002 | −0.110 | 0.055 | −0.006 | −0.027 | 0.022 | −0.001 | |
Ela=Elasticity.
CI=Concentration Index.
Contr=Contribution.
Reference group.
Table 6.
Contributors to inequalities in the presence of edentulism.
| Canada |
United States |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1970s |
2000s |
1970s |
2000s |
||||||||||
| Elaa | CIb | Contrc | Elaa | CIb | Contrc | Elaa | CIb | Contrc | Elaa | CIb | Contrc | ||
| Age | 20–39 yrd | ||||||||||||
| 40–59 yr | 0.085 | 0.033 | 0.003 | 0.290 | 0.101 | 0.029 | 0.450 | 0.111 | 0.050 | 0.111 | 0.098 | 0.011 | |
| 60–74 yr | 0.292 | −0.094 | −0.027 | 0.542 | −0.232 | −0.126 | 0.494 | −0.317 | −0.157 | 0.125 | 0.050 | 0.006 | |
| Sex | Femaled | ||||||||||||
| Male | 0.619 | −0.094 | −0.058 | −0.335 | 0.064 | −0.021 | −0.027 | 0.059 | −0.002 | −0.090 | 0.029 | −0.003 | |
| Age/Sex | Male 20–39 yrd | ||||||||||||
| Male 40–59 yr | −0.015 | 0.069 | −0.001 | 0.259 | 0.156 | 0.040 | 0.001 | 0.172 | <0.000 | 0.013 | 0.112 | 0.002 | |
| Male 60–74 yr | −0.007 | −0.093 | 0.001 | 0.156 | −0.171 | −0.027 | <0.000 | −0.213 | <0.000 | 0.010 | 0.111 | 0.001 | |
| Income | Lowestd | ||||||||||||
| Lower Middle | −0.002 | −0.551 | 0.001 | −0.028 | −0.335 | 0.009 | −0.001 | −0.583 | <0.000 | −0.030 | −0.405 | 0.012 | |
| Middle | −0.003 | −0.118 | <0.000 | −0.028 | 0.022 | −0.001 | −0.036 | −0.202 | 0.007 | −0.075 | 0.053 | −0.004 | |
| Upper middle | −0.010 | 0.355 | −0.003 | −0.021 | 0.315 | −0.007 | −0.053 | 0.318 | −0.017 | −0.108 | 0.326 | −0.035 | |
| Highest | −0.010 | 0.815 | −0.008 | −0.120 | 0.720 | −0.086 | −0.078 | 0.779 | −0.061 | −0.124 | 0.603 | −0.075 | |
| Educational Attainment | <High schoold | ||||||||||||
| High school Grad | −0.318 | 0.090 | −0.028 | −0.146 | 0.035 | −0.005 | −0.267 | 0.163 | −0.043 | −0.211 | 0.089 | −0.019 | |
| Household/Family Size | −0.042 | 0.051 | −0.002 | 0.005 | 0.084 | <0.000 | −0.036 | 0.072 | −0.003 | 0.191 | −0.092 | −0.018 | |
Ela=Elasticity.
CI=Concentration Index.
Contr=Contribution.
Reference group.
The contribution of sex to oral health inequalities was greatest for edentulism in Canada at both time periods, with no large effect on inequalities in the United States or in other oral health outcomes (Table 4, Table 5, Table 6). These results indicate being male had a strong positive association with edentulism in Canada in the 1970s, but a negative association in Canada in the 2000s (Table 6). For measures of decayed and filled teeth, there was no large effect of age or sex on inequalities (Table 4, Table 5).
Notably, income contributed to inequalities in all oral health outcomes. Measures of one or more decayed teeth and edentulism declined with increasing income, with opposite trends for the presence of filled teeth (Table 4, Table 5, Table 6). Similar trends were found with education, as attainment of high school education was negatively associated with reporting tooth decay and edentulism in all surveys. Over time, the contribution of income to inequalities tended to increase, and contribution of education slightly decreased (Table 4, Table 5, Table 6). Between countries, the contribution of income and education to inequalities appear to be greater in the United States than in Canada (Table 4, Table 5, Table 6).
5. Discussion
To our knowledge, this is the first study to explore how changes in social and economic conditions have influenced oral health inequalities by comparing the magnitude of income-related oral health inequalities in Canada and the United States from 1970–2009. Our results identified the persistence and magnitude of oral health inequalities in Canada and the United States over the past 40 years. It revealed the greatest inequalities are exhibited in the presence of untreated disease, characterised as one or more decayed teeth, and demonstrates inequalities in oral disease are greater in the United States than in Canada.
Interestingly, for measures of one or more decayed teeth, our results reveal that despite the decline in the level of untreated decay in both countries there have been increases in income-related inequalities over time (Tables 2 and 3). This is consistent with existing international literature where Mejia et al. (2014) found that as the prevalence of decayed teeth declines in a population, groups of higher socioeconomic status often experience the sharpest decline compared to other groups. They also reported greater social gradients in missing and untreated decayed outcomes with less inequality in filled teeth in an adult Australian population (Mejia et al., 2014). Our findings corroborate the claim that, although dental decay rates have declined over time, inequalities across the income gradient show the poor as having a disproportionately higher share of dental decay.
Measures of one or more filled teeth serve as indicators of previous treatment for dental disease. Thus our results suggest that utilisation and access to dental care to receive restorative treatment continues to be slightly concentrated among the better off. Given the cross-sectional nature of these surveys, it is difficult to determine the time in which dental treatment for teeth was provided or the purpose of treatment (preventive or cosmetic restorations). However, declines in inequalities in one or more filled teeth give insight into the potential societal influences on oral health over the life course, as they provide information on previous utilisation of dental care as well as history of disease.
Our results indicate decreases in income-related inequalities in edentulism over time in both countries. This trend may be due to the overall decline in the prevalence of edentulism in both countries over the past 35 years. Another reason for these declines may be due to increases in tooth retention over the past four decades, which has been attributed to improved conservative dental care philosophies, such as an increased focus on prevention, as well as positive health-seeking behaviours and attitudes exhibited by the general population (U.S. Department of Health and Human Services, 2000).
Our results provide information on contributors unique to different oral health outcomes, in different countries, and at different times. As identified in our analysis, the contribution of age to inequalities in edentulism may be explained by the inverse relationship between retention of teeth and increasing age and diminishing income (Shen, Wildman, & Steele, 2013). The ability to afford dental care treatment after retirement has been cited as a cost-barrier for older adult populations, which is ascribed to the loss of employment-based dental insurance as well as the reduction in income after retirement (Bhatti et al., 2007, Manski et al., 2009, Manski et al., 2010, Kiyak and Reichmuth, 2005). In the United States and Canada, dental insurance coverage for older adults ranges from 14.5 to 46.8 per cent (Health Canada, 2010, Kiyak and Reichmuth, 2005). However, the effect of income and dental insurance coverage on dental care utilisation and cost-barriers to dental care cannot be determined from our analysis.
Our analyses revealed the contribution of sex to oral health inequalities in the Canadian population. Sex differences are rarely explored or identified in the dental literature, where the mechanisms underlying these differences remain unclear (Wamala et al., 2006, Ravaghi et al., 2013). Ravaghi et al. (2013) suggest that access and lifestyle may explain these differences, where lower income women in Canada might have more limited access leading to worse oral health outcomes. On the contrary, Tapp (2009) identified that men were more likely to be self-employed, and have higher unemployment rates than female counterparts, which may suggest affordability as an issue to accessing care for this group. Overall, our results suggest that further investigation is merited into the role of sex in determining inequalities.
Our findings coincide with existing literature on income gradients and the contribution of income to inequalities oral health outcomes. In this regard, cost is often cited as a predominant barrier to accessing dental care, where lower income individuals are more likely to express unmet treatment need or difficulty accessing care and decreased likelihood of reporting dental insurance (Mejia et al., 2014, Manski et al., 2012, Thompson et al., 2014). Thus, the rise in non-standard, temporary, part-time employment has diminished the availability of employment-based dental insurance for many low- and middle-income Canadians and Americans. Our findings support this statement as untreated dental disease is concentrated among the worse-off who may be unable to afford dental care in an environment of insurance scarcity.
The contribution of education to oral health outcomes has been reported in different countries, regardless of the type of social policy around dental care (Pickett & Wilkinson, 2015). It may be argued the knowledge and skills gained through education affect cognitive function, receptiveness to health education message, or better oral health literacy. People from low socioeconomic background, including education as a determinant, are reportedly more likely to engage in unhealthy behaviours, such as poor diet choices (Guarnizo-Herreno et al., 2013a, Guarnizo-Herreno et al., 2013b). Therefore, it is logical to assume those with high school attainment or more would be less likely to exhibit oral disease and more likely to report oral health or treated disease.
Our results provide valuable insight for generating hypotheses on how societal conditions shape individual-level determinants of oral health inequalities. For example, differences in the contribution of educational attainment to inequalities over time may be a result of shifts in general knowledge and conceptualisation of oral health care since the 1970s. As well, variations in the contribution of educational attainment to inequalities between countries may be due to differences in labour force participation trends for those with less than high school education, which could impact their ability to afford care. In the United States, approximately 45% of individuals with less than high school education participate in the labour force compared to 55% in Canada as of 2009 (Quiñonez et al., 2007, McGinn-Shapiro, 2008).
Our findings also suggest that increase in contribution of income to inequalities could be related to changes in the distribution of income within Canada and the United States. Recent work by Bernabé and Marcenes (2011) suggest the degree of state income inequality may be attributed to inequalities in tooth loss in the United States, which may imply if income were more equally distributed across a population, inequalities in oral health would be reduced (Health Canada, 2010). The Organisation for Economic Co-operation and Development (OECD) reported that income inequality in the United States is considerably higher than other developed countries and has increased substantially since the 1980s (Bernabe & Marcenes, 2011); income inequality has also increased in Canada since 1976 (Forster & Levy, 2014). Bhandari et al. (2015) found that income inequality, total health expenditure, public expenditure on health, health system responsiveness, and type of dental health system explained the association between income inequality and use of dental services (Bernabe & Marcenes, 2011). Therefore, changes and differences in dental and social safety nets, and the quality of dental coverage between and within countries may explain differential access and affordability issues to dental care experienced between income groups (Stamm, 1986). All of which reinforces the notion that inequalities in oral health may be explained by factors beyond the individual-level (Bhandari et al., 2015). Although such changes could explain the increased contribution of income to inequalities over time, the mechanisms as to how they relate to health inequalities are not fully understood nor cannot be confirmed from our analysis (Rajotte, 2013).
On that note, our analyses were met with some limitations. First, given the heterogeneity between the four surveys, the availability of consistent data prohibited the number and type of comparisons; this was attributed to differences in data collection methodologies such as questionnaire design and method of clinical examination. Also, due to issues of data disclosure with the 2007–2009 Canadian survey, three broad age groups were used in our analyses, which could mask the complex relationship between age and our outcomes. As well, the exclusion of certain population groups indicates that our findings may not be generalisable to the entire Canadian or American population. Further, there have only been two nationally representative surveys in Canada that contain clinical oral health outcomes that were administered approximately 40 years apart from each other, which prevented comparisons of inequalities in other time periods. Due to the cross-sectional nature of surveys used in this study, our results cannot confirm causal association between any of the explanatory variables on income-related oral health inequalities. Instead, it provides a means to further investigate these potential associations through longitudinal analyses.
Our findings give rise to hypotheses that may help uncover the direct or fundamental causes of social relationships and oral health inequalities. They highlight that oral health outcomes are a result of the complex interaction between societal and individual level factors. As such, a reduction or elimination of oral health inequalities within a population requires an approach that addresses determinants within individuals and society itself. At present, effective approaches to reducing income-related inequalities in health and oral health are not well understood. Although the differences in outcomes among individuals may be ascribed to societal conditions, the underlying mechanisms of these determinants may not be reducible or quantifiable to measurement at present. Therefore, further research is needed to validate the theoretical assumptions between socioeconomic status, society, and oral health outcomes.
6. Conclusion
Inequalities in oral health have persisted and, to some extent, increased over the past 40 years in Canada and the United States. As such, our results suggest that changes in the social and economic environments within Canada and the United States may have played a role in shaping oral health inequalities over time. For example, the sustained rise of income inequality experienced in both countries may explain the increase in contribution of income to oral health inequalities since the 1970s. As well, changes in social policies, labour markets, coverage of dental care, and societal norms of oral hygiene may have also contributed to changes in oral health inequalities. With improvements in oral health at the population-level, it would be logical to assume that inequalities would be reduced. However, greater inequalities were exhibited in oral disease over time. Our results emphasise that although societal conditions impact income-related oral health inequalities, their underlying mechanisms remain unclear. Therefore, further research is needed to better understand the relationship between structural factors, socioeconomic status, and oral health outcomes in order to reduce inequalities.
Acknowledgements
The authors like to acknowledge the assistance and guidance provided by Statistics Canada Research Data Centre and the financial support from the Canadian Foundation for Dental Hygiene Research and Education (CFDHRE) and the Dr. George and Nancy Vasiga Scholarship in Dental Public Health.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ssmph.2016.03.009.
Appendix A. Supplementary material
Supplementary material
References
- Bernabe E., Marcenes W. Income inequality and tooth loss in the United States. Journal of Dental Research. 2011;90(6):724–729. doi: 10.1177/0022034511400081. [DOI] [PubMed] [Google Scholar]
- Bernabe E., Sheiham A. Extent of differences in dental caries in permanent teeth between childhood and adulthood in 26 countries. International Dental Journal. 2014;64(5):241–245. doi: 10.1111/idj.12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhandari B., Newton J.T., Bernabe E. Income inequality and use of dental services in 66 countries. Journal of Dental Research. 2015 doi: 10.1177/0022034515586960. [DOI] [PubMed] [Google Scholar]
- Bhatti T., Rana Z., Grootendorst P. Dental insurance, income and the use of dental care in Canada. Journal of the Canadian Dental Association. 2007;73(1):57. [PubMed] [Google Scholar]
- Blumberg, L. J., Holahan, J., (2004). Work, offers, and take-up: decomposing the source of recent declines in employer-sponsored insurance. Health Policy Online.
- Canadian Institute for Health Information (2012). National health expenditure trends, 1975 to 2012. Ottawa, ON: Canadian Institute for Health Information
- Centers for Disease Control and Prevention (2005). National Health and Nutrition Examination Survey (NHANES): Oral health examiners manual.
- Chen Z., Roy K., Gotway Crawford C.A. Evaluation of variance estimators for the concentration and health achievement indices: a monte carlo simulation. Health Economics. 2012;21(11):1375–1381. doi: 10.1002/hec.1796. [DOI] [PubMed] [Google Scholar]
- Doorslaer Ev, Koolman X., Jones A.M. Explaining income-related inequalities in doctor utilisation in Europe. Health Economics. 2004;13(7):629–647. doi: 10.1002/hec.919. [DOI] [PubMed] [Google Scholar]
- Douglass C.W., Cole K.O. Utilization of dental services in the United States. Journal of Dental Education. 1979;43(4):223–238. [PubMed] [Google Scholar]
- Elani H.W., Harper S., Allison P.J., Bedos C., Kaufman J.S. Socio-economic inequalities and oral health in Canada and the United States. Journal of Dental Research. 2012;91(9):865–870. doi: 10.1177/0022034512455062. [DOI] [PubMed] [Google Scholar]
- Forster M., Levy H. Organisation for Economic Co-operation and Development, Division SP; Paris, France: 2014. United States: tackling high inequalities creating opportunities for all. [Google Scholar]
- Galobardes B., Lynch J., Smith G.D. Measuring socioeconomic position in health research. British Medical Bulletin. 2007;81–82:21–37. doi: 10.1093/bmb/ldm001. [DOI] [PubMed] [Google Scholar]
- Guarnizo-Herreno C.C., Tsakos G., Sheiham A., Watt R.G. Oral health and welfare state regimes: a cross-national analysis of European countries. European Journal of Oral Sciences. 2013;121(3 Pt 1):169–175. doi: 10.1111/eos.12049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guarnizo-Herreno C.C., Watt R.G., Pikhart H., Sheiham A., Tsakos G. Socioeconomic inequalities in oral health in different European welfare state regimes. Journal of Epidemiology and Community Health. 2013;67(9):728–735. doi: 10.1136/jech-2013-202714. [DOI] [PubMed] [Google Scholar]
- Guarnizo-Herreno C.C., Watt R.G., Pikhart H., Sheiham A., Tsakos G. Inequalities in oral impacts and welfare regimes: analysis of 21 European countries. Community Dentistry and Oral Epidemiology. 2014;42(6):517–525. doi: 10.1111/cdoe.12119. [DOI] [PubMed] [Google Scholar]
- Canada Health. Health Canada; Ottawa, ON: 2010. Report on the findings of the oral health component of the canadian health measures survey 2007–2009. [Google Scholar]
- Kakwani N., Wagstaff A., Van Doorslaer E. Socioeconomic inequalities in health: measurement, computation, and statistical inference. Journal of Econometrics. 1997;77(1):87–103. [Google Scholar]
- Kiyak H.A., Reichmuth M. Barriers to and enablers of older adults׳ use of dental services. Journal of Dental Education. 2005;69(9):975–986. [PubMed] [Google Scholar]
- Koolman X., van Doorslaer E. On the interpretation of a concentration index of inequality. Health Economics. 2004;13(7):649–656. doi: 10.1002/hec.884. [DOI] [PubMed] [Google Scholar]
- Listl S. Countries with public dental care coverage have lower social inequalities in the use of dental services than countries without such coverage. The Journal Of Evidence-based Dental Practice. 2015;15(1):41–42. doi: 10.1016/j.jebdp.2014.12.001. [DOI] [PubMed] [Google Scholar]
- Mackenbach J.P. An analysis of the role of health care in reducing socioeconomic inequalities in health: the case of the Netherlands. International Journal of Health Services. 2003;33(3):523–541. doi: 10.2190/C12H-NBA4-7QWE-6K3T. [DOI] [PubMed] [Google Scholar]
- Manski R.J., Moeller J.F., Chen H., St Clair P.A., Schimmel J., Magder L.S. Dental care coverage transitions. The American journal of Managed Care. 2009;15(10):729–735. [PMC free article] [PubMed] [Google Scholar]
- Manski R.J., Moeller J., Chen H., St Clair P.A., Schimmel J., Magder L. Dental care expenditures and retirement. Journal of Public Health Dentistry. 2010;70(2):148–155. doi: 10.1111/j.1752-7325.2009.00156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manski R.J., Moeller J.F., Chen H., St Clair P.A., Schimmel J., Pepper J.V. Wealth effect and dental care utilization in the United States. Journal of Public Health Dentistry. 2012;72(3):179–189. doi: 10.1111/j.1752-7325.2012.00312.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manski R., Moeller J., Chen H., Widstrom E., Lee J., Listl S. Disparity in dental coverage among older adult populations: a comparative analysis across selected European countries and the USA. International Dental Journal. 2015;65(2):77–88. doi: 10.1111/idj.12139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinn-Shapiro M. Medicaid coverage of adult dental services. State Health Policy Monitor. 2008;2(2):1–6. [Google Scholar]
- Mejia G., Jamieson L.M., Ha D., Spencer A.J. Greater inequalities in dental treatment than in disease experience. Journal of Dental Research. 2014;93(10):966–971. doi: 10.1177/0022034514545516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O׳Donnell O.A., Wagstaff A. World Bank Publications; 2008. Analyzing health equity using household survey data: a guide to techniques and their implementation. http://www.worldbank.org/en/topic/health/publication/analyzing-health-equity-using-household-survey-data. [Google Scholar]
- Perry D.A., Freed J.R., Kushman J.E. The California demonstration project in independent practice. Journal of Dental Hygiene. 1994;69(3):137–142. [PubMed] [Google Scholar]
- Pickett K.E., Wilkinson R.G. Income inequality and health: a causal review. Social Science Medicine. 2015;128:316–326. doi: 10.1016/j.socscimed.2014.12.031. [DOI] [PubMed] [Google Scholar]
- Prus S.G. Comparing social determinants of self-rated health across the United States and Canada. Social Science & Medicine. 2011;73(1):50–59. doi: 10.1016/j.socscimed.2011.04.010. [DOI] [PubMed] [Google Scholar]
- Quiñonez C., Grootendorst P., Sherret L., Azarpazhooh A., Locker D. Community Dental Health Services Research Unit, University of Toronto; Toronto, ON: 2007. An environmental scan of provincial and territorial public dental programs in Canada. [Google Scholar]
- Rajotte, J. (2013). Income inequality in Canada: an overview, In: Report of the Standing Committee on Finance, (Ed.), Ottawa, ON; The Office of the Speaker of the House of Commons
- Ramraj C., Weitzner E., Figueiredo R., Quinonez C. A macroeconomic review of dentistry in Canada in the 2000s. Journal of the Canadian Dental Association. 2014 80:e55. [PubMed] [Google Scholar]
- Ravaghi V., Quinonez C., Allison P.J. The magnitude of oral health inequalities in Canada: findings of the Canadian health measures survey. Community Dentistry and Oral Epidemiology. 2013;41(6):490–498. doi: 10.1111/cdoe.12043. [DOI] [PubMed] [Google Scholar]
- Riedy C.A., Ly K.A., Ybarra V., Milgrom P. An FQHC research network in oral health: enhancing the workforce and reducing disparities. Public Health Reports. 2007;122(5):592–601. doi: 10.1177/003335490712200506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose G. Sick individuals and sick populations. International Journal of Epidemiology. 1985;14(1):32–38. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- Schwendicke F., Dorfer C.E., Schlattmann P., Page L.F., Thomson W.M., Paris S. Socioeconomic inequality and caries: a systematic review and meta-analysis. Journal of Dental Research. 2015;94(1):10–18. doi: 10.1177/0022034514557546. [DOI] [PubMed] [Google Scholar]
- Sheiham A., Conway D., Chestnutt I., (2015). Impact of oral diseases and oral health inequalities. In: Social Inequalities in oral health: from evidence to action. London, UK.
- Shen J., Wildman J., Steele J. Measuring and decomposing oral health inequalities in an UK population. Community Dentistry and Oral Epidemiology. 2013;41(6):481–489. doi: 10.1111/cdoe.12071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqi A., Hertzman C. Towards an epidemiological understanding of the effects of long-term institutional changes on population health: a case study of Canada versus the USA. Social Science & Medicine. 2007;64(3):589–603. doi: 10.1016/j.socscimed.2006.09.034. [DOI] [PubMed] [Google Scholar]
- Siddiqi A., Ornelas I.J., Quinn K., Zuberi D., Nguyen Q.C. Societal context and the production of immigrant status-based health inequalities: a comparative study of the United States and Canada. Journal of Public Health Policy. 2013;34(2):330–344. doi: 10.1057/jphp.2013.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqi A., Kawachi I., Keating D.P., Hertzman C. A comparative study of population health in the United States and Canada during the neoliberal era, 1980–2008. International Journal of Health Services. 2013;43(2):193–216. doi: 10.2190/HS.43.2.b. [DOI] [PubMed] [Google Scholar]
- Sisson K.L. Theoretical explanations for social inequalities in oral health. Community Dentistry and Oral Epidemiology. 2007;35(2):81–88. doi: 10.1111/j.1600-0528.2007.00354.x. [DOI] [PubMed] [Google Scholar]
- Stamm J., Waller M., Lewis D., and Stoddart G.,(1986) Dental care programs in Canada: historical development,current status and future directions. Ottawa, ON: Health and Welfare Canada.
- Tapp S. recent trends and future outlook. Office of the Parliamentary Budget Officer; Ottawa: ON: 2009. Canadian labour market developments: recession impacts. [Google Scholar]
- Thompson B., Cooney P., Lawrence H., Ravaghi V., Quiñonez C. Cost as a barrier to accessing dental care: findings from a Canadian population-based study. Journal of Public Health Dentistry. 2014;74(3):210–218. doi: 10.1111/jphd.12048. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health, 2000. NIH Publication no. 00-4713.2014.
- Wagstaff A., Paci P., van Doorslaer E. On the measurement of inequalities in health. Social Science Medicine. 1991;33(5):545–557. doi: 10.1016/0277-9536(91)90212-u. [DOI] [PubMed] [Google Scholar]
- Wagstaff A. The bounds of the concentration index when the variable of interest is binary, with an application to immunization inequality. Health Economics. 2005;14(4):429–432. doi: 10.1002/hec.953. [DOI] [PubMed] [Google Scholar]
- Wamala S., Merlo J., Bostrom G. Inequity in access to dental care services explains current socioeconomic disparities in oral health: the Swedish national surveys of public health 2004–2005. Journal of Epidemiology And Community Health. 2006;60(12):1027–1033. doi: 10.1136/jech.2006.046896. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material