Abstract
Purpose
Juvenile xanthogranuloma (JXG) is a rare histiocytic skin disease primarily of young children, which may also affect ocular structures and in particular the iris.
Observations
This is a case report of a fifty-year-old patient without skin lesions showing a progressive decrease of visual acuity, iris vascularization and a yellowish iris tumor in the iridocorneal angle of his right eye. Treatment with topical and systemic prednisolone led to full recovery of visual acuity, tumor regression and restitutio ad integrum.
Conclusions and importance
Although the juvenile xanthogranuloma is a very rare skin disease of young children, it may also affect the eye and in particular the iris in adult patients. There exists no standard treatment, the first-line therapy in most cases, however, is topical and systemic prednisolone application.
Keywords: Juvenile xanthogranuloma (JXG), Touton giant cell, Histiocytosis, Iris tumor
1. Introduction
Juvenile xanthogranuloma (JXG) is a rare cutaneous disorder which was described for the first time in 1894 by James (“congenital xanthoma multiplex“1) and, in particular, young children are affected. The disease is characterized by fast developing small yellowish skin tumors in the form of small papulonodules with a predilection for the head and neck.2 As these skin tumors show an infiltration by histiocytes and multinucleate Touton giant cells histologically, the disease belongs to the family of the histiocytoses. Although the exact pathogenesis still remains unclear, it has been suggested that the skin lesions consist of complexes formed by serum immunoglobulins and lipids.3 Treatment of the cutaneous lesions is not necessary as they usually regress spontaneously leaving hyperpigmented scars. The juvenile xanthogranuloma may also affect extracutaneous tissues as ocular structures, in particular the iris.
2. Case report
A fifty-year-old patient presented for the first time reporting a progressive decrease of visual acuity on his right eye during the past week. Visual acuity was 20/400 (right eye) and 20/20 (left eye).
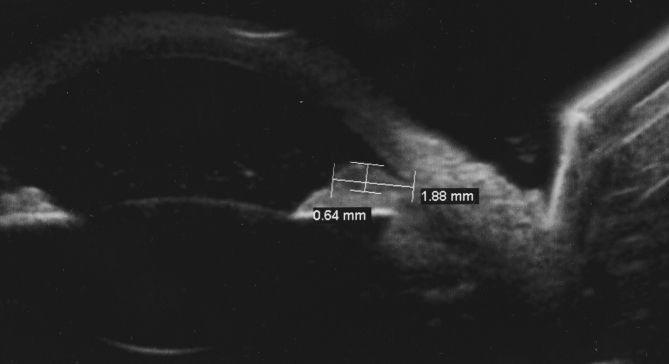
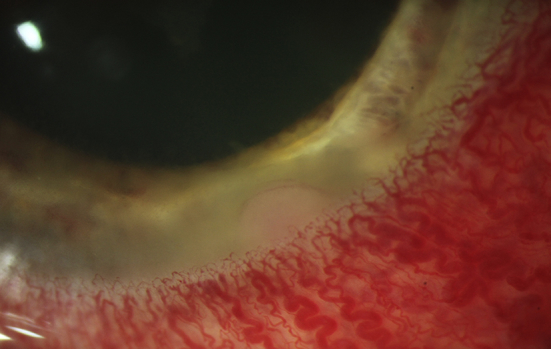
His medical history did not reveal any chronic diseases nor infections in the past. The pupils on both eyes were round and reactive to light, ocular motility was free and OCT-scans of the macula showed normal findings. The intraocular pressure was 27 mmHg (right eye) and 19 mmHg (left eye). Examination at the slit lamp showed no relevant pathology of the left eye. Examination of the right eye of the patient, however, revealed a yellowish iris mass covering the iridocorneal angle from the 5 o'clock to the 6 o'clock position (Fig. 1, Fig. 2). This finding was accompanied by a strong vascularization of the iris, by cells and fibrin in the anterior chamber and by a mild hyposphagma. Because there was an acute eye irritation and the symptoms developed fast during one week, a nevus or neurofibroma could be excluded as a differential diagnose.
Fig. 1.
External slit lamp photograph of the right eye, iris tumor and iris vascularization (initial presentation, photo laboratory, Department of Ophthalmology, Saarland University, 66421 Homburg, Germany).
Fig. 2.
Gonioscopic photograph of the right eye, iris tumor from the 5 o'clock to the 6 o'clock position in the iridocorneal angle (initial presentation, photo laboratory, Department of Ophthalmology, Saarland University, 66421 Homburg, Germany).
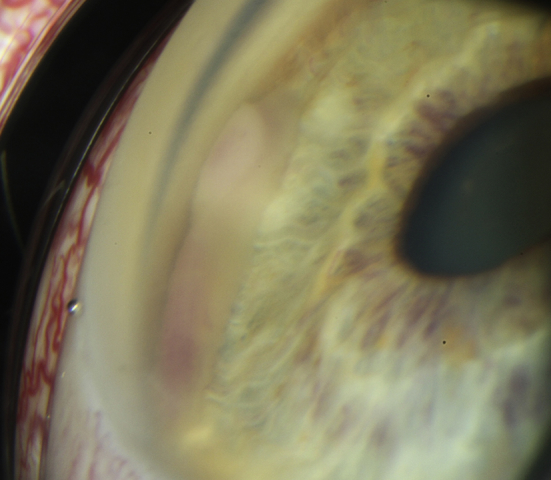
The tumor's infiltration of the iris was revealed by sonographic examination (UBM, Fig. 3). This infiltration was limited to the iris, there was no infiltration of the vitreous body. Because the lesion was suspicious for a xanthogranuloma, granulomatous disorders like tuberculosis, sarcoidosis, granulomatosis with polyangiitis and syphilis were considered as differential diagnoses. Medical laboratory tests (for, e.g., activity of levels of angiotensin converting enzyme and concentrations of soluble interleukine-2 receptor), Venereal Disease Research Laboratory (VDRL) test and Treponema-pallidum-hemagglutination-assay (TPHA), ear-nose-throat and radiological examinations (chest X-ray and computertomography) did not reveal any acute or chronic disease. Strikingly, blood analysis revealed a polyglobulia. Due to this finding, the patient was presented to the hemato-oncologists with suspect of polycythemia vera lateron.
Fig. 3.
Sonographic examination (UBM) of the right eye, iris tumor (initial presentation).
The patient was treated with topical and systemic prednisolone (inflanefran forte drops every hour, prednisolone 100 mg) and Cosopt S drops (twice a day). The consistent application of this therapy gradually led to recovery of visual acuity within four days (visual acuity on the right eye 20/25). The iris vascularization began to decrease, the iris tumor however persisted. Oral prednisolone (100 mg daily, with a reduction by 10 mg a week) and topical prednisolone drops (every hour) were prescribed to the patient. In the follow-up medical examination after one week, the iris tumor had significantly decreased. Supported by this finding, the patient was instructed to taper off prednisolone and to attend a follow-up examination after four weeks. One month later, the iris tumor had completely disappeared and visual acuity had fully recovered (Fig. 4, Fig. 5). This finding remained stable and without recurrence in further follow-up examinations (up to now five months after initial presentation).
Fig. 4.
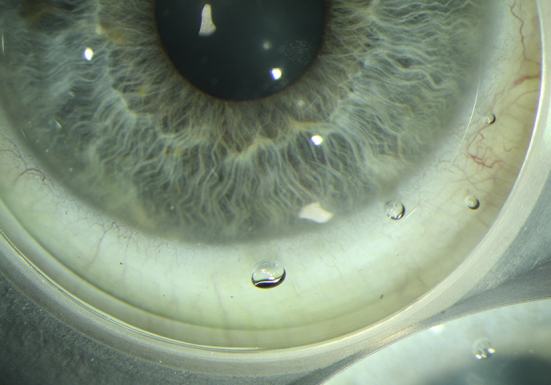
External slit lamp photograph of the right eye one month after initial presentation, restitutio ad integrum (photo laboratory, Department of Ophthalmology, Saarland University, 66421 Homburg, Germany).
Fig. 5.
Gonioscopic photograph of the right eye one month after initial presentation, restitutio ad integrum (photo laboratory, Department of Ophthalmology, Saarland University, 66421 Homburg, Germany).
3. Discussion
Besides the juvenile xanthogranuloma, there are also other histiocytoses which may show ocular manifestations: The Erdheim-Chester disease (ECD) is affecting primarily long bones of adults in middle age and the Langerhans cell histiocytosis, which is characterized by bone marrow affection and involvement of other organs in younger children. Patients with Erdheim-Chester disease may develop lipogranulomatous masses in the orbita, which can lead to exophthalmus, ophthalmoplegia or even blindness due to optic atrophy.4 In patients with Langerhans cell histiocytosis, cases with lytic lesions within the orbital wall and large soft-tissue masses in the orbita leading to proptosis have been described.5 An intraocular tumor due to a histiocytic disease may indicate an intraocular manifestation of the juvenile xanthogranuloma.
The first pediatric case of a juvenile xanthogranuloma with intraocular involvement was published by Blank et al., in 1949.6 They compared histological findings of skin lesions with the lesion in the eye. The ocular symptoms include unilateral atraumatic hyphaema, iritis, decreased visual acuity and secondary glaucoma due to the obstruction of the iridocorneal angle by the iris tumor.7 Nowadays, fine needle aspiration cytology from the lesion or the aqueous may lead to the diagnosis of the juvenile xanthogranuloma,8 but in most cases, the diagnosis “intraocular juvenile xanthogranuloma” is based on the clinical picture alone.9 Zimmerman et al. (196510) postulated five criteria each of which may indicate a possible intraocular manifestation of the juvenile xanthogranuloma: 1) spontaneous hyphaema, 2) a red eye with signs of uveitis, 3) congenital or acquired heterochromia iridis, 4) iris tumor and 5) unilateral glaucoma. Our patient had a unilateral red eye, an iris tumor and he complained of glare and a decreased visual acuity. The intraocular pressure was moderately increased to 27 mmHg (19 mmHg in the other eye) which required topical medication. Clinically the yellowish tumor covered the iridocorneal angle of the right eye from the 5 o'clock to the 6 o'clock position. There were no further lesions neither in the eyes nor in the skin of our fifty-year-old patient.
The majority of the patients with a juvenile xanthogranuloma are less than one year old.7 However cases of older patients have been published with the oldest patient reported up to now aged 77 years.11 In most cases the first and only clinical sign of the disease are the skin lesions. Only 0.4–10% of patients with skin lesions also have ocular lesions.10 The skin lesions have not to be considered as a conditio sine qua non for the diagnosis of an intraocular juvenile xanthogranuloma, because the lesion in the eye may be the only manifestation of the disease. Besides to the iris, the juvenile xanthogranuloma may also affect the orbit, optic nerve, retina and choroidea.7 In the differential diagnosis of the intraocular juvenile xanthogranuloma, amelanotic melanoma, iris leiomyoma, haemangioma, lymphangioma,12 retinoblastoma, and metastasis of a cancer of unknown primary must be considered. The latter could be ruled out in our patient by radiological examination (chest X-ray and computertomography).
As there exists no standard treatment for juvenile xanthogranuloma in the eye, a variety of therapeutical approaches do exist. They all have in common the topical and systemic application of prednisolone and its dose has to be adjusted to the age of the patient. If symptoms persist despite adequate topical and systemic steroid application, Casteels et al. (199312) recommended the subconjunctival application of methylprednisolone (30 mg) adjacent to the lesion, which led to the disappearance of the iris lesion in four patients after one (one patient), two (two patients) or three injections (one patient).
In case of a refusal of steroid therapy or steroid response, other therapeutical approaches are required. Parmley et al. (19987) successfully treated a twenty-five-year-old patient with a juvenile xanthogranuloma of the iris with radiotherapy (initially 4 Gy, and two additional sessions of 6 Gy at intervals of half a year) and long term methothrexate (15 mg a week). Ashkenazy et al. (201413) treated two children with off-label intravitreal bevacizumab (1.25 mg/0.05 ml) with the aim to modulate the intrinsic vascularity of juvenile xanthogranuloma lesions followed by low-dose plaque radiotherapy of 35 Gy over four days, which led to a flat scar without recurrence of the disease.
4. Conclusions
Other granulomatous disorders like, e.g., tuberculosis, sarcoidosis, granulomatosis with polyangiitis and syphilis could be excluded by medical laboratory tests and radiological examination and because steroid therapy led to recovery of visual acuity and disappearance of the tumor in our patient, we concluded from this treatment success that the most likely explanation for our patient's symptoms was in fact a juvenile xanthogranuloma of the iris.
The first-line therapy in most cases is topical and systemic prednisolone application, which may lead to full recovery of visual acuity and to disappearance of the tumor in the eye. In case of steroid responders or non-responders with a reliable diagnosis of intraocular juvenile xanthogranuloma, therapy escalation may be required but at the same time the differential diagnoses should be re-examined again.
Patient consent
The patient provided written consent for publication of this report, including medical record details and photographs.
Funding
No funding or grant support.
Conflict of interest
The authors have no financial disclosures.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Acknowledgements
None.
References
- 1.James W.D. A case of congenital xanthoma multiplex. Br Med J. 1894;N.1763:805. doi: 10.1136/bmj.2.1763.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeBarge L.R., Chan C.C., Greenberg S.C., McLean I.W., Yannuzzi L.A., Nussenblatt R.B. Chorioretinal, iris, and ciliary body infiltration by juvenile xanthogranuloma masquerading as uveitis. Surv Ophthalmol. 1994;39(1):65–71. doi: 10.1016/s0039-6257(05)80046-3. [DOI] [PubMed] [Google Scholar]
- 3.Bullock J.D., Bartley G.B., Campbell R.J., Yanes B., Connelly P.J., Funkhouser J.W. Necrobiotic xanthogranuloma with paraproteinemia: case report and a pathogenetic theory. Ophthalmology. 1986;93(9):1233–1236. doi: 10.1016/s0161-6420(86)33605-4. [DOI] [PubMed] [Google Scholar]
- 4.Alper M.G., Zimmerman L.E., Piana F.G. Orbital manifestations of Erdheim-Chester disease. Trans Am Ophthalmol Soc. 1983;81:64–85. [PMC free article] [PubMed] [Google Scholar]
- 5.Erly W.K., Carmody R.F., Dryden R.M. Orbital histiocytosis X. Am J Neuroradiol. 1995;16(6):1258–1261. [PMC free article] [PubMed] [Google Scholar]
- 6.Blank H., Eglick P.G., Beerman H. Nevoxantho-endothelioma with ocular involvement. Pediatrics. 1949;4(3):349–354. [PubMed] [Google Scholar]
- 7.Parmley V.C., George D.P., Fannin L.A. Juvenile xanthogranuloma of the iris in an adult. Archiv Ophthalmol. 1998;116(3):377–379. doi: 10.1001/archopht.116.3.377. [DOI] [PubMed] [Google Scholar]
- 8.Murthy R., Aratee P., Sujit J., Madhav B. Intraocular juvenile xanthogranuloma masquerading as conjunctivitis in an adult. J Clin Ophthalmol Res. 2015;3(1):27. [Google Scholar]
- 9.Rohrbach J.M. Juvenile xanthogranuloma (JXG) In: Zierhut M., Pavesio C., Ohno S., Oréfice F., Rao N.A., editors. Intraocular Inflammation. Springer; Berlin: 2016. pp. 1487–1492. [Google Scholar]
- 10.Zimmerman L.E. Ocular lesions of juvenile xanthogranuloma: Nevoxanthoendothelioma. Am J Ophthalmol. 1965;60(6):1011–1035. doi: 10.1016/0002-9394(65)92808-4. [DOI] [PubMed] [Google Scholar]
- 11.Sukavatcharin S., Cursino S., Li G., Green R.L., Lim J.I., Rao N.A. Xanthogranuloma of the iris simulating melanoma in an adult. Am J Ophthalmol. 2007;143(3):529–531. doi: 10.1016/j.ajo.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 12.Casteels I., Olver J., Malone M., Taylor D. Early treatment of juvenile xanthogranuloma of the iris with subconjunctival steroids. Br J Ophthalmol. 1993;77(1):57–60. doi: 10.1136/bjo.77.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ashkenazy N., Henry C.R., Abbey A.M., McKeown C.A., Berrocal A.M., Murray T.G. Successful treatment of juvenile xanthogranuloma using bevacizumab. J Am Assoc Pediatr Ophthalmol Strabismus. 2014;18(3):295–297. doi: 10.1016/j.jaapos.2014.01.007. [DOI] [PubMed] [Google Scholar]