Abstract
Purpose
To report two cases of eyeball tattoos with short-term post procedural complications.
Observations
Case 1 is a 26-year-old Mexican man that developed orbital cellulitis and posterior scleritis 2 h after an eyeball tattoo. Patient responded satisfactorily to systemic antibiotic and corticosteroid treatment. Case 2 is a 17-year-old Mexican man that developed two sub-episcleral nodules in the ink injection sites immediately after the procedure.
Conclusions and importance
Eyeball tattoos are performed by non-ophthalmic trained personnel. There are a substantial number of short-term risks associated with this procedure. Long-term effects on the eyes and vision are still unknown, but in a worst case scenario could include loss of vision or permanent damage to the eyes.
Keywords: Eyeball tattoo, Ink, Complications, Uveitis, Scleritis, Orbital cellulitis
1. Introduction
Eyeball tattoos are a relatively new extreme body modification. This procedure, which is performed for cosmetic purposes, involves injecting some type of pigment directly under the bulbar conjunctiva with a needle. In the medical literature there is only one report of short-term complications, seven weeks after the procedure.1 We report two cases of Mexican patients with eyeball tattoos that presented with short-term post procedural complications.
2. Findings
2.1. Case 1
A 26-year-old Mexican man presented with pain, photophobia, decreased visual acuity and eyelid edema in the right eye 2 h after undergoing a green eyeball tattoo and a subconjunctival penicillin injection in a tattoo parlor. Four days later symptomatology worsened and he sought medical care. His past medical history was positive for asthma and penicillin allergy, smoking and using recreational drugs (cocaine, methamphetamines). He also had multiple tattoo and body expansion procedures in the past years.
The patient reported that the green pigment used in the injection was diluted with isopropyl alcohol, distilled water and glycerin.
At admittance best corrected visual acuity (BCVA) was 20/100 in the right eye and 20/25 in the left eye. Intraocular pressure (IOP) was 16 and 14 mmHg, respectively. The right eye showed axial proptosis, restriction of ocular movements, significant eyelid edema, green conjunctival pigmentation, superior subconjunctival hemorrhage and diffuse chemosis (Fig. 1). Sluggish pupil response, no anterior chamber inflammation, clear lens, normal optic disc and radial macular folds were observed. Left eye was normal. Initial workup, chemistry panel and complete blood count (CBC), VDRL (Veneral Disease Research Laboratory), FTA-ABS (Fluorescent treponemal antibody absorption), PPD (Purified protein derivative) and HIV (Human immunodeficiency virus) antibody assay, was unremarkable or negative.
Fig. 1.
Case 1 - Day 1. Right eye external examination shows axial proptosis, restriction of ocular movements, significant eyelid edema, green conjunctival pigmentation, superior subconjunctival hemorrhage and diffuse chemosis. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
A clinical diagnosis of orbital cellulitis and posterior scleritis of the right eye was made. An ultrasound biomicroscopy (UBM) and B-scan were requested. B-scan showed a T-sign and an annular choroidal detachment from the equator to periphery. Retinal optical coherence tomography (OCT) confirmed the presence of macular folds in the right eye.
The patient was admitted for hospitalization. Intravenous antibiotic treatment (ceftriaxone 1 gr BID and clindamycin 300 mg QID) and topical antibiotic (moxifloxacin) were started. Two days later, oral prednisone (0.8 mg/kg/day) was initiated. A right tarsorrhaphy was performed due to conjunctival exposure and after three days the sutures were removed, resulting in clinical improvement.
The patient completed 7 days of oral antibiotic treatment and prednisone was slowly tapered for 30 days.
Fifteen days after starting treatment, proptosis, restriction of ocular movements and chemosis resolved, choroidal detachment disappeared and visual acuity improved to 20/25 in the right eye. The right lower eyelid developed a green pigmentation (Fig. 2).
Fig. 2.
Case 1 - Day 30. Right eye proptosis, restriction of ocular movements and chemosis was resolved. Right lower eyelid was pigmented because apposition of the conjunctiva and ink migration.
2.2. Case 2
A 17-year-old Mexican man, with no significant past medical history and with multiple tattoos was referred for evaluation of scleral nodules in his left eye. Five days previously he had undergone an orange eyeball tattoo in the left eye. The patient noticed that the orange ink did not spread on the surface of the eye and two elevated lesions appeared in the superior area of the eyeball. He reported no ocular pain or decreased visual acuity.
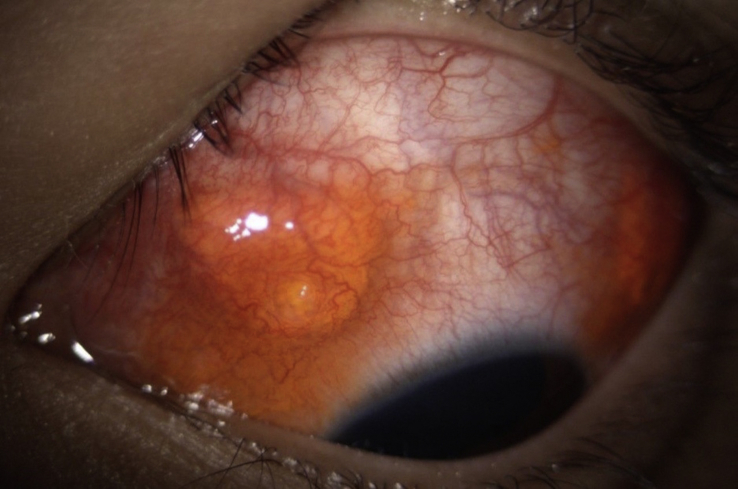
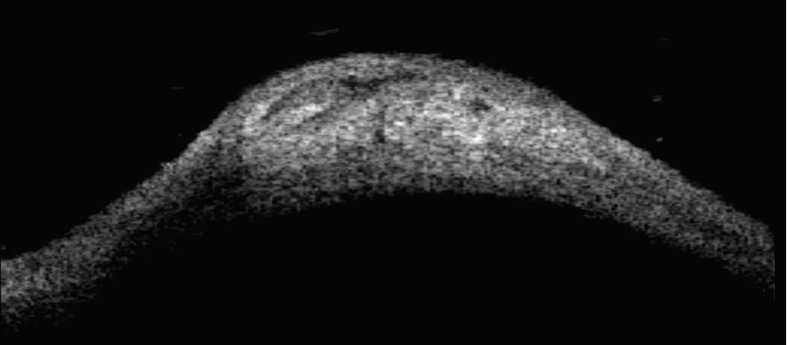
On initial presentation, BCVA was 20/20 and IOP was 16 mmHg in both eyes. Right eye examination was normal. Left eye had two orange nodules in the upper bulbar conjunctiva, corresponding to the two sites of ink infiltration (Fig. 3, Fig. 4). Anterior chamber reaction was absent, lens was clear and fundus was normal. UBM and B-scan were requested. UBM revealed pigment deposits below the episclera without scleral invasion in upper nasal and temporal quadrants (Fig. 5). T sign was not present on B-scan. A diagnosis of nodular episcleritis by chemical pigment was made.
Fig. 3.

Case 2 - Epiescleral nodules. Left eye showed two orange nodules in the upper bulbar conjunctiva. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 4.
Case 2 - Zoom to epiescleral nodules. The nodules were located at the two sites of infiltration of the ink.
Fig. 5.
Case 2 - Ultrasound biomicroscopy of nodules. Ultrasound biomicroscopy shows pigment deposits below episclera without scleral invasion in upper nasal and temporal quadrants.
Oral corticosteroids (prednisone 1 mg/kg/day) and topical antibiotic (moxifloxacin) were started. Patient was lost to follow-up.
3. Discussion
Body modification procedures and tattoos have become increasingly popular among young people.2 In the particular case of eyeball tattoos, they have been described since 2007.3 Pigment is injected directly under the bulbar conjunctiva with a needle. A single ink injection covers about a quarter of the eye, so several injections are required to completely cover the ocular surface.
There are a substantial number of short-term risks associated with this procedure such as ocular pain, blurry vision, photophobia, granulomas and staining of surrounding tissues due to ink migration.
Eyeball tattoos are done by non-ophthalmic trained personnel without the use of a surgical microscope, which increases the risk of serious ocular complications like globe penetration,4 traumatic cataract, retinal detachment and endophthalmitis.1
Moreover, the ink may cause a severe ocular inflammatory reaction, because it acts like a foreign body, and the possibility of allergic reactions to composing metallic elements.
The risk of blindness from tattoo-induced ocular inflammation has also been described. Pathophysiology of this condition involves a delayed type of hypersensitivity reaction to several components of the pigments used, which may contain cobalt, nickel, copper, chromium and iron.5, 6, 7, 8 Skin tattoos have been known to sensitize uvea to the dyes. Injecting the dye directly under the conjunctiva may thus increase the severity of uveitis.1 Finally, the presence of a granuloma can promote long-term scleral thinning or malignancy.9
Case 1 is the first report of posterior scleritis and orbital cellulitis secondary to an eyeball tattoo. In case 2 the patient was lost to follow-up, but it is likely that the sub episcleral nodules evolved towards the formation of granulomas.
Because these procedures are done by non-medical personnel, is important to first rule out associated infections, any penetrating wounds and the presence of ink within the eyeball.
We recommend using B-scan ultrasound to detect the presence of posterior sub-Tenon's fluid, as a manifestation of intraocular inflammation.
A close follow-up of these patients is warranted due to the possibility of delayed type of hypersensitivity reaction to chemical pigments.
In ideal conditions this type of cosmetic procedures should be performed by trained personnel, using a surgical microscope and under sterile conditions. However, there are insufficient reports regarding long-term ocular damage. For this reasons, and for the current conditions in which this procedure is performed, regulations that prohibit its realization are needed.
4. Conclusions
Eyeball tattoos are done by non-ophthalmic trained personnel, which increases the risk of serious ocular complications like globe penetration and endophthalmitis.
Nevertheless, long-term effects on the eyes and vision are uncertain, but in the worst case scenario could include the loss of vision or the eye.
Regulations prohibiting the practice of these procedures are required, because despite warnings of multiple health risks, more people are looking to get this procedure nowadays.
Patient consent
Written informed consent was obtained from patients for publication of these case reports and any accompanying images.
Funding
No funding or grant support.
Conflict of interest
The following authors have no financial disclosures: GADG, RC, DIPS, ECRD, MLAG.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgement
None.
References
- 1.Brodie J., El Galhud H., Bates A. A case of episcleral tattooing–an emerging body modification trend. BMC Ophthalmol. 2015 Aug 8;15:95. doi: 10.1186/s12886-015-0095-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Braverman P.K. Body art: piercing, tattooing, and scarification. Adolesc Med Clin. 2006 Oct;17(3):505–519. doi: 10.1016/j.admecli.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 3.LarrattS Three Blind Mice. http://news.bme.com/2007/07/02/three-blind-mice/(accessed 10 July 2016).
- 4.Jalil A., Ivanova T., Bonshek R., Patton N. Unique case of eyeball tattooing leading to ocular penetration and intraocular tattoo pigment deposition. Clin Exp Ophthalmol. 2015 Aug;43(6):594–596. doi: 10.1111/ceo.12501. [DOI] [PubMed] [Google Scholar]
- 5.Mansour A.M., Chan C.C. Tattoo-associated uveitis. Am J Ophthalmol. 2015 Feb;159(2):408–409. doi: 10.1016/j.ajo.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 6.Ostheimer T.A., Burkholder B.M., Leung T.G., Butler N.J., Dunn J.P., Thorne J.E. Tattoo-associated uveitis. Am J Ophthalmol. 2014 Sep;158(3) doi: 10.1016/j.ajo.2014.05.019. 637–643.e1. [DOI] [PubMed] [Google Scholar]
- 7.Mansour A.M., Chan C.C. Recurrent uveitis preceded by swelling of skin tattoos. Am J Ophthalmol. 1991 Apr 15;111(4):515–516. doi: 10.1016/s0002-9394(14)72395-5. [DOI] [PubMed] [Google Scholar]
- 8.Jacob J., Van Calster J. Skin tattoos and the development of uveitis. Acta Ophthalmol. 2013 Dec;91(8):e650–e652. doi: 10.1111/aos.12216. [DOI] [PubMed] [Google Scholar]
- 9.Multhoff G., Molls M., Radons J. Chronic inflammation in cancer development. Front Immunol. 2012 Jan 12;2:98. doi: 10.3389/fimmu.2011.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]