Abstract
Purpose
Fungal infections post keratoplasty due to contamination of the donor corneal graft have become important issues that need to be addressed. Here we report a case of fungal keratitis and endophthalmitis post penetrating keratoplasty (PKP) due to fungal contamination of the donor corneal graft.
Observations
We present a 52-year-old male who underwent PKP with a donor corneal graft that was later found to be contaminated with fungus. At 4-weeks postoperative, infectious infiltrates suddenly appeared at the border between the host and donor corneal graft, and endophthalmitis concomitantly occurred. A culture of the remnant donor corneoscleral rims and the vitreous fluid obtained during vitreous surgery was found to be positive for Candida albicans. At 6-months post vitreous surgery and intensive anti-fungal medical treatment, both corneal infiltrates and vitreous opacity completely disappeared, and the patient's best-corrected visual acuity recovered to 20/40, with a transparent cornea.
Conclusions and importance
The findings of this case show that prompt intensive medical treatment and surgical intervention effectively saved the vision in a patient with fungal keratitis and endophthalmitis due to contamination of the donor corneal graft.
Keywords: Fungal endophthalmitis, Fungal keratitis, Candida albicans, Penetrating keratoplasty, Donor cornea, Contamination
1. Introduction
Corneal transplantation is a well known and widely-accepted surgical intervention for the treatment of cornea-related disorders and the prevention of blindness.1 A statistical study from the Eye Bank Association of America (Washington, DC) reported that the total number of donor corneas supplied from eye banks in the United States for keratoplasty was 79,304 in 2015.2 However, it has been reported that in 1.4 cases per 10,000 transplants, culture-proven fungal keratitis and endophthalmitis occurred,3 and that fungal infection resulting from contaminated donor corneas can lead to devastating complications post keratoplasty.4, 5, 6, 7, 8, 9 Thus, it is important for physicians to be aware of the possible occurrence of fungal infection at the early postoperative period of corneal transplantation, and that immediate proper treatment is required in such cases.
Here we present a case of fungal keratitis with endophthalmitis due to contaminations from the donor cornea following penetrating keratoplasty (PKP) that was successfully treated by medical and surgical interventions.
2. Case report
This study involved a 52-year-old male patient who underwent PKP combined with intraocular lens suturing in his right eye at Baptist Eye Institute, Kyoto, Japan on October 2, 2015. The primary disorder was a failed corneal graft due to blunt trauma. At the time of corneal transplantation, we found a white opacity in the corneal epithelium and superficial stromal layer of the donor cornea (Fig. 1A), which appeared to be comprised of infectious infiltrates. Thus, the patient underwent transplantation with another donor cornea that was prepared for the next patient on the same day of the operation, which was the contralateral eye with no obvious infiltrates from the same donor (Fig. 1B). The corneal donor was a 58-year-old female, whose cause of death was metastatic colon cancer. The donor death to initial preservation time in Optisol-GS ™ Corneal Storage Media (Bausch & Lomb, Irvine, CA) was 21 hours and 24 minutes, and the elapsed time from donor death to transplantation was 6 days. Slit-lamp and specular microscope examinations performed at the eye bank revealed mild to moderate diffuse epithelial exposure with 25% central sloughing, mild stromal edema, several mild to moderate Descemet's folds, and several peripheral stress lines on the endothelium with an corneal endothelial cell (CEC) density of 2505 cells/mm2. Both donor corneas were obtained from SightLife ™, Seattle, WA.
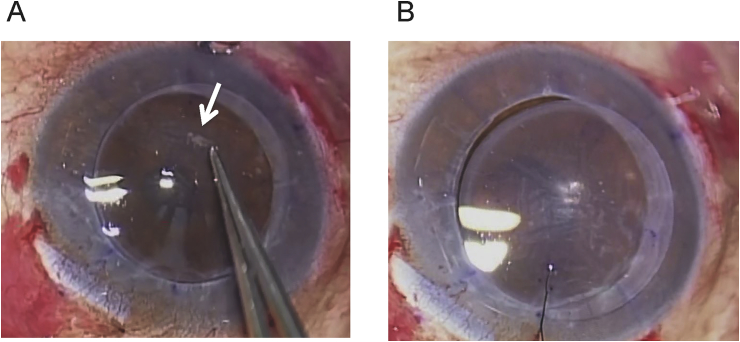
Fig. 1.
Images of the patient's right eye at the time of undergoing penetrating keratoplasty. A, A white opacity (white arrow) which resembled infectious infiltrates was observed on the donor corneal graft, so this graft was removed and not used for the transplantation. B, Instead, a donor corneal graft was prepared from the contralateral eye of the same donor and used for the transplantation.
In this patient, we administered our routine postoperative management consisting of a 4-times-daily topical application of 0.3% gatifloxacin and 0.1% betamethasone eye drops.10 In addition, chloramphenicol eye drops were used, due to the fact that they are mostly sensitive to Methicillin-resistant Staphylococcus aureus in Japan. Since we suspected a possible bacterial or fungal contamination from the donor cornea at the time of surgery, the unused donor cornea and the corneoscleral rims from the used donor cornea were cultured, resulting in Candida albicans being detected in both corneas on October 29th. However, the transplanted cornea had been transparent with no obvious infectious infiltrates and was found to have a CEC density of 2452 cells/mm2 at 25-days postoperative.
On October 29th (i.e., approximately 1-month after surgery), the patient suddenly noticed a visual disturbance, and he revisited the Baptist Eye Institute on October 31st. Upon examination, corneal infiltrates were observed at the 4-o'clock position of the graft border in his right eye, accompanied by conjunctival injection and inflammatory reaction in the anterior chamber. For treatment, a 4-times-daily administration of miconazole 0.1% eye drops and 1% natamycin ointment according to the result of a corneoscleral rim culture was added to the patient's original postoperative treatment course, and the 0.1% betamethasone eye-drop treatment was changed from 4-times daily to twice daily. In addition, a twice-daily administration of 0.1% fluorometholone eye drops and oral prednisolone were added due to the fact that the patient was in the early phase post PKP. After 48-h of treatment, we suspected the occurrence of endophthalmitis, as the patient suddenly reported ocular pain and subsequent detailed retinal fundus and B-scan ultrasound examinations revealed a vitreous opacity. The findings of our previous study in Japan showed that bacteria was most commonly the causative pathogen at the early period post corneal transplantation (i.e., within 7.8-months post surgery), while fungus infection appeared over 2-years post surgery.11 Thus, the patient was treated with an hourly topical administration of 1.5% levofloxacin instead of 0.3% gatifloxacin, which is known to fortify anti-bacterial effect and show critical eradication of gram-positive cocci, including the fluoroquinolone-resistant strains,12 and a once-daily intravenous administration of 1 g ceftazidime. In addition, the patient was administered an intravitreal injection of vancomycin and ceftazidime on November 2nd and 5th due to a suspicion of a bacterial infection as well.
Despite intense antibacterial therapy and moderated antifungal therapy, corneal infiltrates at the graft-host junction gradually expanded to the deeper layer of the cornea and the vitreous opacity enlarged and worsened (Fig. 2A,B,C). Thus, a vitrectomy was performed on November 9th to completely remove of infectious focus in the vitreous and to confirm the diagnosis of causative agents. Since Candida albicans was detected by the culture of vitreous fluid obtained at the time of surgery, medical treatment was shifted from anti-bacterial to intensive anti-fungal treatment, including oral voriconazole and intravenous fosfluconazole in addition to topical antifungal treatment. Following the vitrectomy and the administration of intensive antifungal treatment, the corneal infiltrates and inflammation inside the eye were gradually, yet markedly, improved. Two-days later, a 2-week administration of oral cyclosporine was added in order to prevent rejection of the corneal graft. Approximately 6-months later, the corneal infiltrates and intraocular inflammation completely disappeared and the corneal graft remained transparent (Fig. 2D and E). The patient's visual acuity improved to 20/40 and the CEC density was 2502 cells/mm2. A summary of the intensive treatments is shown in Fig. 3.
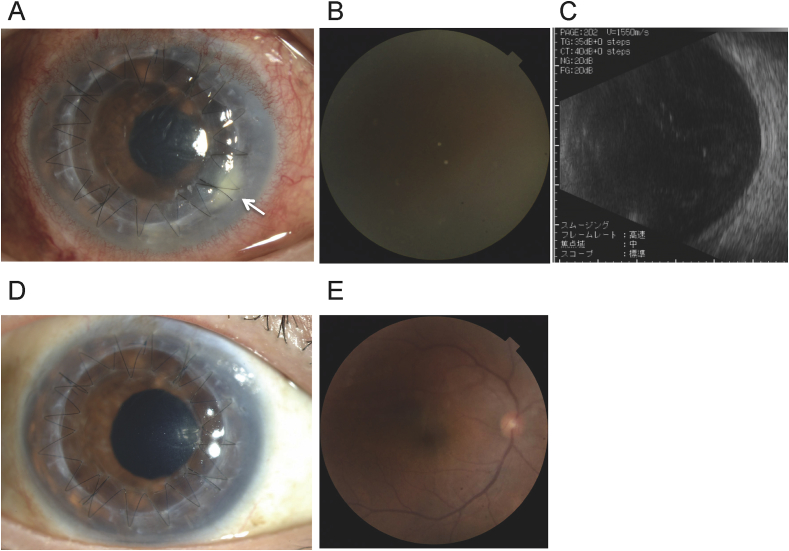
Fig. 2.
Slit-lamp examination, retinal fundus, and B-scan ultrasound images. A-C, slit-lamp examination (A), retinal fundus (B), and B-scan ultrasound (C) images of the patient's right eye prior to undergoing vitrectomy on November 9, 2015. Small white infiltrates (white arrow in A) were observed at the border between the host and donor corneal graft. Retinal fundus and B-scan ultrasound examinations revealed a vitreous opacity. D and E, slit-lamp examination (D) and retinal fundus (E) images of the patient's right eye post intensive treatment (D: slit-lamp image taken on May 10, 2016; E: retinal fundus image taken on December 11, 2015). As can be seen in the images, the white infiltrates on the cornea and vitreous opacity had completely disappeared.
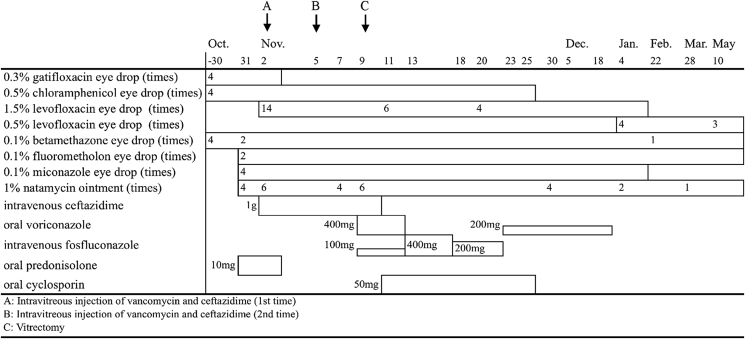
Fig. 3.
Summary of the intensive treatment. A: Intravitreous injection of vancomycin and ceftazidime (1st time), B: Intravitreous injection of vancomycin and ceftazidime (2nd time), C: Vitrectomy.
3. Discussion
Although fungal infections transmitted via corneal transplantation are a very rare occurrence, it has recently become a subject of interest to corneal surgeons and the eye bank community. This is because fungal infection of the eye is a devastating disease. In fact, and as reported in previous studies,5, 6, 8, 9 most patients afflicted with a donor-graft-related fungal infection post PKP must repeat the operation. In the case presented in this study, topical anti-fungal treatment was immediately started in addition to anti-bacterial treatment, as the donor corneoscleral rim culture detected Candida albicans, and endophthalmitis post PKP is reported to be more likely with a culture-positive donor corneoscleral rim.4, 13 In addition, detailed retinal fundus and B-scan ultrasound examinations were repeatedly performed in our patient to evaluate whether the infiltrates had spread to the posterior part of the eye. The surgical intervention, including intravitreal injection and vitrectomy at the appropriate time-points, minimized the damage to the corneal graft and retina and resulted in better visual recovery.
The case presented in this study was quite complicated, with a combination of infectious keratitis and post corneal transplantation at the early postoperative stage. In order to keep corneal transparency without occurring corneal rejection, even during intense infectious treatment, we think that a minimum use of steroids is important. Thus, we did not completely discontinue the steroid treatment, but reduced the frequency of betamethasone eye drops and added to address fluorometholone eye drops. As a result, the findings in this report provide a good insightful method to keep the cornea transparent after intensive treatment including surgical intervention.
Fungal contamination from a donor cornea has become a critical issue, and one that needs to be addressed.3 It has been reported that of 2466 consecutive corneoscleral rims cultured, 325 (13.2%) were found positive for microbial growth, and of those, 28 (8.6%) were found positive for fungus.4 Another report showed that the median annual contamination rate was 5.3%.14 In fact, it has been reported that Candida albicans is responsible for the majority of fungal infections post PKP and Descemet's stripping automated endothelial keratoplasty.3, 4, 5, 6, 7, 9, 15, 16
In our patient, although DNA analysis of the samples obtained from the vitreous fluid and donor corneoscleral rim was not performed, fungal keratitis associated with endophthalmitis was suspected due to the appearance of the donor cornea as well as the cultures of the obtained samples were found to be positive for fungus. Thus, we first initiated anti-fungal treatment in this case due to the well-known high correlation between fungal contaminations of donor corneas and postoperative infections.4, 13 It has been suggested that if drug toxicity to the donor corneal endothelium is minimal, amphotericin B or voriconazole can be added to Optisol-GS ™ in order to prevent the occurrence of fungal endophthalmitis post keratoplasty.17, 18, 19
4. Conclusion
In summary, our prompt intensive medical treatment and surgical intervention effectively saved the vision in a patient with fungal keratitis and endophthalmitis due to contamination of the donor corneal graft. The most important aspect in this current report was the need to adequately perform surgical intervention in addition to intensive medical treatment, which may have been therapeutic in this case, and to use an adequate amount of steroids to keep the cornea transparent, even when the infection occurred. We hope that the findings in this case report will stand as a good reminder of the need to look carefully at all donor tissue prior to transplantation.
Patient consent
Informed consent was obtained in writing from the patient for publication of the report and any accompanying images.
Funding
This research was partially supported in part by the Japanese Society for the Promotion of Science (JSPS) KAKENHI Grant Number 16K20324.
Authorship
All authors confirm that they meet the current ICMJE criteria for authorship.
Conflict of interest statement
Dr. Iliakis reports personal fees from SightLife, outside the submitted work. The following authors have no financial disclosures: K.K., K.W., K.Y., C.S., and S.K.
Acknowledgements
The authors wish to thank John Bush for editing the manuscript.
References
- 1.Tan D.T., Dart J.K., Holland E.J., Kinoshita S. Corneal transplantation. Lancet. 2012;379:1749–1761. doi: 10.1016/S0140-6736(12)60437-1. [DOI] [PubMed] [Google Scholar]
- 2.Eye Bank Association of America; 2015. Eye Banking Statistical Report. [Google Scholar]
- 3.Aldave A.J., DeMatteo J., Glasser D.B. Report of the Eye Bank Association of America medical advisory board subcommittee on fungal infection after corneal transplantation. Cornea. 2013;32:149–154. doi: 10.1097/ICO.0b013e31825e83bf. [DOI] [PubMed] [Google Scholar]
- 4.Keyhani K., Seedor J.A., Shah M.K., Terraciano A.J., Ritterband D.C. The incidence of fungal keratitis and endophthalmitis following penetrating keratoplasty. Cornea. 2005;24:288–291. doi: 10.1097/01.ico..0000138832.3486.70. [DOI] [PubMed] [Google Scholar]
- 5.Sutphin J.E., Pfaller M.A., Hollis R.J., Wagoner M.D. Donor-to-host transmission of Candida albicans after corneal transplantation. Am J Ophthalmol. 2002;134:120–121. doi: 10.1016/s0002-9394(02)01427-7. [DOI] [PubMed] [Google Scholar]
- 6.Kitzmann A.S., Wagoner M.D., Syed N.A., Goins K.M. Donor-related Candida keratitis after Descemet stripping automated endothelial keratoplasty. Cornea. 2009;28:825–828. doi: 10.1097/ICO.0b013e31819140c4. [DOI] [PubMed] [Google Scholar]
- 7.Koenig S.B., Wirostko W.J., Fish R.I., Covert D.J. Candida keratitis after descemet stripping and automated endothelial keratoplasty. Cornea. 2009;28:471–473. doi: 10.1097/ICO.0b013e31818ad9bc. [DOI] [PubMed] [Google Scholar]
- 8.Tappeiner C., Goldblum D., Zimmerli S., Fux C., Frueh B.E. Donor-to-host transmission of Candida glabrata to both recipients of corneal transplants from the same donor. Cornea. 2009;28:228–230. doi: 10.1097/ICO.0b013e318183a3e3. [DOI] [PubMed] [Google Scholar]
- 9.Yamazoe K., Den S., Yamaguchi T., Tanaka Y., Shimazaki J. Severe donor-related Candida keratitis after Descemet's stripping automated endothelial keratoplasty. Graefe's Arch Clin Exp Ophthalmol. 2011;249:1579–1582. doi: 10.1007/s00417-011-1710-0. [DOI] [PubMed] [Google Scholar]
- 10.Kitazawa K., Kayukawa K., Wakimasu K. Cystoid macular edema after Descemet's stripping automated endothelial keratoplasty. Ophthalmology. 2016 doi: 10.1016/j.ophtha.2016.11.001. (in press) [DOI] [PubMed] [Google Scholar]
- 11.Wakimasu K., Sotozono C., Shimizu Y. A retrospective analysis of infection after corneal transplantation. Nippon Ganka Gakkai Zasshi. 2004;108:354–358. [PubMed] [Google Scholar]
- 12.Suzuki T., Tanaka H., Toriyama K. Prospective clinical evaluation of 1.5% levofloxacin ophthalmic solution in ophthalmic perioperative disinfection. J Ocul Pharmacol Ther. 2013;29:887–892. doi: 10.1089/jop.2013.0146. [DOI] [PubMed] [Google Scholar]
- 13.Wilhelmus K.R., Hassan S.S. The prognostic role of donor corneoscleral rim cultures in corneal transplantation. Ophthalmology. 2007;114:440–445. doi: 10.1016/j.ophtha.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 14.Linke S.J., Fricke O.H., Eddy M.T. Risk factors for donor cornea contamination: retrospective analysis of 4546 procured corneas in a single eye bank. Cornea. 2013;32:141–148. doi: 10.1097/ICO.0b013e31825d586b. [DOI] [PubMed] [Google Scholar]
- 15.Gomes J.A., Dana M.R., Dua H.S., Goren M.B., Laibson P.R., Cohen E.J. Positive donor rim culture in penetrating keratoplasty. Cornea. 1995;14:457–462. [PubMed] [Google Scholar]
- 16.Harris D.J., Jr., Stulting R.D., Waring G.O., 3rd, Wilson L.A. Late bacterial and fungal keratitis after corneal transplantation. Spectrum of pathogens, graft survival, and visual prognosis. Ophthalmology. 1988;95:1450–1457. doi: 10.1016/s0161-6420(88)33008-3. [DOI] [PubMed] [Google Scholar]
- 17.Layer N., Cevallos V., Maxwell A.J., Hoover C., Keenan J.D., Jeng B.H. Efficacy and safety of antifungal additives in Optisol-GS corneal storage medium. JAMA Ophthalmol. 2014;132:832–837. doi: 10.1001/jamaophthalmol.2014.397. [DOI] [PubMed] [Google Scholar]
- 18.Ritterband D.C., Shah M.K., Meskin S.W. Efficacy and safety of voriconazole as an additive in Optisol GS: a preservation medium for corneal donor tissue. Cornea. 2007;26:343–347. doi: 10.1097/ICO.0b013e31802d82e8. [DOI] [PubMed] [Google Scholar]
- 19.Duncan K., Parker J., Hoover C., Jeng B.H. The effect of light exposure on the efficacy and safety of amphotericin b in corneal storage media. JAMA Ophthalmol. 2016;134:432–436. doi: 10.1001/jamaophthalmol.2016.0008. [DOI] [PubMed] [Google Scholar]