Abstract
Sleep pattern disruptions have been reported to be associated with an increased risk of obesity. This study was performed to investigate the association between sleep quality and sleep duration with dietary consumption, psychological factors, and obesity in Korean adults. A total of 288 Korean men and women who visited a public health center were included in this study. Data on general characteristics, health-related habits, psychological symptoms, dietary intake, and sleep patterns (including quality and duration) were collected using self-report questionnaires. Approximately half of the included Korean adults experienced sleep of low quality and short duration. Subjects who reported short sleep durations had a significantly higher weight (P=0.015), body mass index (P<0.001), and prevalence of obesity (P=0.012) than those reporting proper sleep durations. After adjustment for covariates, subjects reporting short sleep durations consumed more dietary carbohydrates (P=0.043) and higher levels of perceived stress (P=0.001), depression (P=0.001), and anxiety (P<0.001) than subjects reporting proper sleep durations. However, obesity-related variables, dietary intake and psychosocial symptoms did not differ significantly by reported sleep quality. The results of this study demonstrated that sleep duration but not sleep quality was associated with dietary macronutrient intake and psychological symptoms, which might affect obesity.
Keywords: dietary carbohydrates, sleep quality, sleep duration, psychological variables, obesity
INTRODUCTION
Obesity has been officially recognized as a chronic disease (1) as well as a major risk factor for serious problems, including hypertension, hypercholesterolemia, type 2 diabetes, cardiovascular disease, and some types of cancer (2). Both genetic and environmental factors, such as socioeconomic status, physical activity, and dietary consumption, have been reported to influence obesity risk. Urbanization and industrialization might also be associated with changes in dietary consumption, physical activity, and sleep patterns (2–4). Studies have reported that sleep durations have decreased dramatically over the past few decades (4). Interestingly, a simultaneous increase in the prevalence in obesity has been identified (4).
Insufficient sleep duration may be associated with an increased risk of obesity (5–7). Some studies (6,7), using representative data from the Korean population, have reported short sleep duration to be associated with increased consumption of dietary carbohydrates and/or carbohydrate-rich foods, which may also be associated with a modified risk of obesity. Additionally, obese individuals have been reported to experience more sleep problems, including difficulty falling asleep, sleep disturbances, excessive daytime sleepiness, and insufficient sleep compared to those of normal weight (8,9). To clarify the association between sleep and obesity, sleep patterns should be evaluated, including the assessment of sleep quality as a qualitative indicator and sleep duration as a quantitative indicator. Therefore, in the present study, we examined the associations between obesity, psychological symptoms, and dietary consumption and sleep patterns, including sleep quality, sleep duration, and obesity in a Korean adult population.
SUBJECTS AND METHODS
Subjects
This study was recruited 288 subjects (141 men and 147 women) aged 20 years old who visited the Songpa public health center, which is located in Seoul, Korea. Questionnaires were used to collect data from study subjects between Jan and Feb 2016. The study questionnaires were designed to collect data on general characteristics, health-related habits, psychological symptoms, dietary intake, and sleep patterns. All data were self-reported with the exception of dietary intake. Subjects with current mental illness or who were currently taking sleep or psychological medications that could directly affect sleep pattern were excluded. Additionally, men subjects who consumed <800 kcal/d or ≥4,000 kcal/d and women subjects who consumed <500 kcal/d or ≥3,500 kcal/d were excluded. The study was approved by the Research Council and Ethical Committee of the Ewha Womans University (IRB: 107–18), and all subjects provided written informed consent before participating in the study.
Data collection
General characteristics, such as gender, age, educational level, and occupation, were collected. Educational levels were classified as “≤high school” or “>high school”. Current occupational status was categorized as “unemployed” or “employed”.
Study subjects were asked about alcohol consumption, smoking, physical activity, and use of dietary supplements. Participants were categorized as “non-drinkers” or “drinkers” based on their current alcohol consumption habits and “non-smokers” and “smokers” based on their smoking habits. The consumption of dietary supplements over 3 times per week was assessed, and subjects were classified as non-consumers of dietary supplements (“no”) and dietary supplement consumers (“yes”).
Psychological data, including perceived stress levels, health status and depression, and anxiety symptoms were collected by self-reports. The subjects’ perceived levels of stress and health during the past month were measured using a 5-point Likert scale. Using a score of three times as the cutoff value, subjects were divided into “low stress” and “high stress” groups based on their perceived stress levels and “unhealthy status” and “healthy status” based on their perceived health status. The subjects were divided into “<3 day per week” and “≥3 days per week” groups based on their reported physical activity levels during the past month. Depressive symptoms were measured using the Center for Epidemiologic Studies Depression scale, which may be used to measure depressive symptoms in the general population (10). The scale includes 20 items related to the depressive symptoms experienced during the previous week. The overall scores possible on this scale ranged from 0 to 60. Anxiety symptoms were assessed using the State-Trait Anxiety Inventory, which is a 20-item scale with which the anxiety symptoms experienced during the previous week were assessed (11). The overall scores possible on this scale ranged from 20 to 80.
Body mass index (BMI, kg/m2) was calculated using the following equation: body weight in kilograms divided by the square of height in meters. Obesity was defined in accordance with the definition of obesity in Asian populations proposed by the Western Pacific Regional Office of the World Health Organization as a BMI≥25 kg/m2.
Dietary intake was evaluated using 24-h recall interviews, which were conducted by trained dietitians. To reflect usual dietary consumption habits, all subjects were asked about the food items and their portion sizes of the meal they consumed. The dietary data were analyzed to evaluate average dietary intake using the CAN Pro 4.0 software (Computer-aided nutritional analysis program for professionals, a nutrient database developed by the Korean Nutrition Society (Seoul, Korea). The consumption of each macronutrient (protein, fat, and carbohydrate) was calculated as its percentage of total energy consumption.
Sleep patterns were assessed using the Pittsburgh Sleep Quality Index (PSQI) developed by Buysse et al. (12) and has been widely used to assess sleep quality during the previous month using self-report data. The PSQI consists of 7 elements, including perceived sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction, as has been described previously (12). The total sleep quality score possible ranged from 0 to 21, with higher scores indicating poorer sleep quality. The participants were divided into “poor sleep quality” and “good sleep quality” groups using a cutoff score of 5. Additionally, the participants were divided into “<7.0 hours a day” and “≥7.0 hours a day” based on their reported sleep durations and in accordance with previous studies (13,14).
Statistical analyses
Differences between general characteristics were evaluated using independent Student’s t-tests for continuous variables and chi-square tests for categorical variables. Data are presented as the mean±standard deviation (SD) or N (%). Generalized linear models were used to adjust for confounders, including gender, age, depression, anxiety, alcohol consumption status, and smoking status. A multivariable logistic regression analysis was performed to assess the risk of obesity according to sleep duration and sleep quality as indicated by the calculated odds ratios (ORs) and 95% confidence intervals (CIs). To investigate the association between sleep status and obesity after adjustment for covariates, a logistic regression model was generated. All statistical analyses were completed using SPSS (version 21.0; IBM Corporation, Armonk, NY, USA) software for Windows, and statistical significance was defined as a P<0.05.
RESULTS
The general characteristics were stratified by sleep quality and duration, and these data are shown in Table 1. The average age was 44.2 years, and the average sleep quality score and duration were 5.0 and 6.8 h, respectively. Subjects reporting short sleep durations were significantly older (P<0.001) and reported current alcohol drinking more frequently (P=0.002) compared to subjects reporting proper sleep durations. Short sleep duration was associated with several obesity-related variables. Body weight (65.9±1.2 kg vs. 62.3±0.9 kg, P=0.015) and BMI (23.9±0.3 kg/m2 vs. 22.4±0.2 kg/m2, P<0.001) were significantly higher in subjects reporting short sleep durations compared with those reporting proper sleep durations. In addition, the prevalence of obesity was approximately 1.7 times higher in subjects reporting short sleep durations than in those reporting proper sleep durations (31.8% vs. 18.8%, P=0.012). However, no significant differences were identified in smoking, exercise, or education by reported sleep duration. In addition, none of the general characteristic variables differed significantly by reported sleep quality.
Table 1.
General characteristics of the population according to sleep quality and sleep duration
| Sleep quality | Sleep duration | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Poor (n=97) | Good (n=191) | P | <7 h (n=107) | ≥7 h (n=181) | P | |
| Age (years) | 45.0±1.7 | 43.8±1.3 | 0.582 | 49.8±1.5 | 40.9±1.3 | <0.001 |
| Sex | 0.531 | 0.171 | ||||
| Men | 50 (51.5) | 91 (47.6) | 58 (54.2) | 83 (45.9) | ||
| Women | 47 (48.5) | 100 (52.4) | 49 (45.8) | 98 (54.1) | ||
| Height (cm) | 166.8±1.0 | 165.4±0.6 | 0.209 | 165.6±0.9 | 166.1±0.6 | 0.642 |
| Weight (kg) | 64.5±1.4 | 63.3±0.8 | 0.375 | 65.9±1.2 | 62.3±0.9 | 0.015 |
| BMI (kg/m2) | 23.0±0.3 | 23.0±0.2 | 0.980 | 23.9±0.3 | 22.4±0.2 | <0.001 |
| Obesity prevalence (%) | 28.9 | 20.9 | 0.135 | 31.8 | 18.8 | 0.012 |
| Alcohol consumption | 0.324 | 0.002 | ||||
| Non-drinker | 45 (46.4) | 77 (40.3) | 58 (54.2) | 64 (35.4) | ||
| Current drinker | 52 (53.6) | 114 (59.7) | 49 (45.8) | 117 (64.6) | ||
| Smoking | 0.567 | 0.236 | ||||
| Non-smoker | 83 (85.6) | 168 (88.0) | 90 (84.1) | 161 (89.0) | ||
| Current smoker | 14 (14.4) | 23 (12.0) | 17 (15.9) | 20 (11.0) | ||
| Dietary supplementation | 0.371 | 0.433 | ||||
| No | 51 (52.6) | 111 (58.1) | 57 (53.3) | 105 (58.0) | ||
| Yes | 46 (47.4) | 80 (41.9) | 50 (46.7) | 76 (42.0) | ||
| Exercise (≥30 min) | 0.686 | 0.170 | ||||
| <3 d/wk | 56 (57.7) | 115 (60.2) | 58 (54.2) | 113 (62.4) | ||
| ≥3 d/wk | 44 (42.3) | 76 (39.8) | 49 (45.8) | 68 (37.6) | ||
| Education | 0.061 | 0.523 | ||||
| ≤High school | 33 (34.0) | 87 (45.5) | 42 (39.4) | 78 (43.1) | ||
| >High school | 64 (66.0) | 104 (54.5) | 65 (60.7) | 103 (56.9) | ||
| Job | 0.234 | 0.431 | ||||
| Unemployed | 41 (42.3) | 67 (35.1) | 71 (39.2) | 108 (37.5) | ||
| Employed | 56 (57.7) | 124 (64.9) | 110 (60.8) | 180 (62.5) | ||
Values represent the mean±SD or N (%).
P-values were calculated using the Student’s t-test and the chi-square test.
Significant differences in dietary macronutrient consumption were observed by reported sleep duration but not by reported sleep quality in the crude model and age, gender, alcohol consumption status, and smoking status-adjusted model (Table 2). In the crude model, subjects reporting short sleep durations had significantly higher carbohydrate consumptions (60.9±0.9% vs. 57.4±0.8%, P=0.005) and lower fat consumptions (23.2±0.9% vs. 26.4±0.7%, P=0.004) than subjects reporting proper sleep durations. After adjustment for covariates, carbohydrates were consumed more (P=0.043), but not fats (P=0.090) in subjects with short sleep. However, no significant difference between dietary protein consumption and sleep duration was observed in either the crude or the adjusted model. Additionally, the consumption of all dietary macronutrients did not differ significantly by sleep quality.
Table 2.
Dietary macronutrient intake according to sleep quality and sleep duration
| Sleep quality | Sleep duration | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Poor (n=99) | Good (n=189) | P*1) | P**2) | <7 h (n=107) | ≥7 h (n=181) | P* | P** | |
| Energy (kcal/d) | 1,875.7±56.0 | 1,851.5±39.9 | 0.724 | 0.832 | 1,854.0±52.0 | 1,863.3±41.5 | 0.891 | 0.973 |
| Carbohydrates (% of E) | 58.7±1.1 | 58.7±0.8 | 0.945 | 0.782 | 60.9±0.9 | 57.4±0.8 | 0.005 | 0.043 |
| Protein (% of E) | 16.1±0.4 | 16.2±0.3 | 0.944 | 0.905 | 15.9±0.4 | 16.3±0.3 | 0.369 | 0.134 |
| Fat (% of E) | 25.1±1.0 | 25.2±0.7 | 0.982 | 0.788 | 23.2±0.9 | 26.4±0.7 | 0.004 | 0.090 |
Values represent the mean±SD.
Values were calculated using the Student’s t-test.
Values were calculated using a generalized linear model adjusted for age, sex, alcohol consumption status, and smoking status.
Physiological variable values, including perceived stress, depression, and anxiety according to sleep quality and sleep duration were examined in the crude and adjusted models (Table 3). Perceived stress (P=0.047), depression (P=0.002), and anxiety (P=0.004) by sleep duration were significantly different in the crude model. Subjects reporting short sleep durations reported higher levels of perceived stress (1.6±0.1 vs. 1.3±0.1, P=0.001), depression (14.3±0.9 vs. 10.8±0.6, P=0.001), and anxiety (42.0±1.1 vs. 38.0±0.8, P<0.001) than subjects reporting proper sleep in the adjusted model. However, no significant differences between psychological symptoms and sleep quality observed in either the crude or the adjusted models.
Table 3.
Physiological variable values according to sleep quality and sleep duration
| Sleep quality | Sleep duration | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Poor (n=99) | Good (n=189) | P*1) | P**2) | <7 h (n=107) | ≥7 h (n=181) | P* | P** | |
| Perceived stress | 1.4±0.1 | 1.4±0.1 | 0.524 | 0.722 | 1.6±0.1 | 1.3±0.1 | 0.047 | 0.001 |
| Depression score | 11.9±0.8 | 12.2±0.7 | 0.798 | 0.837 | 14.3±0.9 | 10.8±0.6 | 0.002 | 0.001 |
| Anxiety score | 39.5±1.1 | 39.5±0.8 | 0.987 | 0.799 | 42.0±1.1 | 38.0±0.8 | 0.004 | <0.001 |
Values represent the mean±SD.
Values were calculated using the Student’s t-test.
Values were calculated using a generalized linear model adjusted for age, sex, alcohol consumption status, and smoking status.
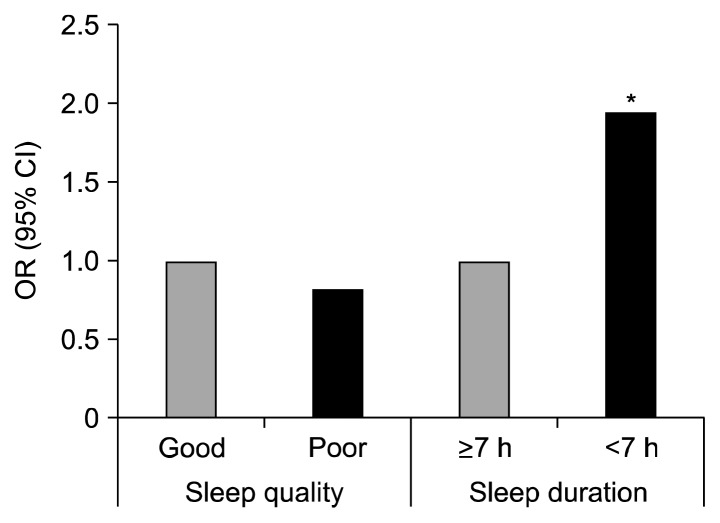
The ORs for risk of obesity by sleep quality and duration were estimated based on multivariate logistic regression models adjusted for age, gender, alcohol consumption status, and smoking status (Fig. 1). A significant association between sleep duration and the ORs for obesity risk was observed (P=0.036). The ORs for obesity risk were 1.95 times (95% CIs=1.05~3.64) higher among subjects reporting short sleep durations compared with those who slept properly after adjusting for age, gender, alcohol drinking, and smoking status. However, no significant differences were observed with the ORs of obesity in terms of sleep quality in the adjusted model.
Fig. 1.
Odd ratios for the associations between obesity and sleep quality and sleep duration. P-values based on the logistic regression adjusted for age, gender, alcohol consumption status, and smoking status. OR (95% CI): odds ratio (95% confidence interval).
DISCUSSION
In this study, 49.0% of Korean adults had low quality sleep according to the PSQI (12) criteria, and 54.0% of the subjects reported short sleep durations of less than 7.0 hours a day (13,14). The obesity-related, dietary macronutrient consumption, and psychological variables were associated with sleep duration but not sleep quality in the age, gender, alcohol drinking, and smoking status-adjusted models.
Short sleep durations were associated with several obesity-related variables, a finding that is consistent with the results of our previous studies (6,7). Body weight, BMI, and prevalence of obesity were higher in participants reporting short sleep durations compared to those in proper sleepers group. These results might be postulated to be associated with changes in dietary consumption (15, 16), the levels of hormones that contribute to metabolic profiles (17–19), and psychological symptoms (20,21).
In this study, significant differences were identified in the associations between dietary macronutrient consumption and psychological symptom and sleep duration after adjustment for age, gender, alcohol drinking, and smoking status. Subjects reporting short sleep durations consumed more dietary carbohydrates and experienced more psychological problems, including perceived stress, anxiety, and depressive symptoms, than subjects reporting proper sleep durations. Some studies (17–19) have reported that sleep deprivation was associated with a reduced level of circulating leptin and elevated level of ghrelin, which may result in increased appetite and food intake. In addition, increased dietary carbohydrate consumption, defined as increased consumption of carbohydrate-rich foods in the form of snacks or meals, have been observed in short sleepers (5,22). Many studies (23–25) have reported an association between psychosocial symptoms and sleep. According to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (23), short sleep duration is one of symptoms of psychological conditions, including depression and anxiety. Furthermore, sleep disorders may directly contribute to increased risk of developing some psychosocial problems, and these problems may lead to obesity.
Unfortunately, in this study, none of the obesity-related dietary consumption or psychosocial symptom variables were significantly associated with sleep quality. These results might be explained by several limitations. First, the sample size was small to derive a definitive conclusion regarding the association between sleep patterns and obesity in Korean. Second, although PSQI is a well-developed and widely used tool for the measurement of sleep quality, sleep quality may be affected by various factors such as physiological variables and seasonal variations. Therefore, further studies will need to be conducted to clarify these associations in a larger population. Although some limitations existed, the results of this study demonstrated that short sleep duration but not poor sleep quality was associated with high dietary macronutrient intake and psychological problems, which might affect obesity.
ACKNOWLEDGEMENTS
The authors declare no competing interests. This research was supported PRogram for Industrial needs-Matched Education (PRIME), Ewha Womans University funded by the Ministry of Education of Korea; and the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science (NRF-2016R1C1B1010094). The authors’ responsibilities were as follows: Yangha Kim (YK) and Miae Doo (MD), study concept and design; Bori Kang (BK) and MD, data collection; MD and BK, data statistical analysis, interpretation and draft of the manuscript; MD and YK, review of the manuscript. All authors read and approved the final version of the manuscript.
Footnotes
AUTHOR DISCLOSURE STATEMENT
The authors declare no conflict of interest.
REFERENCES
- 1.Pollack A. [accessed Apr 2017];AMA recognizes obesity as a disease. 2013 http://www.nytimes.com/2013/06/19/business/ama-recognizesobesity-as-a-disease.html.
- 2.World Health Organization. [accessed Apr 2017];Diet, nutrition and the prevention of chronic diseases. 2003 http://www.who.int/dietphysicalactivity/publications/trs916/en/ [PubMed]
- 3.World Health Organization. [accessed Apr 2017];Global strategy on diet, physical activity and health. 2004 http://www.who.int/dietphysicalactivity/strategy/eb11344/strategy_english_web.pdf.
- 4.Knutson KL, Van Cauter E, Rathouz PJ, DeLeire T, Lauderdale DS. Trends in the prevalence of short sleepers in the USA: 1975–2006. Sleep. 2010;33:37–45. doi: 10.1093/sleep/33.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rahe C, Czira ME, Teismann H, Berger K. Associations between poor sleep quality and different measures of obesity. Sleep Med. 2015;16:1225–1228. doi: 10.1016/j.sleep.2015.05.023. [DOI] [PubMed] [Google Scholar]
- 6.Doo M, Kim Y. Association between sleep duration and obesity is modified by dietary macronutrients intake in Korean. Obes Res Clin Pract. 2016;10:424–431. doi: 10.1016/j.orcp.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Doo M, Kim Y. The risk of being obese according to short sleep duration is modulated after menopause in Korean women. Nutrients. 2017;9:206. doi: 10.3390/nu9030206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vargas PA, Flores M, Robles E. Sleep quality and body mass index in college students: the role of sleep disturbances. J Am Coll Health. 2014;62:534–541. doi: 10.1080/07448481.2014.933344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Komada Y, Narisawa H, Ueda F, Saito H, Sakaguchi H, Mitarai M, Suzuki R, Tamura N, Inoue S, Inoue Y. Relationship between self-reported dietary nutrient intake and self-reported sleep duration among Japanese adults. Nutrients. 2017;9:134. doi: 10.3390/nu9020134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chon KK, Lee MK. MKR: preliminary development of Korean version of CES-D. Korean J Clin Psychol. 1992;11:65–76. [Google Scholar]
- 11.Hahn DW, Lee CH, Chon KK. Korean adaptation of Spielberger’s STAI (K-STAI) Korean J Health Psychol. 1996;1:1–14. [Google Scholar]
- 12.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 13.Bixler E. Sleep and society: an epidemiological perspective. Sleep Med. 2009;10:S3–S6. doi: 10.1016/j.sleep.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 14.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18:148–158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 15.Haghighatdoost F, Karimi G, Esmaillzadeh A, Azadbakht L. Sleep deprivation is associated with lower diet quality indices and higher rate of general and central obesity among young female students in Iran. Nutrition. 2012;28:1146–1150. doi: 10.1016/j.nut.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 16.Markwald RR, Melanson EL, Smith MR, Higgins J, Perreault L, Eckel RH, Wright KP., Jr Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proc Natl Acad Sci USA. 2013;110:5695–5700. doi: 10.1073/pnas.1216951110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Omisade A, Buxton OM, Rusak B. Impact of acute sleep restriction on cortisol and leptin levels in young women. Physiol Behav. 2010;99:651–656. doi: 10.1016/j.physbeh.2010.01.028. [DOI] [PubMed] [Google Scholar]
- 18.Simpson NS, Banks S, Dinges DF. Sleep restriction is associated with increased morning plasma leptin concentrations, especially in women. Biol Res Nurs. 2010;12:47–53. doi: 10.1177/1099800410366301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suarez EC. Self-reported symptoms of sleep disturbance and inflammation, coagulation, insulin resistance and psychosocial distress: evidence for gender disparity. Brain Behav Immun. 2008;22:960–968. doi: 10.1016/j.bbi.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hinz A, Glaesmer H, Brähler E, Löffler M, Engel C, Enzenbach C, Hegerl U, Sander C. Sleep quality in the general population: psychometric properties of the Pittsburgh Sleep Quality Index, derived from a German community sample of 9284 people. Sleep Med. 2017;30:57–63. doi: 10.1016/j.sleep.2016.03.008. [DOI] [PubMed] [Google Scholar]
- 22.Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, Penev PD. Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr. 2009;89:126–133. doi: 10.3945/ajcn.2008.26574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. American Psychiatric Publishing; Washington, DC, USA: 2013. p. 551. [Google Scholar]
- 24.Glozier N, Martiniuk A, Patton G, Ivers R, Li Q, Hickie I, Senserrick T, Woodward M, Norton R, Stevenson M. Short sleep duration in prevalent and persistent psychological distress in young adults: the DRIVE study. Sleep. 2010;33:1139–1145. doi: 10.1093/sleep/33.9.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liang W, Chikritzhs T. Sleep duration and its links to psychological distress, health status, physical activity and body mass index among a large representative general population sample. Int J Clin Med. 2013;4:45–51. doi: 10.4236/ijcm.2013.41010. [DOI] [Google Scholar]