Abstract
Objective:
This meta-analysis aims to determine whether hemoglobin A1c (HbA1c) and perioperative hyperglycemia are associated with the increased risk of periprosthetic joint infection following total knee and hip arthroplasty.
Methods:
A systematic search is performed in Medline (1966–October 2017), PubMed (1966–October 2017), Embase (1980–October 2017), ScienceDirect (1985–October 2017), and the Cochrane Library. Only high-quality studies are selected. A meta-analysis is performed using Stata 11.0 software.
Results:
Six retrospective studies including 26,901 patients meet the inclusion criteria. The present meta-analysis indicates that there are significant differences between groups in terms of perioperative random blood glucose level [weighted mean difference (WMD) = 2.365, 95% confidence interval (95% CI): 1.802–2.929, P = .000] and perioperative hemoglobin A1c level (WMD = 3.266, 95% CI: 2.858–3.674, P = .000). No significant difference is found regarding body mass index (BMI) condition between groups (WMD = 0.027, 95% CI: -0.487 to 0.541, P = .919).
Conclusion:
The present meta-analysis shows that high HbA1c and perioperative hyperglycemia are associated with a higher risk of periprosthetic joint infection following total joint arthroplasty. Screening of HbA1c and perioperative blood glucose is therefore an effective method to predict deep infection.
Keywords: hemoglobin A1c, hyperglycemia, meta-analysis, periprosthetic joint infection, total joint arthroplasty
1. Introduction
Total knee arthroplasty and total hip arthroplasty (TKA and THA) are considered reliably successful procedures for the treatment of degenerative arthritis, rheumatoid arthritis, and traumatic disease such as displaced femoral neck fractures. However, surgical site infections remain a devastating type of complication that is of deep concern for patients and surgeons alike. It can lead to periprosthetic joint infection, which prolongs hospital stays, delays recoveries, and leads to corrective surgeries, which are a financial burden. It has been reported that the infection rate of TKA is 1% to 3% and 0.7% to 2.5% for THA.[1–6]
With an aging population, the number of joint arthroplasty surgeries is expected to rise. There will be an estimated 4 million joint arthroplasties performed annually in the USA by 2030 and approximately 8% of these patients will have diabetes mellitus (DM).[7] Previous studies have reported that the presence DM has been identified as a possible risk factor for postoperative complications such as surgical site infections, nonunion, and other medical complications.[8,9] High-quality evidence is inconsistent regarding the role of glycemic control on the risk of surgical site infections. Marchant et al[9] found that patients with uncontrolled DM were associated with a significantly increased risk of surgical site infections and mortality following total joint arthroplasty. However, this result could not be replicated in recent articles, which measured glycemic control by hemoglobin A1c (HbA1c).[10,11] Perioperative hyperglycemia caused by surgical stress was also reported to be an independent risk factor for postoperative surgical site infection even in patients without a DM diagnosis.
To our knowledge, whether there was a close relationship between perioperative hyperglycemia and postoperative periprosthetic joint infection or not remains controversial. Therefore, we performed a meta-analysis from clinical controlled trials to determine whether HbA1c and perioperative hyperglycemia were associated with an increased risk of periprosthetic joint infection following total knee and hip arthroplasty.
2. Methods
This meta-analysis was reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. All analyses were based on previous published studies; thus, no ethical approval and patient consent are required.
2.1. Search strategy
We systemically search electronic databases, including Embase (1980–October 2017), Medline (1966–October 2017), PubMed (1966–October 2017), ScienceDirect (1985–October 2017), web of science (1950–October 2017), and Cochrane Library for potential relevant articles. Gray academic studies are also identified from the reference of included studies. No language is restricted. The following terms are considered as key words: “Total knee replacement OR arthroplasty,” “Total hip replacement OR arthroplasty,” “hyperglycemia,” “HbA1c,” and “periprosthetic joint infection” were used in combination with Boolean operators AND or OR. The retrieval process is presented in Fig. 1.
Figure 1.
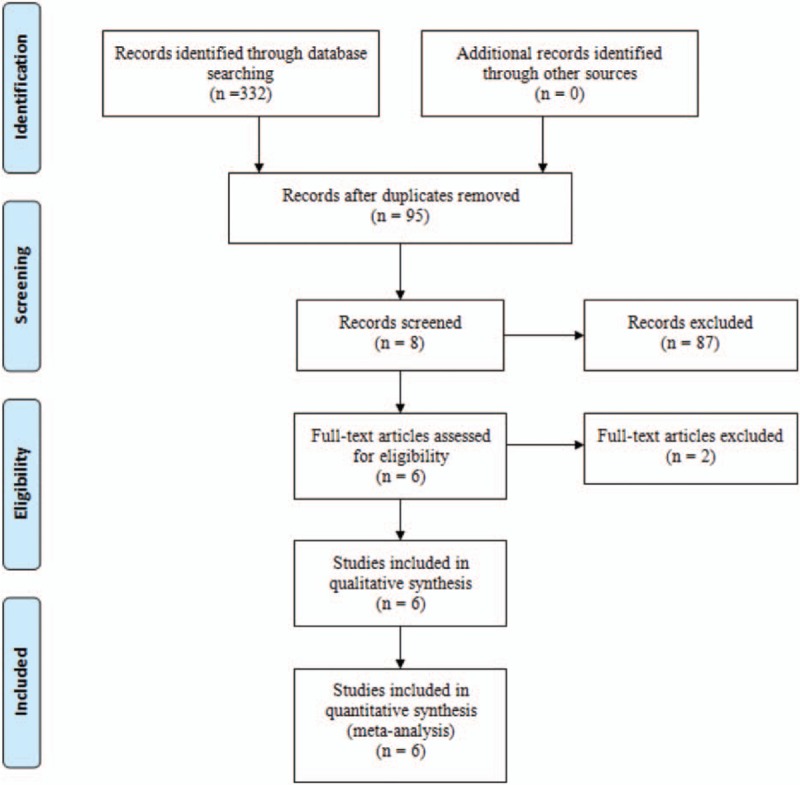
Search results and the selection procedure.
2.2. Inclusion and exclusion criteria
Studies were considered eligible if they meet the following criteria: published clinical retrospective study; a study that was performed to explore the relationship between perioperative hyperglycemia and postoperative periprosthetic joint infection for patient undergoing TKA or THA surgery; cases and controls are defined on the basis of presence or absence of periprosthetic joint infection. Studies will be excluded from present meta-analysis for incomplete data, cases report, conference abstract, or review articles.
2.3. Selection criteria
Two reviewers independently review the abstract of the potential studies. After an initial decision, full text of the studies that potentially meet the inclusion criteria are reviewed and final decision is made. A senior reviewer is consulted in case of disagreement.
2.4. Date extraction
A standard form for date extraction is printed for date extraction. Two reviewers independently extracted the relevant data from the included studies. Details of incomplete data of included articles are received by consulting corresponding author. Following data are extracted: First author names, published year, study design, comparable baseline, intervening procedures, and the incidence of periprosthetic joint infection. Other relevant data are also extracted from individual studies.
2.5. Quality assessment
Quality assessment of included studies is performed by 2 reviewers independently. The Methodological Index for Non-Randomized Studies (MINORS) scale, which assigns scores ranging from 0 to 24, is used to assess the methodological quality of the included studies in the present meta-analysis, which is based on the 12 main items. A consensus is reached through a discussion.
2.6. Data analysis and statistical methods
All calculations are carried out by Stata 11.0 (The Cochrane Collaboration, Oxford, UK). Statistical heterogeneity is assessed on the basis of the value of P and I2 using standard Chi-square test. When I2 >50%, P < .1 is considered to be significant heterogeneity, random-effect model is performed for meta-analysis. Otherwise, fixed-effect model is used. If possible, sensibility analysis is conducted to explore the origins of heterogeneity. The results of dichotomous outcomes are expressed as risk difference (odds ratio, OR) with 95% confidence intervals (95% CIs). For continuous various outcomes, mean difference (MD) and weighted mean difference (WMD) with a 95% CIs is applied for assessment. Funnel plots are created to determine the presence of publication bias.
3. Results
3.1. Search result
A total of 332 studies are preliminarily reviewed. By reading the title and abstracts, 326 reports are excluded from current meta-analysis followed inclusion criteria. No gray reference is obtained. Finally, 6 retrospective studies,[12–17] which have been published between 2010 and 2016 are enrolled in present meta-analysis and includes 532 participates in the infected groups and 26,369 patients in the noninfected groups. Demographic characteristics and the details about the included studies are summarized in Table 1.
Table 1.
Trials characteristics.
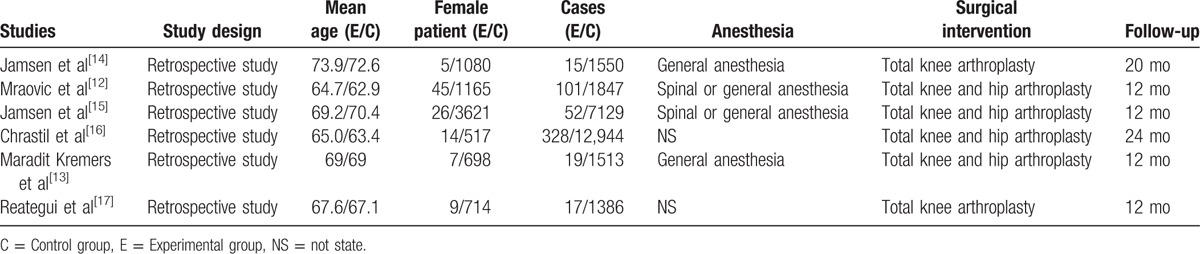
3.2. Study characteristics
The sample size of the included studies ranges from 1403 to 13,272. All of them evaluate the correlation between perioperative hyperglycemia and the increased risk of periprosthetic joint infections following total joint arthroplasty. Experimental groups experience periprosthetic joint infection, while control groups do not experience periprosthetic joint infections. Four studies[12–15] apply general or spinal anesthesia, while the others[16,17] do not report on their use. All[12–17] studies report that the surgical procedure is performed by the same team. All of them suggest the outcomes for at least 95% of their patients. The follow-up period ranges from 12 to 24 months.
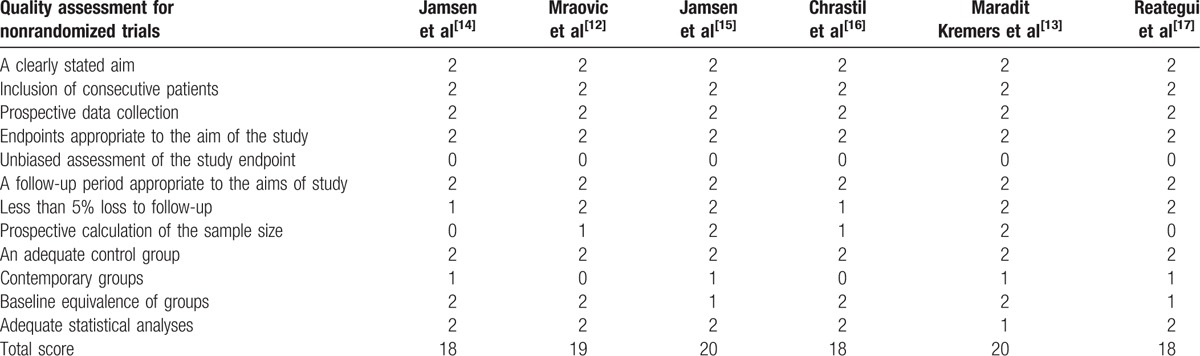
3.3. Methodological quality assessment
The MINORS scale is used to assess nonrandomized controlled trials (non-RCTs) by assigning scores ranging from 0 to 24 (Table 2). The outcome of the methodology quality assessment is as follows: 3 studies[14,16,17] scored 18, 1 study[12] scored 19, and 2 studies[13,15] scored 20.
Table 2.
Methodological quality of the included studies.
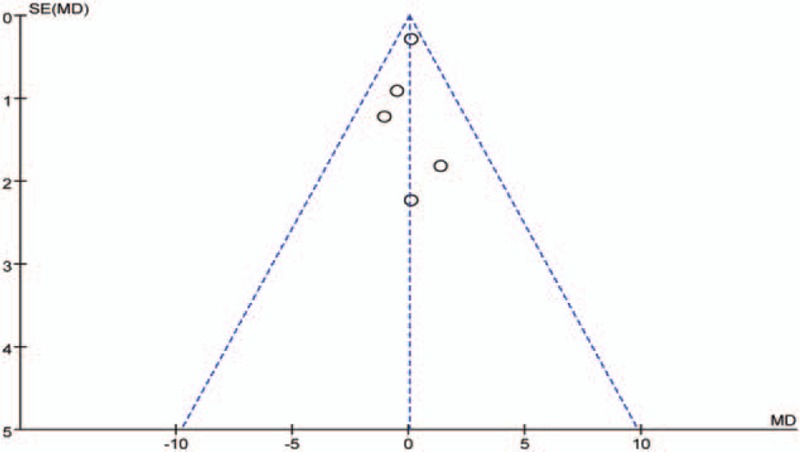
3.4. Publication bias
As only 6 studies reported perioperative random blood glucose, publication bias is assessed and presented in Fig. 2. Funnel plots were symmetrical and a low risk of publication bias was demonstrated. Figure 3 assesses the publication bias of BMI condition, and also shows a low risk. However, publication bias could not be excluded, as the reliability of this kind of assessment is especially weak when a low number of studies are included.
Figure 2.
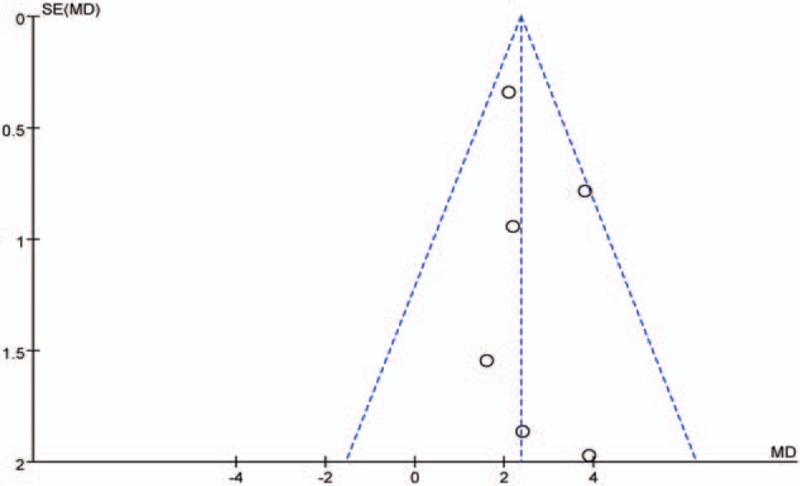
Funnel plot of perioperative random blood glucose level.
Figure 3.
Funnel plot of BMI condition.
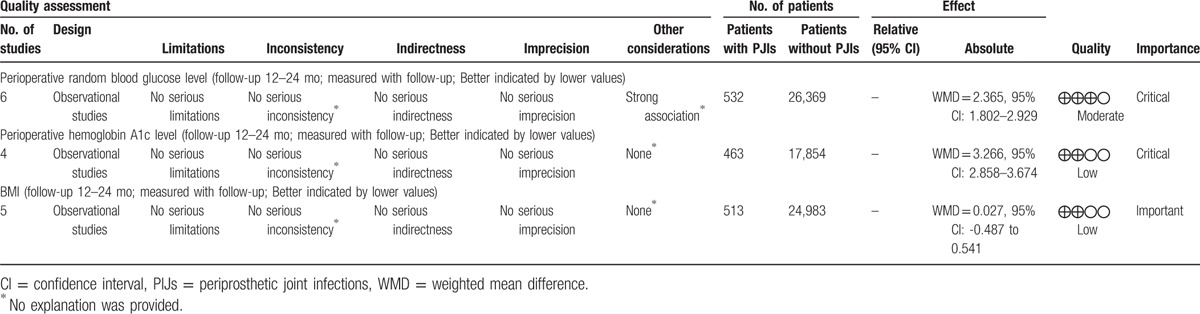
3.5. Evidence level
All outcomes in this meta-analysis were evaluated using the Recommendations Assessment, Development and Evaluation (GRADE) system. The evidence quality for most outcomes was low (Table 3), meaning that further research is likely to significantly change confidence in the effect estimate as well as the estimate.
Table 3.
The GRADE evidence quality for each outcome.
3.6. Outcomes for meta-analysis
3.6.1. Perioperative random blood glucose level
All studies[12–17] report perioperative random blood glucose level following total joint arthroplasty. There is no significant heterogeneity (χ2 = 4.82, df = 5, I2 = 0.0%, P = .438); therefore, a fixed-effects model is used. The result of meta-analysis shows that perioperative random blood glucose level in experimental groups is significantly higher than in control groups (WMD = 2.365, 95% CI: 1.802–2.929, P = .000; Fig. 4).
Figure 4.
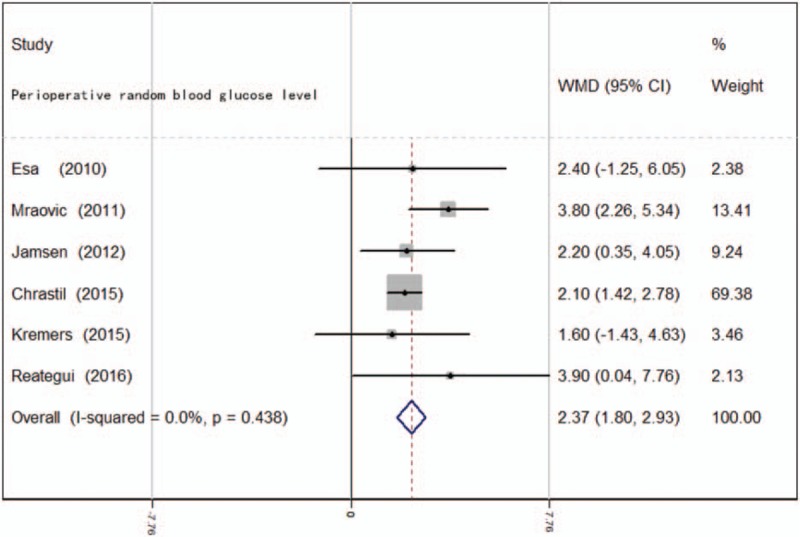
Forest plot diagram showing perioperative random blood glucose level following total joint arthroplasty.
3.6.2. Perioperative hemoglobin A1c level
Four studies[12–14,16] report postoperative A1c level. There is no significant heterogeneity among these studies (χ2 = 6.33, df = 3, I2 = 52.6%, P = .097); therefore, a fixed-effects model is used. Pooled results demonstrate that the perioperative HbA1c level in experimental groups is significantly higher than in control groups (WMD = 3.266, 95% CI: 2.858–3.674, P = .000; Fig. 5).
Figure 5.
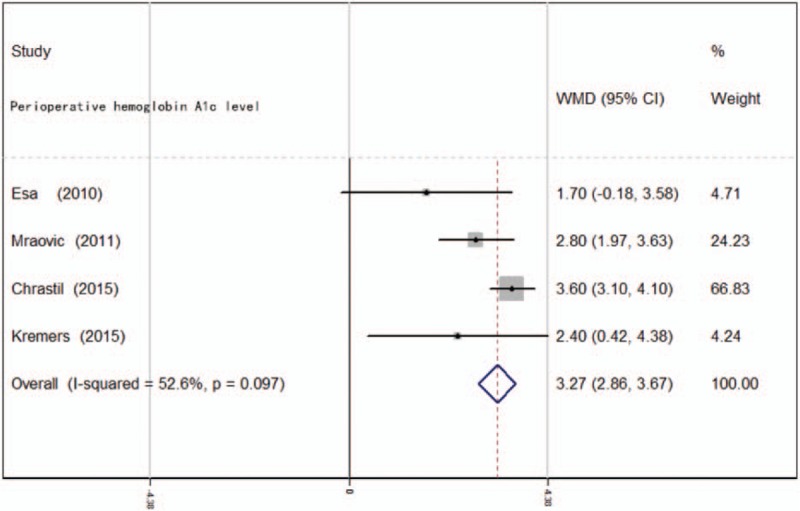
Forest plot diagram showing perioperative hemoglobin A1c level following total joint arthroplasty.
3.6.3. Body mass index (BMI)
Five studies[12–16] report BMI condition for the included patients. There is no significant heterogeneity among these studies (χ2 = 1.67, df = 4, I2 = 0.0%, P = .796); therefore, a fixed-effects model is used. Pooled results demonstrate that there is no significant difference between the groups regarding BMI condition (WMD = 0.027, 95% CI: -0.487 to 0.541, P = .919; Fig. 6).
Figure 6.
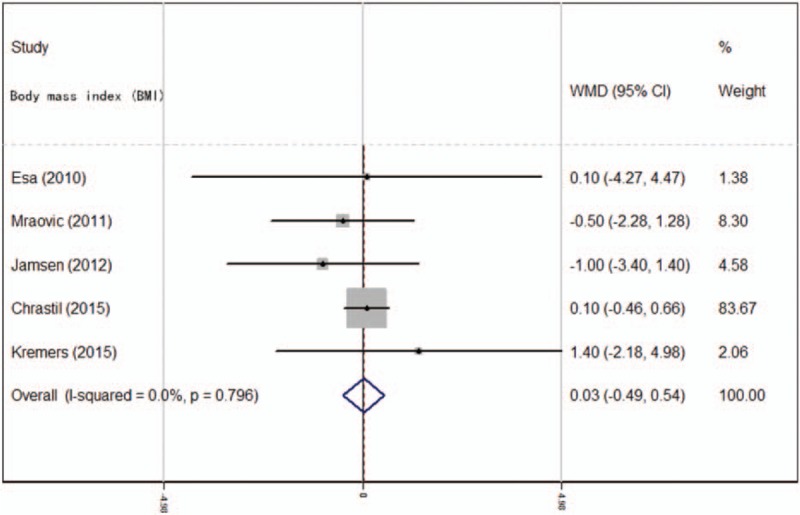
Forest plot diagram showing BMI condition between groups.
4. Discussion
The most important finding of the meta-analysis is that the perioperative random blood glucose level and HbA1c are associated with a significantly higher risk of periprosthetic joint infection. Moreover, no relationship between BMI condition and the risk of infection is identified.
Periprosthetic joint infection is considered one of the most severe postsurgical complications following total joint arthroplasty surgeries. It can lead to substantial health burden and a poor quality of life for patients. Previous studies have reported that the incidence of infection ranges from 1.5% to 6.8%[18–20] among diabetic patients undergoing TKA. Several studies have assessed the risk factors for wound infections; however, any conclusion remains controversial. A substantial number of articles suggest a close relationship between DM and infection, while some studies maintain the opposite view. A recent comparative study found that the postoperative infection rate was 1.2% and 0.7%[21] in patients with or without DM (P > .05). Marchant et al[9] also reported that the incidence of periprosthetic joint infection was similar in patients both with and without DM. One reason for this anomalous result is that it is possible that these studies were not sufficiently powered to reach authoritative conclusions. Routinely used antibiotic-loaded cement, which is suggested as a way to prevent the periprosthetic joint infection, also contributes to the fairly small difference. More importantly, although the number of DM patients is provided in these investigations, none of them attempted to measure perioperative blood glucose levels, or their data were imprecise. Although Marchant et al[9] found no correlation between DM and deep infections, the infection rate was 2.3 times greater in patients with poor glycemic control. Therefore, perioperative blood glucose level is a more convincing predictor than the diagnosis of DM for periprosthetic joint infection. The present meta-analysis indicates that there was a significant difference between the groups regarding perioperative random blood glucose level.
HbA1c is indicative of a patient's glycemic status over a 2 to 3-month time by accessible and objective laboratory examination, and is therefore used as a serological marker for controlling blood glucose in diabetic patients. Some studies have recommended that an HbA1c level of less than 7% could decrease the risk of systemic complications. Therefore, an HbA1c level of 7% has been considered the cutoff for glycemic control in previous studies. Whether or not HbA1c truly is predictive of periprosthetic joint infection remains controversial. Iorio et al[11] report that HbA1c levels are not reliable for predicting the risk of infection after total joint arthroplasties. However, these studies have been criticized for a small number of patient who did not allow an adequately powered analysis. The present meta-analysis indicates that there was a significant difference between the groups with regard to their HbA1c level.
Another worthy question is whether blood glucose and HbA1c testing should or should not be performed as a standard routine for patients undergoing total joint arthroplasties. Subsequently, should there be a delayed operation for patients with abnormal values? The American Diabetes Association recommends that all patients with a DM diagnosis and those who are experiencing hyperglycemia should have their blood glucose monitored.[22] Meanwhile, the Endocrine Society guidelines suggest that blood glucose and HbA1c should be tested for patients with or without a DM diagnosis.[23] This action is based on the relationship between inpatients’ hyperglycemia and the possibility of first being diagnosed with DM during hospitalization. Indeed, it is believable that some of the periprosthetic joint infection cases were medicated by unidentified hyperglycemia or DM. In addition, poor hyperglycemia control is associated with other infections, such as pneumonia, urinary infection, and others. Although we found that HbA1c and perioperative hyperglycemia are predictive of periprosthetic joint infection, the optimal threshold of blood glucose remains unclear. Currently, outcomes for intervention of strict blood glucose are inconclusive. Hence, high-quality randomized controlled trials with long-term follow-up are required in the joint arthroplasty population.
There are several limitations in the present meta-analysis. Only 6 studies were included, and all of them were retrospectives, which are likely to suffer from various types of bias. Some important outcome parameters, such as pneumonia and urinary infection, were not clearly described and could not be reported in the present meta-analysis. The overall GRADE quality of evidence is moderate to low, which influences confidence in any subsequent recommendations. Short-term follow-up may lead to underestimation of complications. Publication bias is an inherent weakness that exists in all meta-analysis.
5. Conclusion
The present meta-analysis shows that high HbA1c and perioperative hyperglycemia are associated with a higher risk of periprosthetic joint infection following total joint arthroplasty. Screening of HbA1c and perioperative blood glucose is therefore an effective method to predict deep infection.
Footnotes
Abbreviations: DM = diabetes mellitus, HbA1c = hemoglobin A1c, THA = total hip arthroplasty, TKA = total knee arthroplasty.
Authorship: GL and JLL conceived the design of the study. YFS performed and collected the data and contributed to the design of the study. LQY finished the manuscript. All authors read and approved the final manuscript.
The authors declare that they have no competing interests.
References
- [1].Tsung JD, Rohrsheim JA, Whitehouse SL, et al. Management of periprosthetic joint infection after total hip arthroplasty using a custom made articulating spacer (CUMARS); the Exeter experience. J Arthroplasty 2014;29:1813–8. [DOI] [PubMed] [Google Scholar]
- [2].National Nosocomial Infections Surveillance S. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control 2004;32:470–85. [DOI] [PubMed] [Google Scholar]
- [3].Maoz G, Phillips M, Bosco J, et al. The Otto Aufranc Award: modifiable versus nonmodifiable risk factors for infection after hip arthroplasty. Clin Orthop Relat Res 2015;473:453–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Liu C, Kakis A, Nichols A, et al. Targeted use of vancomycin as perioperative prophylaxis reduces periprosthetic joint infection in revision TKA. Clin Orthop Relat Res 2014;472:227–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Frank RM, Cross MB, Della Valle CJ. Periprosthetic joint infection: modern aspects of prevention, diagnosis, and treatment. J Knee Surg 2015;28:105–12. [DOI] [PubMed] [Google Scholar]
- [6].Bozic KJ, Grosso LM, Lin Z, et al. Variation in hospital-level risk-standardized complication rates following elective primary total hip and knee arthroplasty. J Bone Joint Surg Am 2014;96:640–7. [DOI] [PubMed] [Google Scholar]
- [7].Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780–5. [DOI] [PubMed] [Google Scholar]
- [8].Stryker LS, Abdel MP, Morrey ME, et al. Elevated postoperative blood glucose and preoperative hemoglobin A1C are associated with increased wound complications following total joint arthroplasty. J Bone Joint Surg Am 2013;95:808–14. S801-S802. [DOI] [PubMed] [Google Scholar]
- [9].Marchant MH, Jr, Viens NA, Cook C, et al. The impact of glycemic control and diabetes mellitus on perioperative outcomes after total joint arthroplasty. J Bone Joint Surg Am 2009;91:1621–9. [DOI] [PubMed] [Google Scholar]
- [10].Adams AL, Paxton EW, Wang JQ, et al. Surgical outcomes of total knee replacement according to diabetes status and glycemic control, 2001 to 2009. J Bone Joint Surg Am 2013;95:481–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Iorio R, Williams KM, Marcantonio AJ, et al. Diabetes mellitus, hemoglobin A1C, and the incidence of total joint arthroplasty infection. J Arthroplasty 2012;27:726–9. e721. [DOI] [PubMed] [Google Scholar]
- [12].Mraovic B, Suh D, Jacovides C, et al. Perioperative hyperglycemia and postoperative infection after lower limb arthroplasty. J Diabetes Sci Technol 2011;5:412–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Maradit Kremers H, Lewallen LW, Mabry TM, et al. Diabetes mellitus, hyperglycemia, hemoglobin A1C and the risk of prosthetic joint infections in total hip and knee arthroplasty. J Arthroplasty 2015;30:439–43. [DOI] [PubMed] [Google Scholar]
- [14].Jamsen E, Nevalainen P, Kalliovalkama J, et al. Preoperative hyperglycemia predicts infected total knee replacement. Eur J Intern Med 2010;21:196–201. [DOI] [PubMed] [Google Scholar]
- [15].Jamsen E, Nevalainen P, Eskelinen A, et al. Obesity, diabetes, and preoperative hyperglycemia as predictors of periprosthetic joint infection: a single-center analysis of 7181 primary hip and knee replacements for osteoarthritis. J Bone Joint Surg Am 2012;94:e101. [DOI] [PubMed] [Google Scholar]
- [16].Chrastil J, Anderson MB, Stevens V, et al. Is hemoglobin A1C or perioperative hyperglycemia predictive of periprosthetic joint infection or death following primary total joint arthroplasty? J Arthroplasty 2015;30:1197–202. [DOI] [PubMed] [Google Scholar]
- [17].Reategui D, Sanchez-Etayo G, Nunez E, et al. Perioperative hyperglycaemia and incidence of post-operative complications in patients undergoing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2015;23:2026–31. [DOI] [PubMed] [Google Scholar]
- [18].Papagelopoulos PJ, Idusuyi OB, Wallrichs SL, et al. Long term outcome and survivorship analysis of primary total knee arthroplasty in patients with diabetes mellitus. Clin Orthop Relat Res 1996;124–32. [DOI] [PubMed] [Google Scholar]
- [19].England SP, Stern SH, Insall JN, et al. Total knee arthroplasty in diabetes mellitus. Clin Orthop Relat Res 1990;130–4. [PubMed] [Google Scholar]
- [20].Serna F, Mont MA, Krackow KA, et al. Total knee arthroplasty in diabetic patients. Comparison to a matched control group. J Arthroplasty 1994;9:375–9. [DOI] [PubMed] [Google Scholar]
- [21].Meding JB, Reddleman K, Keating ME, et al. Total knee replacement in patients with diabetes mellitus. Clin Orthop Relat Res 2003;208–16. [DOI] [PubMed] [Google Scholar]
- [22].American Diabetes Association. Standards of medical care in diabetes–2011. Diabetes Care 2011;34(Suppl 1):S11–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Umpierrez GE, Hellman R, Korytkowski MT, et al. Management of hyperglycemia in hospitalized patients in non-critical care setting: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2012;97:16–38. [DOI] [PubMed] [Google Scholar]


