Abstract
Background:
This meta-analysis aimed to systematically evaluate the effects of probiotics on blood lipid and blood pressure among patients with type 2 diabetes mellitus (T2DM) based on the randomized controlled studies.
Methods:
PubMed, Cochrane, Embase, Wanfang, China National Knowledge Infrastructure, and VIP database were searched by the index words to identify the qualified randomized control trial. The latest research was done in the January 2017. Mean difference (MD) along with 95% confidence interval (CI) was used to analyze the included outcomes.
Results:
Ten trials were included at last with 297 patients in the treatment group and 294 patients in the control group. Probiotics significantly decreased the value of total cholesterol (SMD −0.57, 95% CI −0.92 to 0.21), triglyceride (SMD −0.66, 95% CI −0.93 to 0.39), low-density lipoprotein (SMD −0.40, 95% CI −0.79 to 0.01), systolic blood pressure (WMD −5.04, 95% CI −8.8 to 1.20), diastolic blood pressure (SMD −0.39, 95% CI −0.62 to 0.17), fasting blood glucose (FBG) (SMD 3.54, 95% CI 1.94–5.15) compared with the placebo treatment. Apart from this, probiotics could significantly improve the value of high-density lipoprotein (SMD 0.38, 95% CI 0.03–0.73).
Conclusion:
Probiotics may decrease the indexes of lipid profile, blood pressure, and FBG in patients with T2DM; application of probiotics might be a new method for lipid profiles and blood pressure management in T2DM.
Keywords: blood lipid, blood pressure, meta-analysis, probiotics, type 2 diabetes
1. Introduction
Type 2 diabetes mellitus (T2DM) is 1 of the most common chronic metabolic diseases, which has become the third largest disease after cancer and cardiopathy. The incidence of this disease has considerably increased in worldwide recent years, so it is the main public social problem in the 21st century.[1,2] Previous studies found that about 592 million people will suffer from diabetes by the year 2035 worldwide.[3] In China, 1 of 2 adults may suffer from diabetes.[4] The incentive factors of T2DM are obesity, lack of actives, gene mutation, and so on. Researches show that chronic inflammative reaction is related to the pathogenesis of insulin resistance, the interaction of intestinal flora alteration, heredity, and environment-caused T2DM. Intestinal flora are important environmental factors for the development of T2DM, insulin resistance is the central nodes in metabolic syndrome, and high lipid environment is the important risk factor of insulin resistance. T2DM could lead to multiple severe complications, such as cardiovascular disease, diabetic retinopathy, neuropathy, and nephropathy, so T2DM is exerting heavy burden on global health and becoming 1 of the main causes of death around the world.[5,6]
Recently, probiotics have attracted increased attentions for its effects. Probiotics are well studied for their health benefits, and strengthen the immune system, improve blood lipid metabolism, and reduce oxidative stress and other functions of pharmacological nutrients. It has been demonstrated that probiotics can ameliorate the state of insulin resistance and regulate lipid metabolism in in vitro studies or animal models. However, various kinds of probiotics were used in the human clinical studies and concluded different results; some studies found no obvious effects, whereas others have identified a significant improvement on immune system function and preventing diarrhea. Apart from this, more and more studies showed that probiotics could particularly change the intestinal micro-ecosystem and play a positive role in T2DM treatment.[7–9]
Therefore, we included all the qualified randomized controlled trials (RCTs) to evaluate the effect of probiotics on lipid profiles and blood pressure in T2DM.
2. Materials and methods
2.1. Ethics approval
Ethics approval is waived because the present study does not involve any human participants.
2.2. Search strategy
The Cochrane, Pubmed, Embase, China National Knowledge Infrastructure (CNKI), Wang Fang and Weipu (VIP) were searched for all the relative trials about the efficacy of probiotics in the treatment of patients with T2DM. Others related articles and reference materials were also searched. The latest research was performed on January 2017. Two investigators doing the literature searched independently, and a third investigator was involved when an agreement occurred.
2.3. Inclusion and exclusion criteria
A study was included if it was: RCT; the research objects are patients with T2DM and do not have other serious diseases; the invention of treatment group is yogurt, bread, or others that contain probiotics, the invention of control group is placebo; the outcomes including blood lipid indexes or blood pressure indexes.
A study was excluded if it was: repeat published articles, or the content and result are same; data have obvious mistake; case report, theoretical research, conference report, systematic review, meta-analysis, expert comment; has no the data of outcomes indexes; the studies are animal experiments, chemical research, and other confounding factors.
All the studies were screened by 2 reviewers independently to determine whether the inclusion and exclusion criteria were satisfied, and discrepancies were resolved by a third reviewer.
2.4. Data extraction and quality assessment
The data were extracted from all the included studies and consisted of 2 parts: the basic information and main outcomes. The first parts were about the basic information: the author name, the interventions of treatment group and control group, the sample size, the main age, and the relative information of Jadad. The clinical outcome indexes were: systolic blood pressure (SBP), diastolic blood pressure (DBP), total cholesterol (TC), triglyceride (TG), low-density lipoprotein (LDL), and high-density lipoprotein (HDL). The Jadad scoring checklist was used to appraise the quality of involved studies. We evaluated all the RCTs from the 5 items: statement of randomization; appropriateness of generating randomized sequence; use of double blind; description of double blinding method; detail of withdrawals and dropouts. Studies with a score of less than 3 represented a low-quality and high bias risk; studies which got a score exceeding 3 were indicated as high-quality trails. All the above processes were done by 2 reviewers independently; disagreements between reviewers were resolved by discussion until a consensus was reached.
2.5. Statistical analysis
All statistical analyses were performed in the STATA 10.0 (TX). Chi-square and I2 tests were used to test the heterogeneity of clinical trial results and decided the analysis model (fixed-effect model or random-effect model). When the P value of the chi-square test was ≤.05 and I2 test value was >50%, it was defined as acceptable heterogeneity and assessed by random-effects model. When the P value of the chi-square test was >.05 and I2 test value was ≤50%, it was defined as homogeneous data and assessed by fixed-effects model. The continuous variables are expressed as the mean ± standard deviation (SD) and analyzed by mean difference (MD). The categorical data are presented as percentages and analyzed by relative risk (RR). SBP, DSP, TC, TG, LDL, and HDL were all continuous variables and were analyzed by MD and 95% confidence interval (CI).
3. Results
3.1. Characteristics and quality of included studies
The literature search collected 381 articles at first review, and 297 articles were excluded after screening the titles and abstracts. In the second review, 74 studies were removed for no RCT (8), repeat public (6), theoretical research (15), no clinical outcomes (29), other mix inventions (11), and objects with others diseases (5). The flowchart of article selection is shown in Fig. 1.
Figure 1.
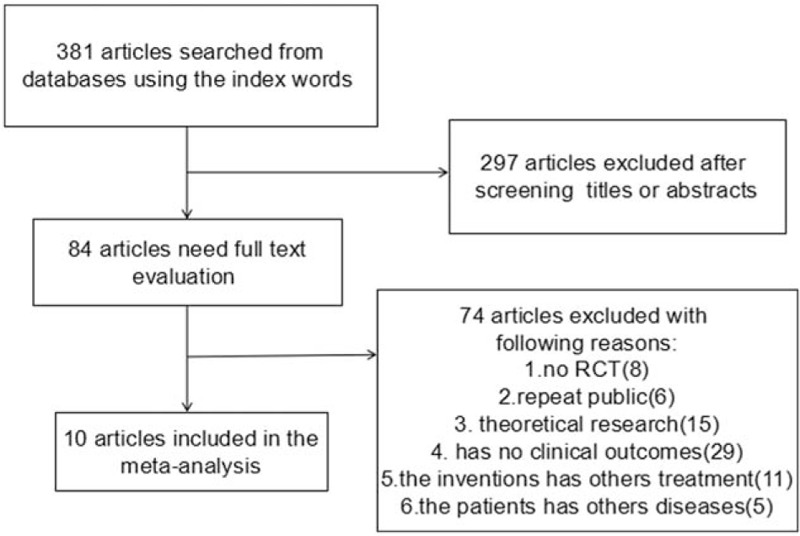
Flow diagram of the literature search and selection process.
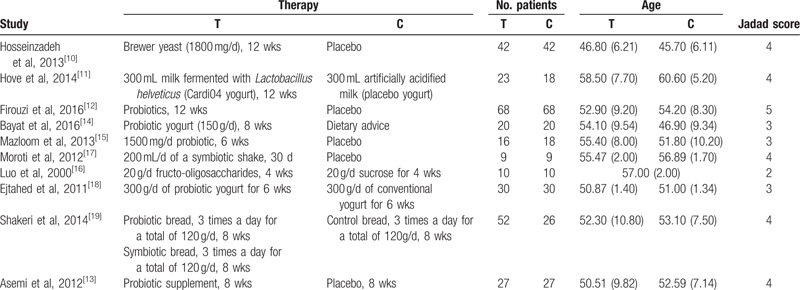
Finally, 10 studies[10–19] were included in the meta-analysis, with 297 patients in the treatment group and 268 patients in the control group. The specific information contains intervention, dosages and duration of treatment, sample size, age, and Jadad core. The characteristics of included studies are present in Table 1. The duration of intervention ranged from 4 to 12 weeks. Probiotic species and dose varied between studies. Four studies reported the change of SBP and DBP. Nine studies provided the data of TC; 10 studies provided the outcome of TG; and 11 studies reported the change of LDL and HDL. The main Jadad score of the included studies was 3.6; the Jadad score of 4 studies was under 4, which represents a low quality, and the Jadad score of the remaining 6 studies was above 4.
Table 1.
The basic characteristic description of the 39 included studies.
3.2. Lipid profiles
Nine studies, with 537 participants, reported the effect of probiotics on TC. Based on the chi-square test P value of .00 < .05 and I2 test value 73.6% > 50%, we chose random-effect model to analyze the value of TC. The results showed that probiotics would significantly decrease the value of TC when compared with the placebo (SMD −0.57, 95% CI −0.92 to 0.21). The forest plot of this effect is present in Fig. 2. Ten studies, with 571 participants, reported the effect of probiotics on TG. Based on the chi-square test P value of .014 < .05 and I2 test value 56.6% > 50%, we chose random-effect model to analyze the value of TG. The results showed that compared with the placebo, probiotics would significantly decrease the value of TG (SMD −0.66, 95% CI −0.93 to 0.39). The forest plot of this effect is present in Fig. 3. All included studies, with 591 participants, reported the effect of probiotics on LDL. Based on the chi-square test P value .00 < .05 and I2 test value 79.5% > 50%, we chose random-effect model to analyze the value of LDL. The results showed that there has significant difference between the 2 groups (SMD −0.40, 95% CI −0.79 to 0.01). The forest plot of this effect is present in Fig. 4. All included studies, with 591 participants, reported the effect of probiotics on HDL. On the basis of the chi-square test P value .00 < .05 and I2 test value 76.1% > 50%, we chose random-effect model to analyze the value of HDL. The results showed that probiotics could significantly improve the value of HDL (SMD 0.38, 95% CI 0.03–0.73). The forest plot of this effect is present in Fig. 5.
Figure 2.
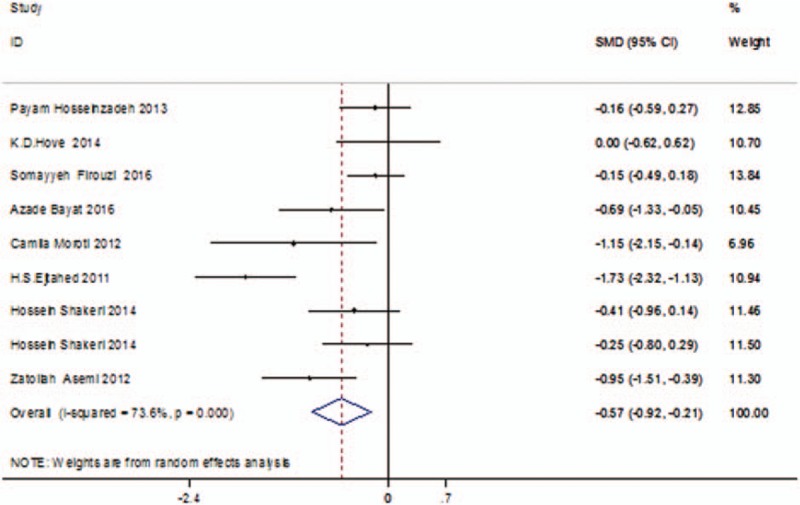
The forest figure of TC that compares between probiotics and placebo. TC = total cholesterol.
Figure 3.
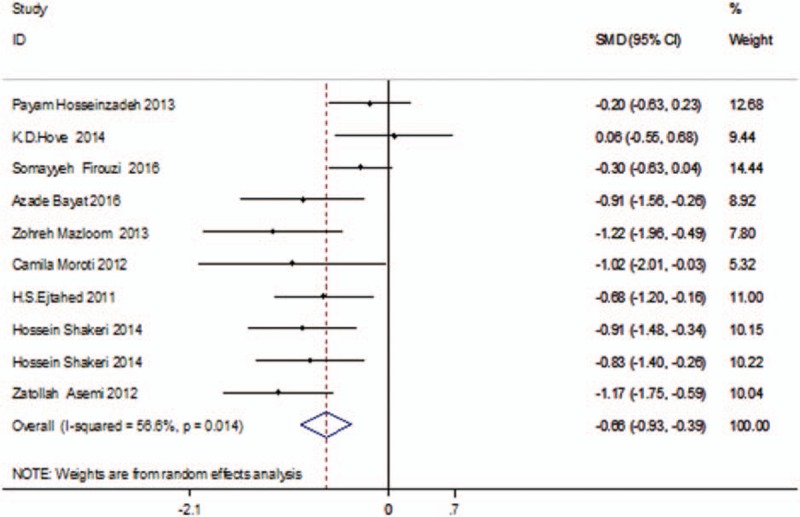
The forest figure of TG that compares between probiotics and placebo. TG = triglyceride.
Figure 4.
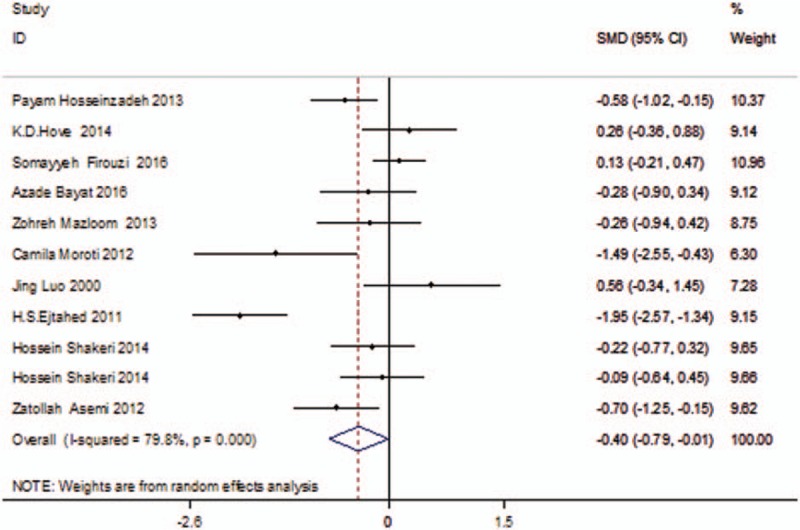
The forest figure of LDL that compares between probiotics and placebo. LDL = low-density lipoprotein.
Figure 5.
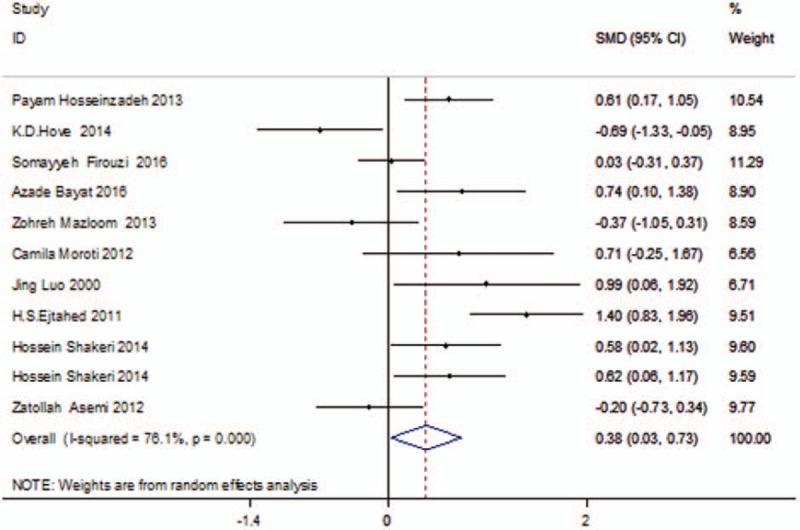
The forest figure of HDL that compares between probiotics and placebo. HDL = high-density lipoprotein.
3.3. Blood pressure
Four studies, with 301 participants, reported the effect of probiotics on SBP. On the basis of the chi-square test P value .955 > .05 and I2 test value 0.0% < 50%, we chose fixed-effect model to analyze the value of SBP. The results showed that there was statistical difference between the 2 groups on the value of SBP (WMD −5.04, 95% CI −8.8 to 1.20). The forest plot of this effect is present in Fig. 6. Four studies, with 301 participants, reported the effect of probiotics on DBP. Based on the chi-square test P value .493 > .05 and I2 test value 0.00% < 50%, we chose fixed-effect model to analyze the value of DBP. The results showed that probiotics could significantly improve the value of DBP (SMD −0.39, 95% CI −0.62 to 0.17). The forest plot of this effect is present in Fig. 7.
Figure 6.
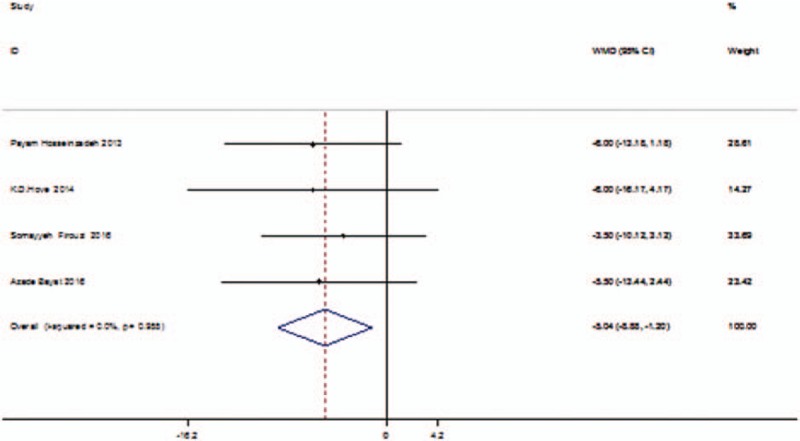
The forest figure of SBP that compares between probiotics and placebo. SBP = systolic blood pressure.
Figure 7.
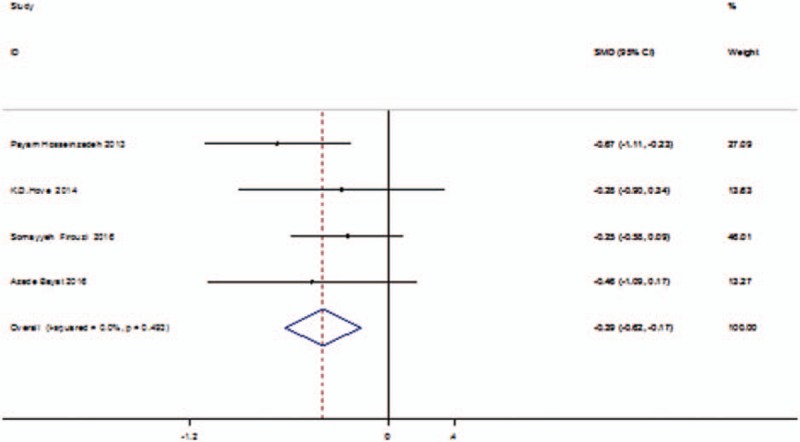
The forest figure of DBP that comparison between probiotic and placebo. DBP = diastolic blood pressure.
3.4. Fasting blood glucose
Eight studies, with 429 participants, reported the effect of probiotics on fasting blood glucose (FBG). On the basis of the chi-square test P value .000 < .05 and I2 test value 96.9% > 50%, we chose random-effect model to analyze the value of FBG. The results showed that FBG was significantly increased in the control group than the probiotics group (SMD 3.54, 95% CI 1.94–5.15). The forest plot of this effect is present in Fig. 8.
Figure 8.
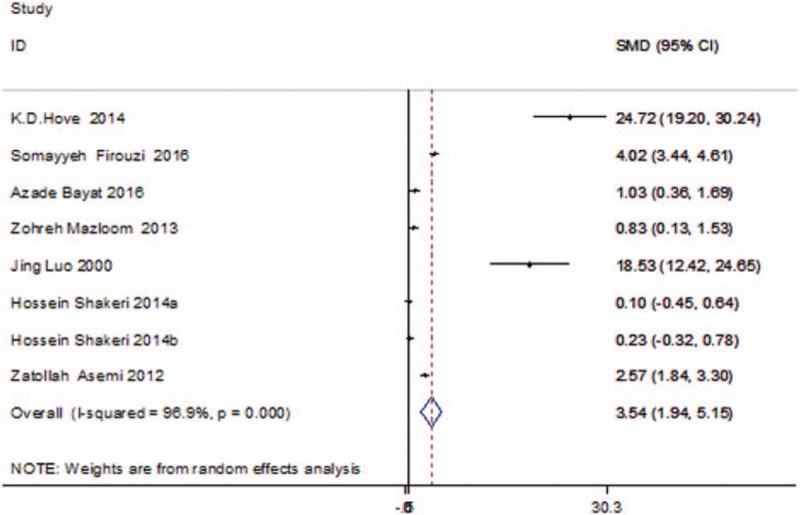
The forest figure of FBG that compares between probiotics and placebo. FBG = fasting blood glucose.
3.5. Quality assessment and potential bias
On the basis of the included and excluded criteria, 10 articles were included in the meta-analysis. The quality assessment and potential bias were accessed by funnel plot, Begg and Mazumdar rank test, and Egger test. The funnel plot for log OR in LDL of included studies was notably symmetrical, suggesting no publication bias (Fig. 9). Also, significant symmetrical was detected by Begg and Mazumdar rank test (Z = 0.62, P = .533). However, the Egger test result shown there has no significant publication bias (P = .373).
Figure 9.
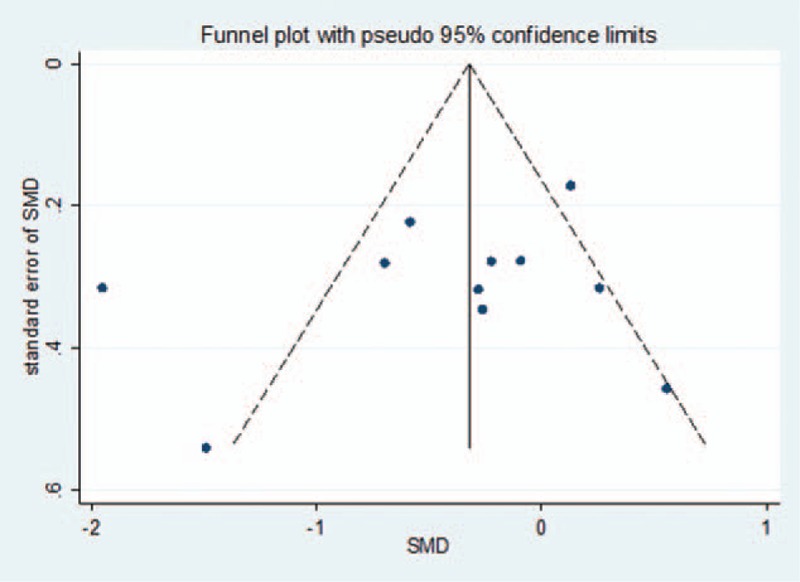
Funnel plot of studies included in the meta-analysis.
4. Discussion
Type 2 diabetes mellitus is the most common metabolic disorder chronic disease across the world. The main symptoms of T2DM are hyperglycemia, insulin resistance and blood lipid, and intestinal microflora imbalance, which can even lead to multiple organ failure such as cardiac arrest, diabetic retinopathy, and so on. The serious influence of T2DM is not only severe pain but also a heavy economic burden which affects everyday life. Recently, clinical studies reported that probiotics could significantly control the indexes of lipid profiles and blood pressure.
Recently, similar meta-analyses have been published about the effect of probiotics on glucose control, lipid profiles, blood pressure, and insulin action. Li et al[20] found that probiotics could alleviate FBG (SMD −0.61 mmol/L) and increase HDL-C (SMD 0.42 nmol/L), but have no significant differences on LDL-C, TC, TG, HbA1c, and HOMA-IR. Zhang et al[21] reported that probiotics could significantly decrease FPG (MD −15.92 mg/dL), HbA1c (MD −0.54%), HOMA-IR (MD −1.08), and insulin concentration (MD −1.35 mlU/L). Hua[22] suggested that compared with control group, probiotics had significant influence on FBG (MD −25.67), TG (−34.74), and GRP (−6.6).
In our meta-analysis, compared with placebo, probiotics could significantly reduce the value of TC (SMD −0.57 mg/dL; Fig. 2), and this is consistent with Hua's results about TC; probiotics also significantly increased the value of HDL (SMD 0.38 mg/dL; Fig. 5), and this conclusion is consisted with Li et al's result about the HDL. The TG level (SMD −0.66; Fig. 3) and LDL level (SMD −0.40; Fig. 4) were all significantly decreased in the probiotics group than in the placebo group. The elevated level of HDL is a protective factor for cardiovascular disease. The levels of TC, TG, and LDL are represented the situation of lipid profiles. Generally, the decrease of TC, TG, and LDL is beneficial for T2DM. The beneficial influence of probiotics on lipid profiles might be due to the inhibition of dietary cholesterol absorption and the suppression of bile acid reabsorption in the small intestine. Apart from this, we also found that the levels of SBP (WMD −5.04 mm Hg; Fig. 6) and DBP (SMD −0.39 mm Hg; Fig. 7) were significantly decreased in the probiotic group compared with that in the placebo group. Due to the insulin resistance, most T2DM patients had high blood pressure along with hyperlipemia. The incidence of T2DM and high blood pressure would lead to stroke or myocardial infarction, and make serious adverse effects on patients’ quality of life. So, control of blood pressure in T2DM is meaningful.
Some advantages of the present meta-analysis were as follows: only RCTs with high-quality score were considered for evaluation; this systemic review findings might be more convincing than any individual study among all included RCTs because that the effect of O3FA supplementation in patients with ESRD was quantitatively determined using pooled large sample size; and this meta-analysis provided evidence for the effects of O3FA supplementation on serum lipids and vascular inflammation markers such as TG, TC, LDL, HDL, CRP, albumin, hemoglobin, homocysteine, SBP, DBP, glucose, lipoprotein(a), and ferritin.
However, there are some limitations which should be brought to attention in this analysis. The limitations are as follows: randomized case-control studies were included; differences in the inclusion criteria and exclusion criteria for patients; different patients with previous disease and treatments were unavailable; most trials with low quality and low Jadad score were included in our study; pooled date were used for analysis, and individual patients’ data were unavailable, so it limited us to make more comprehensive analysis.
5. Conclusions
In conclusion, this meta-analysis suggests that probiotics have beneficial effect on lipid profiles and blood pressure. However, there is still a need of conducting a multicenter, lager-scale, and long-time RCT to confirm the accurate effect of probiotics on T2DM.
Footnotes
Abbreviations: DBP = diastolic blood pressure, FBG = fasting blood glucose, HDL = high-density lipoprotein, LDL = low-density lipoprotein, MD = mean difference, RCT = randomized controlled trial, SBP = systolic blood pressure, T2DM = type 2 diabetes mellitus, TC = total cholesterol, TG = triglyceride.
The authors have no conflicts of interest to disclose.
References
- [1].Han JL, Lin HL. Intestinal microbiota and type 2 diabetes: from mechanism insights to therapeutic perspective. World J Gastroenterol 2014;20:17737–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Huang XD, Huang, Xuedong Study on intestinal flora of patients with type 2 diabetes. Hebei Med 2014;17:1041–3. [Google Scholar]
- [3].Guariguata L, Whiting DR, Hambleton I, et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 2014;103:137–49. [DOI] [PubMed] [Google Scholar]
- [4].Giacco F, Brownlee M. Oxidative stress and diabetic complications. Circ Res 2010;107:1058–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Lefebvre P, Pierson A. The global challenge of diabetes. World Hosp Health Serv 2004;40:37–40. 2. [PubMed] [Google Scholar]
- [6].Iebba V, Nicoletti M, Schippa S. Gut microbiota and the immune system: an intimate partnership in health and disease. Int J Immunopathol Pharmacol 2012;25:823–33. [DOI] [PubMed] [Google Scholar]
- [7].Ushkalova EA. [Role of probiotics in the prevention and treatment of diarrhea of various genesis: focus on linex]. Ter Arkh 2014;86:100–5. [PubMed] [Google Scholar]
- [8].FAO J. WHO Working Group Report on Drafting Guidelines for the Evaluation of Probiotics in Food London. Ontario:2014. [Google Scholar]
- [9].Panwar H, Rashmi HM, Batish VK, et al. Probiotics as potential biotherapeutics in the management of type 2 diabetes: prospects and perspectives. Diabetes Metab Res Rev 2013;29:103–12. [DOI] [PubMed] [Google Scholar]
- [10].Hosseinzadeh P, Djazayery A, Mostafavi SA, et al. Brewer's yeast improves blood pressure in type 2 diabetes mellitus. Iran J Public Health 2013;42:602–9. [PMC free article] [PubMed] [Google Scholar]
- [11].Hove KD, Brons C, Faerch K, et al. Effects of 12 weeks of treatment with fermented milk on blood pressure, glucose metabolism and markers of cardiovascular risk in patients with type 2 diabetes: a randomised double-blind placebo-controlled study. Eur J Endocrinol 2015;172:11–20. [DOI] [PubMed] [Google Scholar]
- [12].Firouzi S, Majid HA, Ismail A, et al. Effect of multi-strain probiotics (multi-strain microbial cell preparation) on glycemic control and other diabetes-related outcomes in people with type 2 diabetes: a randomized controlled trial. Eur J Nutr 2017;56:1535–50. [DOI] [PubMed] [Google Scholar]
- [13].Asemi Z, Zare Z, Shakeri H, et al. Effect of multispecies probiotic supplements on metabolic profiles, hs-CRP, and oxidative stress in patients with type 2 diabetes. Ann Nutr Metab 2013;63:1–9. [DOI] [PubMed] [Google Scholar]
- [14].Bayat A, Azizi-Soleiman F, Heidari-Beni M, et al. Effect of Cucurbita ficifolia and probiotic yogurt consumption on blood glucose, lipid profile, and inflammatory marker in type 2 diabetes. Int J Prev Med 2016;7:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Mazloom Z, Yousefinejad A, Dabbaghmanesh MH. Effect of probiotics on lipid profile, glycemic control, insulin action, oxidative stress, and inflammatory markers in patients with type 2 diabetes: a clinical trial. Iran J Med Sci 2013;38:38–43. [PMC free article] [PubMed] [Google Scholar]
- [16].Luo J, Rizkalla SW, Alamowitch C, et al. Chronic consumption of short-chain fructooligosaccharides by healthy subjects decreased basal hepatic glucose production but had no effect on insulin-stimulated glucose metabolism. Am J Clin Nutr 1996;63:939–45. [DOI] [PubMed] [Google Scholar]
- [17].Moroti C, Souza Magri LF, de Rezende Costa M, et al. Effect of the consumption of a new symbiotic shake on glycemia and cholesterol levels in elderly people with type 2 diabetes mellitus. Lipids Health Dis 2012;11:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Ejtahed HS, Mohtadi-Nia J, Homayouni-Rad A, et al. Effect of probiotic yogurt containing Lactobacillus acidophilus and Bifidobacterium lactis on lipid profile in individuals with type 2 diabetes mellitus. J Dairy Sci 2011;94:3288–94. [DOI] [PubMed] [Google Scholar]
- [19].Shakeri H, Hadaegh H, Abedi F, et al. Consumption of symbiotic bread decreases triacylglycerol and VLDL levels while increasing HDL levels in serum from patients with type-2 diabetes. Lipids 2014;49:695–701. [DOI] [PubMed] [Google Scholar]
- [20].Li C, Li X, Han H, et al. Effect of probiotics on metabolic profiles in type 2 diabetes mellitus: a meta-analysis of randomized, controlled trials. Medicine 2016;95:e4088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Zhang Q, Wu Y, Fei X. Effect of probiotics on glucose metabolism in patients with type 2 diabetes mellitus: a meta-analysis of randomized controlled trials. Medicina (Kaunas) 2016;52:28–34. [DOI] [PubMed] [Google Scholar]
- [22].Hua LM. Type 2 diabetes and probiotics, prebiotics and synbiotics: a meta-analysis. Chin J Microecol 2016;28:1257–68. [Google Scholar]


