Abstract
Rationale:
Gastrointestinal solitary extramedullary plasmacytoma (EMP) is rare, just occupies about 5% of all EMPs. The most common site is small intestine followed by stomach. The colorectal incidence is much rare.
Patient concerns:
A 63-year-old female had an episodic pain around the umbilicus for about one week. The hyperemia and edema in the ileocecal mucosa were found in colonoscopy, and the endoscopy could not cross the ileocecal valve. The pathology specimens showed a high index suspicion of plasmacytoma.
Diagnoses:
The patient was diagnosed with extramedullary plasmacytoma.
Interventions:
A right hemicolectomy surgery was performed to treat the disease.
Outcomes:
Post surgery pathologic report showed low grade malignant mucosa associated marginal zone B cell lymphoma.
Lessons:
We report a case of an extramedullary plasmacytoma in ileocecum with abdominal pain and a review of extramedullary plasmacytoma.
Keywords: extramedullary plasmacytoma, gastrointestinal, ileocecum
1. Introduction
Plasma cell neoplasms can be divided into four groups: multiple myeloma (MM), plasma cell leukemias, solitary bone plasmacytoma (SBP), and solitary extramedullary plasmacytoma (EMP).[1] Gastrointestinal solitary extramedullary plasmacytoma (EMP) is rare, just occupies about 5% of all EMPs. The most common site is small intestine followed by stomach. The colorectal incidence is much rare.
2. Case
A 63-year-old female was presented to our hospital with an episodic pain around the umbilicus for about 1 week. There were no nausea, vomit, haematemesis, melena, hematochezia, or the absence of anal venting of faeces or flatus. She had no history of multiple myeloma and other disease. The patient underwent gastric endoscopy and colonoscopy. She was found to have Helicobacter pylori (HP) positive in gastric endoscopy.
The hyperemiaandedemain theileocecalmucosa were found in colonoscopy, and the endoscope could not cross the ileocecal valve (Fig. 1). Biopsies were obtained from the ileocecal valve and the opening of appendix. The pathology specimens showed a high index suspicion of plasmacytoma (Fig. 2). Immunohistochemistry for the specimens manifested CD38(+), CD138(+), Ki 67 (about 15%), Lambda(±), Kappa(3+), Pan CK(−), Mum-1(+) (Fig. 3). The laboratory data indicated her WBC was 12.42×109/L, a positive vomit and stool occult blood, and normal amylase level. The serum immunofixation electrophoresis, urine immunoglobulins (κ,λ) light chains serum, β2 microglobulin, and bone marrow aspirate index were in normal level. Serum free light chains showed a high level of kappa light chains. The level of immunoglobulin IgM was 0.359 g/L (NR:0.4 −2.3 g/L). Lymphocyte subsets flow analysis showed a low level of CD3+, CD19+, CD45+ brightSS Clow, CD3+ CD8+, CD3+CD4+. CT scan showed a mass in ileocecal region (Fig. 4). Finally, the patient was diagnosed with extramedullary plasmacytoma (EMP) and a right hemicolectomy surgery was performed to treat the disease. Postsurgery pathologic report showed low grade malignant mucosa associated marginal zone B cell lymphoma with plasma cell differentiation and tumor cell metastatis to perienteric lymph nodes.
Figure 1.
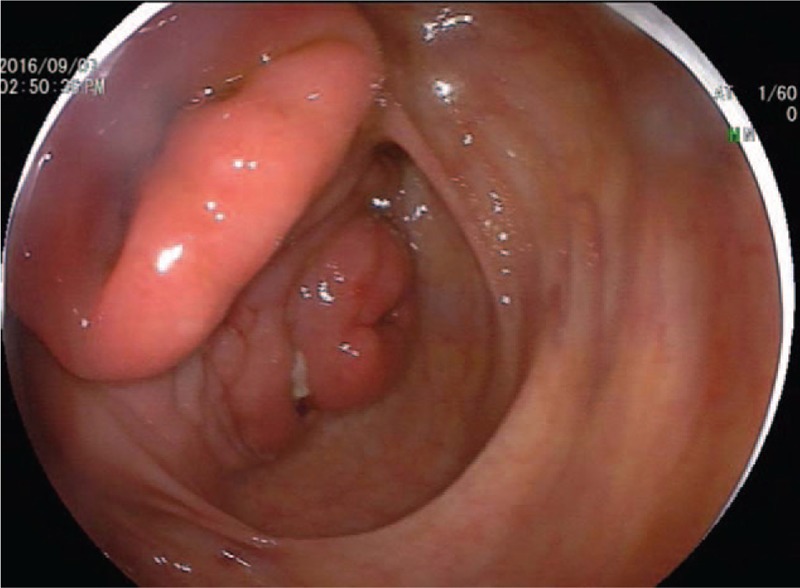
The colonoscopy showed hyperemiaandedemain theileocecalmucosa.
Figure 2.
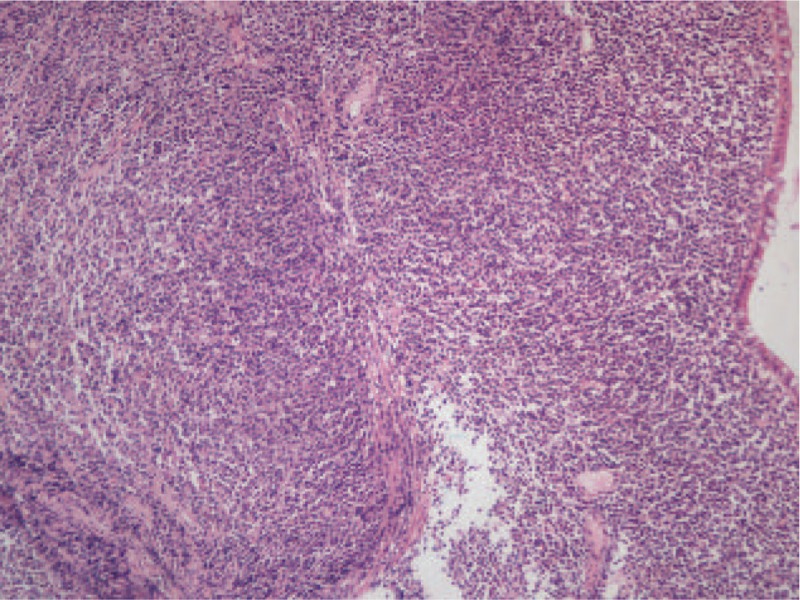
The pathology specimens showed a high index suspicion of plasmacytoma (HE, ×100).
Figure 3.
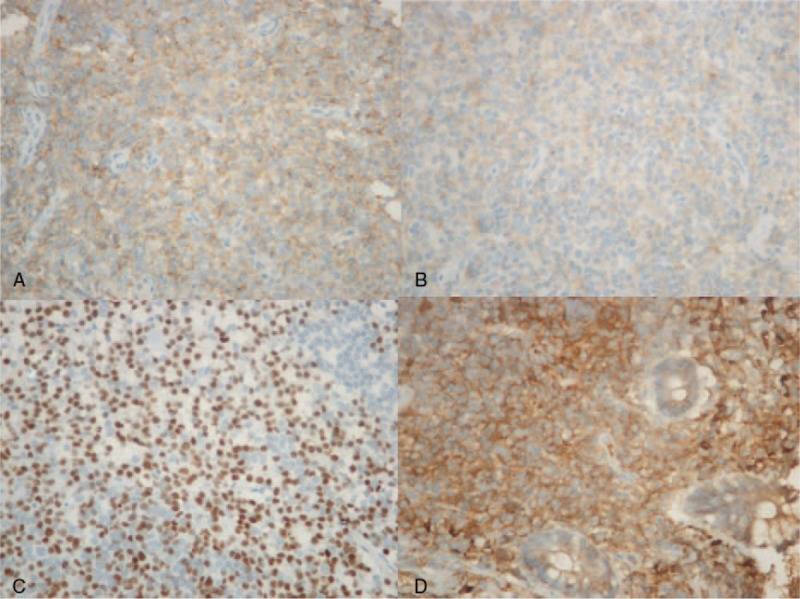
Immunohistochemistry for the specimens presented CD38(+), CD138(+), Ki 67 (about 15%), Lambda(±), Kappa(3+), Pan CK(−), Mum-1(+) (×400). A. CD138 (+), B. CD38 (+), C. Mum-1 (+), D. Kappa (3+).
Figure 4.
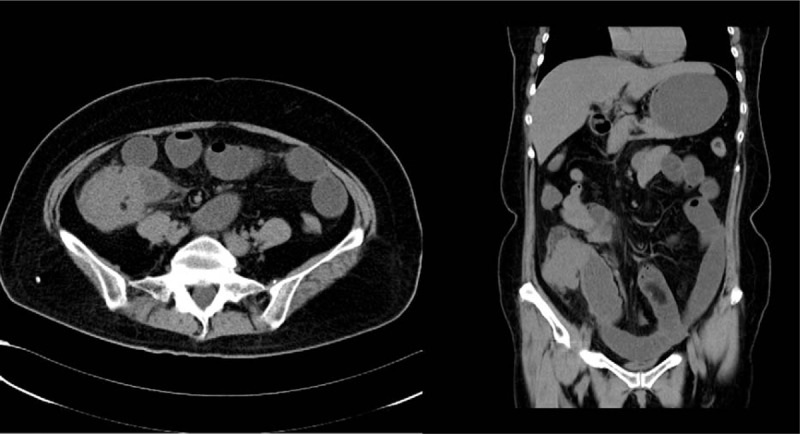
The CT scan showed a mass in ileocecal region.
3. Discussion
Extramedullary plasmocytomas come from soft tissue, which is solitary and have no evidence of multiple myeloma. The incidence of EMP is lower than SBP, accounts for only about 3% of all the plasma cell neoplasia.[2] However, the relationship of EMP and MM is not clear nowadays. About 1/3 of the EMP patients are diagnosed as multiple myeloma within two years after the symptoms.[3] Some studies showed EMP may occur in the early MM and the patient could be easily misdiagnosed in this phase. Extramedullary plasmacytoma regularly occurs in the areas that are full of plasmacyte cells such as in gastrointestinal tract, lymph nodes, spleen, urogenital region and so on.[4] Some articles reported extramedullary plasmacytoma could be divided into 3 stages. The first and second stage refer to the localized disease or extend to the lymph nodes nearby.[5,6] Therefore, the early stage of EMP could be hardly distinguished with other plasma cell neoplasms and it could extend to lymph nodes or adjacent tissue.
About 80% of EMPs occur in the head and neck region and only about 5% of all EMPs occur as gastrointestinal solitary EMP. The most common site is small intestine followed by stomach.[7,8] The incidence in colon is very rare,[9,10] especially in ileoceccal region is significantly low. Gabriel et al showed an extramedullaryileocecalplasmacytoma with a large ileocecal perforation.[11,12] In recent years, extramedullaryileocecalplasmacytoma in ileocaecal region has been reported very rarely. The EMP ratio of male to female is 4:1. And the disease is not common in children or adolescent.[13]
Symptoms of most EMP are not typical. Nasal obstruction, epistaxis, facial pain, or hoarse voice commonly occur in head and neck EMPs. Gastrointestinal EMPs could present as loss of appetite, bleeding, abdominal discomfort or obstruction. So we should take further examination to give a diagnosis of the EMP. There are some accessory examinations to help us diagnose EMP, such as fine-needle aspiration cytology, CT scan, MRI, or PET-CT. And pathology is most important when making a definite diagnosis. Fine-needle aspiration cytology (FNAC) cannot find the plasma cells so it is difficult to make distinction between inflammatory and tumor cells.[14] CT scan and PET-CT can help to find parenchymal lesions and the size and location of the lesion. PET-CT can find out the position of hypermetabolism which can indicate probability of malignancy. For the gastrointestinal lesion of EMP, endoscopy and biopsy are practical modes of diagnosis.
Some studies showed that H pylori may have relationship with infection in gastric EMP.[15,16] But in cases of gastric EMP that we reviewed, all had negative H pylori infection. Although standard treatment of EMP is absent, there are some methods like radiotherapy, chemotherapy and operation. Plasmacytomas are highly sensitive to radiotherapy, with the suggesting dose of 5000 cGy.[17] The United Kingdom Myeloma Forum (UKMF) recommended that in the head and neck EMP, radiation treatment is the better option while in the rest EMPs in other anatomic sites surgical operation should be considered first.[18] For gastrointestinal solitary EMP, endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) for the mucosal or submucosal tissue could be considered.[19] There is a report which showed that a high-dose dexamethasone (40 mg daily for 4 days every 3 weeks) treatment had an effect on ulcer type gastric EMP.[20]
EMP had better prognosis than MM and SBP.[21] As we have mentioned before, in the early MM, it may be misdiagnosed to EMP. So we should take a follow-up for the patients of EMP for a long time. In the aspect of prognosis, EMP may have an optimistic result of survival as the 5-year survival rate is about 82% [22] and 10-year disease-specific survival rate is higher than 50%.[23] Written informed consent was obtained before writing this report and the study protocol was approved by the Clinical Research Ethics Committee of Zhongda Hospital.
Footnotes
Abbreviations: EMP = extramedullary plasmacytoma, EMR = endoscopic mucosal resection, ESD = endoscopic submucosal dissection, HP = Helicobacter pylori, MM = multiple myeloma, SBP = solitary bone plasmacytoma, UKMF = United Kingdom Myeloma Forum.
Grant support: This work was supported by grants from National Natural Science Foundation of China (No. 81602432), Program for Jiangsu Provincial Natural Science Foundation of China (BK20140652).
The authors have no conflicts of interest to disclose.
References
- [1].Guler N. Extramedullary plasmacytoma: tumor occurrence and therapeutic concepts. Cancer 2000;88:240–2. [DOI] [PubMed] [Google Scholar]
- [2].Knowling MA, Harwood AR, Bergsagel DE. Comparison of extramedullary plasmacytomas with solitary and multiple plasma cell tumors of bone. J Clin Oncol 1983;1:255–62. [DOI] [PubMed] [Google Scholar]
- [3].Ahnach M, Marouan S, Rachid M, et al. Extramedullary plasmocytoma relapsing at different sites: an unusual presentation. Pan Afr Med J 2013;14:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Hayes DW, Bennett WA, Heck FJ. Extramedullary lesions in multiple myeloma. AMA Arch Pathol 1952;53:262–72. [PubMed] [Google Scholar]
- [5].Shahrizal TA, Prepageran N, Rahmat O, et al. Isolated extramedullary plasmacytoma of the middle turbinate. Ear Nose Throat J 2009;88:786–9. [PubMed] [Google Scholar]
- [6].Lao W, Chen L, Zhu H, et al. Solitary extramedullary plasmacytoma of anorectum. Int J Colorectal Dis 2007;22:1117–8. [DOI] [PubMed] [Google Scholar]
- [7].Du F, Jiang L, Zhu F, et al. Gastric adenocarcinoma concurrent with paravertebral plasmacytoma: a case report. Oncol Lett 2016;12:1551–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Gohil MH, Bhavsar DC, Suryanarayana U, et al. Plasmacytoma rectum extending to para-rectal region. J Cancer Res Ther 2015;11:662. [DOI] [PubMed] [Google Scholar]
- [9].Lewis K, Thomas R, Grace R, et al. Extramedullary plasmacytomas of the larynx and parapharyngeal space: imaging and pathologic features. Ear Nose Throat J 2007;86:567–9. [PubMed] [Google Scholar]
- [10].Mjoli M, Vorajee N, Naidoo Y, et al. Solitary extramedullary plasmacytoma of the colon, rectum and anus. S Afr J Surg 2016;54:45–7. [PubMed] [Google Scholar]
- [11].Lewin KJ, Ranchod M, Dorfman RF. Lymphomas of the gastrointestinal tract: a study of 117 cases presenting with gastrointestinal disease. Cancer 1978;42:693–707. [DOI] [PubMed] [Google Scholar]
- [12].Gabriel EM, Savu M. Discovery of a rare ileocecal plasmacytoma. J Surg Case Rep 2014;2014:pii: rju016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Bila J, Andjelic B, Bodrozic J, et al. Extramedullary plasmacytoma of the tongue base: a rare presentation of head and neck plasmacytoma. Vojnosanit Pregl 2013;70:972–5. [DOI] [PubMed] [Google Scholar]
- [14].Mitropoulou G, Zizi-Sermpetzoglou A, Moschouris H, et al. Solitary plasmacytoma of the mesentery: a systematic clinician's diagnosis. Case Rep Oncol Med 2017;2017:5901503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Lu HS, Xu YF, Gan MF. Primary gastric plasmacytoma associated with Helicobacter pylori infection: a report of two cases with different prognosis. Int J Hematol 2010;92:174–8. [DOI] [PubMed] [Google Scholar]
- [16].Stasi R, Evangelista ML, Brunetti M, et al. Primary gastric plasmacytoma and Helicobacter pylori infection. J Clin Oncol 2009;27:150–3. [DOI] [PubMed] [Google Scholar]
- [17].Liebross RH, Ha CS, Cox JD, et al. Clinical course of solitary extramedullary plasmacytoma. Radiother Oncol 1999;52:245–9. [DOI] [PubMed] [Google Scholar]
- [18].Han YJ, Park SJ, Park MI, et al. Solitary extramedullary plasmacytoma in the gastrointestinal tract: report of two cases and review of literature. Korean J Gastroenterol 2014;63:316–20. [DOI] [PubMed] [Google Scholar]
- [19].Zhou Y, Xu X, Xu L, et al. Treatment of primary isolated extramedullary plasmacytoma of esophagus with endoscopic submucosal dissection. Clin Gastroenterol Hepatol 2012;10:e21–2. [DOI] [PubMed] [Google Scholar]
- [20].Kang DY, Kim GB, Choi BS, et al. Successful treatment of a primary gastric plasmacytoma mimicking intractable gastric ulcer by using high-dose dexamethasone therapy: a case report. J Med Case Rep 2016;10:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kanavaros P, Stefanaki K, Vlachonikolis J, et al. Immunohistochemical expression of the p53, p21/Waf-1, Rb, p16 and Ki67 proteins in multiple myeloma. Anticancer Res 2000;20(6B):4619–25. [PubMed] [Google Scholar]
- [22].Webb CJ, Makura ZG, Jackson SR, et al. Primary extramedullary plasmacytoma of the tongue base. Case report and review of the literature. ORL J Otorhinolaryngol Relat Spec 2002;64:278–80. [DOI] [PubMed] [Google Scholar]
- [23].Straetmans J, Stokroos R. Extramedullary plasmacytomas in the head and neck region. Eur Arch Otorhinolaryngol 2008;265:1417–23. [DOI] [PubMed] [Google Scholar]


