Abstract
In this study, failure mode and effect analysis (FMEA), a proactive tool, was applied to reduce errors associated with the process which begins with assessment of patient and ends with treatment of complications. The aim of this study is to assess whether FMEA implementation will significantly reduce the incidence of catheter-related bloodstream infections (CRBSIs) in intensive care unit.
The FMEA team was constructed. A team of 15 medical staff from different departments were recruited and trained. Their main responsibility was to analyze and score all possible processes of central venous catheterization failures. Failure modes with risk priority number (RPN) ≥100 (top 10 RPN scores) were deemed as high-priority-risks, meaning that they needed immediate corrective action. After modifications were put, the resulting RPN was compared with the previous one. A centralized nursing care system was designed.
A total of 25 failure modes were identified. High-priority risks were “Unqualified medical device sterilization” (RPN, 337), “leukopenia, very low immunity” (RPN, 222), and “Poor hand hygiene Basic diseases” (RPN, 160). The corrective measures that we took allowed a decrease in the RPNs, especially for the high-priority risks. The maximum reduction was approximately 80%, as observed for the failure mode “Not creating the maximal barrier for patient.” The averaged incidence of CRBSIs was reduced from 5.19% to 1.45%, with 3 months of 0 infection rate.
The FMEA can effectively reduce incidence of CRBSIs, improve the security of central venous catheterization technology, decrease overall medical expenses, and improve nursing quality.
Keywords: catheter-related blood stream infection, failure mode and effective analysis, intervention studies
1. Introduction
Peripherally inserted central catheter (PICC) has been widely used in critical or surgical patients. However, PICC patients are at high risks of blood and concurrent infections. The prevalence of catheter-related blood stream infection (CRBSI) is increasing over the years,[1] which is described as the number of CRBSI cases per 1000 catheter days, as is recommended by USA Centers for Disease Control (CDC) and Joint Commission on Accreditation of Healthcare Organizations. CRBSI prevalence is calculated as follows: total catheter infection cases/d × 1000%. According to CDC reports, the average CRBSI rate of 5.3% is in America,[2] whereas it is 2.04% to 9.82% in the intensive care unit (ICU) of our hospital (the medical center of northwest Sichuan Province). Meanwhile, our infection rate was 19.0%, which is higher than that (14.0%) in a previous report.[3] In view of the high CRBSI rate in the ICU, it is necessary to strengthen the prevention and control strategies.
At present, great multidisciplinary efforts from practitioners and institutions are required for infection risk management. Of them, failure mode and effect analysis (FMEA) is a practical and effective tool for risk management originated in 1950. It is a systematic approach for preventing failure. The failure modes defined in FMEA are any undesirable outcomes, including production loss, injury, or accident. A “customer” is defined as someone or something receiving products or services.[4] FMEA, first employed in industry,[5] is recommended as a proactive risk evaluation technique, because the early development of healthcare system mainly concentrates on drug manufacturing.[6] Gruber et al[7] suggested that FMEA could improve patient safety and medical quality. Zupa et al[8] recommended that FMEA could be applied in any procedure that might affect patient safety. FMEA has been widely applied in defining and eliminating known or latent failures to improve quality management and security. However, it has only been used in medical institutions to promote high-quality medical treatment until recent years.[9] FMEA comprises 7 steps, namely, team establishment, analysis of current work process, latent failure and impact analysis, risk priority number (RPN) calculation and result assessment, corrective action implementation, countermeasure tracking, and outcome measurement.[10,11] This study aimed to reduce RPN score and CRBSI rate to <100% and 3%, respectively, in ICU of our hospital, referring to infection data of advanced national hospitals.
2. Methods
2.1. Study design and study population
This study protocol was approved by the Medical Ethics Committee of Mianyang Centre Hospital. All participants had signed the written informed consent for study participation. This study was conducted in Mianyang Centre Hospital in Sichuan of China, which covers 77,000 square meters, with 2113 sickbeds. About 1.8 million outpatients and 80,000 in-patients were accepted in our hospital annually. Patients undergoing PICC insertion strictly according to the American Intravenous Infusion Association guide were selected from the ICU of Mianyang Centre Hospital from August 2015 to September 2016. Basilic vein was selected as the puncture site using 4Fr single lumen of tube (BD). Longitudinal study ended when any of the following situations occurred: catheter removal in the presence of indication; 48 hours after patient transfer to other department; patient death; and patient discharge. Repeatedly hospitalized patients meeting the monitoring conditions could be re-enrolled as subjects. CRBSI was diagnosed according to CDC criteria promulgated in 2008,[12] which indicated at least 1 of the following signs or symptoms in patients 2 days after central venous catheter indwelling and within 2 days after extubation: a recognized pathogen cultured from 1 or more blood cultures and organism from blood, which was not related to infection at another site; at least 1 of the following signs or symptoms in patients: fever (>38°C), chills, or hypotension, which together with positive laboratory results, were not related to infection at another site. The common skin contaminant was cultured from 2 or more blood cultures drawn on separate occasions. Patients aged ≤1 year having at least 1 of the following signs or symptoms: fever (>38°C, rectal), hypothermia (<37°C, rectal), apnea, or bradycardia, which, together with positive laboratory results, were not related to infection at another site. The common skin contaminant was cultured from 2 or more blood cultures drawn on separate occasions.
Patients recruited from August 2015 to December 2015 were in control group. Firstly, the project scope was determined, and project management team was established based on CRBSI incidence in ICU. Secondly, the venous indwelling catheter care information collection table was formulated to check the prevention process of CRBSI, and to analyze the failure mode and effect. Thirdly, improvement and preventive measures were proposed based on the results, and preparation before implementation was completed. Patients recruited from January to September 2016 were in observation group. The rectification plan was fully implemented in January 2016. The improvement effects were evaluated monthly, and the results were checked and analyzed to adjust the rectification plan. The above processes were repeated until an acceptable score was obtained. Finally, difference in infection incidence between control group and observation group was analyzed.
2.2. Statistical analysis
Statistical analysis was performed using analysis of variance and chi-square test, with in-hospital CRBSI rate as the primary outcome. A difference of P < .01 was considered statistically significant.
2.3. Multidisciplinary team assembly
The multidisciplinary team was assembled aiming to improve the PICC nursing quality and reduce CRBSI infection rate. A working schedule was designed. Our FMEA team comprised 15 medical staff from CRBSI Nursing Department and ICU. It included ICU and infection control center, head nurses, and major nursing personnel from Venous Catheter Departments (including ICU, Oncology, General Surgery, Hematology, Pediatrics, and Hematology). Team members were familiar with nursing process of central venous catheter, experienced in infection control, highly aware and conscious of risk and quality management. All project team members were systemically trained on FMEA knowledge, theme, target, and evaluation standard to clearly understand FMEA purpose and approach.
2.4. Current work process analysis
To recognize all possible failures potentially occurring at each step, a concrete flow diagram was constructed by the team members. PICC diagnosis and treatment was divided into 3 steps: patient evaluation; venipuncture operation and catheter maintenance; and advanced complication management. Factors related to personnel, system, objects, and environment were analyzed according to the flow chart shown in Fig. 1 based on the work experience of team members, open consultation, and discussion to identify the effects of each failure mode on patient nursing. A total of 25 key failure modes were discovered eventually, followed by risk assessments.
Figure 1.
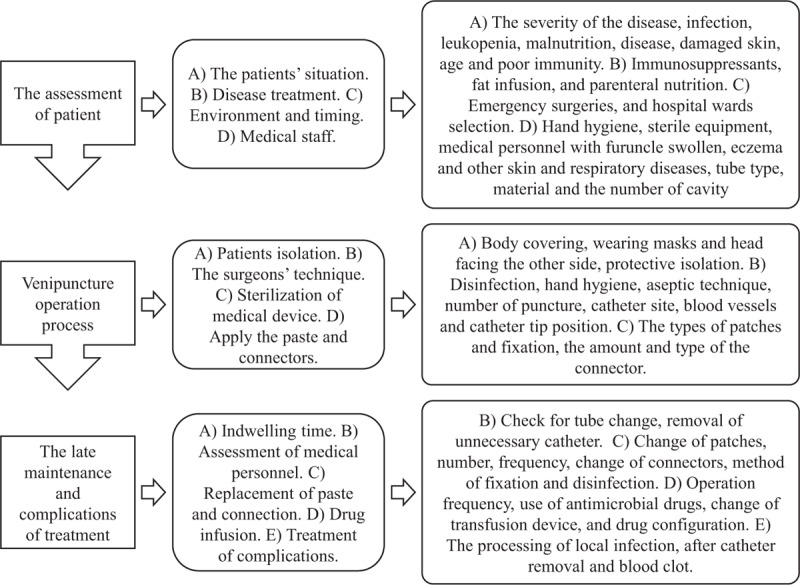
The flow chart of nursing process and key failure modes.
2.5. Latent failure and impact analysis
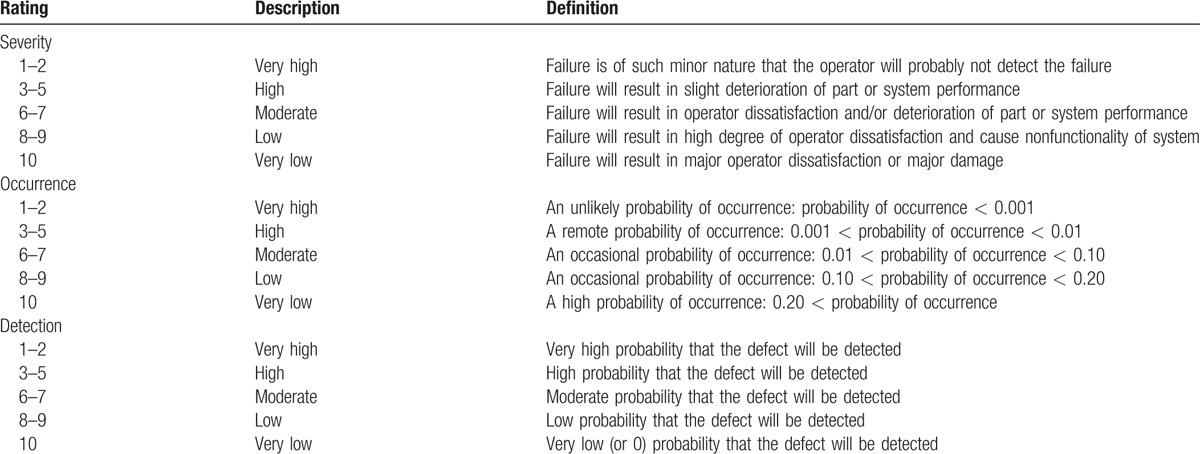
Contents of CRBSI failure mode questionnaire included subsystem function requirements; potential failure modes; consequences, cause, or mechanism of a failure; outcome severity (S); occurrence frequency (O); and likelihood of detection (D). FMEA was applied in determining measures of the highest priority by considering the associated severity (S), occurrence (O), and detection (D). Of them, S indicated the impact of an individual component or an operational procedure failure on a system, which was classified into 10 levels. Severity rating definitions and scoring criteria are shown in Table 1.[13] O represented the occurrence frequency of an individual component or an operating process failure, which was divided into 10 levels. Occurrence rating definitions and scoring criteria were shown in Table 1.[13] D demonstrated the possibility to detect a failure mode, which was classified into 10 levels. Detection rating definitions and scoring criteria were illustrated in Table 1.[13] In this study, FMEA approach and weights of S, O, and D were used for analysis.
Table 1.
Description of Severity, Occurrence and Detection Ratings Used During FMEA Workshop (Towler and Sinnott,[13] 2012).
2.6. RPN calculation and result assessment
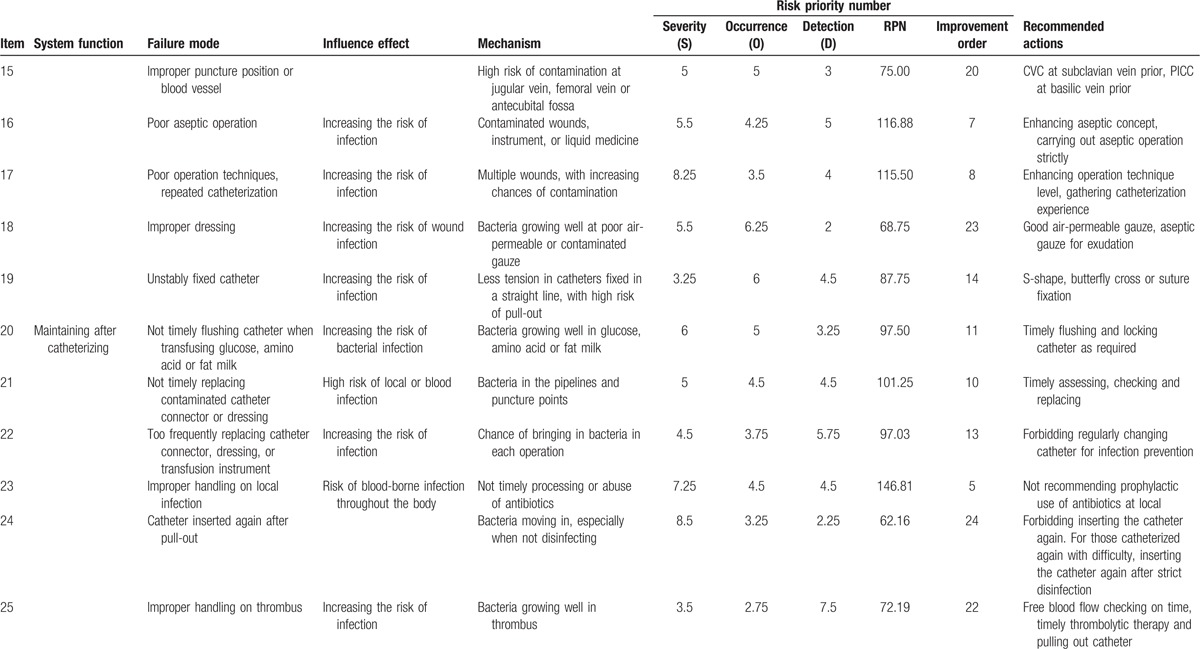
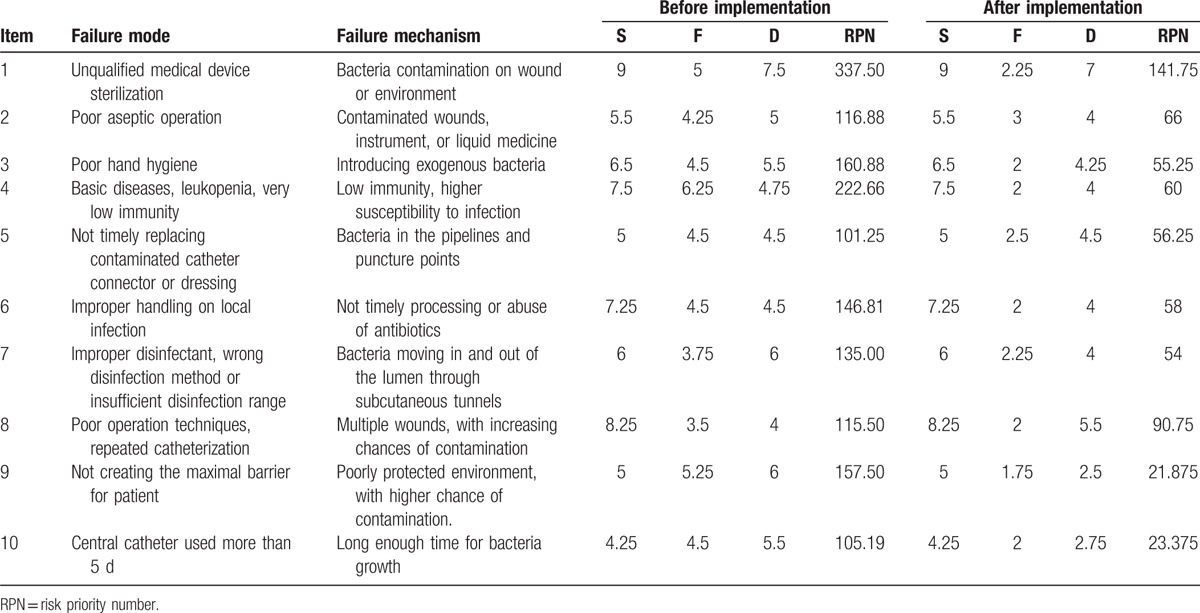
A numerical value was respectively assigned to S, O, and D of each failure mode based on previous adverse event records and personal experience in accordance with the CRBSI failure mode questionnaire. The scores were not changed after 3 rounds of Delphi method. RPN of each failure mode was calculated based on the formula: RPN = S × O × D.[14] The score ranged from 1 to 1000 (Table 2 ).
Table 2.
CRBSI important failure method and effects assessment.
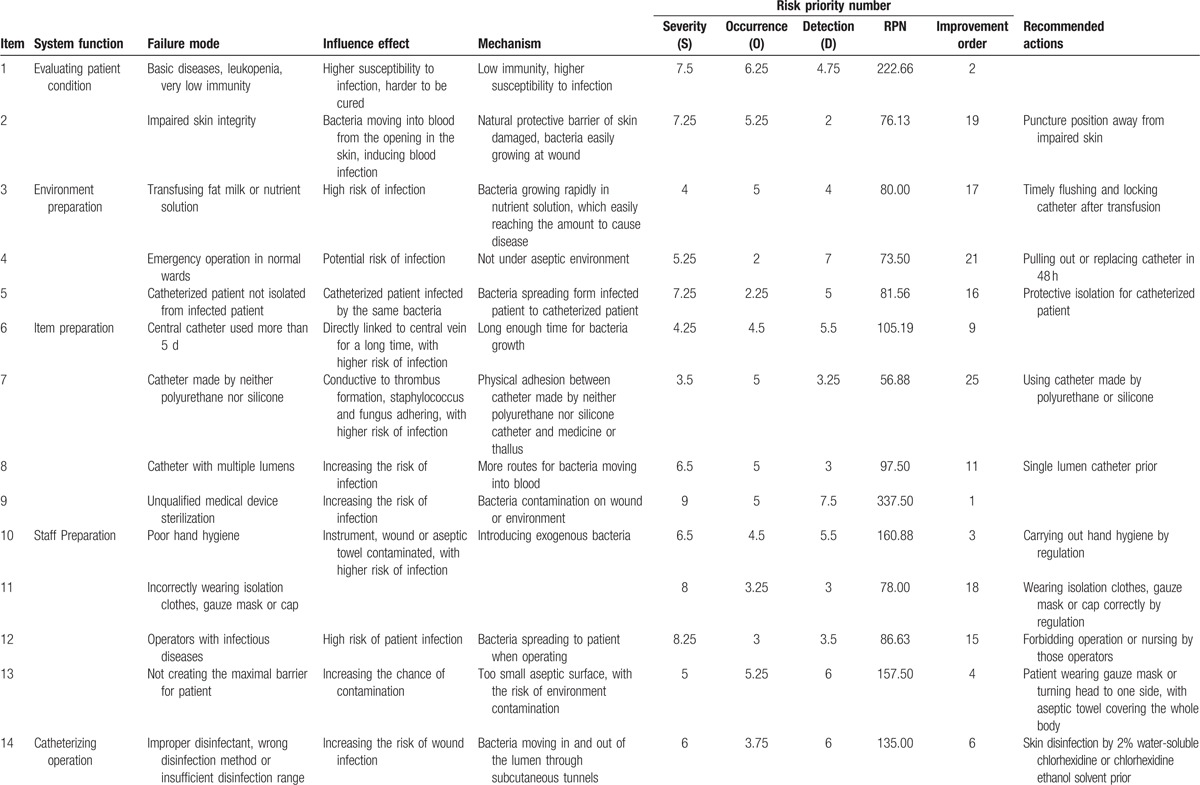
In the current study, the failure modes with RPN <100 had less effect on the entire process. Thus, no intervention was made for simplicity and workload reducing. Only issues with RPN ≥100 (top 10 RPN scores) were selected by our team (Table 3), which was commonly accepted as a threshold.[9,15] Scores of these 10 priority items accounted for 60% of the sum of all RPNs. They were classified as the top priority modes and the crucial factors in the final PICC diagnosis and treatment process. Recommended actions and controls for improvement were also shown in Table 3.
Table 2 (Continued).
CRBSI important failure method and effects assessment.
2.7. Corrective action implementation
Quality control for CRBSI incidence was established in the department. Specifically, a 3-level management model, namely, the head nurse—leaders—nurses, was employed to mobilize all nursing personnel, enhance the sense of responsibility, and improve the consciousness of risk prevention. Work performance was evaluated monthly, puncture method and skills were improved according to FMEA analysis results, and bundles of nursing care were performed. The department was equipped with sufficient disposable central venous puncture bags and drapes. Patients wore an ear-hanging surgical mask, with head facing the other end of the catheter. Disinfected bed sheet was used to cover nose and mouth in patients with a respirator who could not wear a mask. Medical equipment, appliances, and various wound dressings were checked before operation to ensure sterilization standards. Aseptic techniques were strictly operated and preventive strategies were implemented. The whole body of the patient was covered with sterile sheet, and the operation time of invasive treatments was shortened. Meanwhile, hand hygiene education was strengthened among the ICU medical staff. Signs to remind hand-washing were posted in prominent locations. Hand sanitizers were provided and hand-washing condition was improved. Hands of medical staff were regularly monitored for bacteria, and hand hygiene of nursing assistants, cleaners, and visiting personnel was supervised. Aseptic operation and sterile environment should be ensured.
Furthermore, special nursing care was provided for older patients or those subjected to severe diseases, malnutrition, immunosuppressive therapy, or long-term total parenteral nutrition. The pointers of catheters were strictly monitored, and the number and placement time of indwelling catheters was reduced as much as possible. Meanwhile, the catheters were removed immediately after patients were in stable condition and met the criteria for catheter removal. Infection symptoms during catheter indwelling were under close supervision. Predictable treatment and nursing care was provided, and skillful nurses were responsible for catheter puncture and maintenance. Close nurse–patient communication was strengthened, and patients signed the informed consent. Catheters were administered when patients were awake to guarantee effective communication, reduce patient nervousness, and improve the successful rate.
Skin and catheter connectors were disinfected with 0.5% chlorhexidine and alcohol rather than tincture of iodine during wound dressing change and catheterization. Notably, special channels were provided for patients undergoing blood transfusion and parenteral nutrition. Tube removal was considered in the case of local infection. Antimicrobial agents should not be applied into the punctured sites. All nursing staff were trained on the theoretical knowledge and clinical skills during specialized PICC technical training.
A checklist for patients was designed and nursing performance was verified to ensure the completeness of CRBSI nursing procedure, which was composed of the following items: choice of skin disinfectant, maximized sterile barrier in catheterization, hand hygiene, strict disinfection approaches, tube sealing and blunting, aseptic operation, choice of wound dressing and replacement, daily catheter assessment, and timely removal of unnecessary catheter. The checklist had covered all catheterization steps, which were checked by both the team leader and nurses. Meanwhile, the team leader was also responsible for supervision at night.
2.8. Countermeasure tracking
The study was carried out during a 14-month period from August 2015 to September 2016. Collection of baseline data such as catheter-related infections, FMEA, drawing up of bundles of nursing care plan, and preparatory work before measure implementation were completed from August to December 2015, so that all interventions could be fully implemented by January 2016. Nursing performance was evaluated monthly for implementation. Meanwhile, quality indicators of CRBSI were analyzed and shown in Table 4. The implementation rate of each category was evidently improved after intervention. In addition, the questionnaire was accomplished once every 3 months to assess the improvement after applying the FMEA approach. The RPN scores after improvement were recalculated in Table 3, which showed the effectiveness of the proposed measure.
Table 3.
Failure mode of top 10 RPN scores before and after implementation.
3. Results
3.1. RPN score recalculation
Table 3 displayed the results obtained after applying FMEA in managing CRBSI. A total of 25 failure modes were identified, along with the cause, effect, and score index of each item. Additionally, RPNs before and after the second round of FMEA were compared to clearly illustrate any changes. The numerical values in Table 3 indicated no change in severity. In other words, the experts suggested that severity would not change because of certain measures or methods. As to the occurrence and detection after modification, the experts’ grades had apparently changed. As could be observed from the items in Table 3, probability had reduced from the highest score by half. Hence, the experts suggested that the improvement measures could effectively lower the probability of violation.
3.2. Nursing measure implementation to prevent CRBSI
The checklist was evaluated by full-time quality control nurses monthly to evaluate the implementation of core nursing measures, and to analyze the improvement of quality indicators of CRBSI. The evaluation results were publically disclosed, which demonstrated that the nursing measures to prevent CRBSI had been implemented at a rate higher than before (Table 4).
3.3. Comparison of CRBSI infection rate
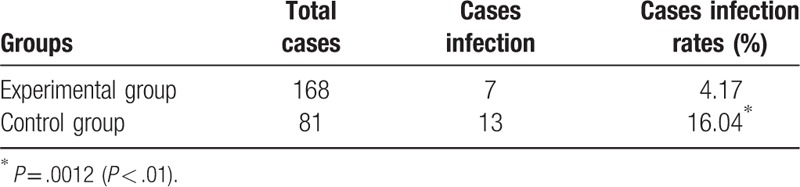
In all, 81 patients (60 males and 21 females) in control group were recruited from August to December 2015, with an average age of 59.1 years. In the meantime, the average time of catheter indwelling in control group was 20.02 days. Altogether, 168 patients (119 males and 49 females) in FMEA group were enrolled from January to September 2016, with an average age of 60.2 years. The average time of catheter indwelling in FMEA patients (or experimental group) was 21.53 days. No statistically significant differences were observed in CRBSI diagnostic standard or general physical conditions between the 2 groups. The infection rate in control group ranged from 4.3% to 7.41% (with an average of 5.19%), compared with 0% to 4.11% in FMEA group (with an average of 1.42%). Importantly, 0% infection rate was achieved in February, April, and September of 2016 (Table 5, Fig. 2). Moreover, the infection rate in FMEA group was outstandingly lower than that in control group (P < .01) (Table 6).
Table 4.
Nursing approaches to prevent CRBSI.
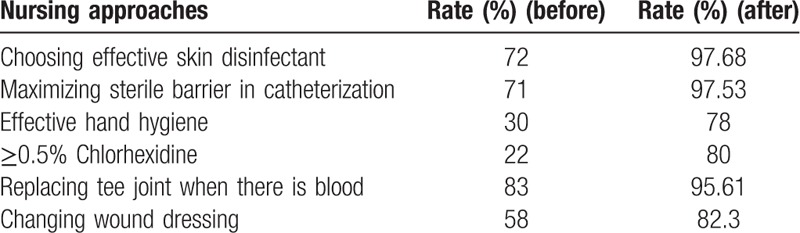
Figure 2.
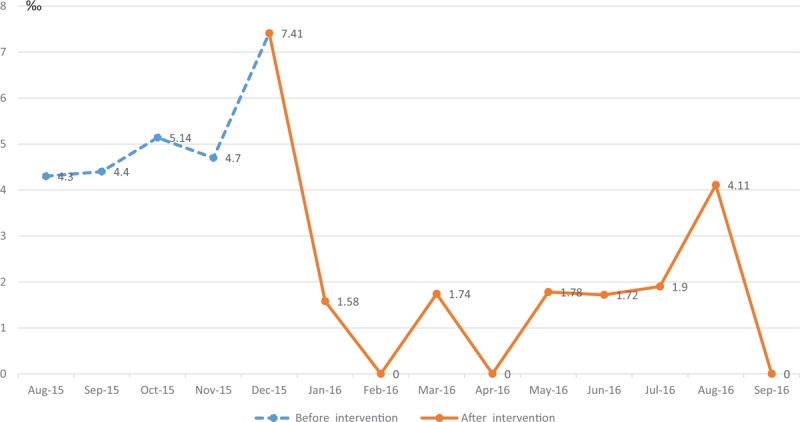
The changing trend graph of infection rate.
Table 5.
Rate of infection in 2 groups.
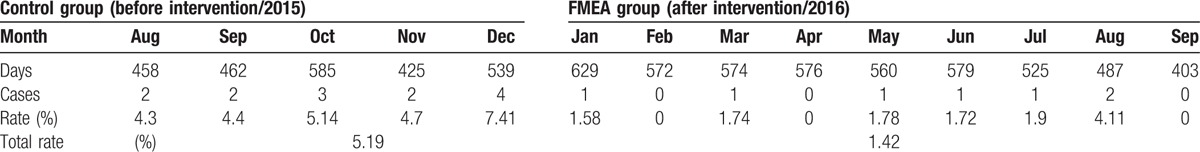
Table 6.
Comparison of infection rates between the 2 groups.
4. Discussion
Catheter-related bloodstream infection is related to numerous problems, such as extended hospital stay, higher medical cost, poorer prognosis, and even life-threatening conditions. Previous study indicates that CRBSI can be prevented.[16] There are diverse risk factors of CRBSI in ICU, which should be controlled by a proper management system. Moreover, the major problems in medical staff are lack of knowledge, awareness of the potential risk factors of infection, basic approaches to prevent CRBSI, and execution and sense of responsibility, which can be improved through training and supervision. Previous studies show that educational training programs can remarkably reduce the CRBSI rate.[17] In our study, systematic training on PICC health nurses with advanced theories, techniques, and strengthened supervision has notably lowered the CRBSI rate. Additionally, systemic problem is a step that is most likely to be overlooked by managers. Managers tend to focus on the liability of an individual's errors instead of the fundamental inspection system when problem occurs. This may conceal the underlying reasons and delay systematic improvement, which may also affect the diagnosis and treatment for patients.
Failure mode and effect analysis is an advanced management concept and strategy recommended by the Joint Commission International, which provides a complete set of working procedures and analysis methods. FMEA is more systematic and forward-looking compared with the other risk management methods, which can prevent failures. This study aims to expand the application of FMEA technique in the project management, so as to determine the possible project quality failure methods in advance.
Few studies have applied FMEA in CRBSI. In our study, all FMEA team members deriving from the functional departments of CRBSI prevention have worked together. The efforts from the whole team are pooled, the diagnosis and nursing process is analyzed in detail, which can avoid the weaknesses in project management and fully clarify the key points in securing catheter indwelling. The most important problems are often overlooked in clinical practice. Notably, the top 10 problems screened by RPN scores are prioritized to optimize effective nursing. CRBSI incidence is used as an indicator of quality management in ICU, and checklist for clinical follow-up is formulated to ensure its implementation, inspection, analysis, and improvement. Our results show that CRBSI incidence is markedly reduced, with 0% infection rate being achieved in February, April, and September of 2016.
Nonetheless, our study is inevitably associated with certain limitations. Firstly, it is limited to 1 ICU with small sample size. Secondly, the follow-up period is not long enough. Therefore, further study on noncritical patients with a large sample size may be needed in the future, so as to confirm the long-term effects of FMEA on preventing CRBSI.
5. Conclusions
In summary, our study confirms that the FMEA technique can achieve the total quality management of venous catheter in terms of overall interests, prospective analysis, and overall performance. It can dominantly quantify recessive risks to standardize risk management, which can finally effectively prevent and control CRBSI in ICU, thus facilitating the continuous improvement of nursing quality.
Acknowledgment
Thanks to the intensive care unit of Mianyang Central Hospital to provide clinical data.
Footnotes
Abbreviations: CDC = Centers for Disease Control, CRBSIs = catheter-related bloodstream infections, FMEA = failure mode and effect analysis, ICU = intensive care unit, PICC = peripherally inserted central catheter, RPN = risk priority number.
The authors report no conflicts of interest.
References
- [1].Rosenthal VD, Maki DG, Jamulitrat S, et al. International Nosocomial Infection Control Consortium (INICC) report, data summary for 2003–2008, issued June 2009. Am J Infect Control 2010;38:95–104. [DOI] [PubMed] [Google Scholar]
- [2].Diana T. Central venous access device infections in the Critical Care Unit. Crit Care Nurs Q 2006;29:117–22. [DOI] [PubMed] [Google Scholar]
- [3].Rupp ME, Lisco SJ, Lipsett PA, et al. Effect of a second generation venous catheter impregnated with chlorhexidine and silver sulfadiazine on central catheter-related infections: randomized, controlled trial. Ann Intern Med 2005;143:570–80. [DOI] [PubMed] [Google Scholar]
- [4].Ebrahimipour V, Rezaie K, Shokravi S. An ontology approach to support FMEA studies. Expert Syst Appl 2010;37:671–7. [Google Scholar]
- [5].Paola L, Giancarlo B, Francesca S, et al. Use of FMEA analysis to reduce risk of errors in prescribing and administering drugs in paediatric wards: a quality improvement report. BMJ Open 2012;2:e001249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lu Y, Teng F, Zhou J, et al. Failure mode and effect analysis in blood transfusion: a proactive tool to reduce risks. Transfusion 2013;53:3080–7. [DOI] [PubMed] [Google Scholar]
- [7].Gruber M, Bertran N, Botter M. An innovative approach to improve quality and efficiency in an outpatient oncology setting: creative application of failure mode and effects analysis (FMEA) and best practices. Oncol Nurs Forum 2016;33:444. [Google Scholar]
- [8].Zupa E, Abbotoy J, Koester D. Using failure mode effect analysis (FMEA) to improve medication safety. Oncol Nurs Forum 2006;33:417. [Google Scholar]
- [9].Ho CC, Liao CJ. The use of failure mode and effects analysis to construct an effective disposal and prevention mechanism for infectious hospital waste. Waste Manag 2011;31:2631–7. [DOI] [PubMed] [Google Scholar]
- [10].Joint Commission on Accreditation of Healthcare Organizations. Revisions to Joint Commission Standards in Support of Patient Safety and Medical/HealthCare Error Reduction. Oakbrook Terrace, IL:2002. [Google Scholar]
- [11].Day S, Dalto J, Fox J, et al. Failure mode and effects analysis as a performance improvement tool in trauma. J Trauma Nurs 2006;13:111–7. [DOI] [PubMed] [Google Scholar]
- [12].Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 2008;36:309–20. [DOI] [PubMed] [Google Scholar]
- [13].Towler G, Sinnott R. Chemical Engineering Design, Safety and Loss Prevention. Massachusetts: Elsevier Ltd; 2012. [Google Scholar]
- [14].Puente J, Pino R, Priore P, et al. A decision support system for applying failure mode and effects analysis. J Qual Reliab Manage 2002;19:137–50. [Google Scholar]
- [15].Feili HR, Akar N, Lotfizadeh H, et al. Risk analysis of geothermal power plant using Failure Modes and Effects Analysis (FMEA) technique. Energy Convers Manage 2013;72:69–76. [Google Scholar]
- [16].Vandijck D, Labeau S, Depaemelaere M, et al. Economic impact of catheter-related bloodstream infections. ICU Manage 2007;7:10. [Google Scholar]
- [17].Warrn DK, Yokoe DS, Climo MW, et al. Preventing catheter-associated bloodstream infections: a survey of policies for insertion and care of central venous catheters from hospitals in the prevention epicenter program. Infect Control Hosp Epidemiol 2006;27:8–13. [DOI] [PubMed] [Google Scholar]


