Abstract
Rationale:
Infectious keratitis is a relatively uncommon but potentially sight-threatening complication of laser in situ keratomileusis (LASIK). Mycobacterial keratitis is usually regarded as late onset keratitis among post-LASIK keratitis. There has been no documented case of Mycobacterium intracellulare post-LASIK keratitis of a long-latent period.
Patient concerns:
A 36-year-old man was referred to our out-patient clinic, for persistent corneal epithelial defect with intrastromal infiltration. He had undergone uneventful bilateral LASIK procedure 4 years before. He complained decreased vision, accompanied by ocular pain, photophobia, and redness in his left eye for 7 months.
Diagnosis:
Lamellar keratectomy was taken using femtosecond laser. Bacterial culture with sequenced bacterial 16s ribosomal DNA confirmed the organism to be M intracellulare.
Interventions:
After 3 months of administration of topical clarithromycin, amikacin, and moxifloxacin, the corneal epithelial defect was resolved and the infiltration was much improved. However, newly developed diffuse haziness with surrounding granular infiltration in the central cornea was noted. Drug toxicity was suspected and topical moxifloxacin was discontinued, resulting in resolution of the diffuse haze with infiltration.
Outcome:
The patient was followed up regularly without medication thereafter and recurrence was not found for 7 years.
Lessons:
This case presents the first case of M intracellulare keratitis after LASIK. LASIK surgeons should aware that post-LASIK keratitis can develop long after the operation and careful suspicion of infectious disease with meticulous diagnostic test is needed.
Keywords: keratitis, mycobacterium, Mycobacterium intracellulare, post-LASIK keratitis
1. Introduction
Infectious keratitis is a relatively uncommon but potentially sight-threatening complication of laser in situ keratomileusis (LASIK). Gram-positive microorganisms and nontuberculous mycobacteria (NTM) are the most commonly isolated organisms. The most frequently NTM species causing post-LASIK keratitis are Mycobacterium chelonae and Mycobacterium fortuitum, and only 4 other species, Mycobacterium abscessus, Mycobacterium mucogenicum, Mycobacterium terrae, and Mycobacterium szulgai, have been identified to cause post-LASIK keratitis.[1–5] Mycobacterial keratitis is usually regarded as late onset keratitis among post-LASIK keratitis, when compared with those by gram-positive bacteria, and the most deferred onset post-LASIK NTM keratitis was 3.5 months after LASIK.[1,6]
There are a few reports about late onset bacterial keratitis more than 2 years after LASIK.[7–9] There was, however, no report of keratitis by NTM with such long-latent period after LASIK. Here, we present a case of infectious keratitis, which occurred 4 years after LASIK, caused by M intracellulare. It was diagnosed through lamellar keratectomy followed by culture and managed successfully by long-term administration of topical clarithromycin and amikacin. To the best of our knowledge, this is the first documented case of M intracellulare post-LASIK keratitis of a long-latent period. Ethical approval was not necessary due to the nature of this study (single case report), and the informed consent was obtained from the patient.
2. Case presentation
A 36-year-old man was referred to our out-patient clinic, for persistent corneal epithelial defect with intrastromal infiltration. He had undergone uneventful bilateral LASIK procedure 4 years before. He complained decreased vision, accompanied by ocular pain, photophobia, and redness in his left eye for 7 months. His medical record showed that he was diagnosed of anterior uveitis and was prescribed topical steroid for 1 month before the initiation of present symptom and sign of keratitis. His corneal epithelial defect and infiltration was not noticed at the beginning of topical steroids application. Previous episodes of epithelial defect, corneal edema, and infiltration at LASIK flap interface were improved with use of topical antibiotics and steroids, but not resolved completely during 7 months before he visited our clinic.
At presentation to our clinic, his right eye was normal with best corrected visual acuity (BCVA) 20/20, while left eye showed 1 paracentral perforated LASIK flap and 1 anterior stromal opacity along the LASIK flap interface outside of the pupil at 3 O’clock position (Fig. 1A and B) with BCVA 20/40. Topical 0.5% moxifloxacin eyedrops (Vigamox, Alcon, TX) was prescribed every 2 h. However, flap perforation occurred and density of the remained corneal infiltrate outside of the perforated area increased during next 2 months (Fig. 1C and D). Lamellar keratectomy was taken for bacterial and fungal culture with corneal tissue, using femtosecond laser (IntraLase, IntraLase Corp., Irvine, CA) with size of 2.0 mm in diameter and 290 μm in depth at the site of infiltrative lesion (Fig. 2A). Tissue specimen was sent for the microbiological study including microbiological cultures and bacterial DNA sequencing. Bacterial culture with corneal tissue yielded growth of nontuberculosis mycobacterium. Sequenced bacterial 16s ribosomal DNA confirmed the organism to be M intracellulare. Topical clarithromycin 1% and topical amikacin 4% every 2 h were prescribed with topical moxifloxacin 4 times daily in the left eye. Corneal epithelial debridement was performed to allow more rapid penetration of the topical antibiotics into the cornea. After 3 months of administration of topical clarithromycin, amikacin, and moxifloxacin, the corneal epithelial defect was resolved and the infiltration was much improved (Fig. 2B).
Figure 1.
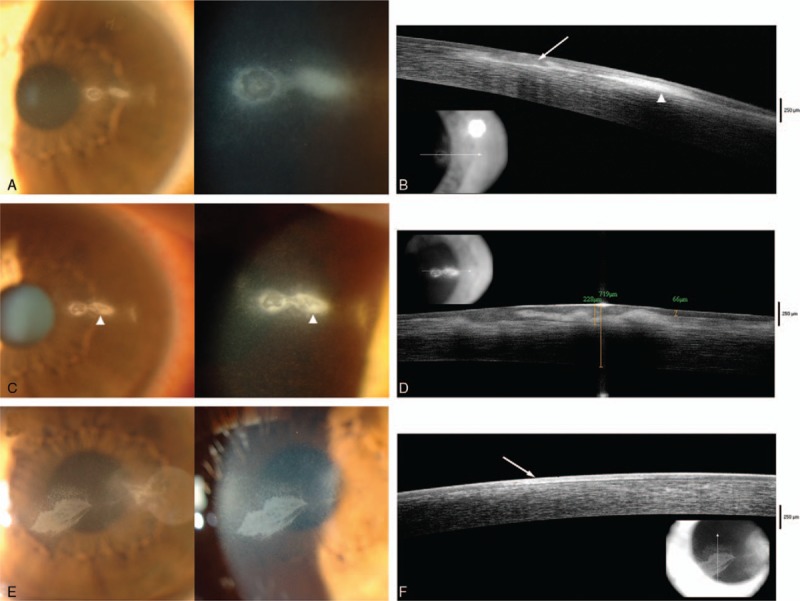
(A) Slit-lamp examination at presentation shows 2 round corneal infiltrates with surrounding edema at 3 O’clock position at initial presentation. (B) Corneal optical coherence tomography shows the LASIK flap was perforated (marked as white arrow) and the infiltration (marked as arrow head) originated from LASIK flap interface. (C) Newly developed LASIK flap perforation on the previously increased corneal infiltrate was noted in slit lamp examination after use of topical moxifloxacin for 1 month (marked as arrow heads). (D) Corneal optical coherence tomography shows perforated flap where the infiltration increased previously. (E) Six months of topical clarithromycin, amikacin, and moxifloxacin to post-LASIK Mycobacterium intracellulare infection produced diffuse epithelial haziness with surrounding small dot-shaped infiltration (marked as arrow heads). (F) Corneal optical coherence tomography confirms this opacity is confined to epithelial layer (marked as white arrow). The infiltration was resolved soon after discontinuation of moxifloxacin.
Figure 2.
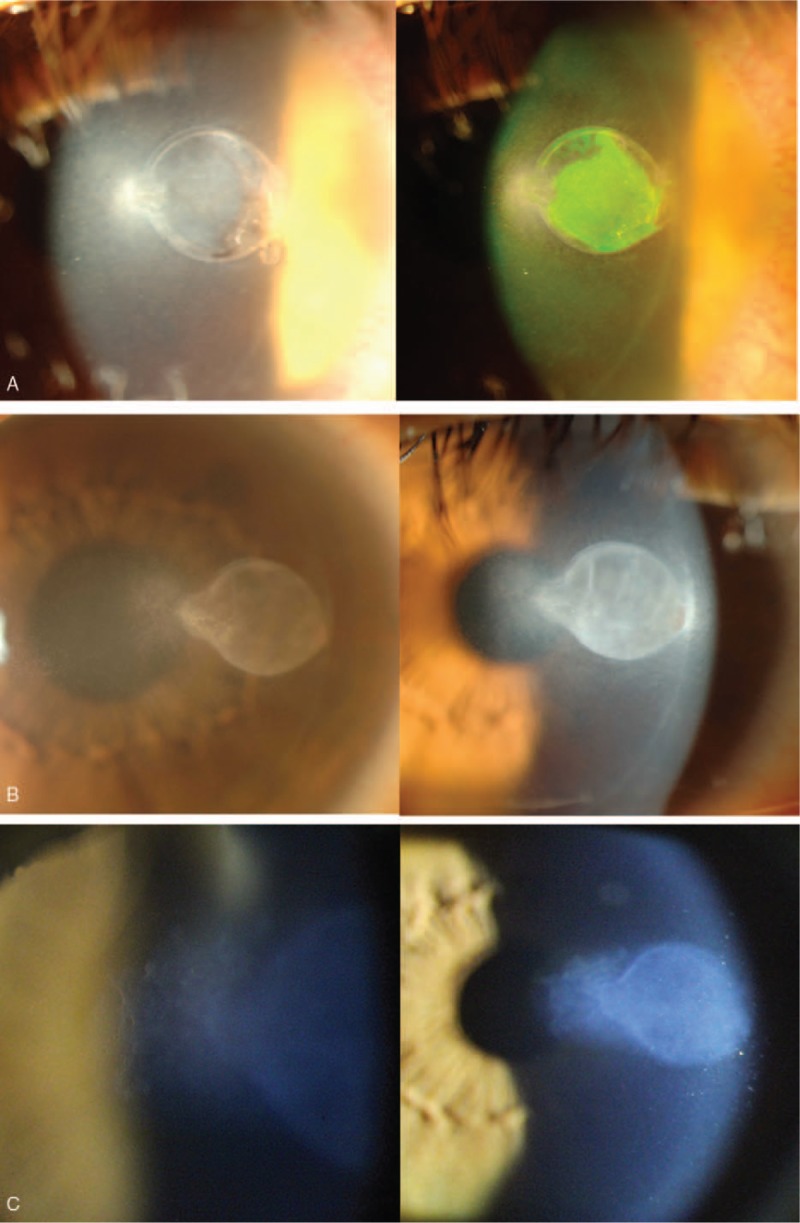
(A) Slit lamp finding 1 day after lamellar keratectomy with femtosecond laser. Newly developed epithelial defect and infiltrative lesion was thought to be the site of active infection, so it was removed completely. (B) After administrating topical clarithromycin, amikacin, and moxifloxacin for 3 months to post-LASIK Mycobacterium intracellulare infection, slit lamp examination showed completely resolved epithelial defect and infiltrative lesion. (C) Stabilized lesion with stromal opacity was noted 7 years after initial presentation.
However, newly developed diffuse haziness (2.5 mm × 1.5 mm sized) with surrounding granular infiltration in the central cornea was noted 6 months after initiation of topical clarithromycin, amikacin, and moxifloxacin (Fig. 1E and F). Drug toxicity was suspected and topical moxifloxacin was discontinued while clarithromycin and amikacin were tapered to 4 times daily resulting in resolution of the diffuse haze with infiltration. Topical amikacin was maintained for 10 months after diagnosis, and topical clarithromycin was prescribed for 13 months. The patient was followed up regularly without medication thereafter and recurrence was not found for 7 years. His corrected visual acuity was 20/20 (Fig. 2C).
3. Discussion
In the literature review, there are 6 species of mycobacterium which had been reported as possible cause of post-LASIK keratitis.[1]Mycobacterium intracellulare is one of the most commonly encountered NTM in the United States which most often affects the lungs. It is classified to Runyon classification III, which is nonchromatogenic, slow growing organism.[10]Mycobacterium intracellulare keratitis has been reported rarely[11–13] but M intracellulare keratitis after LASIK was not described yet.
NTM induced post-LASIK keratitis may be caused by suboptimal sterile preparation of patients and multiple uses of microkeratome blades.[1,5,14] In the usual post-LASIK mycobacterial keratitis cases, the microorganism was introduced to the potential space beneath LASIK flap during surgical procedure and maybe in dormant state until its presentation.
Some cases of post-LASIK keratitis by bacteria other than NTM show latent period of keratitis after the surgery longer than 2 years.[7–9] These reports explain the bacteria, mostly pseudomonas and staphylococcus, invaded through small epithelial break at the flap margin to the interface of lamellar flap. In our case, infection from flap margin is unlikely because mycobacteria are nonflagellated and nonmotile bacteria and the major infiltration in our case was present at the paracentral area of cornea, relatively sparing the margin of flap.[15] Therefore, the bacteria inoculated during LASIK might be in the dormant state during 4 years after procedure to be activated later or might penetrate to the LASIK flap interface through the small epithelial break recently before the initiation of the keratitis.
The NTM keratitis is difficult to treat due to resistance to conventional antibiotics, slow response to therapy requiring protracted treatment period with combined drugs of amikacin, clarithromycin, and 4th-generation fluoroquinolones.[2,4,6,16–18] Multidrug combination therapy has been effective in prior case. The length of medical treatment of NTM keratitis is typically prolonged and no specific guidelines regarding the duration of treatment have been determined. In post-LASIK NTM keratitis cases, treatment duration has ranged from 4 weeks to 9 months, with most resolving after 6 to 8 weeks of treatment.[17,19] In our cases, keratitis was mostly resolved after 3 months of treatment, and treatment was maintained for 13 months and recurrence was not occurred during 7 years of follow up.
Management of NTM keratitis in post-LASIK patient with topical clarithromycin and amikacin is sometimes interrupted due to toxicity of the drugs.[11,13] Surface toxicity and patient discomfort for long period of treatment may limit the dosage of the medication. In our case, the haziness was confined to the epithelium of cornea. Topically administrated ciprofloxacin is well known to cause white corneal deposition of drug, and several other quinolones are reported to cause corneal precipitates.[20] Although corneal precipitates have not been reported with long-term use of moxifloxacin, it might have resulted in the epithelial opacity in our case where it was used for 8 months 4 times a day.
In conclusion, we present the first case of M intracellulare keratitis after LASIK. LASIK surgeons should aware that post-LASIK keratitis can develop long after the operation and careful suspicion of infectious disease with meticulous diagnostic test is needed. After diagnosis of NTM keratitis, combination of topical antibiotics including clarithromycin, amikacin and 4th-generation quinolone can be considered.
Footnotes
Abbreviations: BCVA = best corrected visual acuity, LASIK = laser in situ keratomileusis, NTM = nontuberculous mycobacteria.
EKK is the medical advisory board member of the Avellino LAB USA. Other authors have no conflicts of interest to declare.
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health and Welfare, Republic of Korea (No. HI16C1009).
The authors have no conflicts of interest to disclose.
References
- [1].John T, Velotta E. Nontuberculous (atypical) mycobacterial keratitis after LASIK: current status and clinical implications. Cornea 2005;24:245–55. [DOI] [PubMed] [Google Scholar]
- [2].Fulcher SF, Fader RC, Rosa RH, Jr, et al. Delayed-onset mycobacterial keratitis after LASIK. Cornea 2002;21:546–54. [DOI] [PubMed] [Google Scholar]
- [3].Chung MS, Goldstein MH, Driebe WT, Jr, et al. Mycobacterium chelonae keratitis after laser in situ keratomileusis successfully treated with medical therapy and flap removal. Am J Ophthalmol 2000;129:382–4. [DOI] [PubMed] [Google Scholar]
- [4].Daines BS, Vroman DT, Sandoval HP, et al. Rapid diagnosis and treatment of mycobacterial keratitis after laser in situ keratomileusis. J Cataract Refract Surg 2003;29:1014–8. [DOI] [PubMed] [Google Scholar]
- [5].Chung SH, Roh MI, Park MS, et al. Mycobacterium abscessus keratitis after LASIK with IntraLase femtosecond laser. Ophthalmologica 2006;220:277–80. [DOI] [PubMed] [Google Scholar]
- [6].Chang MA, Jain S, Azar DT. Infections following laser in situ keratomileusis: an integration of the published literature. Surv Ophthalmol 2004;49:269–80. [DOI] [PubMed] [Google Scholar]
- [7].Vieira AC, Pereira T, De Freitas D. Late-onset infections after LASIK. J Refract Surg 2008;24:411–3. [DOI] [PubMed] [Google Scholar]
- [8].Varssano D, Waisbourd M, Berkner L, et al. Late-onset laser in situ keratomileusis-related corneal ulcer—a case series. Cornea 2009;28:586–8. [DOI] [PubMed] [Google Scholar]
- [9].Ferrer C, Rodriguez-Prats JL, Abad JL, et al. Pseudomonas keratitis 4 years after laser in situ keratomileusis. Optom Vision Sci 2011;88:1252–4. [DOI] [PubMed] [Google Scholar]
- [10].Jarzembowski JA, Young MB. Nontuberculous mycobacterial infections. Arch Pathol Lab Med 2008;132:1333–41. [DOI] [PubMed] [Google Scholar]
- [11].Tyagi AK, Kayarkar VV, McDonnell PJ. An unreported side effect of topical clarithromycin when used successfully to treat Mycobacterium avium-intracellulare keratitis. Cornea 1999;18:606–7. [PubMed] [Google Scholar]
- [12].Knapp A, Stern GA, Hood CI. Mycobacterium avium-intracellulare corneal ulcer. Cornea 1987;6:175–80. [DOI] [PubMed] [Google Scholar]
- [13].Ford JG, Huang A, Pflugfelder SC, et al. Nontuberculous mycobacterial keratitis in south Florida. Ophthalmology 1998;105:1652–8. [DOI] [PubMed] [Google Scholar]
- [14].Yamaguchi T, Bissen-Miyajima H, Hori-Komai Y, et al. Infectious keratitis outbreak after laser in situ keratomileusis at a single laser center in Japan. J Cataract Refract Surg 2011;37:894–900. [DOI] [PubMed] [Google Scholar]
- [15].Martinez A, Torello S, Kolter R. Sliding motility in mycobacteria. J Bacteriol 1999;181:7331–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hyon J-Y, Joo M-J, Hose S, et al. Comparative efficacy of topical gatifloxacin with ciprofloxacin, amikacin, and clarithromycin in the treatment of experimental Mycobacterium chelonae keratitis. Arch Ophthal 2004;122:1166–9. [DOI] [PubMed] [Google Scholar]
- [17].Solomon A, Karp CL, Miller D, et al. Mycobacterium interface keratitis after laser in situ keratomileusis. Ophthalmology 2001;108:2201–8. [DOI] [PubMed] [Google Scholar]
- [18].Chandra NS, Torres MF, Winthrop KL, et al. Cluster of Mycobacterium chelonae keratitis cases following laser in-situ keratomileusis. Am J Ophthalmol 2001;132:819–30. [DOI] [PubMed] [Google Scholar]
- [19].Freitas D, Alvarenga L, Sampaio J, et al. An outbreak of Mycobacterium chelonae infection after LASIK. Ophthalmology 2003;110:276–85. [DOI] [PubMed] [Google Scholar]
- [20].Wilhelmus KR, Abshire RL. Corneal ciprofloxacin precipitation during bacterial keratitis. Am J Ophthalmol 2003;136:1032–7. [DOI] [PubMed] [Google Scholar]


