Abstract
Port-wine stains (PWS) are congenital capillary malformations, usually occurring on the face, neck, and other exposed parts of the skin, that have serious psychological and social impact on the patient. Most researchers focus on the treatment of PWS, but the quality of life (QoL) of PWS patients is seldom researched. The objective of this study is to evaluate the QoL of patients with PWS on exposed parts and explore the factors influencing the QoL of PWS patients. The QoL of 197 cases with PWS on exposed parts were prospectively studied using the Dermatology Life Quality Index questionnaire (DLQI), and the factors influencing the patients’ QoL were analyzed by single-factor analysis and multiple-factor logistic regression analysis. The reliability and validity of the QoL of PWS patients were then assessed by DLQI. A total of 197 valid questionnaires were collected. The DLQI scores in PWS cases ranged from 2 to 16, with 2 to 5 in 52.29% (103/197), 6 to 10 in 42.13% (83/197), and 11 to 20 in 5.58% (11/197). The main score elements of the DLQI focused on symptoms and feelings, daily activities, and social entertainment. Single-factor analysis and multiple-factor logistic regression analysis showed that the main influencing factors were female sex, skin hypertrophy, and lesion area >30 cm2. The inter-item correlation averaged 47.46% and the Cronbach α was 0.740, indicating high internal consistency. Correlation of the 6 dimensions of the DLQI questionnaires with the total scores showed that the Spearman correlation coefficient r ranged from 0.550 to 0.782 (P < .001), with symptoms and feelings having a correlation coefficient of 0.782 and a high correlation with total scores. This study shows that PWS has mild to moderate influence on the QoL of most patients, mainly on daily activities, social entertainment, and feelings.
Keywords: Dermatology Life Quality Index (DLQI), port-wine stains (PWS), quality of life, reliability, validity
1. Introduction
Port-wine stains (PWS) are congenital capillary malformations usually occurring on the face, neck, and other exposed parts of the skin, with an incidence 0.3% in newborns. It is a discosmetic dermatosis, and the skin lesions increase with age and can even form papules or nodules or develop into hypertrophic PWS. About a third of hypertrophic PWS ruptures and bleeds when exposed to slight friction (combing hair, shaving),[1] leading to physiological and psychological burden to the patients.
Currently, very few publications have shown a negative impact of PWS on health-related quality of life (QoL) and psychological adjustment in individuals with PWS.[2,3] The objective of this study was to evaluate the QoL of Chinese patients with PWS on exposed parts using the Dermatology Life Quality Index (DLQI) questionnaire, explore the factors influencing the QoL of PWS patients, and assess reliability and validity, which can provide evidence for further psychological intervention and evaluate the effect of therapeutic measure on the QoL of patients.
2. Methods
2.1. Design and sample
This descriptive observational case-control study was carried out at the Anhui Provincial Hospital and at the First Affiliated Hospital of Anhui Medical University. Outpatients seeking treatment for PWS and patients with vitiligo (serving as control) at the Department of Dermatology of Anhui Provincial Hospital and at the Laser Cosmetology Center of the First Affiliated Hospital of Anhui Medical University from January 2013 to December 2016 were assessed for eligibility for this prospective study. Patients younger than 16 years; patients with facial disfigurement; those with concomitant systemic diseases or other dermatoses, or past psychiatric symptoms; and those who were unwilling or unable to communicate were excluded from the study.
2.2. Ethical considerations
This research was approved by the Anhui Provincial Hospital and the First Affiliated Hospital of Anhui Medical University. All subjects gave written informed consent before their inclusion in the study. Ethical standards for research on human beings were based on the Declaration of Helsinki (World Medical Association) and the Convention of the Council of Europe on Human Rights and Biomedicine.
2.3. Procedure
A total of 200 and 198 Chinese patients with PWS and vitiligo, respectively, participated in the study. The skin lesions in all the patients were located on exposed parts. The patients with vitiligo were enrolled as control and were matched with the PWS patients in terms of age, sex, educational level, working status, marital status, residence, and so on. Demographic data and disease-related characteristics were collected in detail, including sex, age, educational background, habitation, marital status, working condition, size and distribution of skin lesions, and so on.
The DLQI questionnaire (http://www.dermatology.org.uk/), designed by Finlay and Khan[4] in 1994 is a self-administered, easy, and user-friendly questionnaire that has been validated for dermatology patients aged 16 years and older. It consists of 10 questions concerning patients’ perception of the impact of skin diseases on different aspects of their QoL over the last week: Q1, symptoms; Q2, feelings; Q3, daily activities; Q4, clothing; Q5, leisure; Q6, sport; Q7, work or school; Q8, relationships; Q9, sexual difficulties; Q10, treatment. These 10 questions covered 6 dimensions, namely, symptoms and feelings (Q1 and Q2), daily activities (Q3 and Q4), leisure (Q5 and Q6), work or school (Q7), personal relationships (Q8 and Q9), and treatment (Q10).
In this study, the skin lesions of the patients mainly appeared on the head or face, which could be covered by special hairstyles; thus, the fourth question was modified as, “In last week, how much did skin problems influence your choice of clothes or hairstyle?” Each item was scored on a 4-point scale: 0, not at all/not relevant; 1, a little; 2, a lot; 3, very much. Scores of individual items (0–3) are added to yield a total score ranging from 0 to 30, with a higher score indicating greater impairment of the patient's QoL. The DLQI bands are as follows: 0 to 1, no effect; 2 to 5, small effect; 6 to 10, moderate effect; 11 to 20, very large effect; 21 to 30, extremely large effect.
The purpose of the investigation was explained to all appropriate patients, and they were informed that participation was voluntary and that the results were harmless and confidential. After informed consent was obtained from the subjects, the questionnaires were distributed, and using unified instruction, the importance of answering the questionnaires was explained in detail. Respondents who could understand the questions finished the scale test independently, whereas those who could not understand the questions were assisted by doctors in finishing the questionnaire through oral and explanation. Then, the questionnaires were collected for analysis.
2.4. Statistical analysis
All valid data were analyzed using SPSS16.0 statistical software (IBM, Armonk, NY), with P < .05 being statistically significant. Measurement data was non-normal distribution and the results are described as median and interquartile range expressed, using rank sum test. The QoL of PWS patients was studied by multifactor nonconditional logistic regression analysis. Construct validity was tested by factor analysis. Reliability was assessed using Cronbach α according to the accepted standard α > 0.7. The correlation among the dimensions of the DLQI questionnaires was analyzed by Spearman correlation.
3. Results
3.1. Questionnaire completion and DLQI scores
Of the 200 PWS patients, 198 patients answered the questionnaire; however, 1 PWS patient answered only 6 questions and was excluded. Hence, 197 patients effectively finished the DLQI questionnaire (98.5%). In 198 vitiligo patients, 1 patient refused to accomplish questionnaire and 1 patient answered only 3 questions. Hence, 196 vitiligo patients effectively finished the DLQI questionnaire (98.99%). It took them 1 to 2 minutes to fulfill the questionnaires independently.
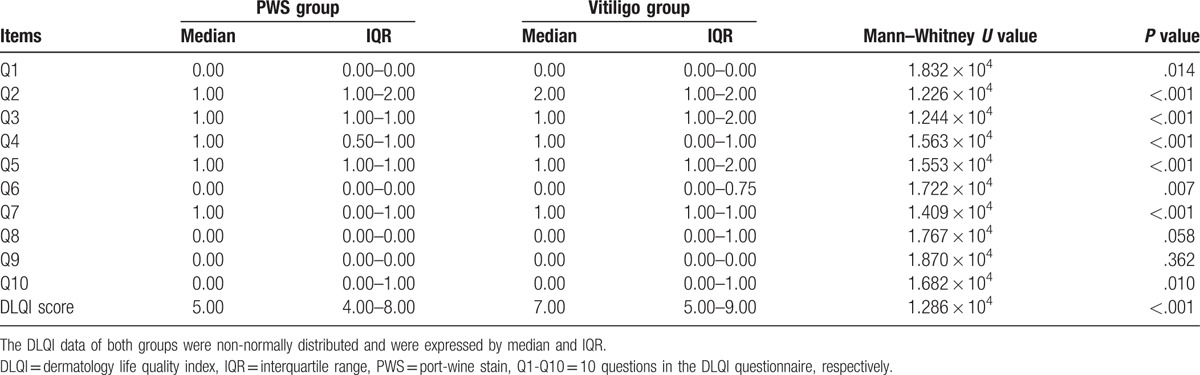
The DLQI scores of PWS and vitiligo patients ranged from 2 to 16 and from 2 to 17, respectively. None of the patients scored 0 to 1 or 21 to 30. The DLQI scores of PWS patients were mainly distributed from 2 to 5 (52.29%) and from 6 to 10 (42.13%), which suggested that PWS had a small and moderate effect on QoL. The DLQI score of vitiligo patients was mainly distributed from 6 to 10 (57.65%) (Table 1). Feelings, daily activities, and social interactions and entertainment are the major scoring elements of DLQI in PWS patients and vitiligo patients. Comparison of PWS and vitiligo patients showed no statistical significance in social relationship and sexual activity (P>.05), but all other aspects had statistical difference (Table 2).
Table 1.
Banding of the Dermatology Life Quality Index with the scores of both groups.
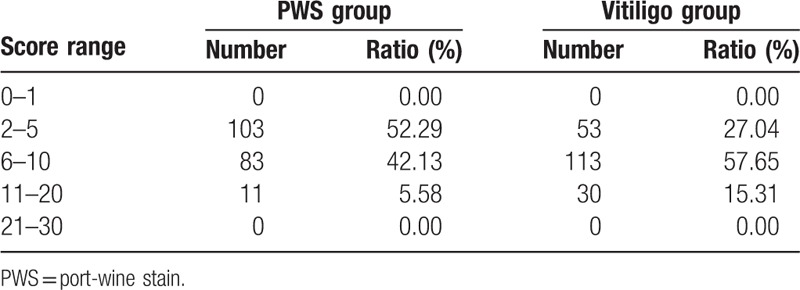
Table 2.
Individual and total Dermatology Life Quality Index scores of both groups.
3.2. Single- and multiple-factor analyses
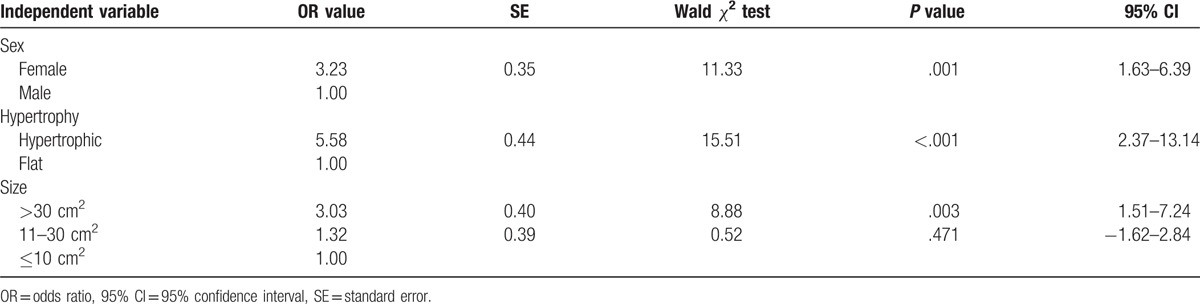
The single-factor analysis showed that the factors that possibly affected DLQI score in PWS patients were sex, hypertrophy, and skin color and size (P<.05) (Table 3). Meanwhile, the multiple-factor regression analysis showed that the major factors influencing the QoL of PWS patients were sex, hypertrophy, and size of skin lesion (P<.05; odds ratio, >1) (Table 4).
Table 3.
Demographic data and disease-related characteristics of the groups of patients.
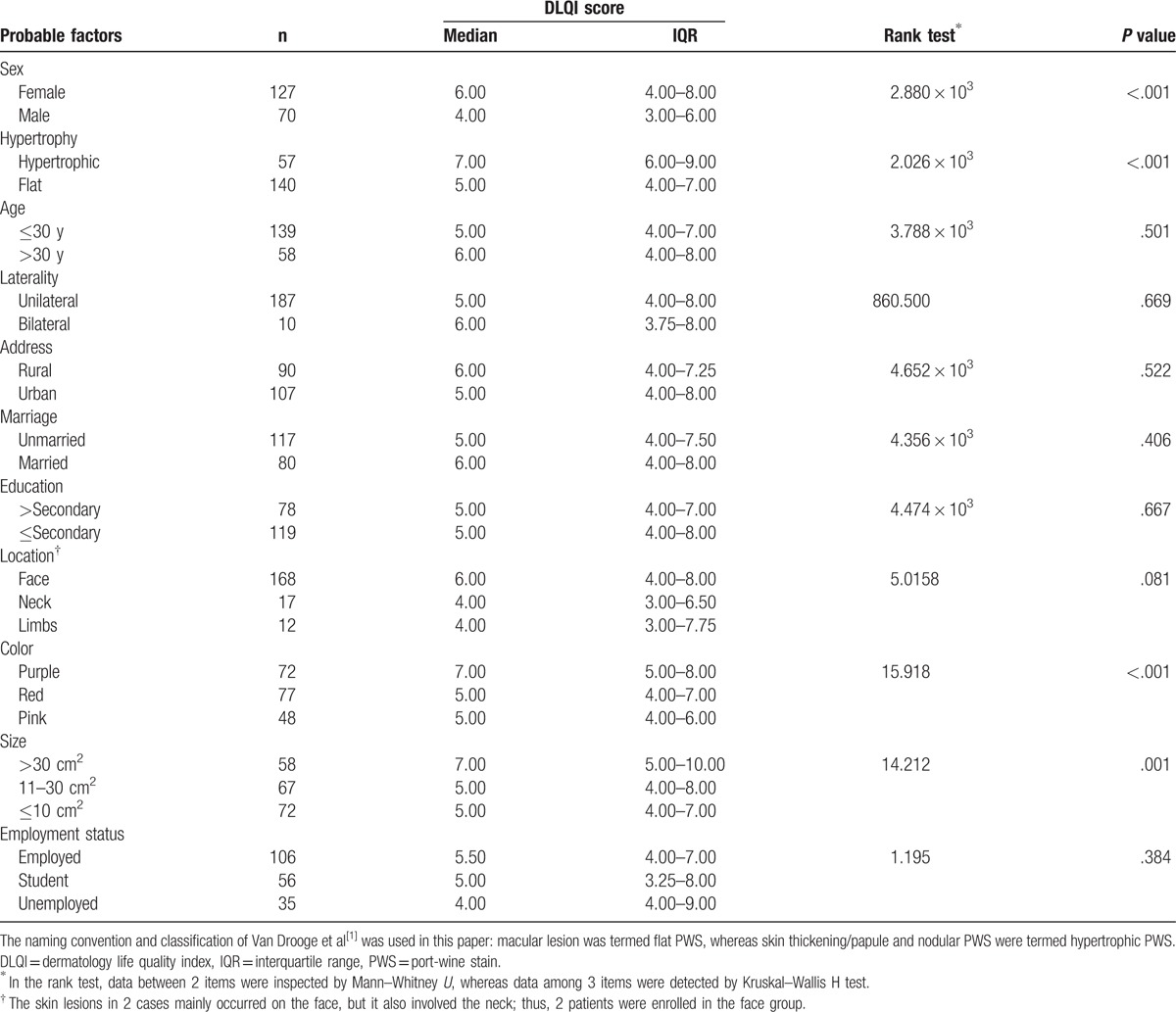
Table 4.
Multiple-factor analysis of factors that correlated with the Dermatology Life Quality Index score in 197 patients with port-wine stain.
3.3. Validity and reliability
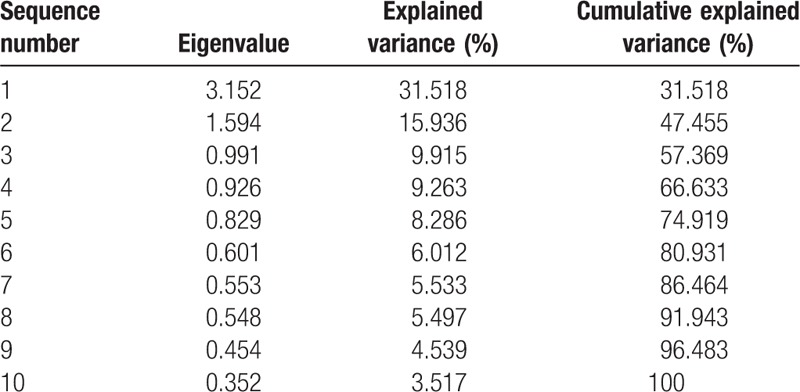
In 197 effective questionnaires, the Kaiser–Meyer–Olkin value (0.786) and Bartlett test of sphericity (χ2 = 421.268, P < .001) support the factor analysis. Through factor analysis of the DLQI questionnaire, the inclusion criteria determined that the eigenvalue was greater than 1; 2 common factors were extracted, and their cumulative contribution rate was 47.46%, which was greater than the minimum standard (40%) of the construct validity test (Table 5). The scree plot shows a decrease in the eigenvalues from the first and second components to the subsequent components, with the subsequent components extracting progressively less from the variance.
Table 5.
Results of the factor analysis of the Dermatology Life Quality Index questionnaire.
Hotelling T statistic (F = 211.707, P < .001) showed that inequality existed in each item of the DLQI questionnaire. The Cronbach α (scale reliability coefficient) of the DLQI score was 0.740, which was higher than the traditional threshold of 0.7, indicating a high degree of internal reliability in the questionnaire; hence, it reflects real and reliable QoL of PWS patients.
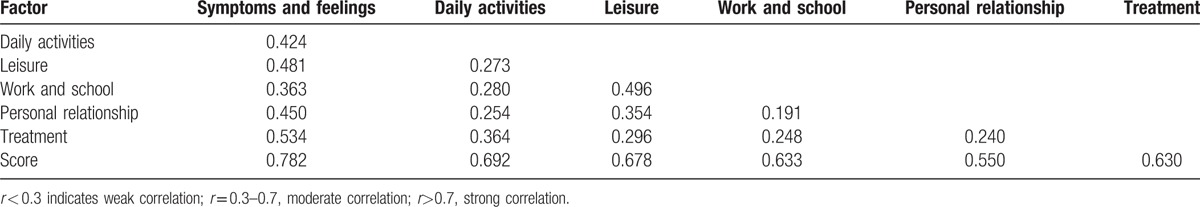
3.4. Correspondence analysis
The correlation coefficient r between 10 items and the DLQI scores ranged from 0.300 to 0.747 (P < .001), whereas the correlation coefficient r between the 6 dimensions and the DLQI score ranged from 0.550 to 0.782 (P < .001), which showed correlation; the r value of symptoms and feelings was the highest, suggesting strong correlation to the DLQI score and then to daily life, leisure, and recreation; personal relationship was the item that least correlated with DLQI score. The correlation coefficient r among the 6 dimensions ranged from 0.191 to 0.534 (P < .001), showing good differentiation among the 6 dimensions (Table 6).
Table 6.
Correlation coefficient matrix among the 6 dimensions of the Dermatology Life Quality Index questionnaire.
4. Discussion and conclusions
As an acknowledged psychosomatic disease, vitiligo has such serious effects on patients’ QoL and mental health that it has attracted the attention of many researchers worldwide. Different rating scales on assessing QoL are widely used on the patients,[5–11] especially DLQI, which has been translated into various languages.[7–11] Furthermore, Wang et al[12] tested and verified the validity and reliability of the DLQI in Chinese version with the help of Professor Andrew Finlay in the University of Wales in 2004, demonstrating that the DLQI in Chinese version was a simple and feasible evaluation tool that could be used for measuring the quality of life in Chinese patients with dermatosis. Thereafter, the Chinese DLQI has been also widely used for treating chronic urticaria,[13] psoriasis,[14] neurodermitis,[15] female genetic alopecia,[16] alopecia areata,[17] and so on, and its reliability and validity have been recognized. PWS is a type of discosmetic dermatosis that has no obvious damage to physical function, and reports of its impact on patients’ QoL are rare. This was the first study that attempted to evaluate the QoL of patients with PWS on exposed parts using the DLQI questionnaire, explored the factors influencing the QoL of PWS patients, analyzed its reliability and validity, and evaluated the feasibility on QoL of PWS patients.
The results showed that the DLQI score scope of PWS patients mainly ranged from 2 to 5 scores (52.29%) and from 6 to 10 scores (42.13%), while the median was 5 scores. The results showed that PWS mostly had mild to moderate impacts upon the quality of life in the patients. According to Spearman correlation analysis, PWS imposed the most significant negative impacts upon patients’ feelings about symptoms. All these research findings are in line with the research results of Hagen.[2] It often caused patients to experience inferiority and social avoidance and fear, thus influencing work, study, interpersonal relations, and other aspects of their daily life. The DLQI average score of PWS patients was lower than that of vitiligo patients, which can possibly be attributed to the damage brought about by PWS on the skin, and since it is a congenital condition, the disease course is very long, whereas vitiligo is a disease acquired after birth, peaking during adolescence. Vitiligo patients have much lower acceptance and self-evaluation.
Sex, age, education, habitation, marriage, employment status, size, and distribution of skin lesions are the factors that possibly affect the QoL of PWS patients. Single-factor analysis suggested that female patients, those with hypertrophic PWS, and those with large lesion area (>30 cm2) had higher DLQI scores and worse QoL. Multiple-factor logistic analysis showed that sex, hypertrophic PWS, and large affected areas were the main factors influencing the QoL of PWS patients, with most female patients paying more attention to their appearance and felt inferior because of the difficulty in hiding the affected skin areas. As some patients with hypertrophic PWS experienced ulceration, hemorrhage, and pain after exposure to slight friction, they could have erroneously identified the lesions progressed to cancer and became increasingly worried, thus influencing their QoL. The color of damage was very important in the single-factor analysis, but it was not a main influencing factor in the multiple-factor analysis. This may be because most of the damage in hypertrophic PWS was prunosus, becoming deeper with the gradual thickening of the skin lesions.
In this study, educational level, habitation, marital status, and employment status were not the main factors influencing QoL, and this can be attributed to advances in information, transportation, and communication. Age has no statistical significance in either single- or multiple-factor analysis, because most young PWS patients were plat type, and they could cover the lesion with proper clothing, hairstyle, and/or cover cream. However, patients in their 30 seconds and especially 40 seconds have a higher rate of PWS thickening and the color becomes deeper, thus having worse effects on their QoL. Lesion location also has no effects on QoL, but this may be because the lesion locations were in exposed parts of body in the study and we only generally classified the damage zones into face, neck, and limbs. In future studies with more samples, the facial zones should be subdivided to understand if damages in different parts have different impacts on QoL.
In conclusion, PWS has slight or midrange influence on the QoL of patients, affecting their daily activities and mental perception, which can result in social avoidance and distress. Thus, during treatment of female PWS patients, those whose lesion areas >30 cm2, or those with hypertrophic PWS, close attention should be paid to the assessment of their QoL and mental status while estimating the extent of their damage. Besides laser therapy, a series of supportive therapies with the aim of answering their questions, correcting their misunderstandings, improving their QoL, and helping them regain their confidence should be performed.
Acknowledgments
The authors acknowledge Dr YF Zou and Dr FM Pan (Department of Epidemiology and Biostatistics, School of Public Health, Anhui Medical University, Hefei, China) for their advice regarding Statistical Analysis. The authors also thank Editage (www.editage.com) for English language editing.
Footnotes
Abbreviations: DLQI = Dermatology Life Quality Index, PWS = port-wine stains, QoL = quality of life.
JW and Y-yZ contributed to this study equally.
The authors have no conflicts of interest to disclose.
References
- [1].van Drooge AM, Beek JF, van der Veen JP, et al. Hypertrophy in port-wine stains: prevalence and patient characteristics in a large patient cohort. J Am Acad Dermatol 2012;67:1214–9. [DOI] [PubMed] [Google Scholar]
- [2].Hagen SL, Grey KR, Korta DZ, et al. Quality of life in adults with facial port-wine stains. J Am Acad Dermatol 2017;76:695–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Schiffner R, Brunnberg S, Hohenleutner U, et al. Willingness to pay and time trade-off: useful utility indicators for the assessment of quality of lifeand patient satisfaction in patients with port wine stains. Br J Dermatol 2002;146:440–7. [DOI] [PubMed] [Google Scholar]
- [4].Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol 1994;19:210–6. [DOI] [PubMed] [Google Scholar]
- [5].Salzes C, Abadie S, Seneschal J, et al. The Vitiligo Impact Patient Scale (VIPs): development and validation of a vitiligo burden assessment tool. J Invest Dermatol 2016;136:52–8. [DOI] [PubMed] [Google Scholar]
- [6].Bonotis K, Pantelis K, Karaoulanis S, et al. Investigation of factors associated with health-related quality of life and psychological distress in vitiligo. J Dtsch Dermatol Ges 2016;14:45–9. [DOI] [PubMed] [Google Scholar]
- [7].Sangma LN, Nath J, Bhagabati D. Quality of life and psychological morbidity in vitiligo patients: a study in a teaching hospital from north-east India. Indian J Dermatol 2015;60:142–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Karelson M, Silm H, Kingo K. Quality of life and emotional state in vitiligo in an Estonian sample: comparison with psoriasis and healthy controls. Acta Derm Venereol 2013;93:446–50. [DOI] [PubMed] [Google Scholar]
- [9].Ingordo V, Cazzaniga S, Medri M, et al. To what extent is quality of life impaired in vitiligo? A multicenter study on Italian patients using the dermatology life quality index. Dermatology 2014;229:240–7. [DOI] [PubMed] [Google Scholar]
- [10].Wong SM, Baba R. Quality of life among Malaysian patients with vitiligo. Int J Dermatol 2012;51:158–61. [DOI] [PubMed] [Google Scholar]
- [11].Wang KY, Wang KH, Zhang ZP. Health-related quality of life and marital quality of vitiligo patients in China. J Eur Acad Dermatol Venereol 2011;25:429–35. [DOI] [PubMed] [Google Scholar]
- [12].Wang XL, Zhao TE, Zhang XQ, et al. [Assessment on the reliability and validity of the Dermatology Life Quality Index in Chinese version]. Zhonghua Liu Xing Bing Xue Za Zhi 2004;25:791–3. [PubMed] [Google Scholar]
- [13].Liu JB, Yao MZ, Si AL, et al. Life quality of Chinese patients with chronic urticaria as assessed by the dermatology life quality index. J Eur Acad Dermatol Venereol 2012;26:1252–7. [DOI] [PubMed] [Google Scholar]
- [14].He Z, Lu C, Basra MK, et al. Psychometric properties of the Chinese version of Dermatology Life Quality Index (DLQI) in 851 Chinese patients with psoriasis. J Eur Acad Dermatol Venereol 2013;27:109–15. [DOI] [PubMed] [Google Scholar]
- [15].An JG, Liu YT, Xiao SX, et al. Quality of life of patients with neurodermatitis. Int J Med Sci 2013;10:593–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Zhuang XS, Zheng YY, Xu JJ. Quality of life in women with female pattern hair loss and the impact of topical minoxidil treatment on quality of life in these patients. Exp Ther Med 2013;6:542–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Qi S, Xu F, Sheng Y, et al. Assessing quality of life in alopecia areata patients in China. Psychol Health Med 2015;20:97–102. [DOI] [PubMed] [Google Scholar]


